Abstract
Background:
Hysterectomy is one of the most common surgical procedures performed in the United States and most are now being performed in a minimally invasive approach. Electrosurgery and vessel sealing devices are needed in order to provide hemostasis and vascular coaptation; however, there is no guiding evidence and limited recommendations for the use of the currently available devices for laparoscopic hysterectomy. The purpose of this study is to provide a systematic review of electrosurgical devices used in benign hysterectomy and perform a meta-analysis to find the overall effect of various outcomes.
Database:
A systematic review was performed by searching the literature using MEDLINE, Embase, Cochrane Central Register of Controlled Trials, and the Cochrane Database of Systematic Review, Science Citation Index Expanded, Emerging Sources Citation Index, Scopus, Epistemonikos, and SciELO databases from each database’s inception date until May 2023.
Conclusion:
Advanced bipolar vessel sealing devices demonstrate reduced blood loss and operative times when compared to conventional electrosurgery, however more high-quality evidence and cost analysis is needed to strengthen the clinical significance of these findings.
Keywords: Advanced bipolar vessel sealing device, Electrosurgery, Gynecology, Laparoscopy, Minimally invasive gynecologic surgery, Ultrasonic device
INTRODUCTION
Rationale
Hysterectomy is one of the most common surgical procedures performed in the United States every year.1,2 Although women undergo hysterectomy due to gynecologic cancer, approximately 90% of hysterectomies are performed for benign indications including abnormal uterine bleeding, uterine leiomyomas, endometriosis, and uterine prolapse.1 Ligation and transection of pelvic vasculature are important steps in this procedure. In a transabdominal hysterectomy, the surgeon may ensure hemostasis with cross-clamping and suture ligating the uterine and uteroovarian vessels; however, most hysterectomies are currently performed using a minimally invasive approach which requires the use of electrosurgery and vessel sealing devices to achieve vascular coaptation. Conventional electrosurgery involves application of current to achieve various tissue effects and can be delivered via monopolar or bipolar instruments. Monopolar and bipolar instruments differ based on where the two electrodes are located. Bipolar vessel electrosurgical devices were developed about 50 years ago in Germany and North America in response to the high risk of thermal injury and complications with the use of monopolar energy.3 As a result, there has been an increase in the number and type of electrosurgical devices for vessel sealing on the market. Previous studies have investigated the vessel sealing capabilities of conventional and advanced bipolar vessel sealing devices compared to ultrasonic devices4; however, there is no comprehensive systematic review comparing the currently available advanced bipolar vessel sealing devices and ultrasonic devices for hysterectomies performed for benign indications.
Objectives
The use of advanced bipolar devices for minimally invasive hysterectomy has many reported benefits over use of conventional monopolar and bipolar electrosurgery. Some of these benefits include better vessel compression and sealing capability, the ability to transect tissue without changing instruments, and decreased risk of thermal injury.4,5 However, limited recommendations are available in the field of gynecology regarding vessel sealing technology and their complications. The objective of this systematic review and meta-analysis is to identify and analyze studies that include important perioperative variables, such as operative time, uterine weight, and complications, following the use of conventional bipolar, advanced bipolar, and/or ultrasonic devices for benign laparoscopic hysterectomy. Furthermore, this review aims to elucidate the benefits and disadvantages of these technologies for use in benign gynecologic hysterectomy.
METHODS
This study was deemed exempt from institutional review board approval. Prior to literature database search, the study protocol was developed and registered with the International Prospective Register of Systematic Reviews (PROSPERO: CRD42023392076). This review and meta-analysis were written following the updated Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA)6 guidelines.
Eligibility Criteria
Randomized controlled trials and observational studies (both prospective and retrospective) that assessed and compared use of either conventional monopolar/bipolar electrosurgery, advanced bipolar vessel sealing devices, or ultrasonic devices in laparoscopic hysterectomies for benign indications were included. Unpublished manuscripts, conference abstracts, and non-English studies were excluded from review. Studies that performed total laparoscopic hysterectomy (TLH), laparoscopic-assisted vaginal hysterectomy (LAVH), and laparoscopic supracervical hysterectomy (LASH) were included. Total vaginal hysterectomy and total abdominal hysterectomy were excluded. Outcomes of interest included operative time, estimated blood loss, perioperative complications (eg, blood transfusion, infection, organ injury, reoperation/return to operating room), conversion to laparotomy or to another device, and thermal spread and tissue injury. Study eligibility required reporting of at least one outcome of interest.
