Abstract
Aim
The Japanese National Clinical Database, which covers more than 95% of the surgeries performed in Japan, is the largest nationwide database. This is the 2021 annual report of the Gastroenterological Section of the National Clinical Database, which aims to present the short‐term outcomes of cases registered in 2021 and discuss significant changes and insights into gastroenterological surgeries observed over the decade.
Methods
We reviewed the data of patients registered in the National Clinical Database between 2012 and 2021.
Results
In total, 5 788 093 cases, including 597 780 cases in 2021, were extracted from the National Clinical Database. The number of surgeries resumed its original trend after a uniform decrease due to the coronavirus disease 2019 pandemic. The patient population continues to age, and the proportion of female patients is steadily increasing. The trend of surgeries being conducted in certified institutions with the involvement of board‐certified surgeons is consistently rising. Moreover, the increasing trend of endoscopic surgery rate is still maintained. Although operative mortality is declining, the trend of increasing postoperative complications continues. Surgery on the esophagus, liver, and pancreas has shown substantial improvements in operative mortality, with a high participation rate of board‐certified surgeons. Surgical procedures with a high incidence of emergency surgeries are characterized by low participation rates of board‐certified surgeons, increased morbidity rates, and worse mortality outcomes.
Conclusion
This overview of surgical patients in Japan, obtained using data extracted from the National Clinical Database, may serve as a critical cornerstone for the future development of gastroenterological surgery.
Keywords: annual report, emergency surgery, gastroenterological surgery, National Clinical Database, surgical outcome
This study presents the annual report of the gastroenterological surgery of the National Clinical Database (NCD) in 2021. In total, 5 788 093 cases, including 597 780 cases in 2021, were extracted from the NCD. The patient population continues to age, and the proportion of female patients is steadily increasing. The trend of surgeries being conducted in certified institutions with the involvement of board‐certified surgeons is consistently rising.
1. INTRODUCTION
The Japanese National Clinical Database (NCD) is the largest nationwide database, which covers more than 95% of the surgeries performed in Japan. 1 , 2 Data registration with the NCD commenced in 2011 and now includes 1.5 million cases annually from more than 5600 facilities, reaching a cumulative total of 17 million cases. 3
The Japanese Society of Gastroenterological Surgery (JSGS) is among the 10 societies involved in the establishment of the NCD and conducts numerous systems and analyses using data in the registry to benefit patients, surgeons, and enrolled facilities. First, the registered cases are used for the board certification system; 121 gastroenterological procedures are classified into three levels of difficulty, forming the basis of board certification applications. Second, nine major surgical procedures were benchmarked to improve the quality of surgical care 4 ; namely, esophagectomy, partial/total gastrectomy, right hemicolectomy, low anterior resection, hepatectomy, pancreaticoduodenectomy, surgery for acute diffuse peritonitis, and liver transplantation. Risk models for mortality 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 and morbidity 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 associated with these nine major procedures have been reported as some of the most significant findings derived from NCD. Third, feedback systems based on risk models were constructed and operated online. 4 For individual patients, a risk calculator can be used to estimate surgical risks based on preoperative clinical information. Furthermore, the NCD can provide surgical outcomes for the enrolled facilities in comparison with national real‐world data. The former can be used to obtain informed consent, whereas the latter can support risk management and performance improvements in facilities.
As mentioned above, the NCD have evolved into an indispensable framework for the advancement of gastroenterological surgery in Japan. The purpose of this report is to understand the current trends and challenges of gastroenterological surgeries and to clarify the path for future advancements, by overviewing gastroenterological surgeries registered in the NCD. Hence, we continue with previous annual reports 22 , 23 , 24 , 25 , 26 by presenting the short‐term outcomes of cases registered in the NCD in 2021 and discuss significant changes and insights into gastroenterological surgeries observed over the decade from 2012 to 2021.
2. PATIENTS AND METHODS
The included patients were those who underwent one or more of the 121 surgical procedures stipulated in the “Training Curriculum for Board‐Certified Surgeons in Gastroenterology,” and had their surgical data recorded from 2012 to 2021 in the NCD system. The clinical data of these patients were collected using the NCD system, as previously reported. 4 , 22 , 23 , 24 , 25 , 26 The number of surgeries, patient sex, age, postoperative complications, mortalities, and proportions of endoscopic and emergency surgeries for each surgical procedure were calculated. The proportion of institutions certified by the JSGS and the participation rates of anesthesiologists and board‐certified surgeons were calculated. Using these data, four main analyses were conducted: analysis of (1) each surgical procedure; (2) annual trends in surgeries by organ; (3) annual trends of endoscopic surgery rate in major surgical procedures; and (4) surgical procedures with high rates of emergency surgery.
Major requirements for board‐certified training institutions include 600 or more gastroenterological operations, as mandated by the accreditation committee, with at least 120 being essential major surgeries done over the preceding 3 years. Board‐certified surgeons are required to undergo training for over 5 years and have experience in performing more than 450 surgical cases at the aforementioned board‐certified training institutions.
When interpreting the data provided, it is necessary to consider the following factors: (a) due to the NCD's limitation of recording a maximum of eight operative procedures per case, the aggregate number of surgeries reported for each result does not accurately represent the total number of surgical cases; (b) data entries with inaccuracies in patient age, sex, and postoperative 30‐day status were omitted from the analysis; (c) postoperative complications that were grade III or more in the Clavien–Dindo (C‐D) classification were defined as severe complications 27 ; (d) the measure of postoperative 30‐day mortality encompasses all instances of death within 30 days following the surgery, irrespective of whether the patient was discharged or not, whereas operative mortality accounts for all deaths occurring during the index hospitalization, which may extend up to 90 days, as well as any deaths occurring after discharge within 30 days from the date of surgery.
3. RESULTS
3.1. Gastroenterological operative procedures in the “Training Curriculum for Board‐Certified Surgeons in Gastroenterology” in 2021
From January 1, 2021, to December 31, 2021, 597 780 patients underwent gastroenterological surgeries, as recorded in the NCD. In the analyses regarding the treated organ, the breakdown of the cases were as follows: esophagus, 8905 cases (1.5%); stomach and duodenum, 56 759 cases (9.5%); small intestine and colon, 240 448 cases (40.2%); rectum and anus, 56 536 cases (9.5%); liver, 26 250 cases (4.4%); gallbladder, 136 111 cases (22.8%); pancreas, 19 722 cases (3.3%); spleen, 1833 cases (0.3%); and others, 51 216 cases (8.5%).
Characteristics of the operative procedures outlined in the “Training Curriculum for Board‐Certified Surgeons in Gastroenterology” for 2021 are detailed in Table 1. Although anesthesiologists participated in most surgical procedures, with a rate exceeding 95%, there were notable exceptions. These included anal surgeries, such as anal sphincteroplasty (23.3%), transanal rectal tumor resection (39.1%), proctocele surgery (55.9%), esophageal and gastric varix surgery (62.0%), external cholecystostomy (63.3%), external pancreatic duct drainage (73.7%), and surgery for hepatic trauma (excluding drainage only) (75.1%), which had participation rates below 80%. Although the participation rates of board‐certified surgeons vary, they generally exceed 90% in highly difficult procedures for each organ. However, even among the surgeries performed in more than 100 cases annually, procedures such as anal sphincteroplasty (53.7%), transanal rectal tumor resection (56.9%), achalasia surgery (53.4%), gastric pyloroplasty (57.5%), and surgery for hepatic trauma (excluding drainage only) (58.6%) had less than 60% participation by board‐certified surgeons.
TABLE 1.
Characteristics of each operative procedure of the “Training Curriculum for Board‐Certified Surgeons in Gastroenterology” in 2021.
| Organ | Difficulty level | Operative procedure | No. of surgeries | Sex male (%) | Age ≥80 (%) | Anesthesiologist participation (%) | Board‐certified surgeon participation (%) | Operating surgeon (%) | |
|---|---|---|---|---|---|---|---|---|---|
| Board‐certified surgeon | Non‐board‐certified surgeon | ||||||||
| Esophagus | Low | Cervical periesophageal abscess drainage | 32 | 68.8 | 9.4 | 87.5 | 96.9 | 71.9 | 28.1 |
| Med | Esophageal suture (perforation, injury) | 183 | 77.6 | 15.8 | 95.1 | 86.9 | 57.9 | 42.1 | |
| Med | Thoracic periesophageal abscess drainage | 23 | 78.3 | 13.0 | 100.0 | 100.0 | 73.9 | 26.1 | |
| Med | Esophageal foreign body extraction | 27 | 40.7 | 44.4 | 96.3 | 85.2 | 55.6 | 44.4 | |
| Med | Esophageal diverticulum resection | 41 | 63.4 | 9.8 | 95.1 | 95.1 | 78.0 | 22.0 | |
| Med | Benign esophageal tumor removal | 70 | 61.4 | 0.0 | 98.6 | 97.1 | 74.3 | 25.7 | |
| Med | Esophageal resection (removal only) | 606 | 81.2 | 15.3 | 97.4 | 91.4 | 75.6 | 24.4 | |
| Med | Esophageal reconstruction (gastric tube reconstruction) | 516 | 82.2 | 7.2 | 99.0 | 95.5 | 78.5 | 21.5 | |
| Med | Esophageal fistula construction | 186 | 77.4 | 12.9 | 96.8 | 96.2 | 83.9 | 16.1 | |
| Med | Esophagocardioplasty | 305 | 38.7 | 25.9 | 97.4 | 82.3 | 56.1 | 43.9 | |
| Med | Achalasia surgery | 189 | 52.9 | 7.9 | 96.3 | 53.4 | 38.1 | 61.9 | |
| High | Esophagectomy | 6193 | 80.3 | 8.4 | 99.2 | 98.6 | 83.5 | 16.5 | |
