Abstract
Purpose:
To identify sleep dimensions (characteristics) that co-occur in premenopausal women. The second aim was to examine associations between multiple dimensions of sleep and a set of demographic, lifestyle, and health correlates. The overarching goal was to uncover patterns of poor-sleep correlates that might inform interventions to improve sleep health of women in this age group.
Methods:
The BioCycle Study included 259 healthy women aged 18–44y recruited between 2005 and 2007 from Western New York. Participants reported sleep data through daily diaries and questionnaires that were used to create five sleep health dimensions (duration, variability, timing, latency, and continuity). We used multivariate analysis – canonical correlation methods – to identify links among dimensions of sleep health and patterns of demographic, psychological, and occupational correlates.
Results:
Two distinct combinations of sleep dimensions were identified. The first - primarily determined by low variability in nightly sleep duration, low variability in bedtime (timing), greater nocturnal awakening, and less sleep onset latency – was distinguished from the second – primarily determined by sleep duration.
The first combination of sleep dimensions was associated with older age and higher parity, fewer depressive symptoms, and higher stress level. The second combination of sleep dimensions was associated with perception of longer sleep duration as optimal, lower parity, not engaging in shift work, older age, lower stress level, higher prevalence of depressive symptoms, and White race.
Conclusion:
Among premenopausal women, we demonstrated distinct patterns of sleep dimensions that co-occur and vary by demographic, health, and lifestyle correlates. These findings shed light on the correlates of sleep health vulnerabilities among young women.
Keywords: Sleep, Sleep health, Sleep variability, Insomnia, Bedtime, Women’s health
Introduction
Optimal sleep is vital for physical and mental health across the lifespan, while poor sleep is linked to cognitive dysfunction, obesity, chronic diseases and pain, motor vehicle accidents, and mortality.[1–7] Sleep disorders impact 50–70 million Americans at some point in their lives, [8] and play a major role in sleep health. However, beyond pathologies, sleep health is also influenced by biological needs and social factors that change along the lifespan. For example, sufficient sleep duration for school-age children ranges between 10 and 13 h per night, while adults need 7–8 h nightly.[9] Also decreasing with age is social jetlag, i.e., inconsistent sleep patterns between weekdays and weekends. [10,11] Sleep health is a multidimensional construct encompassing sleep quantity, continuity, efficiency, regularity, timing and quality.[12]
Sex differences in sleep health have been attributed to interactions between biological, environmental, social, and cultural factors.[13] Relative to men and across the lifespan, women report more sleep disturbances,[14–17] lower sleep quality and insufficient sleep.[18,19] However, despite apparent gender disparities in sleep health, women-focused sleep data are still limited. Reports in non-pregnant women during their childbearing years are scant, though they highlight their vulnerable sleep health across multiple dimensions.[19–21] Beyond ovarian hormones, sleep in young women is also influenced by mood disorders, which disproportionately burden women, relative to men.[17] A meta-analysis of 29 studies demonstrated that insomnia symptoms are significantly higher in women than men along the lifespan and across countries.[22] Moreover, women from racial and ethnic minority groups are more likely to experience inadequate sleep duration.[20]
Thus far, correlates of poor sleep have been reported for individual sleep dimensions. However, poor sleep may be multidimensional with concurrent disturbances. Yet, reports on the co-occurrence of poor-sleep dimensions in young women are rare.[23,24] As women may be susceptible to multiple sleep disturbances, we sought to: 1) examine distinct patterns of poor-sleep dimensions among premenopausal women and 2) identify associations between a set of demographic, lifestyle, and health correlates and multiple sleep dimensions among these women. Here, we examine simultaneously multiple potential correlates of poor sleep across several specific dimensions and assess for combinations of correlates that may co-occur. We consider a collection of five poor-sleep dimensions (lower mean sleep duration, variability in sleep duration, long sleep onset latency, bedtime variability, and nocturnal awakening) in relation to eight demographic, psychological, and occupational correlates.
Methods
Study population
The BioCycle Study included 259 healthy, regularly menstruating women aged 18–44 years[25] recruited between 2005 and 2007 from Western New York. All study participants provided written informed consent. Women were excluded if they used oral contraceptives within three months of enrollment, dietary supplements, or prescription medications. Pregnant women, those who breastfed less than six months before enrollment, women with a diagnosis of polycystic ovary syndrome, recent history of infections, chronic medical conditions, and women whose body mass index (BMI) at screening <18 or >35 kg/m2, were also excluded. The recruitment diagram of this study is shown in supplemental Figure 1. This study employed a micro-longitudinal design with intense measurements within a relatively short time. Women were followed along two menstrual cycles and provided biospecimens and questionnaire data at key reproductive time points: the second day of the menstrual cycle, mid- and late follicular phase, and early, mid-, and late luteal phase.[25] Sociodemographic and health information and lifestyle habits were collected through questionnaires and daily diaries.
Dimensions of sleep
Sleep data, obtained through daily diaries and questionnaires, were used to define five dimensions of poor sleep: lower mean sleep duration, variability in sleep duration, long sleep onset latency, variability in bedtime, and nocturnal awakening. Specifically, sleep duration and variability were computed from repeated sleep duration entries recorded in daily diaries, the gold standard tool for self-report sleep data.[26] Women reported their sleep duration along two menstrual cycles using the following question: “please write in the total number of hours and minutes you slept last night plus any time you napped today. For example, if you went to bed at 11pm last night and slept until 7am this morning and took a half-hour nap after lunch today, your response would be 8 h 30 min.” Diary data included 13,038 entries of sleep duration ranging between 16 and 86 entries across two menstrual cycles of 255 women, representing a 90 % completion rate. We excluded four women with insufficient sleep data in their diaries (<14 days of sleep duration entries).
Sleep items included in baseline questionnaires – administered at first clinic visit – were used to calculate bedtime variability, i.e., the difference between reported bedtime on weekdays (Sunday-Thursday) and weekends (Friday-Saturday). Information on two key insomnia symptoms, nocturnal awakening, and sleep onset latency, were collected from these two questions: 1) “On average, how do you sleep during the night? a) without waking up during the night, b) wake up once or twice during the night, c) wake up frequently during the night”; and 2) “what is the amount of time to fall asleep on weekdays and weekends?” (in minutes). Women were classified into two groups based on their reported nocturnal awakenings frequency – women with no nocturnal awakening, and those who reported at least one awakening per night.