Information Sources and Search Strategy
A comprehensive literature database search was conducted to find all relevant literature on electrosurgical devices used for hysterectomy. The database search strategy was developed by a health science librarian (T.J.B.) in consultation with Z.E.O-D. and O.O.C-T. The Ovid Medline search strategy was peer-reviewed by another medical librarian using the Peer Review for Electronic Search Strategies tool.7
Studies were identified by T.J.B. by developing and running searches in MEDLINE (1946 to present), Embase (1974 to present), Cochrane Central Register of Controlled Trials (1991 to present), and the Cochrane Database of Systematic Review (2005 to present) [all via the Wolters Kluwer Ovid interface]; Science Citation Index Expanded (1975 to present) and Emerging Sources Citation Index (2018 to present) [both via the Clarivate Analytics Web of Science interface]; Scopus [via the Elsevier website]; Epistemonikos; and SciELO databases. Clinical trial registers were also searched.
The search strategy was written for Ovid Medline and translated using each database's syntax, controlled vocabulary, and search fields. MeSH terms, EMTREE terms, and text words were used for the search concepts of electrosurgery, electrosurgical devices, bipolar energy devices, ultrasonic devices, vessel sealing, hysterectomy, and their synonyms. Search strategies were translated in part with the assistance of the Institute for Evidence-Based Healthcare Polyglot Search Translator.8 Filters to remove animal studies were used in the database searches. Otherwise, no language, date, or publication type limits were applied during the search phase. Citation searching was performed. All databases and registers were searched on May 26, 2023. The full search strategies are available here: https://osf.io/sqm5v.
All database records were downloaded to EndNote 20 (Clarivate, Philadelphia, PA),9 then uploaded to Covidence10 web-based software for deduplication, screening, and data extraction.
Study Selection
All title, abstract, and study screening was performed within Covidence.10 Titles and abstracts were individually screened by two independent authors (T.S.H., Y.H., P.E.C., Z.E.O-D., and O.O.C-T.), and any conflicts were resolved by a third reviewer. Full text review was conducted by T.S.H. and O.O.C-T. with conflicts being resolved by either P.E.C. or Y.H.
Data Extraction
Data were extracted within Covidence,10 using a standard data extraction template for outcomes of interest. Data from individual studies were extracted by two independent authors (T.S.H., Y.H., P.E.C., and O.O.C-T.). Any conflicts of data extraction were resolved by a third reviewer.
The primary outcomes of our study are: operative time (both total operative time from incision to close and hysterectomy operative time [defined as start of ligation of utero-ovarian vasculature to colpotomy]), estimated blood loss, perioperative complications including urinary (injury to bladder/ureter(s), fistula formation), bowel (minor, major requiring colostomy), cuff (dehiscence/evisceration, hematoma, cellulitis), conversion to laparotomy or a secondary electrosurgical device, and reoperation. The secondary outcomes of our study are physician-reported satisfaction/ease of use of device. These outcomes will be analyzed for each device (conventional monopolar/bipolar devices, advanced bipolar vessel sealing devices, and ultrasonic devices) to identify significant differences. Baseline characteristics were collected including age, indication for surgery, and uterine dimensions, when available.
Assessment of Risk of Bias
Once reviewers completed full-text screening and data extraction, quality assessment was performed within Covidence10 using the Cochrane Risk of Bias (RoB 2) tool11 for randomized controlled trials and the Risk of Bias In Nonrandomized Studies – of Interventions (ROBINS-I) assessment tool12 for observational studies. Characteristics such as how cohorts were recruited, whether outcomes/exposures were accurately measured to reduce bias, and whether authors accounted for confounding factors in the design/analysis were used for the quality and risk of bias assessments. Quality assessment for each study was completed independently by two authors (T.S.H., Y.H., P.E.C., and O.O.C-T.) and any disagreements were resolved by a third author.
Data Synthesis
For binary outcomes, relative risk (RR) and corresponding 95% confidence intervals (CI) were calculated. For continuous outcomes, the mean difference (MD) between groups was extracted or calculated. The RR or MD was pooled across the studies using the DerSimonian and Laird random effects method with Hartung-Knapp-Sidik-Jonkman (HKSJ) variance correction when the number of studies within a meta-analysis was larger than three. When the number of studies was three or less than three, the fixed-effect model was used based on the Mantel and Haenszel method because of concern about instability of study variance. Heterogeneity between studies was evaluated using the I2 indicator. Statistical methods to assess publication bias were not able to be utilized because the number of studies included in the analysis was small (n < 10). Two-tailed P-values less than 0.05 were considered statistically significant. All statistical analyses were conducted using Stata version 17.0 (Stata LLC, College Station, TX).
RESULTS
Study Selection
The literature search identified 5,765 references. Duplicates were excluded and 3,943 references underwent title and abstract screening. After title and abstract screening, 89 studies underwent full text review, and 22 studies were identified and included in the final analysis. The flowchart for study selection is shown in Figure 1. Of the 22 studies included in the final analysis, there were 13 randomized controlled trials,13–25 4 prospective cohort studies,26–29 3 retrospective cohort studies,30–32 and 2 case-control studies.33,34
Figure 1.
PRISMA flow diagram of study selection. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-analyses.