| High | Esophageal reconstruction (colon reconstruction) | 36 | 88.9 | 5.6 | 100.0 | 91.7 | 63.9 | 36.1 | |
| High | Esophageal bypass | 117 | 80.3 | 7.7 | 98.3 | 100.0 | 66.7 | 33.3 | |
| High | Bronchoesophageal fistula surgery | 7 | 57.1 | 0.0 | 85.7 | 100.0 | 100.0 | 0.0 | |
| High | Secondary esophageal reconstruction | 374 | 81.6 | 11.8 | 98.9 | 96.8 | 72.5 | 27.5 | |
| Stomach and duodenum | Low | Gastrostomy and suture gastrorrhaphy | 64 | 60.9 | 21.9 | 96.9 | 82.8 | 40.6 | 59.4 |
| Low | Diverticulectomy, polypectomy (excluding endoscopic resection) | 128 | 53.9 | 19.5 | 96.1 | 92.2 | 50.0 | 50.0 | |
| Low | Truncal vagotomy | 0 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Low | Gastroenterostomy (including duodenal jejunostomy) | 5944 | 62.8 | 28.8 | 97.0 | 86.4 | 41.9 | 58.1 | |
| Low | Gastric fistula construction (excluding PEG) | 1460 | 63.9 | 28.0 | 93.1 | 79.9 | 45.5 | 54.5 | |
| Low | Gastric pyloroplasty | 106 | 79.2 | 3.8 | 96.2 | 57.5 | 28.3 | 71.7 | |
| Low | Gastric volvulus surgery and rectopexy | 64 | 20.3 | 48.4 | 95.3 | 84.4 | 46.9 | 53.1 | |
| Low | Gastric suture (including gastric suture for gastric rupture, suture closure for gastroduodenal perforation, omental implantation and omental transposition) | 5327 | 65.1 | 25.6 | 93.6 | 75.1 | 30.0 | 70.0 | |
| Low | Local gastrectomy (including wedge resection) | 4878 | 50.7 | 14.6 | 96.6 | 89.2 | 49.8 | 50.2 | |
| Med | Gastrectomy (including distal, pylorus preserving, and segmental) | 28 771 | 66.6 | 26.7 | 96.4 | 90.7 | 55.9 | 44.1 | |
| Med | Selective vagotomy | 3 | 66.7 | 0.0 | 100.0 | 66.7 | 33.3 | 66.7 | |
| High | Total gastrectomy (including proximal gastrectomy) | 10 010 | 73.8 | 22.6 | 96.5 | 89.4 | 55.6 | 44.4 | |
| High | Left upper abdominal exenteration | 4 | 100.0 | 0.0 | 100.0 | 100.0 | 75.0 | 25.0 | |
| Small intestine and colon | Low | Enterotomy and enterorrhaphy | 4268 | 55.5 | 26.5 | 93.7 | 78.9 | 40.4 | 59.6 |
| Low | Disinvagination (invasive) | 152 | 45.4 | 29.6 | 96.7 | 76.3 | 21.7 | 78.3 | |
| Low | Partial small bowel resection (benign) | 9017 | 57.5 | 30.9 | 95.0 | 78.9 | 36.6 | 63.4 | |
| Low | Ileocecal resection (benign) | 4970 | 58.6 | 18.4 | 94.6 | 79.0 | 34.4 | 65.6 | |
| Low | Partial colectomy and sigmoid colectomy (benign) | 8536 | 62.2 | 25.9 | 95.0 | 80.8 | 37.3 | 62.7 | |
| Low | Appendectomy | 56 071 | 55.1 | 6.6 | 93.1 | 68.3 | 24.3 | 75.7 | |
| Low | Enterostomy and closure (without enterectomy) | 28 205 | 62.8 | 20.4 | 96.0 | 83.3 | 45.0 | 55.0 | |
| Med | Small bowel resection (malignant) | 3620 | 56.8 | 20.4 | 97.1 | 85.2 | 42.1 | 57.9 | |
| Med | Ileocecal resection (malignant) | 15 488 | 46.2 | 33.6 | 96.1 | 86.0 | 37.3 | 62.7 | |
| Med | Partial colectomy and sigmoid colectomy (malignant) | 30 536 | 57.2 | 24.9 | 96.3 | 87.1 | 46.8 | 53.2 | |
| Med | Right hemicolectomy | 22 027 | 51.0 | 33.9 | 95.8 | 85.3 | 44.1 | 55.9 | |
| Med | Left hemicolectomy | 6018 | 57.6 | 24.9 | 95.9 | 85.9 | 49.2 | 50.8 | |
| Med | Total colectomy | 1546 | 58.2 | 21.8 | 96.2 | 84.0 | 49.9 | 50.1 | |
| Med | Intestinal obstruction surgery (with enterectomy) | 26 275 | 49.2 | 37.9 | 94.4 | 76.6 | 33.8 | 66.2 | |
| Med | Enterostomy and closure (with enterectomy) | 23 231 | 62.9 | 18.5 | 95.9 | 82.7 | 42.2 | 57.8 | |
| High | Proctocolectomy and ileoanal (canal) anastomosis | 440 | 61.8 | 1.4 | 99.3 | 95.7 | 77.0 | 23.0 | |
| Rectum | Low | Transanal rectal tumor resection | 3527 | 49.6 | 12.6 | 39.1 | 56.9 | 36.1 | 63.9 |
| Low | Proctocele surgery (transanal) | 2396 | 14.2 | 66.0 | 55.9 | 63.1 | 37.9 | 62.1 | |
| Med | Abdominoperineal resection (benign) | 1056 | 59.8 | 21.2 | 93.7 | 82.1 | 48.3 | 51.7 | |
| Med | High anterior resection | 11 841 | 58.1 | 18.3 | 96.7 | 89.1 | 54.3 | 45.7 | |
| Med | Hartmann's procedure | 6408 | 55.9 | 38.5 | 96.3 | 83.1 | 39.4 | 60.6 | |
| Med | Proctocele surgery (abdominoperineal) | 2198 | 10.7 | 58.9 | 91.9 | 83.9 | 51.5 | 48.5 | |
| Med | Malignant anorectal tumor excision (transanal) | 706 | 52.5 | 30.3 | 80.0 | 79.7 | 56.1 | 43.9 | |
| Med | Anal sphincteroplasty (by tissue replacement) | 2603 | 54.9 | 11.6 | 23.3 | 53.7 | 37.2 | 62.8 | |
| High | Abdominoperineal resection (malignant) | 4909 | 63.5 | 21.3 | 96.7 | 91.2 | 66.1 | 33.9 | |
| High | Low anterior resection | 20 403 | 62.8 | 14.1 | 96.3 | 90.7 | 65.9 | 34.1 | |
| High | Total pelvic exenteration | 454 | 71.8 | 4.8 | 98.5 | 92.7 | 73.6 | 26.4 | |
| High | Anorectal malignant tumor excision (posterior approach) | 35 | 54.3 | 20.0 | 80.0 | 88.6 | 48.6 | 51.4 | |
| Liver | Low | Hepatorrhaphy | 63 | 55.6 | 27.0 | 87.3 | 69.8 | 27.0 | 73.0 |
| Low | Liver abscess drainage (excluding percutaneous procedures) | 40 | 67.5 | 27.5 | 85.0 | 95.0 | 45.0 | 55.0 | |
| Low | Hepatic cyst resection, suture, drainage | 966 | 24.0 | 18.5 | 97.0 | 88.5 | 43.7 | 56.3 | |
| Low | Liver biopsy (excluding percutaneous procedures) | 351 | 49.0 | 2.6 | 91.2 | 88.0 | 39.0 | 61.0 | |
| Low | Liver coagulo‐necrotic therapy (excluding percutaneous procedures) | 439 | 72.9 | 19.1 | 98.4 | 92.9 | 66.3 | 33.7 | |
| Med | Partial hepatectomy | 12 492 | 66.7 | 15.7 | 98.0 | 95.7 | 69.5 | 30.5 | |
| Med | Lateral segmentectomy | 1382 | 65.9 | 20.3 | 97.7 | 94.9 | 64.5 | 35.5 | |
| Med | Esophageal and gastric varix surgery | 50 | 62.0 | 10.0 | 62.0 | 40.0 | 32.0 | 68.0 | |
| High | Surgery for hepatic trauma (excluding drainage only) | 394 | 67.3 | 19.3 | 75.1 | 58.6 | 27.4 | 72.6 | |
| High | Hepatectomy (segmentectomy or more; excluding lateral segmentectomy) | 6491 | 67.8 | 15.4 | 98.2 | 97.6 | 80.2 | 19.8 | |
| High | Subsegmentectomy | 2656 | 70.8 | 16.8 | 97.3 | 97.0 | 79.0 | 21.0 | |
| High | Liver transplantation | 791 | 51.2 | 0.3 | 99.1 | 98.9 | 77.2 | 22.8 | |
| High | Hepatopancreatoduodenectomy | 135 | 67.4 | 5.2 | 96.3 | 99.3 | 88.9 | 11.1 | |
| Gall bladder | Low | Cholangiotomy | 63 | 57.1 | 33.3 | 98.4 | 90.5 | 47.6 | 52.4 |
| Low | Cholecystolithotomy | 64 | 62.5 | 37.5 | 92.2 | 84.4 | 45.3 | 54.7 | |
| Low | Cholecystectomy | 129 693 | 55.0 | 17.7 | 95.0 | 80.0 | 34.9 | 65.1 | |
| Low | External cholecystostomy | 139 | 60.4 | 47.5 | 63.3 | 65.5 | 36.0 | 64.0 | |
| Low | Cystoenteric anastomosis | 36 | 52.8 | 52.8 | 97.2 | 86.1 | 55.6 | 44.4 | |
| Med | Choledocholithotomy | 2015 | 60.4 | 38.5 | 94.1 | 85.5 | 48.2 | 51.8 | |
| Med | Biliary tract reconstruction | 295 | 57.6 | 20.3 | 96.9 | 96.3 | 70.2 | 29.8 | |
| Med | Biliary bypass | 967 | 125.9 | 26.8 | 97.2 | 94.1 | 57.5 | 42.5 | |
| Med | Cholangioplasty | 96 | #REF! | 21.9 | 92.7 | 91.7 | 63.5 | 36.5 | |
| Med | Duodenal papilloplasty | 29 | 58.6 | 27.6 | 82.8 | 93.1 | 72.4 | 27.6 | |
| Med | Choledocal dilatation | 278 | 25.9 | 2.2 | 97.8 | 91.0 | 66.2 | 33.8 | |
| Med | Biliary fistula closure | 16 | 50.0 | 43.8 | 93.8 | 87.5 | 31.3 | 68.8 | |
| High | Surgery for bile duct trauma (excluding drainage only) | 235 | 58.7 | 25.5 | 95.7 | 90.2 | 53.6 | 46.4 | |
| High | Malignant gallbladder tumor surgery (excluding simple cholecystectomy) | 1039 | 51.9 | 23.1 | 98.5 | 94.9 | 61.2 | 38.8 | |
| High | Malignant bile duct tumor surgery | 1108 | 69.4 | 23.1 | 96.9 | 97.3 | 81.3 | 18.7 | |
| High | Biliary atresia surgery | 38 | 39.5 | 0.0 | 100.0 | 50.0 | 21.1 | 78.9 | |
| Pancreas | Low | External pancreatic cyst drainage | 4 | 100.0 | 0.0 | 100.0 | 25.0 | 25.0 | 75.0 |
| Low | External pancreatic duct drainage | 19 | 73.7 | 10.5 | 73.7 | 78.9 | 73.7 | 26.3 | |
| Med | Pancreatorrhaphy | 4 | 100.0 | 25.0 | 100.0 | 75.0 | 75.0 | 25.0 | |
| Med | Partial pancreatic resection | 145 | 46.9 | 5.5 | 98.6 | 95.2 | 77.2 | 22.8 | |
| Med | Distal pancreatectomy (benign) | 1422 | 46.8 | 9.1 | 97.3 | 94.4 | 74.0 | 26.0 | |
| Med | Pancreatic cyst‐enterostomy | 20 | 70.0 | 15.0 | 95.0 | 85.0 | 55.0 | 45.0 | |
| Med | Pancreatic (duct) enterostomy | 280 | 70.4 | 8.2 | 94.6 | 97.5 | 69.3 | 30.7 | |
| Med | Acute pancreatitis surgery | 50 | 64.0 | 8.0 | 94.0 | 80.0 | 54.0 | 46.0 | |
| Med | Pancreatolithiasis surgery | 14 | 78.6 | 7.1 | 100.0 | 85.7 | 71.4 | 28.6 | |
| Med | Plexus pancreaticus capitalis resection | 0 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| High | Surgery for pancreatic trauma (excluding drainage only) | 59 | 69.5 | 13.6 | 93.2 | 74.6 | 50.8 | 49.2 | |
| High | Pancreaticoduodenectomy | 11 764 | 60.2 | 16.7 | 98.1 | 97.4 | 75.5 | 24.5 | |
| High | Distal pancreatectomy (malignant) | 5091 | 55.6 | 17.8 | 97.8 | 96.5 | 75.3 | 24.7 | |
| High | Total pancreatectomy | 635 | 54.3 | 12.1 | 98.7 | 98.7 | 81.3 | 18.7 | |
| High | Duodenum preserving pancreas head resection | 38 | 47.4 | 5.3 | 97.4 | 89.5 | 60.5 | 39.5 | |
| High | Segmental pancreatic resection | 153 | 50.3 | 5.2 | 98.7 | 99.3 | 76.5 | 23.5 | |
| High | Pancreas transplantation | 23 | 60.9 | 0.0 | 100.0 | 100.0 | 95.7 | 4.3 | |
| Spleen | Low | Splenorrhaphy | 24 | 62.5 | 16.7 | 91.7 | 66.7 | 25.0 | 75.0 |
| Med | Splenectomy | 1789 | 55.9 | 12.7 | 96.4 | 91.2 | 61.3 | 38.7 | |
| Med | Partial splenectomy | 20 | 45.0 | 10.0 | 95.0 | 45.0 | 20.0 | 80.0 | |
| Other | Low | Localized intra‐abdominal abscess surgery | 2243 | 60.5 | 17.9 | 92.0 | 75.8 | 34.5 | 65.5 |
| Low | Exploratory laparotomy | 13 325 | 60.6 | 18.6 | 94.8 | 82.5 | 42.8 | 57.2 | |
| Med | Acute diffuse peritonitis surgery | 15 776 | 58.8 | 28.0 | 95.1 | 80.3 | 34.4 | 65.6 | |
| Med | Ventral hernia surgery | 14 399 | 46.5 | 21.1 | 94.4 | 74.4 | 37.4 | 62.6 | |
| Med | Diaphragm suture | 285 | 56.5 | 22.1 | 96.8 | 83.2 | 51.6 | 48.4 | |
| Med | Esophageal hiatus hernia surgery | 1231 | 31.0 | 41.0 | 96.2 | 89.7 | 61.7 | 38.3 | |
| Med | Retroperitoneal tumor surgery | 1425 | 49.0 | 9.9 | 97.4 | 88.8 | 60.3 | 39.7 | |
| Med | Abdominal wall/mesenteric/omental tumor resection | 2085 | 50.3 | 10.2 | 96.5 | 82.4 | 46.8 | 53.2 | |
| Med | Gastrointestinal perforation closure | 391 | 65.7 | 26.3 | 92.8 | 80.3 | 38.1 | 61.9 | |
| High | Diaphragmatic hiatus hernia surgery | 56 | 57.1 | 23.2 | 96.4 | 92.9 | 55.4 | 44.6 | |
The short‐term outcomes of the operative procedures outlined in the “Training Curriculum for Board‐Certified Surgeons in Gastroenterology” in 2021 are presented in Table 2. Among the procedures performed in more than 100 cases annually, those with high surgical mortality rates (>10%) included surgery for hepatic trauma (excluding drainage only) (26.6%), closure of gastrointestinal perforations (16.2%), surgery for acute diffuse peritonitis (11.5%), esophageal bypass (11.1%), esophageal fistula construction (10.8%), and external cholecystostomy (10.1%). These procedures predominantly involved emergency surgeries, and a high proportion of patients experienced palliative or symptomatic relief.
TABLE 2.