Sociodemographic, lifestyle, and health correlates
The selection of potential correlates for dimensions of poor sleep was informed by the scientific literature. Specifically, we included demographic characteristics, such as age, race and ethnicity, and education level,[27,28] as well as parity, mood, and shift work.[29–31]
Race and ethnicity were self-reported by study participants using categories based on the US Office of Management and Budget’s Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity (American Indian, Asian Indian, Black, Chinese and other Asian, Hispanic, Pacific Islander, White, or Unspecified). Women reported their age, work status and schedules using the following question: “Have your jobs involved exposure to any of the following? Rotating shifts (defined as work schedules in which the time changes between days, evenings (between 4pm and midnight) and/or nights (between midnight and 8 a.m.))”. To calculate parity, we used the number of daughters and sons reported by participants. At first clinic visit, a validated instrument for depression screening, the Center for Epidemiologic Studies-Depression (CES-D), was administered to assess depressive symptoms,[32] and stress level was evaluated through the 14-item Perceived Stress Scale.[33] Finally, women reported their perception of the optimal sleep duration with the following question: “what do you consider an adequate or optimum number of hours of sleep?”.
Statistical analysis
We used linear moments (L-moments), a mathematical approach for characterization of probability distributions,[34] to estimate robust measures of woman-specific mean sleep duration and variability in sleep duration along two menstrual cycles. Equivalent to the mean absolute deviation, variability in sleep duration quantifies the spread of sleep duration entries below or above a woman’s habitual sleep duration. This measure captures characteristics of the sleep distribution beyond traditional averages and standard deviations.
Descriptive statistics were used to examine the distribution of sleep measures of all women. We evaluated the marginal relationships between sleep disturbances and sociodemographic, lifestyle, and health characteristics. Means and standard deviations were computed for continuous sleep measures (sleep duration, variability in sleep duration, and time to fall asleep). For binary sleep measures, i.e., wake up ≥1 time per night and bedtime variability ≥2 h, we calculated frequencies and proportions. Group differences were evaluated with Kruskal-Wallis and Chi-square tests for continuous and categorical sleep measures, respectively.
Pearson correlation coefficients were used to describe the pairwise association among sleep dimensions. To examine the relationships among a set of potential sociodemographic, health, and lifestyle correlates and multiple sleep dimensions simultaneously, we used principal component analysis (PCA) and canonical correlation analysis (CCA). PCA examines the correlations within the multiple dimensions of sleep. In contrast, CCA simultaneously examines associations between multiple sleep dimensions and a set of potential correlates. These relationships were evaluated using biplots, and by considering correlation between each measured sleep dimension or correlate and a composite identified through either PCA or CCA. One biplot represents a set of sleep dimensions while the other displays a set of potential sleep correlates. The configuration of arrows in both plots indicates relationships between the two sets of variables. We interpreted each PCA or CCA factor as defining a pattern of sleep dimensions or patterns of poor sleep correlates that co-occur as a composite measure. Each pattern is a linear combination (defined through estimated loadings) of directly measured variables with well-defined direction and scale. Following convention, loadings with magnitude exceeding 0.35 were used to interpret each factor.
Ethical approval
The original BioCycle Study was approved by the Health Sciences Institutional Review Board at the University at Buffalo, which served as the Institutional Review Board designated by the National Institutes of Health under a reliance agreement.
Results
Descriptive statistics of sleep dimensions
The mean sleep duration was 7.2 h, with a range of 4.2–10.6 h. More than a third of women reported insufficient sleep duration, defined as less than 7 h per night, by the American Academy of Sleep Medicine.[9] High variability in sleep duration was less common, as most women (82 %) reported consistent sleep duration, corresponding to less than one hour variation in sleep duration. Inconsistent bedtime, i.e., the difference of two or more hours between weekdays and weekends, was apparent among a third of women. Long sleep onset latency (≥30 min) and nocturnal awakening at least once during the night were reported by 24 % and 54 % of women, respectively. (Table 1)
Table 1.
Dimensions of Poor Sleep in Premenopausal Women: The Biocycle Study.
| Mean sleep duration, hours/night | |
|---|---|
| Range | 4.4, 10.6 |
| Mean (SD) | 7.2 (0.7) |
| Proportion <7 h (%) | 36 |
| Variability (dispersion) in sleep duration, hours/night | |
| Range | 0.02, 1.78 |
| Mean (Median) | 0.74 (0.70) |
| Proportion <1 h (%) | 82 |
| Variability in bedtime | |
| Range | 0.00, 7.8 |
| Mean (Median) | 1.5 (1.5) |
| Proportion <2 h (%) | 67 |
| Sleep-onset latency on weekdays, minutes (%) | |
| Range | 0, 90 |
| Mean (SD) | 16.7 (12.8) |
| Proportion ≥ 30 min (%) | 24 |
| Nocturnal awakenings (%) | |
| Never | 46 |
| ≥ 1 time/night | 54 |
Variability in Sleep duration corresponds to the spread of sleep duration entries below or above woman’s habitual sleep duration; Bedtime variability is defined as ≥2 h difference between weekday and weekend bedtime; Nocturnal awakening is defined as ≥1 awakening per night.
Mean sleep duration was lower and variability in sleep duration was higher among women who reported shift work and those who reported <7 h as optimal sleep duration.
Variability in sleep duration was apparent among younger women (18–22y) and women without children. Sleep onset latency was almost twice as long in women younger than 30y relative to women aged 40+y. Similarly, nocturnal awakenings were more frequent as age increased and among women with children. Black and Hispanic women, those with less than a college education, women with depressive symptoms, and those without children were more likely to report variability in bedtime. (Table 2)
Table 2.