Study Characteristics and Results of Individual Studies
Sample sizes from the included studies ranged from 18 to 429 participants. Studies investigated conventional monopolar and bipolar electrosurgery, advanced bipolar vessel sealing devices (LigaSure [Covidien, Mansfield, MD], EnSeal [Ethicon Endo-surgery, US, LLC], the Plasma Kinetic system [Gyrus ACMI, Southborough, MA], Halo PKS Cutting Forceps [Olympus, Canada], and BiCision [ERBE, Marietta, GA]), and ultrasonic devices (Harmonic ACE [Ethicon Endo-Surgery, Cincinnati, OH, formerly UltraCision]).
Meta-analysis was able to be performed for the following outcomes of interest: estimated blood loss, operative time, and uterine weight. There was insufficient data to include perioperative complications. Similarly, there was insufficient data to report on the secondary outcome of interest (physician-reported satisfaction).
Results of Syntheses and Risk of Bias in Studies
Estimated Blood Loss
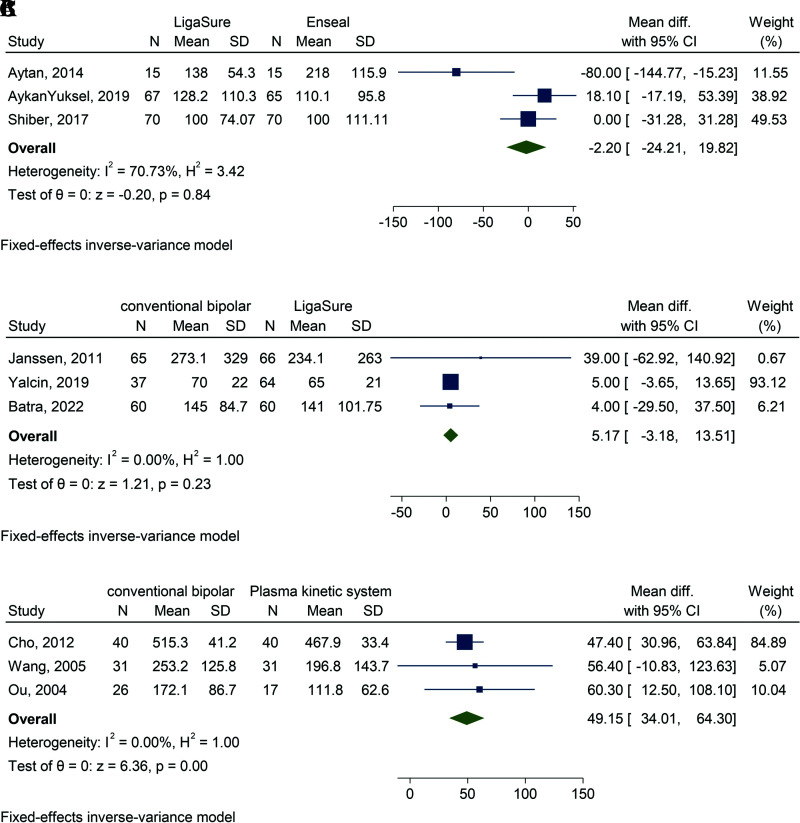
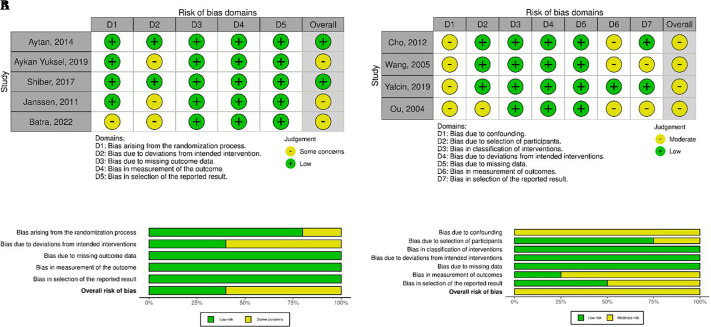
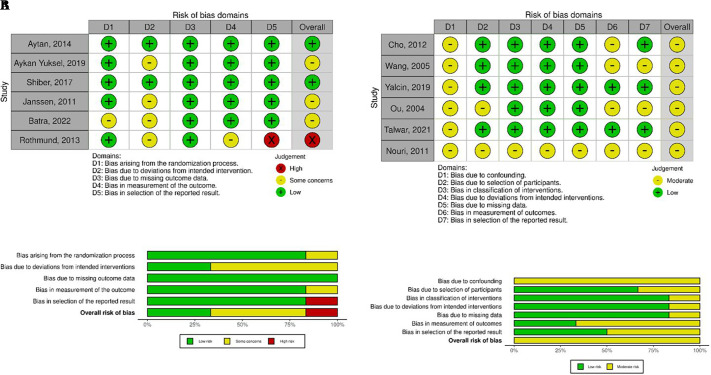
The weighted mean difference (wmd) was used to calculate the difference in estimated blood loss between devices. There were three device comparisons that had enough studies to undergo meta-analysis. When LigaSure was compared to Enseal, there was an observed –2.2 mL difference in blood loss, but this was not statistically significant (95% CI, –24.2–19.8; P = .844) (Figure 2A). For this comparison, three studies were used, representing 302 patients, and substantial heterogeneity was observed (I2 = 70.7%).13,18,21 Conventional electrosurgery had 5.2 mL more blood loss compared to LigaSure, but this also was not statistically significant (95% CI, –3.2–13.5; P = .225). For this comparison, three studies were included with 352 patients and minimal heterogeneity (I2 = 0%)19,24,30 (Figure 2B). Three studies had sufficient details to estimate the blood loss between conventional electrosurgery and the Plasma Kinetic system, representing 185 patients.27,29,31 Conventional electrosurgery had significantly more blood loss at 49.2 mL compared to the Plasma Kinetic system (95% CI, 34.0–64.3; P ≤ .001) (Figure 2C). The heterogeneity score between studies was not important (I2 = 0%). The risk of bias of the included studies for comparing estimated blood loss is reported in Figure 3.