Number of surgeries and short‐term outcome of each operative procedure of the “Training Curriculum for Board‐Certified Surgeons in Gastroenterology” in 2021.
| Organ | Difficulty level | Operative procedure | No. of surgeries | Endoscopic surgeries (%) | Emergency surgeries (%) | Postoperative complications (%) a | Re‐operations (%) | Postoperative 30‐day mortalities (%) | Operative mortalities (%) b |
|---|---|---|---|---|---|---|---|---|---|
| Esophagus | Low | Cervical periesophageal abscess drainage | 32 | 21.9 | 59.4 | 28.1 | 9.4 | 3.1 | 3.1 |
| Med | Esophageal suture (perforation, injury) | 183 | 19.1 | 74.9 | 36.6 | 13.7 | 3.3 | 4.9 | |
| Med | Thoracic periesophageal abscess drainage | 23 | 17.4 | 91.3 | 21.7 | 30.4 | 4.3 | 8.7 | |
| Med | Esophageal foreign body extraction | 27 | 22.2 | 88.9 | 22.2 | 0.0 | 0.0 | 3.7 | |
| Med | Esophageal diverticulum resection | 41 | 34.1 | 0.0 | 12.2 | 4.9 | 0.0 | 0.0 | |
| Med | Benign esophageal tumor removal | 70 | 81.4 | 0.0 | 0.0 | 2.9 | 0.0 | 0.0 | |
| Med | Esophageal resection (removal only) | 606 | 63.5 | 8.7 | 20.1 | 16.5 | 1.5 | 3.8 | |
| Med | Esophageal reconstruction (gastric tube reconstruction) | 516 | 71.7 | 1.2 | 21.5 | 5.0 | 1.0 | 3.1 | |
| Med | Esophageal fistula construction | 186 | 49.5 | 26.9 | 39.8 | 31.2 | 2.2 | 10.8 | |
| Med | Esophagocardioplasty | 305 | 76.7 | 2.6 | 4.6 | 2.0 | 1.0 | 1.0 | |
| Med | Achalasia surgery | 189 | 91.5 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| High | Esophagectomy | 6193 | 74.8 | 0.9 | 23.0 | 5.7 | 0.7 | 1.4 | |
| High | Esophageal reconstruction (colon reconstruction) | 36 | 55.6 | 0.0 | 25.0 | 16.7 | 2.8 | 2.8 | |
| High | Esophageal bypass | 117 | 12.0 | 2.6 | 32.5 | 9.4 | 6.0 | 11.1 | |
| High | Bronchoesophageal fistula surgery | 7 | 14.3 | 14.3 | 57.1 | 14.3 | 0.0 | 0.0 | |
| High | Secondary esophageal reconstruction | 374 | 15.2 | 2.1 | 32.9 | 10.4 | 0.8 | 2.4 | |
| Stomach and duodenum | Low | Gastrostomy and suture gastrorrhaphy | 64 | 14.1 | 62.5 | 10.9 | 3.1 | 0.0 | 0.0 |
| Low | Diverticulectomy, polypectomy (excluding endoscopic resection) | 128 | 16.4 | 23.4 | 13.3 | 5.5 | 1.6 | 2.3 | |
| Low | Truncal vagotomy | 0 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Low | Gastroenterostomy (including duodenal jejunostomy) | 5944 | 33.6 | 9.7 | 15.1 | 5.2 | 5.0 | 8.5 | |
| Low | Gastric fistula construction (excluding PEG) | 1460 | 15.4 | 16.5 | 20.5 | 4.7 | 6.3 | 9.8 | |
| Low | Gastric pyloroplasty | 106 | 17.0 | 43.4 | 4.7 | 5.7 | 0.9 | 0.9 | |
| Low | Gastric volvulus surgery and rectopexy | 64 | 71.9 | 20.3 | 14.1 | 4.7 | 1.6 | 1.6 | |
| Low | Gastric suture (including gastric suture for gastric rupture, suture closure for gastroduodenal perforation, omental implantation and omental transposition) | 5327 | 38.6 | 91.5 | 17.7 | 5.7 | 5.7 | 7.5 | |
| Low | Local gastrectomy (including wedge resection) | 4878 | 71.3 | 3.1 | 3.1 | 1.4 | 0.3 | 0.5 | |
| Med | Gastrectomy (including distal, pylorus preserving and segmental) | 28 771 | 56.3 | 1.8 | 7.5 | 2.5 | 0.7 | 1.1 | |
| Med | Selective vagotomy | 3 | 66.7 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| High | Total gastrectomy (including proximal gastrectomy) | 10 010 | 33.8 | 1.9 | 12.5 | 3.9 | 1.3 | 2.2 | |
| High | Left upper abdominal exenteration | 4 | 0.0 | 0.0 | 75.0 | 25.0 | 0.0 | 0.0 | |
| Small intestine and colon | Low | Enterotomy and enterorrhaphy | 4268 | 18.6 | 29.7 | 17.0 | 7.7 | 4.5 | 7.5 |
| Low | Disinvagination (invasive) | 152 | 29.6 | 80.3 | 5.3 | 2.0 | 2.6 | 3.3 | |
| Low | Partial small bowel resection (benign) | 9017 | 21.1 | 62.5 | 20.4 | 10.4 | 6.7 | 9.1 | |
| Low | Ileocecal resection (benign) | 4970 | 44.7 | 49.1 | 10.3 | 4.1 | 2.2 | 3.0 | |
| Low | Partial colectomy and sigmoid colectomy (benign) | 8536 | 35.6 | 45.3 | 15.5 | 6.3 | 4.1 | 5.6 | |
| Low | Appendectomy | 56 071 | 73.9 | 67.6 | 1.8 | 1.0 | 0.1 | 0.2 | |
| Low | Enterostomy and closure (without enterectomy) | 28 205 | 40.7 | 28.4 | 16.0 | 7.6 | 3.5 | 5.7 | |
| Med | Small bowel resection (malignant) | 3620 | 32.2 | 17.4 | 12.1 | 4.8 | 2.8 | 4.2 | |
| Med | Ileocecal resection (malignant) | 15 488 | 65.2 | 5.7 | 4.9 | 2.2 | 0.6 | 0.9 | |
| Med | Partial colectomy and sigmoid colectomy (malignant) | 30 536 | 64.8 | 3.6 | 6.3 | 3.6 | 0.5 | 0.9 | |
| Med | Right hemicolectomy | 22 027 | 56.9 | 8.2 | 7.4 | 3.4 | 1.4 | 2.1 | |
| Med | Left hemicolectomy | 6018 | 56.1 | 9.2 | 10.1 | 4.8 | 2.0 | 2.9 | |
| Med | Total colectomy | 1546 | 33.1 | 33.4 | 23.9 | 9.5 | 7.9 | 9.8 | |
| Med | Intestinal obstruction surgery (with enterectomy) | 26 275 | 25.7 | 68.3 | 10.2 | 4.4 | 2.4 | 3.4 | |
| Med | Enterostomy and closure (with enterectomy) | 23 231 | 19.4 | 21.2 | 13.6 | 5.3 | 3.2 | 4.5 | |
| High | Proctocolectomy and ileoanal (canal) anastomosis | 440 | 52.7 | 7.7 | 10.5 | 4.3 | 0.9 | 1.1 | |
| Rectum | Low | Transanal rectal tumor resection | 3527 | 2.4 | 1.4 | 0.7 | 0.8 | 0.1 | 0.1 |
| Low | Proctocele surgery (transanal) | 2396 | 0.8 | 1.3 | 1.9 | 2.5 | 0.2 | 0.2 | |
| Med | Abdominoperineal resection (benign) | 1056 | 13.1 | 19.3 | 18.4 | 6.6 | 2.5 | 3.8 | |
| Med | High anterior resection | 11 841 | 74.9 | 3.4 | 5.6 | 3.5 | 0.4 | 0.6 | |
| Med | Hartmann's procedure | 6408 | 23.3 | 58.6 | 20.8 | 6.0 | 5.6 | 7.5 | |
| Med | Proctocele surgery (abdominoperineal) | 2198 | 58.6 | 0.7 | 2.2 | 1.6 | 0.2 | 0.4 | |
| Med | Malignant anorectal tumor excision (transanal) | 706 | 19.5 | 7.4 | 7.2 | 3.8 | 1.0 | 1.4 | |
| Med | Anal sphincteroplasty (by tissue replacement) | 2603 | 1.8 | 2.2 | 0.8 | 1.2 | 0.0 | 0.1 | |
| High | Abdominoperineal resection (malignant) | 4909 | 73.9 | 0.8 | 12.3 | 4.7 | 0.6 | 0.8 | |
| High | Low anterior resection | 20 403 | 75.3 | 1.3 | 10.4 | 6.1 | 0.5 | 0.6 | |
| High | Total pelvic exenteration | 454 | 33.0 | 1.5 | 32.4 | 8.8 | 0.9 | 1.8 | |
| High | Anorectal malignant tumor excision (posterior approach) | 35 | 14.3 | 0.0 | 11.4 | 5.7 | 0.0 | 0.0 | |
| Liver | Low | Hepatorrhaphy | 63 | 11.1 | 85.7 | 34.9 | 23.8 | 11.1 | 12.7 |
| Low | Liver abscess drainage (excluding percutaneous procedures) | 40 | 32.5 | 42.5 | 20.0 | 2.5 | 5.0 | 5.0 | |
| Low | Hepatic cyst resection, suture, drainage | 966 | 79.3 | 5.5 | 2.8 | 1.2 | 0.2 | 0.2 | |
| Low | Liver biopsy (excluding percutaneous procedures) | 351 | 13.7 | 26.2 | 4.0 | 7.4 | 0.6 | 1.4 | |
| Low | Liver coagulo‐necrotic therapy (excluding percutaneous procedures) | 439 | 33.5 | 0.5 | 3.4 | 2.1 | 0.2 | 0.9 | |
| Med | Partial hepatectomy | 12 492 | 43.9 | 0.7 | 6.4 | 1.9 | 0.4 | 0.5 | |
| Med | Lateral segmentectomy | 1382 | 41.6 | 1.5 | 5.2 | 2.1 | 0.4 | 0.7 | |
| Med | Esophageal and gastric varix surgery | 50 | 48.0 | 20.0 | 6.0 | 14.0 | 2.0 | 2.0 | |
| High | Surgery for hepatic trauma (excluding drainage only) | 394 | 5.3 | 82.0 | 48.5 | 49.0 | 22.8 | 26.6 | |
| High | Hepatectomy (segmentectomy or more; excluding lateral segmentectomy) | 6491 | 17.7 | 0.5 | 15.1 | 2.5 | 1.3 | 2.1 | |
| High | Subsegmentectomy | 2656 | 34.4 | 0.3 | 7.4 | 1.3 | 0.3 | 0.4 | |
| High | Liver transplantation | 791 | 0.6 | 10.1 | 23.1 | 12.6 | 2.1 | 3.5 | |
| High | Hepatopancreatoduodenectomy | 135 | 0.0 | 0.7 | 51.1 | 8.9 | 4.4 | 8.9 | |
| Gall bladder | Low | Cholangiotomy | 63 | 11.1 | 22.2 | 15.9 | 3.2 | 1.6 | 1.6 |
| Low | Cholecystolithotomy | 64 | 28.1 | 15.6 | 10.9 | 4.7 | 0.0 | 0.0 | |
| Low | Cholecystectomy | 129 693 | 72.9 | 16.3 | 3.6 | 1.1 | 0.4 | 0.6 | |
| Low | External cholecystostomy | 139 | 28.8 | 51.8 | 24.5 | 14.4 | 4.3 | 10.1 | |
| Low | Cystoenteric anastomosis | 36 | 11.1 | 5.6 | 22.2 | 5.6 | 5.6 | 11.1 | |
| Med | Choledocholithotomy | 2015 | 34.9 | 14.0 | 9.1 | 0.1 | 1.2 | 1.9 | |
| Med | Biliary tract reconstruction | 295 | 5.8 | 3.1 | 20.7 | 4.7 | 1.7 | 3.1 | |
| Med | Biliary bypass | 967 | 4.9 | 10.9 | 16.9 | 5.2 | 2.0 | 3.4 | |
| Med | Cholangioplasty | 96 | 12.5 | 18.8 | 25.0 | 2.1 | 2.1 | 2.1 | |
| Med | Duodenal papilloplasty | 29 | 13.8 | 3.4 | 10.3 | 10.3 | 3.4 | 3.4 | |
| Med | Choledocal dilatation | 278 | 26.3 | 1.8 | 9.0 | 3.2 | 0.4 | 0.4 | |
| Med | Biliary fistula closure | 16 | 31.3 | 43.8 | 31.3 | 12.5 | 6.3 | 18.8 | |
| High | Surgery for bile duct trauma (excluding drainage only) | 235 | 22.1 | 52.8 | 27.2 | 11.1 | 5.1 | 6.8 | |
| High | Malignant gallbladder tumor surgery (excluding simple cholecystectomy) | 1039 | 7.6 | 0.7 | 11.8 | 1.8 | 0.3 | 0.5 | |
| High | Malignant bile duct tumor surgery | 1108 | 0.8 | 0.5 | 33.6 | 5.6 | 3.2 | 5.7 | |
| High | Biliary atresia surgery | 38 | 47.4 | 28.9 | 21.1 | 10.5 | 0.0 | 0.0 | |
| Pancreas | Low | External pancreatic cyst drainage | 4 | 0.0 | 25.0 | 0.0 | 25.0 | 0.0 | 0.0 |
| Low | External pancreatic duct drainage | 19 | 0.0 | 63.2 | 57.9 | 31.6 | 5.3 | 21.1 | |
| Med | Pancreatorrhaphy | 4 | 0.0 | 100.0 | 75.0 | 25.0 | 0.0 | 25.0 | |
| Med | Partial pancreatic resection | 145 | 35.9 | 0.7 | 16.6 | 2.1 | 0.0 | 0.7 | |
| Med | Distal pancreatectomy (benign) | 1422 | 52.3 | 4.1 | 16.8 | 2.3 | 0.7 | 0.9 | |
| Med | Pancreatic cyst‐enterostomy | 20 | 5.0 | 10.0 | 25.0 | 5.0 | 10.0 | 10.0 | |
| Med | Pancreatic (duct) enterostomy | 280 | 0.0 | 7.5 | 18.6 | 4.6 | 2.1 | 3.6 | |
| Med | Acute pancreatitis surgery | 50 | 16.0 | 58.0 | 52.0 | 14.0 | 6.0 | 16.0 | |
| Med | Pancreatolithiasis surgery | 14 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| Med | Plexus pancreaticus capitalis resection | 0 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| High | Surgery for pancreatic trauma (excluding drainage only) | 59 | 5.1 | 78.0 | 44.1 | 25.4 | 8.5 | 13.6 | |
| High | Pancreaticoduodenectomy | 11 764 | 5.2 | 0.7 | 24.1 | 3.3 | 0.9 | 1.6 | |
| High | Distal pancreatectomy (malignant) | 5091 | 33.4 | 0.8 | 20.0 | 2.1 | 0.3 | 0.7 | |
| High | Total pancreatectomy | 635 | 1.9 | 3.5 | 15.7 | 4.6 | 1.9 | 3.0 | |
| High | Duodenum preserving pancreas head resection | 38 | 0.0 | 0.0 | 26.3 | 2.6 | 2.6 | 5.3 | |
| High | Segmental pancreatic resection | 153 | 8.5 | 1.3 | 34.0 | 2.0 | 0.7 | 0.7 | |
| High | Pancreas transplantation | 23 | 0.0 | 73.9 | 34.8 | 43.5 | 0.0 | 4.3 | |
| Spleen | Low | Splenorrhaphy | 24 | 16.7 | 87.5 | 29.2 | 29.2 | 8.3 | 8.3 |
| Med | Splenectomy | 1789 | 29.9 | 1.2 | 14.6 | 5.5 | 2.6 | 3.7 | |
| Med | Partial splenectomy | 20 | 35.0 | 20.0 | 10.0 | 15.0 | 0.0 | 0.0 | |
| Other | Low | Localized intra‐abdominal abscess surgery | 2376 | 32.7 | 70.5 | 14.6 | 6.6 | 2.2 | 3.2 |
| Low | Exploratory laparotomy | 12 401 | 49.3 | 30.3 | 16.8 | 13.2 | 6.2 | 9.0 | |
| Med | Acute diffuse peritonitis surgery | 15 542 | 22.1 | 92.6 | 27.3 | 7.8 | 8.0 | 11.5 | |
| Med | Ventral hernia surgery | 14 136 | 32.0 | 11.4 | 3.9 | 2.0 | 0.6 | 0.9 | |
| Med | Diaphragm suture | 294 | 34.0 | 40.5 | 19.7 | 9.5 | 4.4 | 6.5 | |
| Med | Esophageal hiatus hernia surgery | 1217 | 62.8 | 7.9 | 8.0 | 4.1 | 1.4 | 2.2 | |
| Med | Retroperitoneal tumor surgery | 1551 | 10.9 | 2.1 | 9.2 | 3.5 | 0.3 | 0.5 | |
| Med | Abdominal wall/mesenteric/omental tumor resection | 2054 | 31.3 | 15.3 | 7.7 | 4.3 | 0.9 | 1.9 | |
| Med | Gastrointestinal perforation closure | 421 | 11.9 | 90.5 | 35.4 | 14.0 | 11.6 | 16.2 | |
| High | Diaphragmatic hiatus hernia surgery | 56 | 37.5 | 42.9 | 12.5 | 3.6 | 10.7 | 12.5 |
Complications were defined by Clavien–Dindo grade IIIa‐V.