Sociodemographic and lifestyle characteristics in relation to dimensions of poor sleep: The BioCycle Study (2005–2007).
| Sociodemographic and lifestyle characteristics | N (%) | Sleep duration mean (hrs) Mean ± SD | Variability in sleep duration (hrs) Mean ± SD | Sleep-onset latency (min) Mean ± SD | Nocturnal awakening n (%) | Bedtime variability n (%) |
|---|---|---|---|---|---|---|
| Overall | 257 | 7.2 ± 0.7 | 0.7 ± 0.3 | 16.7 ± 12.8 | 139 (54.1) | 86 (33.5) |
| Age | ||||||
| 18–22 years | 107 (41.6) | 7.2 ± 0.7 | 0.9 ± 0.3 | 18.4 ± 12.2 | 41 (38.3) | 56 (52.3) |
| 23–29 years | 67 (26.1) | 7.3 ± 0.9 | 0.7 ± 0.3 | 18.5 ± 14.3 | 35 (52.2) | 17 (25.4) |
| 30–39 years | 51 (19.8) | 7.4 ± 0.6 | 0.6 ± 0.2 | 14.9 ± 13.3 | 39 (76.5) | 11 (21.6) |
| 40+ years | 32 (12.5) | 7.1 ± 0.5 | 0.5 ± 0.2 | 9.9 ± 7.0 | 24 (75) | 2 (6.2) |
| P value | 0.160 | <0.001 | 0.001 | <0.001 | <0.001 | |
| Race and Ethnicity | ||||||
| Asian | 26 (10.1) | 7.3 ± 0.8 | 0.8 ± 0.4 | 19.5 ± 10.8 | 12 (46.2) | 11 (42.3) |
| Asian-Indian | 13 (5.1) | 7.1 ± 1 | 0.7 ± 0.3 | 19.6 ± 9.4 | 6 (46.2) | 4 (30.8) |
| Black | 47 (18.3) | 7.1 ± 0.9 | 0.8 ± 0.3 | 16.8 ± 13.3 | 26 (55.3) | 21 (44.7) |
| Hispanic | 11 (4.3) | 7.1 ± 0.9 | 0.7 ± 0.4 | 16.3 ± 8.5 | 7 (63.6) | 4 (36.4) |
| White | 151 (58.8) | 7.3 ± 0.6 | 0.7 ± 0.3 | 15.9 ± 13.4 | 84 (55.6) | 45 (29.8) |
| Other | 9 (3.5) | 7.1 ± 1 | 0.6 ± 0.2 | 18.3 ± 13.6 | 4 (44.4) | 1 (11.1) |
| P value | 0.224 | 0.283 | 0.323 | <0.001 | <0.001 | |
| Education | ||||||
| High school or less | 32 (12.5) | 7.1 ± 0.7 | 0.7 ± 0.2 | 14.6 ± 8.3 | 17 (53.1) | 13 (40.6) |
| Some college | 121 (47.1) | 7.2 ± 0.7 | 0.8 ± 0.3 | 17.8 ± 12.8 | 57 (47.1) | 54 (44.6) |
| College | 76 (29.6) | 7.4 ± 0.8 | 0.7 ± 0.3 | 15.8 ± 11.7 | 50 (65.8) | 15 (19.7) |
| Above College | 28 (10.9) | 7.3 ± 0.7 | 0.7 ± 0.3 | 16.9 ± 18.7 | 15 (53.6) | 4 (14.3) |
| P value | 0.252 | 0.001 | 0.552 | 0.020 | <0.001 | |
| Shift work | ||||||
| Yes | 153 (63.8) | 7.1 ± 0.7 | 0.8 ± 0.3 | 16.6 ± 12.6 | 73 (47.7) | 55 (35.9) |
| No | 87 (36.2) | 7.5 ± 0.7 | 0.7 ± 0.3 | 16.3 ± 13.5 | 55 (63.2) | 23 (26.4) |
| P value | <0.001 | 0.007 | 0.922 | 0.051 | 0.240 | |
| Sleep perception | ||||||
| <7 | 26 (10.2) | 6.6 ± 0.7 | 0.9 ± 0.3 | 18.4 ± 13.6 | 18 (13.9) | 8 (30.8) |
| ≥7 | 230 (89.8) | 7.3 ± 0.7 | 0.7 ± 0.3 | 16.5 ± 12.7 | 14 (11.1) | 52 (23.1) |
| P value | <0.001 | 0.037 | 0.542 | 0.141 | 0.647 | |
| Stress Score | ||||||
| Low ≤22 | 165 (64.5) | 7.3 ± 0.7 | 0.7 ± 0.3 | 16.8 ± 13.5 | 86 (52.1) | 56 (33.9) |
| Moderate/high >22 | 91 (35.5) | 7.1 ± 0.8 | 0.8 ± 0.3 | 16.6 ± 11.4 | 53 (58.2) | 30 (33.0) |
| P value | 0.231 | 0.431 | 0.731 | 0.261 | 0.401 | |
| Depression Score | ||||||
| <16 | 229 (92.3) | 7.3 ± 0.7 | 0.7 ± 0.3 | 16.6 ± 12.7 | 126 (55.0) | 74 (32.3) |
| ≥16 | 19 (7.7) | 7 ± 0.7 | 0.8 ± 0.4 | 19.7 ± 15.6 | 9 (47.4) | 11 (57.9) |
| P value | 0.118 | 0.736 | 0.499 | 0.003 | <0.001 | |
| Parity | ||||||
| 0 | 187 (74.5) | 7.3 ± 0.8 | 0.8 ± 0.3 | 18.1 ± 12.8 | 89 (47.6) | 75 (40.1) |
| ≥1 | 64 (25.5) | 7.1 ± 0.6 | 0.5 ± 0.2 | 12.3 ± 11.9 | 47 (73.4) | 8 (12.5) |
| P value | 0.315 | <0.001 | <0.001 | <0.001 | <0.001 | |
P values are from Kruskal Wallis for continuous variables and Chi-square tests for categorical variables; sleep perception refers to optimal sleep duration as reported by participants; Stress score is calculated from the 14-item Perceived Stress Scale instrument; Depression Score based on the CES-D tool; Variability in Sleep duration corresponds to the spread of sleep duration entries below or above woman’s habitual sleep duration; Bedtime variability is defined as ≥2 h difference between weekday and weekend bedtime; Nocturnal awakening is defined as ≥1 awakening per night; Other race and ethnicity refers to American Indian, Asian Indian, Chinese or other Asian, Pacific Islander or unspecified.