Figure 2.
Forest plots for estimated blood loss. (A) Forest plot for estimated blood loss when LigaSure is compared to Enseal. N, number of patients; SD, standard deviation; CI, confidence interval. (B) Forest plot for estimated blood loss when conventional electrosurgery is compared to LigaSure. N, number of patients; SD, standard deviation; CI, confidence interval. (C) Forest plot for estimated blood loss when conventional electrosurgery is compared to plasma kinetic system. N, number of patients; SD, standard deviation; CI, confidence interval.
Figure 3.
Risk of bias for estimated blood loss. (A) Risk of bias for estimated blood loss in randomized controlled trials (risk of bias tool for randomized trials). (B) Risk of bias for estimated blood loss in nonrandomized studies (risk of bias in nonrandomized studies – of interventions).
Operative Time
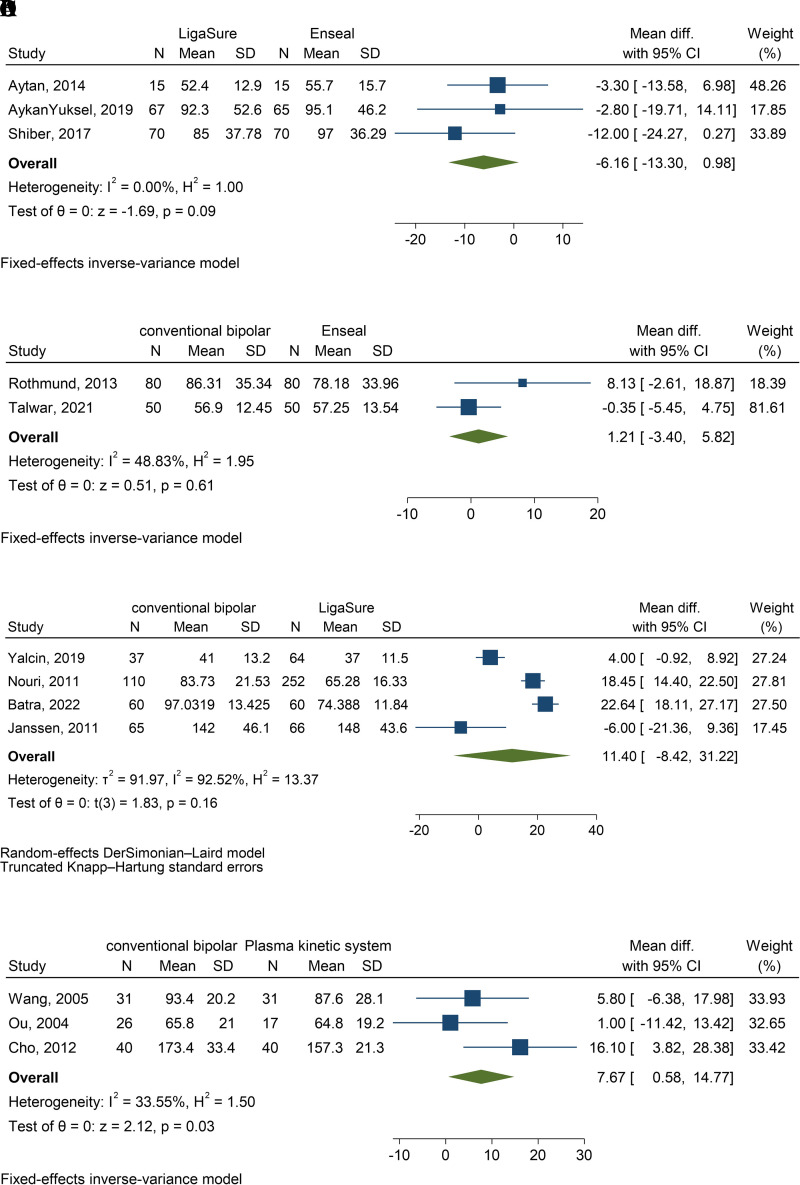
Several device comparisons had sufficient studies to undergo meta-analysis when considering difference in operative time. Three studies compared LigaSure to Enseal, representing 302 patients.13,18,21 Operative time was 6.2 minutes faster when using LigaSure compared to Enseal, but this was not statistically significant (95% CI, −13.3–0.9; P = .091) (Figure 4A). Heterogeneity score of the three studies was not important (I2 = 0%). However, Aykan Yuksel et al18 specifically reported on the operative time for the hysterectomy portion of the procedure (defined as time from start of transection of the round ligament to completion of colpotomy), and in that case, LigaSure was significantly faster than Enseal (25.7 ± 15.2 minutes vs 38.2 ± 22.0 minutes, P = .001).18 Two studies compared conventional electrosurgery to Enseal, representing 260 patients.14,33 Operative time was 1.2 minutes longer in the conventional electrosurgery group compared to Enseal, but this was not statistically significant (95% CI, −3.4–5.8; P = .607) (Figure 4B). Heterogeneity score for the two studies was moderate (I2 = 48.8%). Rothmund et al14 also reported on the operative time for the hysterectomy portion of the procedure (defined as time from transection of cornual structures to complete ligation of uterine vessels, immediately