Operative mortality was a rate that combined 30‐day mortality and hospitalization death in 31–90 days after surgery.
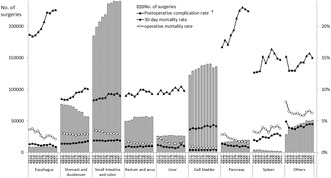
3.2. Annual trends in organ‐specific surgical procedures
Figure 1 illustrates the trends in the number of gastroenterological surgeries and key outcomes in Japan from 2012 to 2021. Long‐term trends indicate an increasing trend in the number of surgeries for five regions: the small intestine and colon, rectum and anus, gallbladder, pancreas, and the “others” classification. Conversely, the number of surgeries for the esophagus and liver remained stable, while those for the stomach and duodenum, and spleen showed decreasing trends. Notably, from a short‐term perspective, there was a decrease in the number of surgeries across all areas in 2020; however, the numbers rebounded, except for that of surgeries for the stomach and duodenum, liver, and spleen.
FIGURE 1.
Annual changes in the number of surgeries, 30‐day and operative mortality rates, and complication rates of each organ. †Postoperative complication was defined as grades IIIa–V in the Clavien–Dindo classification.
Table 3 summarizes the sex ratio and age distribution by organ in surgeries performed over a decade. The proportion of female patients increased in all organs, with the most significant increases observed in the spleen, esophagus, stomach, and duodenum. Across all organs, there has been an increase in the proportion of patients aged ≥70 years, particularly those >80 years. Conversely, the proportion of patients <60 years of age generally decreased, except for surgeries for the rectum and anus, wherein the proportion slightly increased.
TABLE 3.
Annual changes in surgeries of each organ by sex and age of patients.
| Organ | Year | No. of surgeries | Sex (%) | Age (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | <60 | 60 to 64 | 65–69 | 70–74 | 75–79 | ≥80 | |||
| Esophagus | 2012 | 8819 | 82.2 | 17.8 | 22.1 | 19.7 | 20.0 | 19.5 | 12.9 | 6.0 |
| 2013 | 8642 | 81.5 | 18.5 | 20.8 | 17.5 | 21.0 | 20.6 | 13.2 | 6.9 | |
| 2014 | 9021 | 81.5 | 18.4 | 20.8 | 16.5 | 21.4 | 20.9 | 13.8 | 6.6 | |
| 2015 | 8943 | 80.8 | 19.2 | 19.6 | 15.3 | 22.4 | 22.5 | 13.1 | 7.1 | |
| 2016 | 9212 | 79.6 | 20.4 | 20.1 | 14.4 | 22.9 | 20.5 | 14.5 | 7.5 | |
| 2017 | 9359 | 80.0 | 20.0 | 19.3 | 13.4 | 24.4 | 19.4 | 15.5 | 8.0 | |
| 2018 | 9286 | 78.4 | 21.6 | 19.0 | 12.8 | 21.3 | 21.6 | 16.7 | 8.7 | |
| 2019 | 9224 | 78.6 | 21.4 | 18.8 | 13.1 | 19.4 | 22.8 | 17.3 | 8.6 | |
| 2020 | 8713 | 79.0 | 21.0 | 18.4 | 13.5 | 18.3 | 23.5 | 16.5 | 9.8 | |
| 2021 | 8905 | 78.0 | 22.0 | 19.0 | 12.5 | 17.8 | 24.4 | 16.5 | 9.8 | |
| Stomach and duodenum | 2012 | 76 186 | 68.3 | 31.7 | 18.9 | 14.4 | 14.5 | 17.1 | 16.4 | 18.6 |
| 2013 | 75 583 | 67.9 | 32.1 | 18.6 | 13.1 | 15.5 | 17.2 | 16.9 | 18.7 | |
| 2014 | 74 920 | 67.6 | 32.4 | 17.9 | 12.1 | 16.0 | 17.8 | 16.7 | 19.5 | |
| 2015 | 73 877 | 67.8 | 32.2 | 17.4 | 11.1 | 17.1 | 17.8 | 16.6 | 19.9 | |
| 2016 | 72 234 | 67.8 | 32.2 | 17.0 | 10.2 | 18.1 | 17.1 | 16.6 | 21.0 | |
| 2017 | 68 287 | 67.2 | 32.8 | 16.3 | 9.9 | 17.5 | 17.3 | 17.2 | 21.8 | |
| 2018 | 65 152 | 66.9 | 33.1 | 16.0 | 9.0 | 16.4 | 18.0 | 17.5 | 23.2 | |
| 2019 | 63 610 | 66.5 | 33.5 | 15.6 | 8.8 | 15.0 | 19.0 | 18.5 | 23.2 | |
| 2020 | 57 171 | 66.6 | 33.4 | 15.3 | 8.2 | 13.8 | 20.1 | 18.5 | 24.1 | |
| 2021 | 56 759 | 65.9 | 34.1 | 15.7 | 7.7 | 12.6 | 20.9 | 18.1 | 25.0 | |
| Small intestine and colon | 2012 | 184 810 | 56.7 | 43.3 | 36.4 | 10.7 | 10.7 | 12.2 | 12.5 | 17.4 |
| 2013 | 198 677 | 56.9 | 43.1 | 35.6 | 10.1 | 11.3 | 12.7 | 12.4 | 17.8 | |
| 2014 | 206 857 | 56.9 | 43.1 | 34.7 | 9.4 | 12.0 | 13.1 | 12.4 | 18.4 | |
| 2015 | 214 453 | 57.1 | 42.9 | 34.0 | 8.9 | 12.9 | 13.1 | 12.3 | 18.7 | |
| 2016 | 218 228 | 57.3 | 42.7 | 33.7 | 8.4 | 13.6 | 12.5 | 12.4 | 19.3 | |
| 2017 | 235 359 | 56.7 | 43.3 | 32.7 | 8.0 | 13.2 | 12.7 | 12.9 | 20.5 | |
| 2018 | 236 496 | 56.9 | 43.1 | 32.2 | 7.7 | 12.6 | 13.4 | 13.2 | 21.1 | |
| 2019 | 239 612 | 56.3 | 43.7 | 32.1 | 7.4 | 11.7 | 13.9 | 13.5 | 21.2 | |
| 2020 | 238 631 | 56.2 | 43.8 | 32.6 | 7.3 | 10.7 | 14.6 | 13.4 | 21.5 | |
| 2021 | 240 448 | 56.0 | 44.0 | 31.9 | 7.3 | 10.3 | 15.5 | 12.7 | 22.3 | |
| Rectum and anus | 2012 | 49 704 | 58.3 | 41.7 | 22.3 | 14.8 | 14.6 | 15.5 | 14.3 | 18.5 |
| 2013 | 49 980 | 58.0 | 42.0 | 20.9 | 13.9 | 15.2 | 16.1 | 14.6 | 19.3 | |
| 2014 | 51 454 | 58.3 | 41.7 | 20.4 | 13.1 | 16.0 | 16.4 | 14.2 | 19.9 | |
| 2015 | 56 092 | 57.8 | 42.2 | 22.3 | 11.8 | 16.7 | 15.7 | 14.0 | 19.4 | |
| 2016 | 55 666 | 57.3 | 42.7 | 22.0 | 11.1 | 17.9 | 15.0 | 13.6 | 20.4 | |
| 2017 | 56 144 | 56.7 | 43.3 | 22.2 | 10.2 | 17.3 | 15.1 | 14.2 | 21.0 | |
| 2018 | 56 162 | 56.9 | 43.1 | 22.2 | 9.8 | 15.9 | 15.8 | 14.6 | 21.6 | |
| 2019 | 57 706 | 56.3 | 43.7 | 22.5 | 9.5 | 14.8 | 16.5 | 14.9 | 21.9 | |
| 2020 | 55 536 | 56.2 | 43.8 | 22.7 | 9.2 | 13.7 | 17.6 | 14.7 | 22.1 | |
| 2021 | 56 536 | 55.7 | 44.3 | 23.1 | 9.0 | 12.8 | 18.7 | 14.1 | 22.3 | |
| Liver | 2012 | 26 288 | 66.3 | 33.7 | 22.1 | 15.7 | 16.7 | 18.0 | 17.4 | 10.2 |
| 2013 | 25 814 | 66.1 | 33.9 | 21.3 | 14.6 | 17.6 | 18.7 | 17.3 | 10.5 | |
| 2014 | 26 518 | 66.3 | 33.7 | 21.5 | 13.7 | 18.1 | 19.8 | 16.6 | 10.3 | |
| 2015 | 26 378 | 65.7 | 34.3 | 20.8 | 12.8 | 18.9 | 19.4 | 16.5 | 11.5 | |
| 2016 | 27 212 | 66.4 | 33.6 | 20.3 | 11.5 | 20.5 | 18.6 | 17.0 | 12.1 | |
| 2017 | 27 397 | 65.8 | 34.2 | 20.1 | 11.0 | 20.2 | 18.8 | 17.2 | 12.7 | |
| 2018 | 26 531 | 66.5 | 33.5 | 19.6 | 10.3 | 18.8 | 19.6 | 17.8 | 13.8 | |
| 2019 | 26 582 | 66.3 | 33.7 | 19.4 | 10.1 | 16.5 | 21.1 | 18.6 | 14.2 | |
| 2020 | 26 614 | 66.0 | 34.0 | 20.6 | 9.5 | 15.1 | 21.7 | 18.7 | 14.4 | |
| 2021 | 26 250 | 65.2 | 34.8 | 20.8 | 9.9 | 14.1 | 22.4 | 17.3 | 15.5 | |
| Gall bladder | 2012 | 122 513 | 55.2 | 44.8 | 32.9 | 13.8 | 12.4 | 13.9 | 13.2 | 13.8 |
| 2013 | 129 162 | 55.3 | 44.7 | 32.6 | 12.9 | 13.0 | 14.2 | 13.2 | 14.0 | |
| 2014 | 131 182 | 55.6 | 44.4 | 32.1 | 11.8 | 13.9 | 14.5 | 13.2 | 14.5 | |
| 2015 | 133 126 | 55.6 | 44.4 | 32.0 | 11.2 | 15.0 | 14.1 | 13.0 | 14.8 | |
| 2016 | 137 360 | 55.4 | 44.6 | 32.6 | 10.6 | 15.5 | 13.1 | 12.9 | 15.3 | |
| 2017 | 138 267 | 55.6 | 44.4 | 32.2 | 10.2 | 15.1 | 13.5 | 13.2 | 15.8 | |
| 2018 | 139 844 | 55.3 | 44.7 | 31.8 | 9.7 | 14.2 | 14.2 | 13.4 | 16.7 | |
| 2019 | 140 214 | 55.4 | 44.6 | 31.6 | 9.6 | 13.3 | 14.7 | 13.9 | 16.9 | |
| 2020 | 134 332 | 55.9 | 44.1 | 31.3 | 9.1 | 12.2 | 15.6 | 14.0 | 17.8 | |
| 2021 | 136 111 | 55.2 | 44.8 | 31.7 | 9.1 | 11.5 | 16.6 | 13.0 | 18.2 | |
| Pancreas | 2012 | 15 550 | 60.0 | 40.0 | 19.8 | 15.2 | 17.0 | 19.5 | 18.2 | 10.3 |
| 2013 | 16 380 | 59.7 | 40.3 | 19.1 | 13.6 | 18.0 | 20.7 | 17.7 | 10.9 | |
| 2014 | 17 313 | 59.5 | 40.5 | 18.4 | 12.4 | 19.0 | 21.0 | 18.2 | 11.1 | |
| 2015 | 17 407 | 59.1 | 40.9 | 18.2 | 11.3 | 19.4 | 21.6 | 18.1 | 11.4 | |
| 2016 | 18 238 | 58.9 | 41.1 | 18.2 | 10.4 | 19.9 | 20.4 | 19.0 | 12.2 | |
| 2017 | 19 138 | 59.2 | 40.8 | 17.7 | 9.9 | 19.5 | 19.9 | 20.1 | 12.9 | |
| 2018 | 19 152 | 58.6 | 41.4 | 16.9 | 9.2 | 18.2 | 21.5 | 20.4 | 13.7 | |
| 2019 | 19 703 | 58.3 | 41.7 | 17.0 | 9.2 | 16.5 | 21.6 | 21.1 | 14.6 | |
| 2020 | 19 947 | 58.1 | 41.9 | 16.7 | 8.4 | 14.6 | 22.8 | 21.9 | 15.6 | |
| 2021 | 19 722 | 57.9 | 42.1 | 17.0 | 8.4 | 13.7 | 24.2 | 20.8 | 15.9 | |
| Spleen | 2012 | 4142 | 61.4 | 38.6 | 32.9 | 16.3 | 15.0 | 15.1 | 12.9 | 7.8 |
| 2013 | 4509 | 61.8 | 38.2 | 30.8 | 14.9 | 15.9 | 16.5 | 13.1 | 8.7 | |
| 2014 | 4272 | 61.8 | 38.2 | 29.9 | 13.0 | 17.3 | 17.0 | 13.8 | 9.1 | |
| 2015 | 3568 | 60.4 | 39.6 | 29.7 | 11.4 | 17.3 | 16.6 | 14.1 | 10.8 | |
| 2016 | 3171 | 57.3 | 42.7 | 31.9 | 11.7 | 17.7 | 15.7 | 12.5 | 10.5 | |
| 2017 | 2864 | 58.7 | 41.3 | 31.6 | 11.0 | 18.1 | 16.0 | 13.3 | 10.0 | |
| 2018 | 2544 | 56.6 | 43.4 | 32.6 | 9.9 | 15.6 | 16.9 | 13.9 | 11.1 | |
| 2019 | 2413 | 55.2 | 44.8 | 31.3 | 10.5 | 16.8 | 15.8 | 13.1 | 12.5 | |
| 2020 | 2096 | 54.4 | 45.6 | 32.8 | 11.4 | 12.6 | 16.7 | 14.1 | 12.4 | |
| 2021 | 1833 | 55.9 | 44.1 | 32.0 | 9.8 | 13.4 | 17.5 | 14.7 | 12.7 | |
| Others | 2012 | 28 779 | 55.4 | 44.6 | 31.1 | 11.7 | 11.7 | 13.8 | 13.7 | 18.0 |
| 2013 | 36 363 | 53.1 | 46.9 | 28.3 | 10.9 | 12.7 | 14.1 | 14.8 | 19.1 | |
| 2014 | 39 854 | 53.7 | 46.3 | 28.1 | 10.1 | 13.1 | 14.5 | 14.4 | 19.8 | |
| 2015 | 41 465 | 53.2 | 46.8 | 27.4 | 9.4 | 14.0 | 14.5 | 14.2 | 20.6 | |
| 2016 | 43 523 | 54.0 | 46.0 | 27.5 | 9.2 | 14.6 | 13.5 | 14.0 | 21.2 | |
| 2017 | 45 622 | 54.1 | 45.9 | 27.0 | 8.2 | 14.7 | 13.5 | 14.6 | 21.9 | |
| 2018 | 46 587 | 54.1 | 45.9 | 26.8 | 8.2 | 14.0 | 14.4 | 14.7 | 21.9 | |
| 2019 | 50 525 | 54.8 | 45.2 | 27.0 | 8.1 | 12.7 | 15.3 | 15.0 | 21.9 | |
| 2020 | 50 048 | 54.5 | 45.5 | 27.2 | 7.9 | 11.9 | 16.0 | 14.9 | 22.1 | |
| 2021 | 51 216 | 54.6 | 45.4 | 27.6 | 7.8 | 11.3 | 17.1 | 14.0 | 22.2 | |
Table 4 compiles the data on the institutions where surgeries were performed and the participation rates of anesthesiologists and board‐certified surgeons. Long‐term trends indicate that surgeries for all organs are increasingly being performed at certified or affiliated institutions. However, in 2021, there was a slight decrease in the number of spleen and liver surgeries performed at these institutions. The participation rates of anesthesiologists and board‐certified surgeons in surgery increased annually across all areas. Notably, the participation rate of anesthesiologists in rectal and anal surgeries was approximately 87%, which was approximately 10% lower than that in other areas. Furthermore, the involvement of board‐certified surgeons in surgeries of the esophagus, liver, and pancreas is exceptionally high, exceeding 95%.