Associations within the multiple sleep dimensions
Among sleep dimensions, we found statistically significant associations between variability in bedtime and variability in sleep duration (r = 0.40), between long sleep onset latency and nocturnal awakening (r = 0.18), and between long sleep onset latency and sleep duration (r = 0.15). Moreover, associations were apparent between lower bedtime variability and frequent nocturnal awakening (r=−0.21), see Table S1. We identified two factors defining the pattern of sleep dimensions, which explain 55 % of the total variance observed among sleep dimensions. The first factor is associated with higher variability in sleep duration, higher bedtime variability, shorter mean sleep duration and less frequent nocturnal awakening. The second factor is mainly driven by higher sleep onset latency, frequent nocturnal awakening, and higher variability in sleep duration. (Fig. 1, Table S2).
Fig. 1.
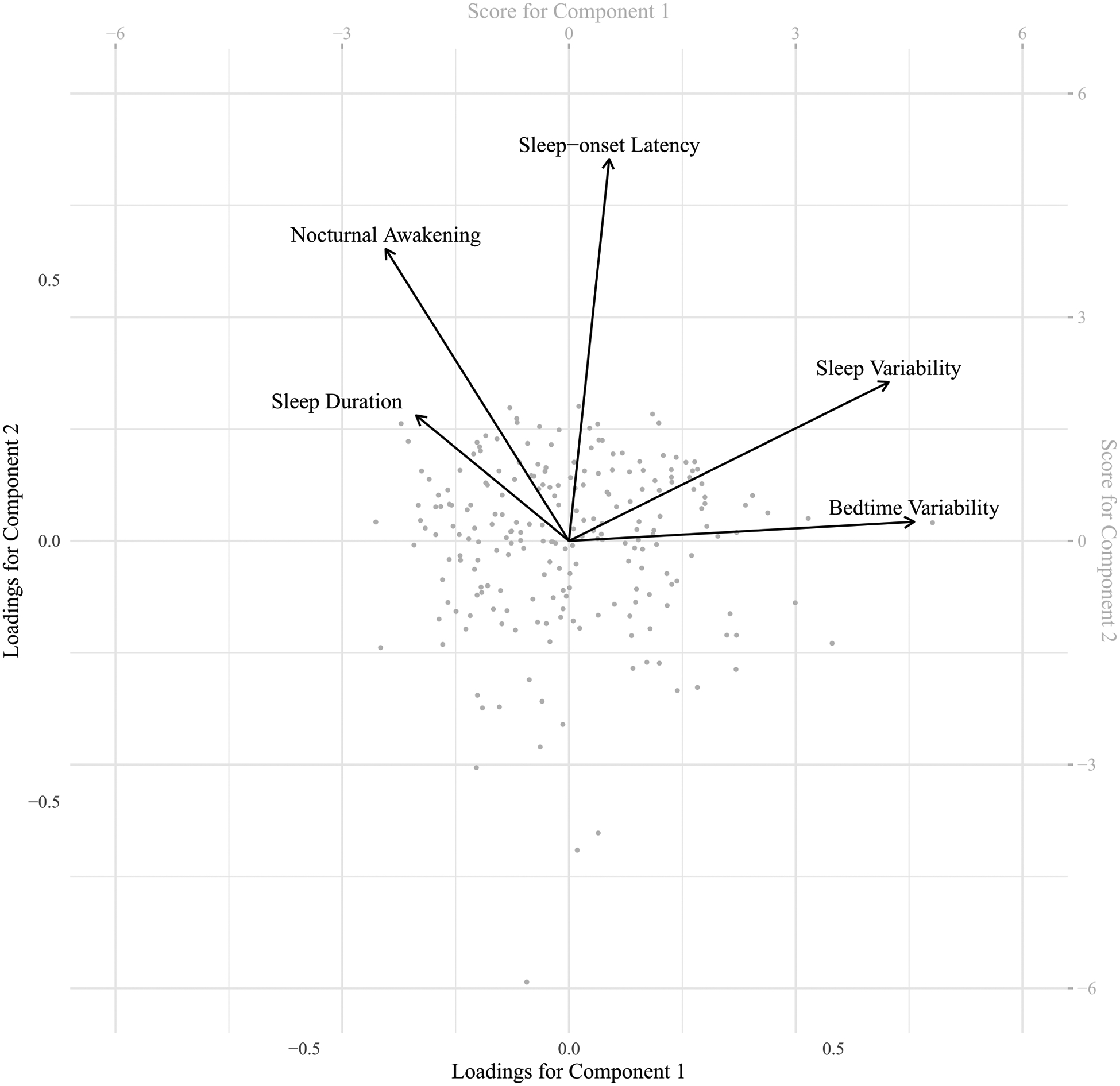
Biplot showing co-occurrence of sleep dimensions based on principal component analysis; arrows indicate variable loading for each component, points correspond to person-specific scores.
Simultaneous associations among multiple sleep dimensions and potential correlates
Examinations of potential relationships between sleep dimensions and demographic, lifestyle, and health correlates suggested associations between age and sleep onset latency (r=−0.23), between age and nocturnal awakening (r = 0.33), between age and bedtime variability (r=−0.35), and between age and sleep variability (r=−0.38). Parity was also found to be associated with all sleep dimensions except sleep duration. More shift work was observed to be associated with higher sleep variability (0.20) and lower sleep duration (−0.25). Furthermore, sleep perception corresponding to optimal sleep duration was associated with higher mean sleep duration (Table S3).
We then evaluated linear combinations within two sets of variables that are mutually correlated. Here, the first set of variables is dimensions of sleep, and the second set includes demographic, lifestyle, and health correlates. Two independent pairs of correlated factors were found (p < 0.05). The sleep domain is distinguished by one factor reflecting low variability in nightly sleep duration, low bedtime variability, frequent nocturnal awakening, and low sleep onset latency (Fig. 2, Table S5). This sleep domain factor is associated with a combination of correlates including older age and parity, lower prevalence of depression, and higher stress (r = 0.6, p < 0.01, Table S4). The second sleep domain factor is primarily determined by mean sleep duration and is associated with greater perception of optimal sleep duration, less parity, less participation in shift work, older age, lower stress, more depression, and White race (r = 0.45, p value<0.01, Fig. 2, Table S5).
Fig. 2.
