Abstract
An antibody microarray assay was developed for Salmonella serotyping based on the Kauffmann-White scheme. A model (8 by 15) array was constructed using 35 antibodies for identification of 20 common Salmonella serovars and evaluated using 117 target and 73 nontarget Salmonella strains. The assay allowed complete serovar identification of 86 target strains and partial identification of 30 target strains and allowed exclusion of the 73 nontarget strains from the target serovars.
The genus Salmonella consists of over 2,500 serovars, as determined by its somatic (O) and flagellar (H) antigens. A slide agglutination test is commonly used in serotyping for Salmonella spp. based on the Kauffmann-White scheme (11, 12), which involves over 250 antisera. The current serotyping method only allows detection of a single antibody-antigen reaction at a time, requires well-experienced technologists to perform, consumes relatively high volumes of reagents, and takes a minimum of 3 days to perform a minimum of three antibody-antigen reactions to determine a serotype. The number of reactions and the time required can be many times greater if a less-common serovar is tested.
DNA-based alternative approaches, such as PCR, have been developed to identify a particular serovar (1, 7). However, the PCR methods only detect a limited number of serovars at a time, and many different genetic markers are still to be developed or verified for identification of various serovars (8). In this research, a new antibody microarray-based assay that allows parallel analysis of multiple antigens was investigated for Salmonella serotyping.
Salmonella antisera were purchased from Statens Serum Institut (Copenhagen, Denmark) or provided by the Office International des Épizooties Reference Laboratory for Salmonellosis, Public Health Agency of Canada (Guelph, Ontario, Canada). The antisera were diluted to 1 to 5 mg protein per ml in Micro Printing buffer (TeleChem International, Sunnyvale, CA), and then spotted in quadruplets at a density of 400 spots/cm2 onto SuperEpoxy microarray slides (TeleChem International) under a humidity of 58 to 60% with SMP8 spotting pins (TeleChem International) using the SpotBot Protein Edition arrayer (TeleChem International). The epoxy-functionalized glass slide allowed completion of the coupling reaction within 10 min after printing. Cy5-labeled dCTP (Amersham Biosciences, Baie d'Urfe, Quebec, Canada) was included in the spotting solution at a concentration of 20 fmol/μl to monitor spotting quality. The slides were scanned after spotting under the Cy5 channel (670 nm) of the scanner so that the slides with compromised spotting quality were identified prior to their use.
Salmonella strains (Table 1) were obtained from the OIE Reference Laboratory for Salmonellosis, Public Health Agency of Canada. Overnight cultures (0.5 ml) were inactivated at 63°C for 10 min and washed with 1.0 ml phosphate-buffered saline (PBS). The cells were fluorescently labeled by incubating the cells for 30 min in 100 μl PBS containing 5 μl Eosin Y solution [0.2% of Eosin Y (Sigma, Oakville, Ontario, Canada), 0.02% of phloxine B, and 0.5% glacial acetic acid in 60% ethanol]. The cells were collected and resuspended in 300 μl of blocking buffer (0.2 mg/ml bovine serum albumin and 50 mg/ml skim milk in PBS). The cell suspension was applied to a microarray slide in a hybridization chamber gasket (Molecular Probes, Eugene, OR), incubated at room temperature for 60 min in a humidity chamber, then washed three times with PBS plus 0.1% Tween 20 and twice with PBS, and dried with a slide centrifuge.
TABLE 1.