TABLE 4.
Annual changes in surgeries of each organ by institution type and specialist participation rate.
| Organ | Year | No. of surgeries | Institution type (%) | Anesthesiologist participation (%) | Board‐certified surgeon participation (%) | Operating surgeon (%) | |||
|---|---|---|---|---|---|---|---|---|---|
| Certified institution | Affiliated institution | Others | Board‐certified surgeon | Non‐board‐ certified surgeon | |||||
| Esophagus | 2012 | 8819 | 78.1 | 5.9 | 16.0 | 97.4 | 87.0 | 62.7 | 37.3 |
| 2013 | 8642 | 90.6 | 7.1 | 2.4 | 97.3 | 88.4 | 64.4 | 35.6 | |
| 2014 | 9021 | 91.1 | 6.1 | 2.8 | 97.9 | 90.1 | 67.6 | 32.4 | |
| 2015 | 8943 | 91.5 | 6.0 | 2.5 | 97.9 | 91.1 | 69.4 | 30.6 | |
| 2016 | 9212 | 92.4 | 5.0 | 2.6 | 98.2 | 91.2 | 70.0 | 30.0 | |
| 2017 | 9359 | 92.7 | 4.0 | 3.3 | 97.9 | 92.5 | 71.8 | 28.2 | |
| 2018 | 9286 | 93.8 | 4.0 | 2.2 | 98.5 | 94.7 | 75.2 | 24.8 | |
| 2019 | 9224 | 94.3 | 3.8 | 1.9 | 98.4 | 94.2 | 76.4 | 23.6 | |
| 2020 | 8713 | 95.2 | 3.2 | 1.5 | 98.9 | 95.7 | 78.3 | 21.7 | |
| 2021 | 8905 | 95.9 | 2.7 | 1.4 | 98.7 | 96.0 | 79.2 | 20.8 | |
| Stomach and duodenum | 2012 | 76 186 | 63.5 | 15.6 | 20.9 | 93.5 | 70.3 | 35.6 | 64.4 |
| 2013 | 75 583 | 76.3 | 19.3 | 4.4 | 93.3 | 73.5 | 37.7 | 62.3 | |
| 2014 | 74 920 | 77.0 | 18.2 | 4.8 | 93.6 | 75.9 | 39.2 | 60.8 | |
| 2015 | 73 877 | 77.1 | 18.3 | 4.6 | 93.9 | 76.1 | 39.2 | 60.8 | |
| 2016 | 72 234 | 79.6 | 16.1 | 4.3 | 94.6 | 78.7 | 41.0 | 59.0 | |
| 2017 | 68 287 | 79.6 | 15.3 | 5.1 | 94.8 | 79.7 | 41.8 | 58.2 | |
| 2018 | 65 152 | 80.0 | 14.8 | 5.1 | 95.1 | 81.4 | 43.2 | 56.8 | |
| 2019 | 63 610 | 81.3 | 14.2 | 4.5 | 95.4 | 83.8 | 46.1 | 53.9 | |
| 2020 | 57 171 | 80.8 | 14.8 | 4.4 | 95.7 | 85.4 | 47.6 | 52.4 | |
| 2021 | 56 759 | 81.3 | 14.2 | 4.4 | 96.2 | 88.1 | 51.1 | 48.9 | |
| Small intestine and colon | 2012 | 184 810 | 60.6 | 18.2 | 21.2 | 88.9 | 59.9 | 25.4 | 74.6 |
| 2013 | 198 677 | 72.6 | 22.2 | 5.2 | 89.6 | 62.7 | 26.6 | 73.4 | |
| 2014 | 206 857 | 73.0 | 21.4 | 5.6 | 90.8 | 65.4 | 28.1 | 71.9 | |
| 2015 | 214 453 | 73.8 | 20.7 | 5.5 | 91.6 | 66.3 | 28.5 | 71.5 | |
| 2016 | 218 228 | 75.6 | 19.0 | 5.5 | 92.4 | 68.1 | 29.5 | 70.5 | |
| 2017 | 235 359 | 76.0 | 18.0 | 6.0 | 92.9 | 70.1 | 31.1 | 68.9 | |
| 2018 | 236 496 | 76.3 | 17.5 | 6.1 | 93.3 | 71.8 | 32.6 | 67.4 | |
| 2019 | 239 612 | 77.1 | 17.1 | 5.8 | 94.1 | 74.0 | 33.2 | 66.8 | |
| 2020 | 238 631 | 76.5 | 17.9 | 5.6 | 94.5 | 75.9 | 34.2 | 65.8 | |
| 2021 | 240 448 | 77.5 | 16.9 | 5.6 | 95.1 | 79.5 | 37.6 | 62.4 | |
| Rectum and anus | 2012 | 49 704 | 60.4 | 18.2 | 21.4 | 85.7 | 68.6 | 37.6 | 62.4 |
| 2013 | 49 980 | 72.9 | 21.7 | 5.4 | 87.3 | 71.2 | 39.4 | 60.6 | |
| 2014 | 51 454 | 73.5 | 20.9 | 5.6 | 87.9 | 73.7 | 41.6 | 58.4 | |
| 2015 | 56 092 | 72.5 | 20.8 | 6.7 | 84.9 | 73.5 | 41.5 | 58.5 | |
| 2016 | 55 666 | 74.1 | 19.4 | 6.6 | 85.7 | 74.7 | 42.1 | 57.9 | |
| 2017 | 56 144 | 73.8 | 18.2 | 8.0 | 84.8 | 76.1 | 43.9 | 56.1 | |
| 2018 | 56 162 | 74.1 | 17.9 | 8.0 | 85.2 | 77.2 | 46.7 | 53.3 | |
| 2019 | 57 706 | 74.9 | 17.3 | 7.8 | 86.0 | 80.1 | 48.9 | 51.1 | |
| 2020 | 55 536 | 74.5 | 18.6 | 6.8 | 86.7 | 81.7 | 51.0 | 49.0 | |
| 2021 | 56 536 | 75.8 | 17.6 | 6.6 | 87.4 | 84.0 | 55.2 | 44.8 | |
| Liver | 2012 | 26 288 | 74.2 | 9.2 | 16.7 | 95.4 | 85.7 | 57.4 | 42.6 |
| 2013 | 25 814 | 86.3 | 10.7 | 2.9 | 96.3 | 87.5 | 57.1 | 42.9 | |
| 2014 | 26 518 | 86.3 | 10.0 | 3.7 | 96.4 | 89.0 | 59.6 | 40.4 | |
| 2015 | 26 378 | 87.3 | 9.5 | 3.2 | 96.6 | 89.1 | 59.1 | 40.9 | |
| 2016 | 27 212 | 88.4 | 8.8 | 2.9 | 96.8 | 90.0 | 59.6 | 40.4 | |
| 2017 | 27 397 | 89.0 | 7.8 | 3.1 | 97.1 | 91.8 | 62.5 | 37.5 | |
| 2018 | 26 531 | 89.4 | 7.1 | 3.5 | 97.3 | 92.8 | 64.1 | 35.9 | |
| 2019 | 26 582 | 89.7 | 6.8 | 3.6 | 97.3 | 94.1 | 66.4 | 33.6 | |
| 2020 | 26 614 | 89.6 | 7.2 | 3.1 | 97.4 | 94.7 | 67.7 | 32.3 | |
| 2021 | 26 250 | 90.6 | 6.1 | 3.3 | 97.4 | 95.2 | 70.9 | 29.1 | |
| Gall bladder | 2012 | 122 513 | 57.5 | 19.6 | 22.9 | 92.1 | 62.8 | 26.3 | 73.7 |
| 2013 | 129 162 | 69.9 | 24.1 | 5.9 | 92.2 | 65.4 | 27.3 | 72.7 | |
| 2014 | 131 182 | 70.3 | 23.3 | 6.4 | 92.3 | 67.4 | 28.1 | 71.9 | |
| 2015 | 133 126 | 70.8 | 22.8 | 6.4 | 92.9 | 68.4 | 28.1 | 71.9 | |
| 2016 | 137 360 | 72.4 | 21.3 | 6.3 | 93.5 | 69.4 | 28.9 | 71.1 | |
| 2017 | 138 267 | 72.6 | 20.1 | 7.3 | 93.7 | 71.4 | 29.9 | 70.1 | |
| 2018 | 139 844 | 72.5 | 20.1 | 7.4 | 94.1 | 73.1 | 31.1 | 68.9 | |
| 2019 | 140 214 | 73.5 | 19.4 | 7.1 | 94.4 | 75.7 | 32.3 | 67.7 | |
| 2020 | 134 332 | 72.9 | 20.2 | 6.9 | 94.8 | 77.7 | 33.8 | 66.2 | |
| 2021 | 136 111 | 73.4 | 19.7 | 6.9 | 95.1 | 80.5 | 36.1 | 63.9 | |
| Pancreas | 2012 | 15 550 | 72.8 | 8.7 | 18.5 | 96.3 | 86.5 | 59.9 | 40.1 |
| 2013 | 16 380 | 86.5 | 11.0 | 2.4 | 95.9 | 87.6 | 60.2 | 39.8 | |
| 2014 | 17 313 | 86.9 | 9.9 | 3.3 | 96.2 | 89.1 | 61.3 | 38.7 | |
| 2015 | 17 407 | 88.4 | 9.1 | 2.4 | 96.4 | 90.3 | 61.6 | 38.4 | |
| 2016 | 18 238 | 89.8 | 8.0 | 2.3 | 96.8 | 91.1 | 62.4 | 37.6 | |
| 2017 | 19 138 | 90.4 | 7.1 | 2.5 | 97.2 | 92.3 | 63.9 | 36.1 | |
| 2018 | 19 152 | 91.3 | 6.4 | 2.3 | 97.3 | 93.4 | 66.5 | 33.5 | |
| 2019 | 19 703 | 91.9 | 6.2 | 1.9 | 97.2 | 95.1 | 69.2 | 30.8 | |
| 2020 | 19 947 | 91.9 | 6.3 | 1.8 | 97.6 | 95.7 | 70.4 | 29.6 | |
| 2021 | 19 722 | 92.8 | 5.4 | 1.8 | 97.9 | 96.8 | 75.3 | 24.7 | |
| Spleen | 2012 | 4142 | 70.5 | 9.5 | 20.0 | 81.7 | 75.8 | 44.4 | 55.6 |
| 2013 | 4509 | 83.2 | 13.8 | 3.0 | 95.2 | 75.4 | 43.3 | 56.7 | |
| 2014 | 4272 | 85.4 | 11.5 | 3.1 | 94.6 | 77.5 | 45.2 | 54.8 | |
| 2015 | 3568 | 85.6 | 12.3 | 2.1 | 94.8 | 78.9 | 45.5 | 54.5 | |
| 2016 | 3171 | 86.8 | 10.1 | 3.1 | 95.7 | 80.5 | 48.0 | 52.0 | |
| 2017 | 2864 | 87.4 | 9.3 | 3.3 | 95.3 | 82.3 | 49.1 | 50.9 | |
| 2018 | 2544 | 86.9 | 9.7 | 3.4 | 95.3 | 84.7 | 49.3 | 50.7 | |
| 2019 | 2413 | 88.1 | 8.7 | 3.2 | 96.2 | 86.8 | 54.0 | 46.0 | |
| 2020 | 2096 | 88.6 | 9.2 | 2.2 | 96.5 | 88.3 | 55.7 | 44.3 | |
| 2021 | 1833 | 88.3 | 8.8 | 2.8 | 96.3 | 90.3 | 60.3 | 39.7 | |
| Others | 2012 | 28 779 | 65.7 | 15.2 | 19.1 | 91.0 | 61.1 | 27.6 | 72.4 |
| 2013 | 36 363 | 76.1 | 19.3 | 4.6 | 91.5 | 63.4 | 28.5 | 71.5 | |
| 2014 | 39 854 | 76.6 | 18.2 | 5.1 | 91.9 | 64.9 | 29.7 | 70.3 | |
| 2015 | 41 465 | 78.0 | 17.2 | 4.8 | 92.4 | 65.6 | 29.4 | 70.6 | |
| 2016 | 43 523 | 79.4 | 15.8 | 4.8 | 92.7 | 67.3 | 30.3 | 69.7 | |
| 2017 | 45 622 | 80.1 | 14.8 | 5.1 | 93.1 | 69.7 | 32.3 | 67.7 | |
| 2018 | 46 587 | 80.2 | 14.2 | 5.7 | 93.8 | 71.2 | 33.1 | 66.9 | |
| 2019 | 50 525 | 80.9 | 13.9 | 5.3 | 94.3 | 74.0 | 35.2 | 64.8 | |
| 2020 | 50 048 | 80.4 | 14.7 | 4.9 | 94.3 | 76.1 | 37.0 | 63.0 | |
| 2021 | 51 216 | 82.1 | 13.4 | 4.5 | 94.9 | 79.6 | 39.5 | 60.5 | |
Table 5 presents the temporal changes in the complication and mortality rates. Operative mortality decreased across all areas compared to a decade ago, with the most significant reductions observed in surgeries involving the pancreas (−46.4%), esophagus (−41.7%), and liver (−34.8%). However, the surgical complications slowly increased or remained stable. A modest decline was observed after experiencing minor peaks over the past 2–3 years.