before cervical detachment). In this subgroup, conventional electrosurgery was 11.3 minutes faster, which was statistically significant (95% CI, −17.8 to −4.83; P ≤ .001).14 There were four studies that compared operative time between conventional electrosurgery and LigaSure, which represented 714 patients.19,24,30,34 The heterogeneity between these studies was substantial (I2 = 92.5%). Conventional electrosurgery was 11.4 minutes slower compared to LigaSure, but this was not significant (95% CI, −8.4–31.2; P = .2) (Figure 4C). There were three studies that compared conventional electrosurgery to the Plasma Kinetic system, with a total of 185 patients,27,29,31 and moderate heterogeneity (I2 = 33.6%). Conventional electrosurgery was 7.7 minutes slower than Plasma Kinetic system, and this was statistically significant (95% CI, 0.6–14.8; P = .034) (Figure 4D). The risk of bias of the included studies that compared operative time is depicted in Figure 5.
Figure 4.
Forest plots for operative time. (A) Forest plot for operative time when LigaSure is compared to Enseal. N, number of patients; SD, standard deviation; CI, confidence interval. (B) Forest plot for operative time when conventional electrosurgery is compared to Enseal. N, number of patients; SD, standard deviation; CI, confidence interval. (C) Forest plot for operative time when conventional electrosurgery is compared to LigaSure. N, number of patients; SD, standard deviation; CI, confidence interval. (D) Forest plot for operative time when conventional electrosurgery is compared to plasma kinetic system. N, number of patients; SD, standard deviation; CI, confidence interval.
Figure 5.
Risk of bias for operative time. (A) Risk of bias for operative time in randomized controlled trials (risk of bias tool for randomized trials). (B) Risk of bias for operative time in nonrandomized studies (risk of bias in nonrandomized studies – of interventions).
Uterine Weight
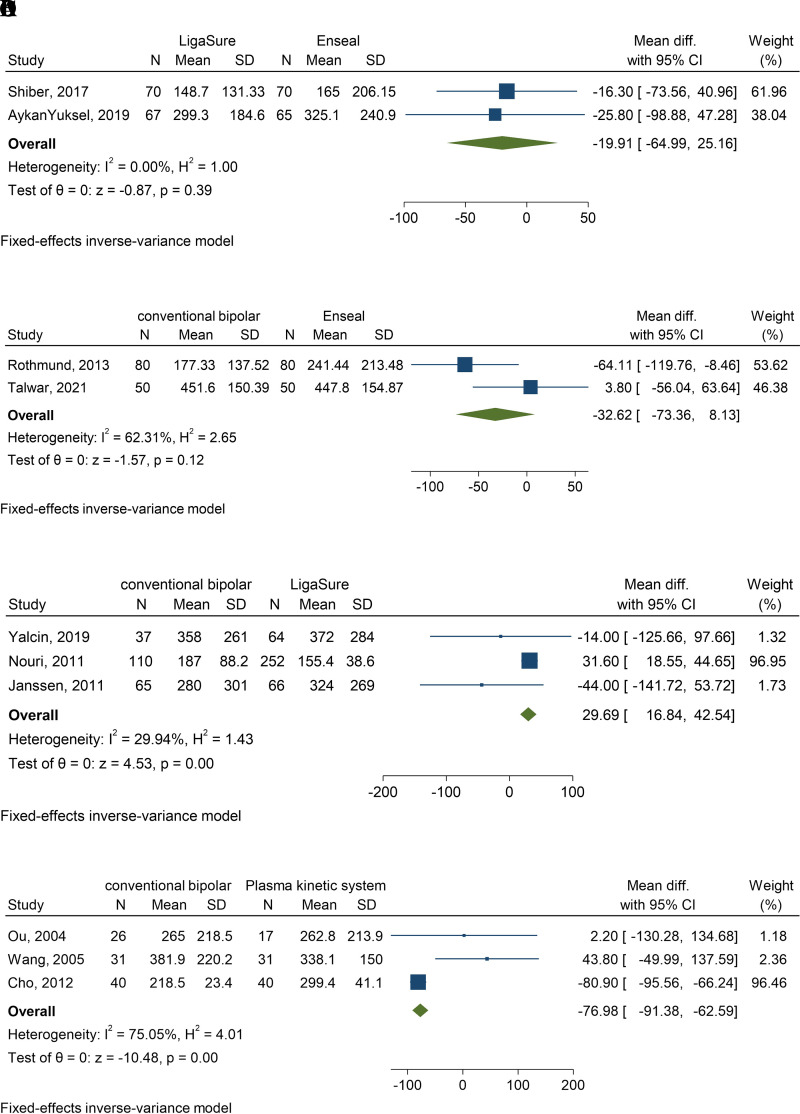
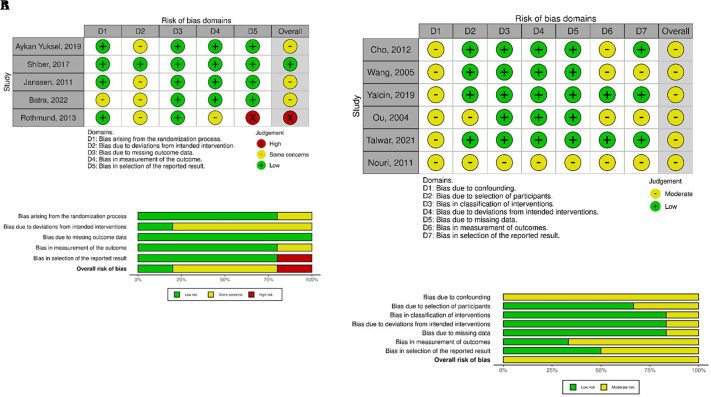