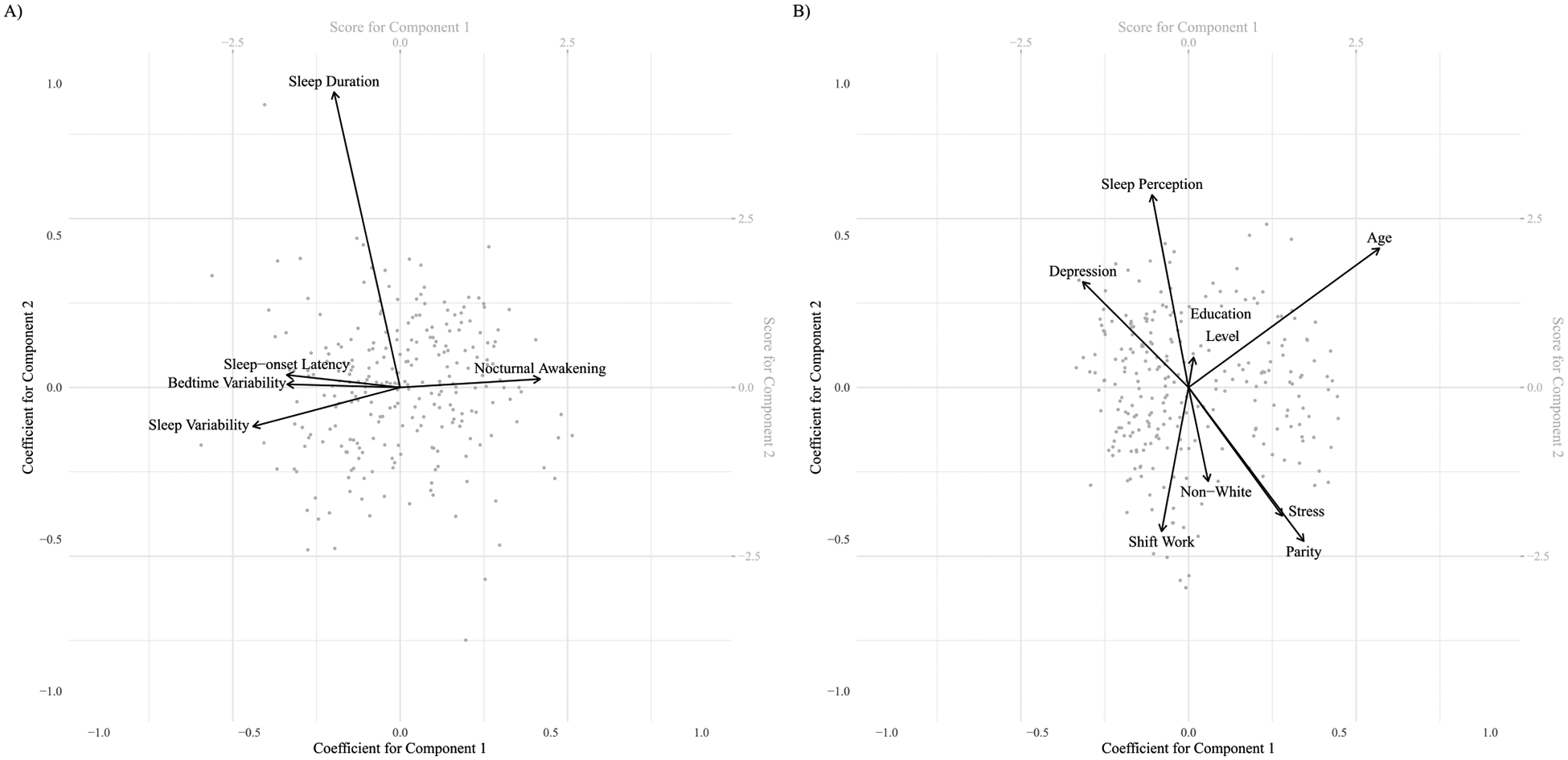
Biplot showing associations between sleep dimensions (2A) and their correlates (2B) based on canonical correlation analysis; arrows indicate variable loading for each component, points correspond to person-specific scores.
Discussion
In a cohort of premenopausal women aged 18–44y, this study examines correlations between multidimensionality of poor sleep and a set of demographic, lifestyle, and health correlates. Two distinct patterns of correlations between sleep dimensions and correlates were identified. The first distinguished women with frequent nocturnal awakenings, consistent sleep duration and bedtime, and short sleep onset latency. These women tended to be older, having more children, with higher stress levels, but fewer depressive symptoms. A second independent correlation pattern distinguished women with longer sleep duration and was apparent among older, White women with less children, who did not reported shiftwork, had lower stress levels, but more depressive symptoms, and who perceived longer sleep as an optimal sleep duration. These findings highlight the need for distinct strategies to improve sleep health that account for concurrent sleep dimensions according to relevant demographic characteristics.
Among premenopausal women, we found a high prevalence (54 %) of nocturnal awakening, while insufficient sleep duration (<7 h) and variability in weeknight/weekend bedtime (≥2 h) was reported by a third of these women. Our findings highlight the prevalence of multiple dimensions of poor sleep among reproductive-age women. Specifically, we found that young women may experience trouble falling asleep and higher variability in sleep duration and timing, while older women may be more vulnerable to nocturnal awakening. The prevalence and frequency of age-specific nocturnal awakening were evaluated previously in a representative survey of >8900 US adults from Texas, New York and California. Survey participants were interviewed by phone and provided data on their overall health, sleep health and habits. Detailed assessment of nocturnal awakenings included the frequency per night and per week, as well as the reason for the awakening and the duration of each episode. This survey found that frequent nocturnal awakening was positively associated with age and varied by sex, as women reported more frequent nocturnal awakening than men.[35] Moreover, a systematic review of the literature examined correlates of variability in sleep and wake times among adults, associated higher variability in sleep timing with younger age, non-White race and ethnicity, and poor mood. [36] These findings were consistent with the high variability in sleep duration we observed among younger, non-White women.