TABLE 5.
Annual changes in surgeries of each organ by complication and mortality rates.
| Organ | Year | No. of surgeries | No. of postoperative complications (%) a | No. of postoperative 30‐day mortalities (%) | No. of operative mortalities (%) b |
|---|---|---|---|---|---|
| Esophagus | 2012 | 8819 | 1653 (18.7) | 117 (1.3) | 315 (3.6) |
| 2013 | 8642 | 1593 (18.4) | 121 (1.4) | 327 (3.8) | |
| 2014 | 9021 | 1679 (18.6) | 115 (1.3) | 289 (3.2) | |
| 2015 | 8943 | 1709 (19.1) | 103 (1.2) | 304 (3.4) | |
| 2016 | 9212 | 1805 (19.6) | 100 (1.1) | 238 (2.6) | |
| 2017 | 9359 | 1938 (20.7) | 108 (1.2) | 208 (2.2) | |
| 2018 | 9286 | 2065 (22.2) | 108 (1.2) | 246 (2.6) | |
| 2019 | 9224 | 2035 (22.1) | 119 (1.3) | 246 (2.7) | |
| 2020 | 8713 | 1963 (22.5) | 95 (1.1) | 212 (2.4) | |
| 2021 | 8905 | 2011 (22.6) | 84 (0.9) | 183 (2.1) | |
| Stomach and duodenum | 2012 | 76 186 | 6447 (8.5) | 1085 (1.4) | 2381 (3.1) |
| 2013 | 75 583 | 6380 (8.4) | 1059 (1.4) | 2269 (3.0) | |
| 2014 | 74 920 | 6328 (8.4) | 1064 (1.4) | 2174 (2.9) | |
| 2015 | 73 877 | 6418 (8.7) | 1007 (1.4) | 2110 (2.9) | |
| 2016 | 72 234 | 6413 (8.9) | 1066 (1.5) | 2016 (2.8) | |
| 2017 | 68 287 | 6455 (9.5) | 1046 (1.5) | 1863 (2.7) | |
| 2018 | 65 152 | 6228 (9.6) | 1048 (1.6) | 1833 (2.8) | |
| 2019 | 63 610 | 6159 (9.7) | 1022 (1.6) | 1826 (2.9) | |
| 2020 | 57 171 | 5849 (10.2) | 977 (1.7) | 1679 (2.9) | |
| 2021 | 56 759 | 5741 (10.1) | 1047 (1.8) | 1612 (2.8) | |
| Small intestine and colon | 2012 | 184 810 | 15 395 (8.3) | 3564 (1.9) | 6583 (3.6) |
| 2013 | 198 677 | 16 709 (8.4) | 3723 (1.9) | 6803 (3.4) | |
| 2014 | 206 857 | 17 776 (8.6) | 3822 (1.9) | 6961 (3.4) | |
| 2015 | 214 453 | 18 372 (8.6) | 4019 (1.9) | 7092 (3.3) | |
| 2016 | 218 228 | 19 020 (8.7) | 3933 (1.8) | 6621 (3.0) | |
| 2017 | 235 359 | 21 854 (9.3) | 4588 (1.9) | 7118 (3.0) | |
| 2018 | 236 496 | 21 881 (9.3) | 4452 (1.9) | 7116 (3.0) | |
| 2019 | 239 612 | 22 061 (9.2) | 4671 (1.9) | 7298 (3.0) | |
| 2020 | 238 631 | 22 344 (9.4) | 4791 (2.0) | 7261 (3.0) | |
| 2021 | 240 448 | 21 581 (9.0) | 4609 (1.9) | 6730 (2.8) | |
| Rectum and anus | 2012 | 49 704 | 4488 (9.0) | 462 (0.9) | 802 (1.6) |
| 2013 | 49 980 | 4684 (9.4) | 517 (1.0) | 858 (1.7) | |
| 2014 | 51 454 | 4711 (9.2) | 449 (0.9) | 792 (1.5) | |
| 2015 | 56 092 | 4986 (8.9) | 519 (0.9) | 824 (1.5) | |
| 2016 | 55 666 | 5194 (9.3) | 503 (0.9) | 766 (1.4) | |
| 2017 | 56 144 | 5600 (10.0) | 556 (1.0) | 829 (1.5) | |
| 2018 | 56 162 | 5622 (10.0) | 522 (0.9) | 803 (1.4) | |
| 2019 | 57 706 | 5573 (9.7) | 563 (1.0) | 839 (1.5) | |
| 2020 | 55 536 | 5383 (9.7) | 555 (1.0) | 797 (1.4) | |
| 2021 | 56 536 | 5250 (9.3) | 577 (1.0) | 798 (1.4) | |
| Liver | 2012 | 26 288 | 2454 (9.3) | 310 (1.2) | 605 (2.3) |
| 2013 | 25 814 | 2549 (9.9) | 275 (1.1) | 575 (2.2) | |
| 2014 | 26 518 | 2466 (9.3) | 246 (0.9) | 481 (1.8) | |
| 2015 | 26 378 | 2537 (9.6) | 234 (0.9) | 451 (1.7) | |
| 2016 | 27 212 | 2543 (9.3) | 222 (0.8) | 382 (1.4) | |
| 2017 | 27 397 | 2724 (9.9) | 214 (0.8) | 364 (1.3) | |
| 2018 | 26 531 | 2737 (10.3) | 189 (0.7) | 372 (1.4) | |
| 2019 | 26 582 | 2624 (9.9) | 201 (0.8) | 334 (1.3) | |
| 2020 | 26 614 | 2804 (10.5) | 338 (1.3) | 475 (1.8) | |
| 2021 | 26 250 | 2573 (9.8) | 271 (1.0) | 390 (1.5) | |
| Gall bladder | 2012 | 122 513 | 4587 (3.7) | 531 (0.4) | 1082 (0.9) |
| 2013 | 129 162 | 4982 (3.9) | 546 (0.4) | 1130 (0.9) | |
| 2014 | 131 182 | 5020 (3.8) | 569 (0.4) | 1097 (0.8) | |
| 2015 | 133 126 | 5231 (3.9) | 541 (0.4) | 1036 (0.8) | |
| 2016 | 137 360 | 5320 (3.9) | 559 (0.4) | 980 (0.7) | |
| 2017 | 138 267 | 5761 (4.2) | 576 (0.4) | 968 (0.7) | |
| 2018 | 139 844 | 5964 (4.3) | 584 (0.4) | 954 (0.7) | |
| 2019 | 140 214 | 5748 (4.1) | 565 (0.4) | 935 (0.7) | |
| 2020 | 134 332 | 5888 (4.4) | 620 (0.5) | 978 (0.7) | |
| 2021 | 136 111 | 5702 (4.2) | 612 (0.4) | 930 (0.7) | |
| Pancreas | 2012 | 15 550 | 2595 (16.7) | 213 (1.4) | 437 (2.8) |
| 2013 | 16 380 | 2917 (17.8) | 211 (1.3) | 482 (2.9) | |
| 2014 | 17 313 | 2966 (17.1) | 195 (1.1) | 423 (2.4) | |
| 2015 | 17 407 | 3229 (18.6) | 185 (1.1) | 379 (2.2) | |
| 2016 | 18 238 | 3543 (19.4) | 185 (1.0) | 390 (2.1) | |
| 2017 | 19 138 | 4076 (21.3) | 219 (1.1) | 365 (1.9) | |
| 2018 | 19 152 | 4309 (22.5) | 178 (0.9) | 325 (1.7) | |
| 2019 | 19 703 | 4522 (23.0) | 199 (1.0) | 335 (1.7) | |
| 2020 | 19 947 | 4520 (22.7) | 205 (1.0) | 345 (1.7) | |
| 2021 | 19 722 | 4415 (22.4) | 164 (0.8) | 290 (1.5) | |
| Spleen | 2012 | 4142 | 528 (12.7) | 84 (2.0) | 138 (3.3) |
| 2013 | 4509 | 575 (12.8) | 79 (1.8) | 139 (3.1) | |
| 2014 | 4272 | 549 (12.9) | 88 (2.1) | 137 (3.2) | |
| 2015 | 3568 | 543 (15.2) | 88 (2.5) | 144 (4.0) | |
| 2016 | 3171 | 449 (14.2) | 76 (2.4) | 117 (3.7) | |
| 2017 | 2864 | 434 (15.2) | 65 (2.3) | 89 (3.1) | |
| 2018 | 2544 | 418 (16.4) | 69 (2.7) | 104 (4.1) | |
| 2019 | 2413 | 380 (15.7) | 71 (2.9) | 97 (4.0) | |
| 2020 | 2096 | 313 (14.9) | 63 (3.0) | 87 (4.2) | |
| 2021 | 1833 | 270 (14.7) | 49 (2.7) | 69 (3.8) | |
| Others | 2012 | 28 779 | 4388 (15.2) | 1399 (4.9) | 2293 (8.0) |
| 2013 | 36 363 | 4712 (13.0) | 1401 (3.9) | 2346 (6.5) | |
| 2014 | 39 854 | 5176 (13.0) | 1521 (3.8) | 2489 (6.2) | |
| 2015 | 41 465 | 5380 (13.0) | 1541 (3.7) | 2545 (6.1) | |
| 2016 | 43 523 | 5975 (13.7) | 1760 (4.0) | 2684 (6.2) | |
| 2017 | 45 622 | 6539 (14.3) | 1909 (4.2) | 2699 (5.9) | |
| 2018 | 46 587 | 6645 (14.3) | 1865 (4.0) | 2710 (5.8) | |
| 2019 | 50 525 | 7750 (15.3) | 2221 (4.4) | 3220 (6.4) | |
| 2020 | 50 048 | 7838 (15.7) | 2267 (4.5) | 3284 (6.6) | |
| 2021 | 51 216 | 7697 (15.0) | 2293 (4.5) | 3173 (6.2) |
Complications were defined by Clavien–Dindo grade IIIa–V.
Operative mortality was a rate that combined 30‐day mortality and hospitalization death in 31–90 days after surgery.
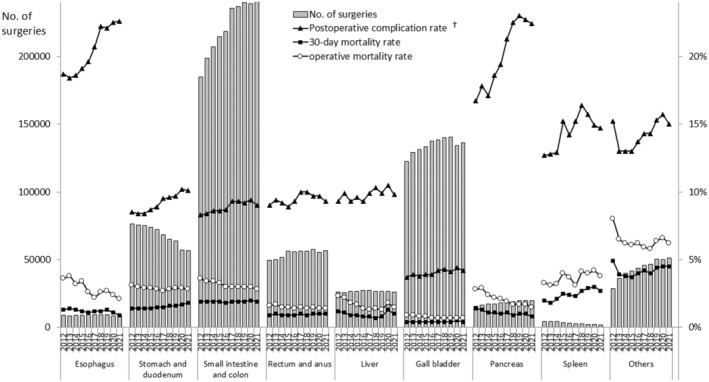
3.3. Endoscopic surgery rate in major surgical procedures
Figure 2 presents the trends in the endoscopic surgery rates across eight major surgical procedures. Within these procedures, established as benchmarks for improving surgical quality, the rates of endoscopic surgery have maintained their trend in recent years, still increasing by approximately 3% annually. Particularly, esophagectomy has exhibited the most significant increase in endoscopic surgery since 2016.