The difference in uterine weight between devices was compared between devices in many studies and allowed for meta-analysis. There were two studies that compared LigaSure to Enseal, totaling 272 patients13,18. The wmd between LigaSure and Enseal was –19.9 grams, which was not statistically significant (95% CI, −64.9–25.2; P = .387) (Figure 6A). Heterogeneity between studies was not important (I2 = 0%). There were two studies comparing conventional electrosurgery to Enseal, representing 260 patients. Uterine weight was −32.6 grams in the conventional electrosurgery group compared to Enseal, which was not statistically different (95% CI, −73.4–8.1; P = .117) (Figure 6B).14,33 Heterogeneity between studies was substantial (I2 = 62.3%). Three studies compared conventional electrosurgery to LigaSure with a total of 594 patients19,30,34 and a heterogeneity score that was not important (I2 = 29.9%) (Figure 6C). The wmd between conventional electrosurgery and LigaSure was significant at 29.7 grams (95% CI, 16.8–42.5; P ≤ .001). Conventional electrosurgery was compared to Plasma Kinetic system in three studies, representing 185 patients.27,29,31 Studies had substantial heterogeneity (I2 = 75.1%). The wmd between conventional electrosurgery and Plasma Kinetic system was −76.9 grams (95% CI, −91.4 to –62.6; P ≤ .001). The risk of bias in the included studies that compared uterine weight is depicted in Figure 7.
Figure 6.
Forest plots for uterine weight. (A) Forest plot for uterine weight when LigaSure is compared to Enseal. N, number of patients; SD, standard deviation; CI, confidence interval. (B) Forest plot for uterine weight when conventional electrosurgery is compared to Enseal. N, number of patients; SD, standard deviation; CI, confidence interval. (C) Forest plot for uterine weight when conventional electrosurgery is compared to LigaSure. N, number of patients; SD, standard deviation; CI, confidence interval. (D) Forest plot for uterine weight when conventional electrosurgery is compared to plasma kinetic system. N, number of patients; SD, standard deviation; CI, confidence interval.
Figure 7.
Risk of bias for uterine weight. (A) Risk of bias for uterine weight in randomized controlled trials (risk of bias tool for randomized trials). (B) Risk of bias for uterine weight in nonrandomized studies (risk of bias in nonrandomized studies – of interventions).