A high prevalence of sleep disturbances among women is common along their lifespans and has been observed in small and large samples. For example, a large study with young women and men aged 17–30y found that most participants reported at least one sleep disturbance occurring occasionally or frequently, i.e., nocturnal awakening (37 %), and delayed sleep onset (51 %). Furthermore, sex-specific analysis suggested higher frequency of nocturnal awakening and longer sleep onset latency among women in comparison to men.[37] Other studies supported the high burden of poor sleep health in young women, suggesting 40 % and 34 % prevalence of insufficient sleep duration and insomnia symptoms, respectively.[38,39] A high burden of insomnia on women was also shown in a study with 50,000 women and men who attended colleges and universities in Norway. Specifically, this study found that the prevalence of insomnia among women was higher in comparison to men, 34 % and 22 %, respectively.[38] A similar study among 1741 students who were randomly selected from a US-based university confirmed the higher incidence of chronic insomnia among women than men, 13 % and 6 %, respectively and correlated insomnia with age younger than <35y, non-White race and ethnicity, poor sleep and poor mood.[39]
Links between demographic, health, and lifestyle characteristics and sleep disturbances in young women are limited, as most studies focused on pregnant or peri- and post-menopausal women. Nonetheless, our findings were congruent with current evidence. For example, a large survey of >9700 reproductive-age women from Canada found insufficient sleep duration to be correlated with race and ethnicity, higher parity, living in urban areas, and smoking. Low sleep quality was linked to racial and ethnic minorities, lower education attainment, poor mood, living in urban areas and unhealthy diet.[20] Risk factors of sleep health among reproductive-age women were also examined by a recent review that linked a high prevalence of poor sleep quality to women from racial and ethnic minorities, those with low income, living in an urban settings, and mothers to young children. Correlations between poor sleep quality, stress and mood disorders among all age groups were also noted. [21]
Sex-specific disparities in sleep health have been consistently reported among women and men from racial and ethnic minority groups, such that non-White individuals experience higher prevalence of insufficient sleep duration, variability in sleep and nocturnal awakenings compared with White adults.[40–42] Similarly, our data suggest a higher burden of sleep disturbances among non-White women, including nocturnal awakenings and higher bedtime variability. These findings are attributed to differential exposures to social and environmental of sleep health among racial and ethnic groups.[42] Interestingly, women who perceived a higher number of hours as an optimal sleep duration reported longer mean sleep duration than those with misperceived sufficient sleep duration.
During their childbearing years, many young women endure psychosocial challenges and stressors as they pursue higher education, join the workforce and build their families.[21,43] This balancing act has a negative influence on the sleep health of women across racial and ethnic groups.[44–46] Support for the poor sleep women endure is provided by global cross-sectional studies reporting a significant prevalence of poor sleep that impact up to 40 % of women during the childbearing years. [20,47,48] A Canadian health survey among women aged 18–44y that examined demographic and health correlates of sleep duration, identified non-White race and ethnicity, parity, urbanicity, and smoking as correlates of short sleep duration. [20] Data from the National Health and Nutrition Examination Survey found some disparities in sleep health among women aged 15–44y from different racial and ethnic background who were more likely to report shorter sleep duration, but less likely to report trouble sleeping.[47] These findings highlight the multidimensionality of sleep health and warrant attention to potential sleep disparities among young women with distinct socio-demographic and health profiles. Sleep disturbances have been consistently associated with poor mental health. As expected, our data indicated that women with low variability in both sleep duration and in bedtime and shorter sleep onset latency reported fewer depressive symptoms, but surprisingly, they also reported higher stress scores.[48,49] Potential explanations to the reported higher stress could be related to family and work responsibilities, [50] as these women were likely to have a higher number of children and engage in shift work.
The present study has several strengths. First, including a diverse sample of women with a wide array of sociodemographic and lifestyle characteristics allows the identification of distinct patterns correlates of poor sleep. Second, it captures multiple dimensions of poor sleep among women during their childbearing years, an understudied population. Third, variability in sleep duration was assessed along two menstrual cycles, which accounted for changes in sleep associated with hormonal changes and reproductive function.[51] Finally, we utilized canonical correlation analysis to find linear combinations within two sets of variables that are mutually correlated. This powerful statistical approach allowed us to assess correlations between two sets of variables simultaneously: the first set was demographic, health, and lifestyle correlates, with a second set of multiple dimensions of poor sleep.
However, some limitations should be noted. While sleep duration and variability in sleep duration were assessed with repeated entries in sleep diaries, the gold standard of self-reported sleep duration,[26] other sleep data were cross-sectionally reported. This comparison of poor sleep correlates and multiple dimensions of poor sleep was performed without ascertainment that the former preceded the latter, meaning that despite the 60-day sampling period, the study was essentially cross-sectional. Therefore, identification of associations cannot confirm cause-and-effect relationships. The question about shift work refers to any prior exposure to work during the night or to rotating shifts which could represent current or past engagement in irregular work schedules. We acknowledge that employment status could be associated with sleep patterns, however, this study focused on night and rotating shift work as the primary employment-related factors given their direct impact on circadian rhythms and sleep patterns. Moreover, most women in this study are college students and 74 % of all women are either unemployed or employed part time. The sample was limited to 257 reproductive age and relatively healthy women with complete data (among 449 who were initially screened, 318 eligible and 276 enrolled) who lived in Western New York. Therefore, generalization of the findings to the many women who do have significant medical comorbidities, or who live in other regions, may have to await studies of larger samples over broader geographic distributions. Nonetheless, these data provide some initial insight into several dimensions of poor sleep and their potential correlates, within an important, understudied demographic, namely women of reproductive age, as opposed to other stages of life that have achieved more attention in research published to this point.
Conclusions
This study identified two patterns of sleep dimensions and their demographic, health, and lifestyle correlates among reproductive-age women. These data suggest that along the reproductive-age spectrum, younger women may experience trouble falling asleep and higher variability in sleep duration and sleep timing, while older women may be vulnerable to nocturnal awakening. Distinct strategies to improve sleep health among reproductive-age women should account for concurrent dimensions of poor sleep according to relevant demographic characteristics.
Supplementary Material
Funding
Dr. Dunietz was supported by a Mentored Research Scientist Development Award from the National Heart, Lung, and Blood Institute (K01 HL144914).
This work was partially supported by the Intramural Research Program of the National Institutes of Health (authors EFS, SLM). The BioCycle Study was funded under the following Eunice Kennedy Shriver National Institute of Child Health and Human Development contracts: HHSN275200403394C HHSN275201100002I, and Task 1 HHSN27500001.