FIGURE 2.
Annual changes in the rate of endoscopic surgery in the eight major surgical procedures. † including pylorus‐preserving gastrectomy and segmental gastrectomy, ‡ including proximal gastrectomy, § segmentectomy or more; excluding lateral segmentectomy.
3.4. Operative procedures with high rates of emergency surgeries
Table 6 lists the top 20 procedures with the highest rates of emergency surgery among those performed in more than 100 cases annually, out of 80 applicable procedures. The list predominantly includes procedures related to abdominal trauma, acute abdomen, and oncology emergencies. Compared to the remaining 60 procedures, these 20 procedures have a lower participation rate of board‐certified surgeons (median, 80.0% vs. 90.9%), and notably higher rates of postoperative complications (18.7% vs. 12.0%), re‐operations (7.8% vs. 3.9%), postoperative 30‐day mortalities (4.5% vs. 0.9%), and operative mortalities (7.2% vs. 1.4%).
TABLE 6.
Top 20 operative procedures with the highest rates of emergency surgery.
| Order | Organ/difficulty level | Operative procedure | No. of surgeries | Emergency surgeries (%) | Board‐certified surgeon participation (%) | Postoperative complications (%) a | Re‐operations (%) | Postoperative 30‐day mortalities (%) | Operative mortalities (%) b |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Ot/med | Acute diffuse peritonitis surgery | 15 542 | 92.6 | 80.3 | 27.3 | 7.8 | 8.0 | 11.5 |
| 2 | St/low | Gastric suture c | 5327 | 91.5 | 75.1 | 17.7 | 5.7 | 5.7 | 7.5 |
| 3 | Ot/med | Gastrointestinal perforation closure | 421 | 90.5 | 80.3 | 35.4 | 14.0 | 11.6 | 16.2 |
| 4 | Li/high | Surgery for hepatic trauma d | 394 | 82.0 | 58.6 | 48.5 | 49.0 | 22.8 | 26.6 |
| 5 | In/low | Disinvagination (invasive) | 152 | 80.3 | 76.3 | 5.3 | 2.0 | 2.6 | 3.3 |
| 6 | Es/med | Esophageal suture (perforation, injury) | 183 | 74.9 | 86.9 | 36.6 | 13.7 | 3.3 | 4.9 |
| 7 | Ot/low | Localized intra‐abdominal abscess surgery | 2376 | 70.5 | 75.8 | 14.6 | 6.6 | 2.2 | 3.2 |
| 8 | In/med | Intestinal obstruction surgery (with enterectomy) | 26 275 | 68.3 | 76.6 | 10.2 | 4.4 | 2.4 | 3.4 |
| 9 | In/low | Appendectomy | 56 071 | 67.6 | 68.3 | 1.8 | 1.0 | 0.1 | 0.2 |
| 10 | In/low | Partial small bowel resection (benign) | 9017 | 62.5 | 78.9 | 20.4 | 10.4 | 6.7 | 9.1 |
| 11 | Re/med | Hartmann's procedure | 6408 | 58.6 | 83.1 | 20.8 | 6.0 | 5.6 | 7.5 |
| 12 | Gb/high | Surgery for bile duct trauma e | 235 | 52.8 | 90.2 | 27.2 | 11.1 | 5.1 | 6.8 |
| 13 | Gb/low | External cholecystostomy | 139 | 51.8 | 65.5 | 24.5 | 14.4 | 4.3 | 10.1 |
| 14 | In/low | Ileocecal resection (benign) | 4970 | 49.1 | 79.0 | 10.3 | 4.1 | 2.2 | 3.0 |
| 15 | In/low | Partial colectomy and sigmoid colectomy (benign) | 8536 | 45.3 | 80.8 | 15.5 | 6.3 | 4.1 | 5.6 |
| 16 | St/low | Gastric pyloroplasty | 106 | 43.4 | 57.5 | 4.7 | 5.7 | 0.9 | 0.9 |
| 17 | Ot/med | Diaphragm suture | 294 | 40.5 | 83.2 | 19.7 | 9.5 | 4.4 | 6.5 |
| 18 | In/med | Total colectomy | 1546 | 33.4 | 84.0 | 23.9 | 9.5 | 7.9 | 9.8 |
| 19 | Ot/low | Exploratory laparotomy | 12 401 | 30.3 | 82.5 | 16.8 | 13.2 | 6.2 | 9.0 |
| 20 | In/low | Enterotomy and enterorrhaphy | 4268 | 29.7 | 78.9 | 17.0 | 7.7 | 4.5 | 7.5 |
Abbreviations: Es, esophagus; Gb, gall bladder; In, small intestine and colon; Li, liver; Ot, others; Re, rectum; St, stomach and duodenum.
Complications were defined by Clavien–Dindo grade IIIa–V.
Operative mortality was a rate that combined 30‐day mortality and hospitalization death in 31 to 90 days after surgery.
Gastric suture includes gastric suture for gastric rupture, suture closure for gastroduodenal perforation, and omental implantation and omental transposition.
Surgery for hepatic trauma excludes drainage only.
Surgery for bile duct trauma excludes drainage only.
4. DISCUSSION
By comprehensively reviewing data from actual clinical practices in Japan registered in the NCD, this section addresses the following: the number of surgeries, patient demographics, surgical environments, endoscopic surgery, and surgical outcomes, particularly for the esophagus, liver, pancreas, and Acute Care Surgery (ACS), and highlights studies focusing on the gender of surgeons.
The impact of the coronavirus disease 2019 pandemic has led to a decrease in surgeries across all areas, 28 with an overall reduction of 2.7%. 26 However, the data suggest a return to the original trends by 2021. This result indicates that surgical care was gradually returning to normalcy as treatments and the healthcare system for the coronavirus disease 2019 were organized, clarifying appropriate measures for surgical patients. Upon closer examination, it appears that the increase in surgical procedures in the small intestine, colon, rectum and anus, gallbladder, pancreas, and others may be attributed to improved diagnostic capabilities for diseases and the growing older adult population. Conversely, the decrease in the number of stomach and duodenum, and spleen surgeries may be influenced by a reduction in disease incidence rates and the development of alternative treatment methods. 29 , 30
Consistent with earlier reports, there was a clear trend towards aging in patients undergoing surgery. Notably, there has been a significant increase in the proportion of patients ≥80 years, which is likely attributable to the rise in the aging population 31 and the extension of healthy life expectancy. 32 However, the proportion of patients <60 years undergoing surgery for rectal and anal issues has exhibited a slight increase, likely due to the westernization of diets, stress, and decreased physical activity, contributing to the incidence of rectal tumors. 33 While the proportion of male patients remained high in all areas, the last decade has generally demonstrated a shift towards an increasing ratio of female patients. This trend can be attributed to the growing aging population and the higher proportion of women in the older adult population. 31
The trend of surgeries being conducted in certified institutions under the management of anesthesiologists, with the involvement of board‐certified surgeons, is becoming consistently stronger despite some variations across different organs. Receiving surgical training in a well‐equipped environment is beneficial for trainee surgeons, and most importantly, maintaining a high surgical standard is advantageous and desirable for patients. 34
The trend of increasing endoscopic surgery is expected to persist in the foreseeable future. This trend has been significantly influenced by the widespread adoption of robotic surgery into daily practice, in addition to laparoscopic and thoracoscopic surgeries. As the advantages of robotic surgery become increasingly apparent, particularly in procedures where endoscopic surgery is relatively less common, the proportion of endoscopic surgeries is likely to further increase. Moreover, there is considerable anticipation regarding the performance and innovative features of surgical robots that will emerge in the future.
General trends in surgical outcomes remained consistent. The most significant observation was the uniform decline in operative mortality across all areas. There is substantial significance in maintaining these results as the number of surgeries and the proportion of older adult patients continue to increase. This reflects the tangible efforts of Japanese gastrointestinal surgeons to improve outcomes. However, an increase in complications, diverging from the trend in operative mortality, has been noted previously, making the control of complications an ongoing challenge.
We further focus on the surgical outcomes of two critical issues: the first concerns surgeries involving the esophagus, liver, and pancreas, and the second pertains to ACS. The esophagus, liver, and pancreas share the common outcome of substantial improvements in operative mortality in recent years. A distinguishing characteristic is the limited number of surgeries compared to other areas, with a relatively high proportion of these being high‐difficulty surgeries. However, what appears most crucial is the notably high participation rate of board‐certified surgeons, which can be interpreted as contributing to favorable outcomes. While the importance of board‐certified surgeons in surgeries has already been reported in some quarters, 35 , 36 the matter at hand involves devising ways to train more board‐certified surgeons and enhance their engagement across a broader range of organ specialties.
The second issue is how to improve ACS outcomes. The traditional pillars of ACS encompass trauma, emergency general surgery, and surgical critical care, 37 with surgical rescue being recently added to these core areas. 38 These are characterized by a lower participation rate of board‐certified surgeons compared to other procedures, as well as higher rates of complications, re‐operations, and notably worse morbidities. Unlike elective surgeries that pursue curative treatment from an anatomical perspective, the formulation of treatment strategies for time‐sensitive surgeries requires a different approach. Merely increasing the participation rate of board‐certified surgeons may not be sufficient to improve ACS outcomes significantly. To improve surgical outcomes for severe traumas, including hepatic trauma which exhibited the highest operative mortality in this data set, it may be necessary to establish specialized institutions, such as trauma centers and ACS centers, to a certain extent, and consolidate cases similar to practices in Western countries. 39
Enhancing the education of gastroenterological surgeons in the field of ACS and strengthening their collaboration with acute care surgeons could further accelerate the development of gastroenterological surgery. Notably, the Japanese ACS Society became an associate member of the NCD in 2021, suggesting the establishment of a cooperative environment in both clinical and research aspects.
Between 2013 and 2022, 98 research projects in the field of gastroenterological surgery that use big data from the NCD were approved and reported on a rolling basis in scholarly papers. Among them, 12 papers were published in 2022, covering topics such as high‐complexity esophageal 40 , 41 , 42 and pancreatic 43 , 44 cancer surgery, coronavirus disease 2019‐related issues, 45 , 46 and surgeon's sex‐related aspects, 47 , 48 which indicates a heightened interest in these areas.
Given that this is the first large‐scale study on the surgeon's sex in the field of gastroenterological surgery, an overview is provided here. One of the two studies compared the surgical experience available to surgeons of different sexes, while the other compared surgical outcomes based on the sex of gastroenterological surgeons. The first study found that female surgeons had less surgical experience than male surgeons in Japan, and this gap tended to widen with an increase in years of experience, especially for medium‐ and high‐difficulty procedures. 47 The second study found that female gastrointestinal surgeons were more frequently responsible for patients with comorbid conditions, although they performed fewer surgeries than their male counterparts. Despite these disadvantages, no significant differences were observed in the risk of surgical mortality between male and female surgeons. 48 Both studies yield important conclusions that suggest addressing these gender gaps could further advance the field of gastroenterological surgery.
In summary, we presented the short‐term outcomes of 2021 and the surgical trends of the decade based on the NCD, along with the latest research findings. It is evident that the NCD will continue to be a critical cornerstone for the future development of gastroenterological surgery.
AUTHOR CONTRIBUTIONS
Sunao Ito: Conceptualization; project administration; writing – original draft. Arata Takahashi: Data curation; investigation; methodology; resources; software. Hideki Ueno: Conceptualization; project administration; supervision; writing – review and editing. Shuji Takiguchi: Conceptualization; project administration; writing – original draft. Yoshiki Kajiwara: Conceptualization; data curation; formal analysis; project administration; writing – original draft; writing – review and editing. Yoshihiro Kakeji: Conceptualization; supervision; writing – review and editing. Susumu Eguchi: Conceptualization; supervision; writing – review and editing. Takanori Goi: Conceptualization; supervision; writing – review and editing. Akio Saiura: Conceptualization; supervision; writing – review and editing. Akira Sasaki: Conceptualization; supervision; writing – review and editing. Hiroya Takeuchi: Conceptualization; supervision; writing – review and editing. Chie Tanaka: Conceptualization; supervision; writing – review and editing. Masaji Hashimoto: Conceptualization; supervision; writing – review and editing. Naoki Hiki: Conceptualization; supervision; writing – review and editing. Akihiko Horiguchi: Conceptualization; supervision; writing – review and editing. Satoru Matsuda: Conceptualization; supervision; writing – review and editing. Tsunekazu Mizushima: Conceptualization; supervision; writing – review and editing. Hiroyuki Yamamoto: Conceptualization; data curation; formal analysis; investigation; methodology; resources; supervision; writing – review and editing. Yuko Kitagawa: Conceptualization; project administration; supervision; writing – review and editing. Ken Shirabe: Conceptualization; project administration; supervision; writing – review and editing.
CONFLICT OF INTEREST STATEMENT
Yuko Kitagawa is Editor‐in‐Chief and Hideki Ueno, Hiroya Takeuchi, Naoki Hiki, and Akihiko Horiguchi are Associate Editors of Annals of Gastroenterological Surgery. Shuji Takiguchi, Yoshihiro Kakeji, Susumu Eguchi, Takanori Goi, Akio Saiura, Chie Tanaka, Satoru Matsuda, Tsunekazu Mizushima, and Ken Shirabe are editorial board members of Annals of Gastroenterological Surgery. Arata Takahashi and Hiroyuki Yamamoto are affiliated with the Department of Healthcare Quality Assessment at the University of Tokyo that is a social collaboration department supported by grants from the National Clinical Database, Johnson & Johnson K.K., and Nipro Co and Intuitive Surgical Sàrl. Other authors have no conflicts of interest.
ETHICS STATEMENT
Approval of the research protocol by an Institutional Reviewer Board: N/A.