Complications
Intraoperative and postoperative complications were reported in most studies, however, there was significant heterogeneity in reporting, severity classification, and follow-up periods. Due to this, statistical analysis was unreliable, and we will instead report the data descriptively. There were no reported complications for the Halo PKS, BiCision, or Marseal devices. Out of 280 cases performed with the Enseal device, there was 1 reoperation, 1 infection, 1 vascular injury, 1 bowel injury, and 2 genitourinary injuries. The LigaSure device was used in 729 cases, and 1 reoperation, 4 infections, 1 bowel injury, and 2 genitourinary injuries were reported. The Harmonic had 1 genitourinary injury out of 404 total cases. The plasma kinetic system had 1 genitourinary injury of 148 cases. Conventional electrosurgery represented 785 total cases and reported 3 reoperations, 1 vaginal cuff dehiscence, 8 infections, 1 bowel injury, and 2 genitourinary injuries.
DISCUSSION
Principle Findings
In the pooled analysis comparing clinical outcomes among different vessel sealing devices in benign laparoscopic hysterectomy, conventional electrosurgery had more blood loss and longer operative times compared to the Plasma Kinetic system.27,29,31 Pooled analysis demonstrated that conventional electrosurgery had significantly smaller uteri compared to the Plasma Kinetic system, which adds significance to these findings since uterine weight is positively correlated with increased blood loss and operative time.35 Hysterectomies using Enseal had longer operative times compared to LigaSure use, but shorter operative times compared to conventional electrosurgery.14,21 No statistically significant differences in blood loss or operative time were found when comparing conventional electrosurgery to LigaSure19,24,30,34 and no difference in blood loss when LigaSure was compared to Enseal.13,18,21 Although statistically significant differences in blood loss were observed, the differences are likely not clinically significant in general practice.
There were several comparisons that were represented by single studies and not amenable to meta-analysis. One study compared LigaSure to the Harmonic device and demonstrated that LigaSure had statistically significant less blood loss (−64.9 mL; 95% CI, −93.3 to −36.4; P ≤ .001) and operative times (−31.4 minutes; 95% CI, −34.3 to −28.4; P ≤ .001) compared to Harmonic.32 Halo PKS had significantly less blood loss compared to Enseal.21 Other studies did not reach statistical significance for comparing estimated blood loss and operative time.15,16,21,22,33
In this meta-analysis, there were no statistically significant differences in other clinical outcomes such as intraoperative or postoperative complications, length of hospital stay, or conversion to another device.
Comparison with Existing Literature
Previous studies have compared advanced bipolar devices to conventional electrosurgical and ultrasonic instruments by measuring technical parameters like vessel sealing time, maximum vessel diameter, and thermal spread.3–5 In summary, advanced bipolar devices have demonstrated superior sealing capabilities relative to conventional electrosurgical devices, while there is less evidence to suggest the same advantage over ultrasonic devices.4
This systematic review compares multiple advanced bipolar devices both to each other and to other device types and reports differences in clinical outcomes such as estimated blood loss and operative time. One other systematic review compared similar outcomes of interest between advanced bipolar devices and conventional bipolar electrosurgery but chose to combine devices into common groups rather than comparing them individually.36 In this meta-analysis, advanced bipolar devices consistently had less blood loss and shorter operative times compared to conventional electrosurgery (Figures 2C, 4A, 4D), which aligns with Zorzato et al’s findings.36
Strengths and Limitations
The decision to separate advanced bipolar devices and compare them to each other is both a strength and limitation of this study. If pooled together, it would increase the statistical power of advanced bipolar devices. However, the authors felt it was important to compare these devices individually to provide guiding evidence to surgeons in the selection of electrosurgical devices for hysterectomy for benign indications. This limited the ability to perform pooled analyses for clinical outcomes of interest. When reviewing the data, it is also important to consider there are many other devices on the market that have not been utilized in prior studies and were therefore not represented in the findings.
We chose to include studies that performed total laparoscopic hysterectomy, laparoscopic supracervical hysterectomy, and laparoscopic-assisted vaginal hysterectomy. We recognize that there are variations in each of these procedures and may have differences in operative time and blood loss. Prior studies have suggested that LAVH has reduced operative time compared to TLH and LASH has decreased EBL compared to LAVH.37,38 We opted to include studies that performed LASH and LAVH to increase our statistical power, as this accounted for five studies and over 1,000 patients. In addition to hysterectomy type, we acknowledge that differences in operative time and EBL exist depending on surgeon experience and level of training and whether the case was performed at a training institution with resident or fellow involvement. These data were unavailable for all studies and therefore not included in the final analysis.
Although this systematic review and meta-analysis report many statistically significant findings, the clinical relevance is likely not significant. When considering difference in estimated blood loss, the statistically significant findings ranged between 49.2 and 100 mL difference (Table 1), which would not result in a change in clinical management. Differences in operative times ranged from 7.7 to 31.4 minutes. There is evidence to suggest increased operative times in gynecologic surgery leads to increased 30-day postoperative complications, increasing linearly in 60-minute intervals.39–41 This could also have significant financial impact when considering that the mean cost per minute in the operating room is around $36–$37 USD.42 A cost analysis of each device is beyond the scope of this review but could be an area for future research.