Target Salmonella serovars tested by the protein microarray assay
| Serovar | No. of strainsb | Antigen formulasa | Positive microarray results |
|---|---|---|---|
| Agona | 5 | 1,4,[5],12:f,g,s:[1,2] | 4,5,12:G,s |
| 2 | 1,4,[5],12:f,g,s:[1,2] | 4,5,12:G,h | |
| Berta | 5 | 1,9,12:[f],g,[t]:- | 9,12:G,[t],h |
| Braenderup | 3 | 6,7,14:e,h:e,n,z15 | 5,61,7:h:z15,s |
| 2 | 6,7,14:e,h:e,n,z15 | 5,61,7:h,s | |
| Brandenburg | 5 | 4,[5],12:1,v:e,n,z15 | 4,12:L,v:z15 |
| Derby | 6 | 1,4,[5],12:f,g:[1,2] | 4,5,12:G |
| Enteritidis | 9 | 1,9,12:[f],g,m,[p]:[1,7] | 9,12:G,m,[h] |
| Hadar | 5 | 6,8:z10:e,n,x | 5,61,8:z10:x,L |
| Heidelberg | 9 | 1,4,[5],12:r:1,2 | 4,5,12:r:2 |
| Infantis | 4 | 6,7,14:r:1,5 | 61,7:r:5,s |
| 1 | 6,7,14:r:1,5 | r,m,s | |
| Javiana | 5 | 1,9,12:1,z28:1,5 | 9,12:L,z28:5,h,G |
| Mbandaka | 5 | 6,7,14:z10:e,n,z15 | 5,61,7:z10:z15,s |
| Montevideo | 6 | 6,7,14:g,m,[p],s:[1,2,7] | 61,7:G,s |
| Muenchen | 5 | 6,8:d:1,2:[z67] | 61,8:d:2 |
| 1 | 6,8:d:1,2:[z67] | 5,8:d | |
| Newport | 5 | 6,8,20:e,h:1,2:[z67] | 61,8:h:2 |
| Oranienburg | 5 | 6,7,14:m,t:[z57] | 61,7:m,t |
| Panama | 5 | 1,9,12:1,v:1,5 | 9,12:L,v:5,h |
| Saintpaul | 5 | 1,4,[5],12:e,h:1,2 | 4,5,12:h:2 |
| Stanley | 5 | 1,4,[5],12,27:d:1,2 | 4,5,12:d:2 |
| Thompson | 4 | 6,7,14:k:1,5 | 61,7:k:5,G,i,s |
| 1 | 6,7,14:k:1,5 | 61,7:5 | |
| Typhimurium | 9 | 1,4,[5],12:i:1,2 | 4,5,12:i:2 |
O or H factor that may be present or absent without relation to phage conversion is in brackets; somatic factors that are determined by phage conversion are underlined.
The microarray profiles allowed correct one-step identification of 86 strains (bold type).
Antibody-antigen reaction signals were scanned using the VersArray ChipReader and its associated software (Bio-Rad) on the Cy3 (570 nm) channel. Images were analyzed qualitatively by visual examination. The presence of fluorescent signal at a particular spot was considered positive for the corresponding antibody-antigen reaction. Quality control for slide and cell processing was achieved by including pools of antibodies on the array, including commercial poly A and poly B, two pools of O factor antisera (OC1 and OC2), and two pools of H factor or H phase antisera (HC1 and HC2) that were also used as individuals on the microarray. Positive signals for at least one of the control pools indicate normal performance of the assay.
Antibody array construction.
Two types of commercial microarray slides, SuperAldehyde and SuperEpoxy substrates, were tested. Antibodies were successfully immobilized onto both types of the slides. The SuperEpoxy substrate was preferred and used in our microarray construction because it did not require additional cross-linking, baking, or drying for antibody coupling and allowed completion of the coupling reaction within 10 min after printing. Two types of printing buffers, Micro Printing and Protein Printing, were compared. The former resulted in higher printing quality.
Optimal antibody concentrations were determined by testing serial dilutions (equivalent to protein concentrations from 0.3 to 15 mg/ml) of each antibody for printing and by the reaction signals generated using 20 reference strains of 20 target serovars (Table 1). Different antibodies exhibited different optimal concentrations which also varied with different strains used (Fig. 1). Overall, the optimal antibody concentration ranged from 1 to 5 mg/ml, which is similar to what was reported by other researchers (3). We also found that the printed slides could be stored at room temperature in a slide box for up to a week prior to use (prolonged storage was not tested in this study) and that storing the printed slides overnight at room temperature in a desiccator with 10% humidity or at 4°C in a slide box significantly reduced the reactivity of the antibodies on the slides. In addition, we found that adding Cy5-dCTP to the printing buffer provided a simple way to monitor the printing quality without noticeable adverse effects. The Cy5 dye signal can also be used to normalize the fluorescence signals of samples for data analysis. Labeling the antisera can be a better alternative but was not attempted in this research.