Informed Consent: N/A.
Registry and the Registration No. of the study/trial: N/A.
Animal Studies: N/A.
ACKNOWLEDGMENTS
The authors would like to thank all the medical staff, surgical clinical reviewers, and hospitals for their continued efforts in participating and entering the data for this NCD. The authors would also like to thank Mr. Keita Shimoakasho of the JSGS and Ms. Hitomi Okamoto of the NCD for their generous cooperation and providing important information for this article.
Ito S, Takahashi A, Ueno H, Takiguchi S, Kajiwara Y, Kakeji Y, et al. Annual report on National Clinical Database 2021 for gastroenterological surgery in Japan. Ann Gastroenterol Surg. 2025;9:32–59. 10.1002/ags3.12868
REFERENCES
- 1. Seto Y, Kakeji Y, Miyata H, Iwanaka T. National Clinical Database (NCD) in Japan for gastroenterological surgery: brief introduction. Ann Gastroenterol Surg. 2017;1(2):80–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kakeji Y, Yamamoto H, Ueno H, Eguchi S, Endo I, Sasaki A, et al. Development of gastroenterological surgery over the last decade in Japan: analysis of the National Clinical Database. Surg Today. 2021;51(2):187–193. [DOI] [PubMed] [Google Scholar]
- 3. National Clinical Database Home page. 2023 [cited 2023 Nov 1]. Available from: http://www.ncd.or.jp/
- 4. Gotoh M, Miyata H, Hashimoto H, Wakabayashi G, Konno H, Miyakawa S, et al. National Clinical Database feedback implementation for quality improvement of cancer treatment in Japan: from good to great through transparency. Surg Today. 2016;46(1):38–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ohkura Y, Miyata H, Konno H, Udagawa H, Ueno M, Shindoh J, et al. Development of a model predicting the risk of eight major postoperative complications after esophagectomy based on 10 826 cases in the Japan National Clinical Database. J Surg Oncol. 2020;121(2):313–321. [DOI] [PubMed] [Google Scholar]
- 6. Kunisaki C, Miyata H, Konno H, Saze Z, Hirahara N, Kikuchi H, et al. Modeling preoperative risk factors for potentially lethal morbidities using a nationwide Japanese web‐based database of patients undergoing distal gastrectomy for gastric cancer. Gastric Cancer. 2017;20(3):496–507. [DOI] [PubMed] [Google Scholar]
- 7. Kikuchi H, Miyata H, Konno H, Kamiya K, Tomotaki A, Gotoh M, et al. Development and external validation of preoperative risk models for operative morbidities after total gastrectomy using a Japanese web‐based nationwide registry. Gastric Cancer. 2017;20(6):987–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yoshida T, Miyata H, Konno H, Kumamaru H, Tangoku A, Furukita Y, et al. Risk assessment of morbidities after right hemicolectomy based on the National Clinical Database in Japan. Ann Gastroenterol Surg. 2018;2(3):220–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Watanabe T, Miyata H, Konno H, Kawai K, Ishihara S, Sunami E, et al. Prediction model for complications after low anterior resection based on data from 33,411 Japanese patients included in the National Clinical Database. Surgery. 2017;161(6):1597–1608. [DOI] [PubMed] [Google Scholar]
- 10. Yokoo H, Miyata H, Konno H, Taketomi A, Kakisaka T, Hirahara N, et al. Models predicting the risks of six life‐threatening morbidities and bile leakage in 14,970 hepatectomy patients registered in the National Clinical Database of Japan. Medicine (Baltimore). 2016;95(49):e5466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Aoki S, Miyata H, Konno H, Gotoh M, Motoi F, Kumamaru H, et al. Risk factors of serious postoperative complications after pancreaticoduodenectomy and risk calculators for predicting postoperative complications: a nationwide study of 17,564 patients in Japan. J Hepatobiliary Pancreat Sci. 2017;24(5):243–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Saze Z, Miyata H, Konno H, Gotoh M, Anazawa T, Tomotaki A, et al. Risk models of operative morbidities in 16,930 critically ill surgical patients based on a Japanese Nationwide database. Medicine (Baltimore). 2015;94(30):e1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Marubashi S, Ichihara N, Kakeji Y, Miyata H, Taketomi A, Egawa H, et al. “real‐time” risk models of postoperative morbidity and mortality for liver transplants. Ann Gastroenterol Surg. 2018;3(1):75–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Takeuchi H, Miyata H, Gotoh M, Kitagawa Y, Baba H, Kimura W, et al. A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web‐based database. Ann Surg. 2014;260(2):259–266. [DOI] [PubMed] [Google Scholar]
- 15. Kurita N, Miyata H, Gotoh M, Shimada M, Imura S, Kimura W, et al. Risk model for distal gastrectomy when treating gastric cancer on the basis of data from 33,917 Japanese patients collected using a nationwide web‐based data entry system. Ann Surg. 2015;262(2):295–303. [DOI] [PubMed] [Google Scholar]
- 16. Watanabe M, Miyata H, Gotoh M, Baba H, Kimura W, Tomita N, et al. Total gastrectomy risk model: data from 20,011 Japanese patients in a nationwide internet‐based database. Ann Surg. 2014;260(6):1034–1039. [DOI] [PubMed] [Google Scholar]
- 17. Kobayashi H, Miyata H, Gotoh M, Baba H, Kimura W, Kitagawa Y, et al. Risk model for right hemicolectomy based on 19,070 Japanese patients in the National Clinical Database. J Gastroenterol. 2014;49(6):1047–1055. [DOI] [PubMed] [Google Scholar]
- 18. Matsubara N, Miyata H, Gotoh M, Tomita N, Baba H, Kimura W, et al. Mortality after common rectal surgery in Japan: a study on low anterior resection from a newly established nationwide large‐scale clinical database. Dis Colon Rectum. 2014;57(9):1075–1081. [DOI] [PubMed] [Google Scholar]
- 19. Kenjo A, Miyata H, Gotoh M, Kitagawa Y, Shimada M, Baba H, et al. Risk stratification of 7,732 hepatectomy cases in 2011 from the National Clinical Database for Japan. J Am Coll Surg. 2014;218(3):412–422. [DOI] [PubMed] [Google Scholar]
- 20. Kimura W, Miyata H, Gotoh M, Hirai I, Kenjo A, Kitagawa Y, et al. A pancreaticoduodenectomy risk model derived from 8575 cases from a national single‐race population (Japanese) using a web‐based data entry system: the 30‐day and in‐hospital mortality rates for pancreaticoduodenectomy. Ann Surg. 2014;259(4):773–780. [DOI] [PubMed] [Google Scholar]
- 21. Nakagoe T, Miyata H, Gotoh M, Anazawa T, Baba H, Kimura W, et al. Surgical risk model for acute diffuse peritonitis based on a Japanese nationwide database: an initial report on the surgical and 30‐day mortality. Surg Today. 2015;45(10):1233–1243. [DOI] [PubMed] [Google Scholar]
- 22. Kakeji Y, Takahashi A, Udagawa H, Unno M, Endo I, Kunisaki C, et al. Surgical outcomes in gastroenterological surgery in Japan: report of National Clinical database 2011–2016. Ann Gastroenterol Surg. 2017;2(1):37–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hasegawa H, Takahashi A, Kakeji Y, Ueno H, Eguchi S, Endo I, et al. Surgical outcomes of gastroenterological surgery in Japan: report of the National Clinical Database 2011–2017. Ann Gastroenterol Surg. 2019;3(4):426–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kakeji Y, Takahashi A, Hasegawa H, Ueno H, Eguchi S, Endo I, et al. Surgical outcomes in gastroenterological surgery in Japan: report of the National Clinical Database 2011–2018. Ann Gastroenterol Surg. 2020;4(3):250–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Marubashi S, Takahashi A, Kakeji Y, Hasegawa H, Ueno H, Eguchi S, et al. Surgical outcomes in gastroenterological surgery in Japan: report of the National Clinical Database 2011‐2019. Ann Gastroenterol Surg. 2021;5(5):639–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kajiwara Y, Takahashi A, Ueno H, Kakeji Y, Hasegawa H, Eguchi S, et al. Annual report on National Clinical Database 2020 for gastroenterological surgery in Japan. Ann Gastroenterol Surg. 2023;7(3):367–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Masuda N, et al. Extended Clavien‐Dindo classification of surgical complications: Japan clinical oncology group postoperative complications criteria. Surg Today. 2016;46(6):668–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Okuyama A, Watabe M, Makoshi R, Takahashi H, Tsukada Y, Higashi T. Impact of the COVID‐19 pandemic on the diagnosis of cancer in Japan: analysis of hospital‐based cancer registries. Jpn J Clin Oncol. 2022;52(10):1215–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Arnold M, Park JY, Camargo MC, Lunet N, Forman D, Soerjomataram I. Is gastric cancer becoming a rare disease? A global assessment of predicted incidence trends to 2035. Gut. 2020;69(5):823–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Yamada M, Li M, Iino T. Pneumococcal vaccine coverage in Japan among patients with a history of splenectomy: results of a retrospective administrative database study. Vaccine. 2021;39(19):2692–2697. [DOI] [PubMed] [Google Scholar]
- 31. Statistics Bureau of Japan Home page. 2024. [cited 2024 Jan 31]. Available from: https://www.stat.go.jp/english/index.html
- 32. Ministry of Health, Labour and Welfare of Japan Home page. 2024. [cited 2024 Jan 31]. Available from: https://www.mhlw.go.jp/english/
- 33. Hofseth LJ, Hebert JR, Chanda A, Chen H, Love BL, Pena MM, et al. Early‐onset colorectal cancer: initial clues and current views. Nat Rev Gastroenterol Hepatol. 2020;17(6):352–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Konno H, Kamiya K, Kikuchi H, Miyata H, Hirahara N, Gotoh M, et al. Association between the participation of board‐certified surgeons in gastroenterological surgery and operative mortality after eight gastroenterological procedures. Surg Today. 2017;47(5):611–618. [DOI] [PubMed] [Google Scholar]
- 35. Arita J, Yamamoto H, Kokudo T, Hasegawa K, Miyata H, Toh Y, et al. Impact of board certification system and adherence to the clinical practice guidelines for liver cancer on post‐hepatectomy risk‐adjusted mortality rate in Japan: a questionnaire survey of departments registered with the National Clinical Database. J Hepatobiliary Pancreat Sci. 2021;28(10):801–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Endo I, Hirahara N, Miyata H, Yamamoto H, Matsuyama R, Kumamoto T, et al. Mortality, morbidity, and failure to rescue in hepatopancreatoduodenectomy: an analysis of patients registered in the National Clinical Database in Japan. J Hepatobiliary Pancreat Sci. 2021;28(4):305–316. [DOI] [PubMed] [Google Scholar]
- 37. Moore EE. Acute care surgery: the safety net hospital model. Surgery. 2007;141(3):297–298. [DOI] [PubMed] [Google Scholar]
- 38. Kutcher ME, Sperry JL, Rosengart MR, Mohan D, Hoffman MK, Neal MD, et al. Surgical rescue: the next pillar of acute care surgery. J Trauma Acute Care Surg. 2017;82(2):280–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Demetriades D, Martin M, Salim A, Rhee P, Brown C, Chan L. The effect of trauma center designation and trauma volume on outcome in specific severe injuries. Ann Surg. 2005;242(4):512–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Watanabe M, Toh Y, Ishihara R, Kono K, Matsubara H, Murakami K, et al. Comprehensive registry of esophageal cancer in Japan, 2014. Esophagus. 2022;19(1):1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Nakajima Y, Tachimori H, Miyawaki Y, Fujiwara N, Kawada K, Sato H, et al. A survey of the clinical outcomes of cervical esophageal carcinoma surgery focusing on the presence or absence of laryngectomy using the National Clinical Database in Japan. Esophagus. 2022;19(4):569–575. [DOI] [PubMed] [Google Scholar]
- 42. Okamura A, Yamamoto H, Watanabe M, Miyata H, Kanaji S, Kamiya K, et al. Association between preoperative HbA1c levels and complications after esophagectomy: analysis of 15,801 esophagectomies from the National Clinical Database in Japan. Ann Surg. 2022;276(5):e393–e399. [DOI] [PubMed] [Google Scholar]
- 43. Nakata K, Yamamoto H, Miyata H, Kakeji Y, Kitagawa Y, Nakamura M. Comparison of outcomes between laparoscopic and open pancreaticoduodenectomy without radical lymphadenectomy: results of coarsened exact matching analysis using national database systems. Asian J Endosc Surg. 2022;15(1):15–21. [DOI] [PubMed] [Google Scholar]
- 44. Uemura S, Endo H, Ichihara N, Miyata H, Maeda H, Hasegawa H, et al. Day of surgery and mortality after pancreatoduodenectomy: a retrospective analysis of 29 270 surgical cases of pancreatic head cancer from Japan. J Hepatobiliary Pancreat Sci. 2022;29(7):778–784. [DOI] [PubMed] [Google Scholar]
- 45. Ikeda N, Yamamoto H, Taketomi A, Hibi T, Ono M, Niikura N, et al. The impact of COVID‐19 on surgical procedures in Japan: analysis of data from the National Clinical Database. Surg Today. 2022;52(1):22–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Maeda H, Endo H, Yamamoto H, Miyata H, Munekage M, Taketomi A, et al. Effects of the COVID‐19 pandemic on gastroenterological surgeries in 2020: a study using the National Clinical Database of Japan. Ann Gastroenterol Surg. 2022;7(3):407–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kono E, Isozumi U, Nomura S, Okoshi K, Yamamoto H, Miyata H, et al. Surgical experience disparity between male and female surgeons in Japan. JAMA Surg. 2022;157(9):e222938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Okoshi K, Endo H, Nomura S, Kono E, Fujita Y, Yasufuku I, et al. Comparison of short term surgical outcomes of male and female gastrointestinal surgeons in Japan: retrospective cohort study. BMJ. 2022;378:e070568. [DOI] [PubMed] [Google Scholar]