Footnotes
CRediT authorship contribution statement
Xinrui Wu: Writing – review & editing, Writing – original draft, Formal analysis. Galit Levi Dunietz: Writing – review & editing, Writing – original draft, Supervision, Funding acquisition, Conceptualization. Kerby Shedden: Writing – review & editing, Supervision, Methodology, Conceptualization. Ronald D. Chervin: Conceptualization, Supervision, Writing – review & editing. Erica C. Jansen: Conceptualization, Formal analysis, Writing – review & editing. Xiru Lyu: Formal analysis. Louise M. O’Brien: Supervision, Writing – review & editing. Ana Baylin: Writing – review & editing, Supervision. Jean Wactawski-Wende: Writing – review & editing, Resources, Methodology, Data curation. Enrique F. Schisterman: Resources, Methodology, Data curation, Writing – review & editing. Sunni L. Mumford: Resources, Methodology, Data curation, Writing – review & editing.
Declaration of competing interest
none.
Supplementary materials
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.sleepe.2024.100093.
References
- [1].Gottlieb DJ, Ellenbogen JM, Bianchi MT, Czeisler CA. Sleep deficiency and motor vehicle crash risk in the general population: a prospective cohort study. BMC Med Mar 20 2018;16(1):44. 10.1186/s12916-018-1025-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Malhotra A, Loscalzo J. Sleep and cardiovascular disease: an overview. Prog Cardiovasc Dis Jan-Feb 2009;51(4):279–84. 10.1016/j.pcad.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Whibley D, Guyer HM, Swanson LM, Braley TJ, Kratz AL, Dunietz GL Sleep disturbance as a moderator of the association between physical activity and later pain onset among American adults aged 50 and over: evidence from the Health and Retirement Study. BMJ Open. Jun 7 2020;10(6):e036219. doi: 10.1136/bmjopen-2019-036219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Jansen EC, Dunietz GL, Matos-Moreno A, Solano M, Lazcano-Ponce E, Sánchez-Zamorano LM Bedtimes and blood pressure: a prospective cohort study of Mexican adolescents. Am J Hypertens. Mar 13 2020;33(3):269–277. doi : 10.1093/ajh/hpz191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res 2009;18(2):148–58. [DOI] [PubMed] [Google Scholar]
- [6].Marshall NS, Wong KK, Cullen SR, Knuiman MW, Grunstein RR. Sleep apnea and 20-year follow-up for all-cause mortality, stroke, and cancer incidence and mortality in the Busselton Health Study cohort. J. Clin. Sleep Med 2014;10(4):355–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Jansen EC, Dunietz GL, Chervin RD, et al. Adiposity in adolescents: the interplay of sleep duration and sleep variability. J Pediatr 2018;203:309–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Institute of Medicine (US) Committee on Sleep Medicine and Research. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Colten HR, Altevogt BM, editors. Washington (DC): National Academies Press (US); 2006. [PubMed] [Google Scholar]
- [9].Hirshkowitz M, Whiton K, Albert SM, et al. National sleep foundation’s sleep time duration recommendations: methodology and results summary. Sleep Heal 2015;1(1):40–3. [DOI] [PubMed] [Google Scholar]
- [10].Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol Int 2006;23(1–2):497–509. 10.1080/07420520500545979. [DOI] [PubMed] [Google Scholar]
- [11].Roenneberg T, Wirz-Justice A, Merrow M. Life between clocks: daily temporal patterns of human chronotypes. J Biol Rhythms Feb 2003;18(1):80–90. 10.1177/0748730402239679. [DOI] [PubMed] [Google Scholar]
- [12].Buysse DJ. Multidimensional sleep health: a conceptual overview. Innov Aging 2018. Nov 11;2(Suppl 1):595. 10.1093/geroni/igy023.2210. eCollection 2018 Nov. [DOI] [Google Scholar]
- [13].Mallampalli MP, Carter CL. Exploring sex and gender differences in sleep health: a Society for Women’s Health Research Report. J Womens Health (Larchmt) Jul 2014;23(7):553–62. 10.1089/jwh.2014.4816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Suh S, Cho N, Zhang J. Sex differences in insomnia: from epidemiology and etiology to intervention. Curr Psychiatry Rep Aug 9 2018;20(9):69. 10.1007/s11920-018-0940-9. [DOI] [PubMed] [Google Scholar]
- [15].Guidozzi F Gender differences in sleep in older men and women. Climacteric Oct 2015;18(5):715–21. 10.3109/13697137.2015.1042451. [DOI] [PubMed] [Google Scholar]
- [16].Galland BC, Gray AR, Penno J, Smith C, Lobb C, Taylor RW. Gender differences in sleep hygiene practices and sleep quality in New Zealand adolescents aged 15 to 17 years. Sleep Heal Apr 2017;3(2):77–83. 10.1016/j.sleh.2017.02.001. [DOI] [PubMed] [Google Scholar]
- [17].Pengo MF, Won CH, Bourjeily G. Sleep in women across the life span. Chest Jul 2018;154(1):196–206. 10.1016/j.chest.2018.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Li L, Nakamura T, Hayano J, Yamamoto Y. Age and gender differences in objective sleep properties using large-scale body acceleration data in a Japanese population. Sci Rep May 11 2021,;11(1):9970. 10.1038/s41598-021-89341-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Jonasdottir SS, Minor K, Lehmann S. Gender differences in nighttime sleep patterns and variability across the adult lifespan: a global-scale wearables study. Sleep 2020;44(2). 10.1093/sleep/zsaa169. [DOI] [PubMed] [Google Scholar]
- [20].Vézina-Im L-A, Lebel A, Gagnon P, Nicklas TA, Baranowski T. Individual correlates of sleep among childbearing age women in Canada. Behav Sleep Med 2019;17(5): 634–45. 10.1080/15402002.2018.1435547. 2019/09/03. [DOI] [PubMed] [Google Scholar]
- [21].Redeker NS. Sleep health in women of childbearing age. J Womens Health Mar 2020;29(3):430–4. 10.1089/jwh.2020.8349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Zhang B, Wing YK. Sex differences in insomnia: a meta-analysis. Sleep Jan 2006;29(1):85–93. 10.1093/sleep/29.1.85. [DOI] [PubMed] [Google Scholar]
- [23].Dunietz GL, Shedden K, Michels KA, et al. Variability in sleep duration and biomarkers of cardiovascular disease across the menstrual cycle. Am J Epidemiol Mar 16 2023. 10.1093/aje/kwad060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Dunietz GL, Shedden K, Lyu X, et al. Patterns of sleep duration and metabolic biomarkers across the menstrual cycle. J Clin Endocrinol Metab Mar 26 2024. 10.1210/clinem/dgae191. [DOI] [PubMed] [Google Scholar]