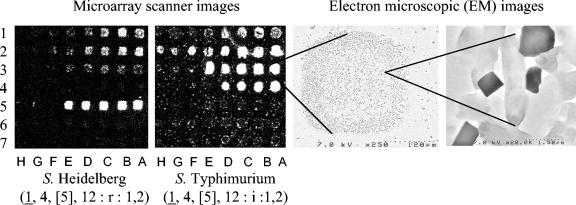
FIG. 1.
Examples of antibody microarray images, indicating (a) the cells captured by the antibody microarray; (b) both phase flagellar (H1 and H2) antigens and O antigens detected simultaneously; and (c) different antibodies exhibited different optimal concentrations which also varied with different strains used. Rows 1 to 7 of the microarrays contained antibodies O:4, O:5, H:2, H:i, H:r, O:9, and H:m. Columns A to H of the microarrays represent twofold (0, 2, 4, 8, 16, 32, 64, and 128) serial dilutions of the original antibody concentrates whose protein concentrations were between 16 and 54 mg/ml. The two electron microscopic images were taken at magnifications of ×250 and ×20,000, respectively.
Salmonella cell labeling.
Two fluorescent dyes, Eosin Y and Cy3 monofunctional reactive dye (Amersham Biosciences), were tested for labeling Salmonella cells by directly incubating the cells with the dyes. The cells labeled with either of the dyes consistently produced similarly strong fluorescent signals when scanned under the Cy3 (570 nm) channel of the scanner. Eosin Y has been used to study histology slides for more than 30 years (10) and to our knowledge has not been described for use as a fluorescence dye in microarray experiments. It is similar in absorption and fluorescence (2) to Cy3 but is much less expensive and easier to handle since it is stable at room temperature in a water solution. The Salmonella cell labeling method developed in this research was simple to perform with low cost. The free dye can be separated and removed simply by washing the cells. No column separation was necessary, as required by other protein labeling methods.
Salmonella cell capturing.
It was necessary to preblock the unreacted epoxide groups on the microarray before applying the labeled Salmonella cells for capturing. Blocking buffer containing skim milk and bovine serum albumin was effective in reducing background and increasing positive signals significantly. It has been described that blocking unreacted functional groups on a microarray with 1% bovine serum albumin was effective to test cell adhesion using microarrays (5). Skim milk may have blocked the nonspecific binding of antigens to the epoxy substrate of the microarray. It may have also reduced antibody loss on the microarray. After the arrays were blocked, labeled cells were applied directly on top of the array and captured by the immobilized antibodies specifically. The optimal volume of the overnight cultures used for capturing was approximately 0.5 ml (equivalent to 2 ×109 to 5 ×109 cells), which gave the most intensive positive signals, as determined by testing culture volumes ranging from 0.05 to1.5 ml (data not shown). In the assay, a cell inactivation step was included prior to applying the cells onto the microarray slides to minimize the risk of Salmonella infection of assay operators. We found that inactivating Salmonella cells by brief heating at 63°C had little negative impact on simultaneous detection of different antigens.
Simultaneous detection of somatic O and flagellar H1 and H2 antigens.
In traditional Salmonella serotyping assays, O serogroups and H phase 1 and phase 2 antigens need to be tested separately. In this study, they were detected simultaneously in a single test. As illustrated by the example in Fig. 1, the O serogroups O:4 and O:5, the H phase 1 antigen H:i, and the H phase 2 antigen H:2 were detected simultaneously for the serovar Typhimurium; similar results were obtained for the serovar Heidelberg, which exhibited a positive reaction to the H phase 1 antibody H:r instead of H:i. This allowed one-step identification of the serovars. Most Salmonella strains express one flagellar antigen at a time in a single cell, with a switching rate of 10−3 to 10−5 for expressing different antigens and need to grow in a medium containing specific phase 1 antiserum to force the expression of phase 2 antigens (phase inversion) to facilitate their detection with specific antibodies (6). The microarray developed in this study did not involve any phase inversion, although some of the H phase 2 antibody-antigen reactions resulted in weak signals, such as the H:2 reaction for the serovar Heidelberg (Fig. 1). Use of different antibodies or cell growth and treatment conditions in future studies may improve these phase 2 reactions.
Evaluation of a model antibody array for Salmonella serotyping.
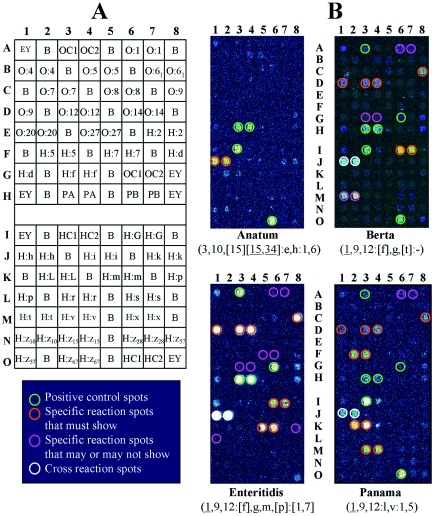
The existing Kauffmann-White scheme was used to devise combinations of antisera for typing 20 commonly isolated and clinically important Salmonella serovars (Table 1). A model microarray was constructed to contain 35 antibodies, including 11 O factor antisera, 9 H phase antisera, 13 H factor antisera, and 2 O multigroup antisera. Figure 2A demonstrates the layout of the antisera within the 8 by 15 array. The model antibody array was evaluated using 117 Salmonella strains that belonged to the 20 target serovars (Table 1) and 73 strains that belonged to 38 nontarget serovars. The microarray profiles allowed correct one-step identification of 86 (bold text in Table 1) of the 117 target strains.
FIG. 2.
Representative microarray images for identification of Salmonella serovars using the model antibody microarray assay. Panel A: map of the antibodies on the model microarray. EY, Eosin Y solution (used for locating arrays). B, printing buffer. PA and PB, poly A and poly B, respectively. OC1 and OC2, pools of O factor antisera; HC1 and HC2, pools of H factor/phase antisera that were also used as individuals on the microarray. Panel B: microarray images for identification of Salmonella serovars Berta, Enteritidis, and Panama and also for exclusion of serovar Anatum from the 20 target serovars. The figure represents half of the actual array (the duplicate part is not shown).
Figure 2B shows representative images of the serotyping results for serovars Anatum, Berta, Enteritidis, and Panama. Fourteen additional strains (9 Enteritidis and 5 Berta, italic text in Table 1) exhibited positive reactions to their corresponding antibodies, although their serovars could not be finalized due to the incomplete antibody panel on the microarray. The remaining 17 strains that belonged to serovars Agona (two strains), Braenderup (two strains), Infantis (one strain), Montevideo (six strains), Muenchen (one strain), and Thompson (five strains) could not be identified because some of their flagellar antigens did not react to their specific antibodies, particularly H:2, H:k, H:m, H:s, and H:z15. One strain of serovar Infantis showed a specific positive reaction only to H: r, and nonspecific reactions to H:m and H:s. Repeated testing of the strains resulted in the same microarray patterns.
The microarray results also allowed exclusion of all 73 nontarget strains from the 20 target serovar list. For example, serovar Anatum did not react to any of the specific antisera on the array except the controls and H:h so it was excluded from the target serovar list. Weak or strong cross-reactions were observed with 8 of the 35 antibodies, particularly with O:5, H:h, and H:s. Most of the cross-reactions, however, did not interfere with data interpretation.
The antibodies were polyclonal rabbit antisera previously tested to be specific using the traditional agglutination method. The reasons for their cross-reactions in the microarray tests could be that the microarray detection may exhibit strong signals for the “late” or “weak” reactions which, as observed visually, are considered negative in the traditional agglutination test. Inclusion of more specific antibodies and additional antibodies on the microarray might minimize the impact of the cross-reactions and allow exclusion of closely related serovars. One of the advantages of the microarray-based test is the flexibility to allow the addition of an extensive selection of the required antisera on the same microarray in order to complete serotyping in a single test.