- [25].Wactawski-Wende J, Schisterman EF, Hovey KM, et al. BioCycle study: design of the longitudinal study of the oxidative stress and hormone variation during the menstrual cycle. Paediatr Perinat Epidemiol Mar 2009;23(2):171–84. 10.1111/j.1365-3016.2008.00985.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Mallinson DC, Kamenetsky ME, Hagen EW, Peppard PE. Subjective sleep measurement: comparing sleep diary to questionnaire. Nat Sci Sleep 2019;11:197–206. 10.2147/nss.S217867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Billings ME, Cohen RT, Baldwin CM, et al. Disparities in sleep health and potential intervention models: a focused review. Chest 2021;159(3):1232–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Madrid-Valero JJ, Martínez-Selva JM, BRd Couto, Sánchez-Romera JF, Ordoñana JR. Age and gender effects on the prevalence of poor sleep quality in the adult population. Gaceta sanitaria 2017;31:18–22. [DOI] [PubMed] [Google Scholar]
- [29].Härdelin G, Holding BC, Reess T, Geranmayeh A, Axelsson J, Sundelin T. Do mothers have worse sleep than fathers? Sleep imbalance, parental stress, and relationship satisfaction in working parents. Nat Sci Sleep 2021;13:1955–66. 10.2147/nss.S323991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Toffol E, Kalleinen N, Urrila AS, et al. The relationship between mood and sleep in different female reproductive states. BMC Psych 2014;14(1):177. 10.1186/1471-244X-14-177. 2014/06/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Monk TH, Buysse DJ, Billy BD, et al. Shiftworkers report worse sleep than day workers, even in retirement. J Sleep Res 2013;22(2):201–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1(3):385–401. [Google Scholar]
- [33].Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983:385–96. [PubMed] [Google Scholar]
- [34].Hosking JR. L-moments: analysis and estimation of distributions using linear combinations of order statistics. J Royal Statist Soc Series B 1990;52(1):105–24. [Google Scholar]
- [35].Ohayon MM. Nocturnal awakenings and comorbid disorders in the American general population. J Psychiatr Res 2008;43(1):48–54. 10.1016/j.jpsychires.2008.02.001. 2008/11/01/. [DOI] [PubMed] [Google Scholar]
- [36].Bei B, Wiley JF, Trinder J, Manber R. Beyond the mean: a systematic review on the correlates of daily intraindividual variability of sleep/wake patterns. Sleep Med Rev 2016;28:108–24. 10.1016/j.smrv.2015.06.003. 2016/08/01/. [DOI] [PubMed] [Google Scholar]
- [37].Coren S The prevalence of self-reported sleep disturbances in young adults. Int J Neurosci 1994;79(1–2):67–73. [DOI] [PubMed] [Google Scholar]
- [38].Sivertsen B, Vedaa Ø, Harvey AG, et al. Sleep patterns and insomnia in young adults: a national survey of Norwegian university students. J Sleep Res Apr 2019;28(2):e12790. 10.1111/jsr.12790. [DOI] [PubMed] [Google Scholar]
- [39].Singareddy R, Vgontzas AN, Fernandez-Mendoza J, et al. Risk factors for incident chronic insomnia: a general population prospective study. Sleep Med Apr 2012;13(4):346–53. 10.1016/j.sleep.2011.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Caraballo C, Mahajan S, Valero-Elizondo J, et al. Evaluation of temporal trends in racial and ethnic disparities in sleep duration among US adults, 2004–2018. JAMA Netw Open 2022;5(4). 10.1001/jamanetworkopen.2022.6385. e226385–e226385%J JAMA Network Open. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Jackson CL, Powell-Wiley TM, Gaston SA, Andrews MR, Tamura K, Ramos A. Racial/ethnic disparities in sleep health and potential interventions among women in the United States. J Womens Health Mar 2020;29(3):435–42. 10.1089/jwh.2020.8329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Johnson DA, Jackson CL, Williams NJ, Alcántara C. Are sleep patterns influenced by race/ethnicity - a marker of relative advantage or disadvantage? Evidence to date. Nat Sci Sleep 2019;11:79–95. 10.2147/nss.S169312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Sudha J, Karthikeyan P. Work life balance of women employee: a literature review. Int J Manage Res Rev 2014;4(8):797. [Google Scholar]
- [44].Johnson DA, Lisabeth L, Lewis TT, et al. The contribution of psychosocial stressors to sleep among African Americans in the Jackson Heart Study. Sleep 2016;39(7):1411–9. 10.5665/sleep.5974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Furuichi W, Shimura A, Miyama H, et al. Effects of job stressors, stress response, and sleep disturbance on presenteeism in office workers. Neuropsychiatr Dis Treat 2020:1827–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Zambrano DN, Mindell JA, Reyes NR, Hart CN, Herring SJ. It’s Not All About My Baby’s Sleep”: a qualitative study of factors influencing low-income african american mothers’ sleep quality. Behav Sleep Med 2016;14(5):489–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Amyx M, Xiong X, Xie Y, Buekens P. Racial/ethnic differences in sleep disorders and reporting of trouble sleeping among women of childbearing age in the United States. Matern Child Health J Feb 2017;21(2):306–14. 10.1007/s10995-016-2115-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Barsha RAA, Hossain MB. Peer reviewed: trouble sleeping and depression among US women aged 20 to 30 Years. Prev Chronic Dis 2020:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Sun W, Cheung FTW, Chan NY, et al. The impacts of intra-individual daily sleep variability on daytime functioning and sleep architecture in healthy young adults: an experimental study. J Sleep Res May 2024;33(3):e13967. 10.1111/jsr.13967. [DOI] [PubMed] [Google Scholar]
- [50].Sumra MK, Schillaci MA. Stress and the multiple-role woman: taking a closer look at the “Superwoman. PLoS ONE 2015;10(3):e0120952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Michels KA, Mendola P, Schliep KC, et al. The influences of sleep duration, chronotype, and nightwork on the ovarian cycle. Chronobiol Int 2020;37(2): 260–71. 10.1080/07420528.2019.1694938. 2020/02/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