The model array was designed to cover the top 20 commonly isolated and clinically important serovars, representing 80 to 90% of Salmonella isolates collected in Canada (4, 9). Further modifications to include additional antisera and isolates are planned for validation of the system side by side with the traditional Kauffmann-White method in order to implement the method in diagnostic laboratories. The protein microarray assay developed in this research is a more rapid and potentially cost-effective alternative to the current slide agglutination method for Salmonella serotyping. This platform could probably be extended to perform detection and serotyping of other bacteria.
Acknowledgments
This research was supported by the OMAF (Ontario Ministry of Agriculture and Food) Food Safety Research Program.
We are grateful to Linda Cole and Betty Wilkie, Public Health Agency of Canada, for their technical expertise and advice in Salmonella serotyping and to Andrew Moor, Laboratory Services, University of Guelph, for his help with EM examination.
REFERENCES
- 1.Agron, P. G., R. L. Walker, H. Kinde, S. J. Sawyer, D. C. Hayes, J. Wollard, and G. L. Andersen. 2001. Identification by subtractive hybridization of sequences specific for Salmonella enterica serovar enteritidis. Appl. Environ. Microbiol. 67:4984-4991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Birla, L., A. M. Cristian, and M. Hillebrand. 2004. Absorption and steady state fluorescence study of interaction between eosin and bovine serum albumin. Spectrochim. Acta A Mol. Biomol. Spectrosc. 60:551-556. [DOI] [PubMed] [Google Scholar]
- 3.Delehanty, J. B., and F. S. Ligler. 2002. A microarray immunoassay for simultaneous detection of proteins and bacteria. Anal. Chem. 74:5681-5687. [DOI] [PubMed] [Google Scholar]
- 4.Demczuk, W., R. Ahmed, D. Woodward, C. Clark, and F. Rodgers. 2001. National Enteric Surveillance Program 2000 annual summary. Minister of Public Works and Government Services, Guelph, Canada.
- 5.Falsey, J. R., M. Renil, S. Park, S. Li, and K. S. Lam. 2001. Peptide and small molecule microarray for high throughput cell adhesion and functional assays. Bioconjug. Chem. 12:346-353. [DOI] [PubMed] [Google Scholar]
- 6.Fierer, J., and D. G. Guiney. 2001. Diverse virulence traits underlying different clinical outcomes of Salmonella infection. J. Clin. Invest. 107:775-780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herrera-Leon, S., J. R. McQuiston, M. A. Usera, P. I. Fields, J. Garaizar, and M. A. Echeita. 2004. Multiplex PCR for distinguishing the most common phase-1 flagellar antigens of Salmonella spp. J. Clin. Microbiol. 42:2581-2586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McQuiston, J. R., R. Parrenas, M. Ortiz-Rivera, L. Gheesling, F. Brenner, and P. I. Fields. 2004. Sequencing and comparative analysis of flagellin genes fliC, fljB, and flpA from Salmonella. J. Clin. Microbiol. 42:1923-1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muckle, A., L. Cole, and C. Poppe. 2001. Salmonella serovars and Salmonella phagetypes identified by the O.I.É. Reference Laboratory for Salmonellosis at the Health Canada Laboratory for Foodborne Zoonoses. Year 2001 Annual Report. Unpublished data.
- 10.Novelli, A. 1969. The use of fluorescence microscopy for histopathologic preparations stained by hematoxylin eosin. Pathologica 61:5-16. [PubMed] [Google Scholar]
- 11.Popoff, M. Y. 2001. Antigenic formulas of the Salmonella serovars, 8th ed. W.H.O. Collaborating Centre for Reference and Research on Salmonella. World Health Organization, Geneva, Switzerland.
- 12.Popoff, M. Y., J. Bockemuhl, and L. L. Gheesling. 2003. Supplement 2001 (no. 45) to the Kauffmann-White scheme. Res. Microbiol. 154:173-174. [DOI] [PubMed] [Google Scholar]