Table 1.
Key Outcomes for Included Studies
| Outcome | Comparison | Number of Studies | Number of Patients | Weighted Mean Difference (wmd) | 95% CI, Min | 95% CI, Max | P-value | I2 |
|---|---|---|---|---|---|---|---|---|
| Blood loss (mL) | Halo PKS vs Enseal | 1 | 30 | −100 | −166.8 | −33.2 | 0.003 | NA |
| LigaSure vs Enseal | 3 | 302 | −2.2 | −24.2 | 19.8 | 0.84 | 70.7 | |
| Conventional vs Enseal | 1 | 100 | 3.56 | −4.8 | 11.9 | 0.40 | NA | |
| Harmonic vs Halo PKS | 1 | 30 | 20 | −22.1 | 62.1 | 0.35 | NA | |
| LigaSure vs Harmonic | 1 | 40 | −64.9 | −93.3 | −36.4 | <0.001 | NA | |
| Conventional vs Harmonic | 1 | 40 | −5.4 | −24.3 | 13.5 | 0.58 | NA | |
| Conventional vs LigaSure | 3 | 352 | 5.2 | −3.2 | 13.5 | 0.23 | 0 | |
| Conventional vs plasma kinetic system | 3 | 185 | 49.2 | 34.0 | 64.3 | <0.001 | 0 | |
| Operative time (minutes) | Harmonic vs BiCision | 1 | 60 | −0.5 | −1.4 | 0.4 | 0.29 | NA |
| Halo PKS vs Enseal | 1 | 30 | −3.8 | −14.5 | 6.9 | 0.49 | NA | |
| LigaSure vs Enseala | 3 | 302 | −6.2 | −13.3 | 0.9 | 0.09 | 0 | |
| Conventional vs Ensealb | 2 | 260 | 1.2 | −3.4 | 5.8 | 0.61 | 48.8 | |
| LigaSure vs Halo PKS | 1 | 30 | 0.5 | −9.2 | 10.2 | 0.92 | NA | |
| LigaSure vs Harmonic | 1 | 40 | −31.4 | −34.3 | −28.4 | <0.001 | NA | |
| Marseal vs LigaSure | 1 | 74 | 3.7 | −4.5 | 11.9 | 0.37 | NA | |
| Conventional vs LigaSure | 4 | 714 | 11.4 | −8.4 | 31.2 | 0.20 | 92.5 | |
| Conventional vs plasma kinetic system | 3 | 185 | 7.7 | 0.6 | 14.8 | 0.03 | 33.6 | |
| Uterine weight (g) | LigaSure vs Enseal | 2 | 272 | −19.9 | −64.9 | 25.2 | 0.39 | 0 |
| Conventional vs Enseal | 2 | 260 | −32.6 | −73.4 | 8.1 | 0.12 | 62.3 | |
| LigaSure vs Harmonic | 1 | 40 | 6.8 | −19.2 | 32.9 | 0.61 | NA | |
| Conventional vs Harmonic | 1 | 60 | 50.0 | −112.4 | 212.4 | 0.55 | NA | |
| Conventional vs LigaSure | 3 | 594 | 29.7 | 16.8 | 42.5 | <0.001 | 29.9 | |
| Conventional vs plasma kinetic system | 3 | 185 | −76.9 | −91.4 | −62.6 | <0.001 | 75.1 |
Abbreviations: CI, confidence interval; NA, not applicable.
aOne study compared operative times for just the hysterectomy portion of the procedure. In this subgroup, LigaSure was 12.5 minutes faster than Enseal (P ≤ .001).
bOne study compared operative times for just the hysterectomy portion of the procedure. In this subgroup, conventional electrosurgery was 11.3 minutes slower than Enseal (P ≤ .001).
CONCLUSIONS AND IMPLICATIONS
In summary, the findings of this study demonstrate reduced blood loss and operative times for advanced bipolar devices compared to conventional electrosurgery, with the strongest available evidence in support of the Plasma Kinetic system. The clinical relevance of these findings is limited, and more prospective, comparative research studies are needed. One device does not appear superior to another, and we recommend that electrosurgical device selection be done per surgeon preference. Surgeons may want to consider the reduced operative times of advanced bipolar devices, as this may reduce overall complications and operating room costs. For future studies, a detailed cost analysis may improve the clinical relevance of comparing different vessel sealing devices.
Footnotes
Conflict of interests: none.
Disclosure: none.
Funding sources: none.
Contributor Information
Toni S. Horton, Department of Medical and Surgical Gynecology, Mayo Clinic College of Medicine & Science, Jacksonville, FL. (Drs. Horton, Coombs, and Cardenas-Trowers).
Paulette E. Coombs, Department of Medical and Surgical Gynecology, Mayo Clinic College of Medicine & Science, Jacksonville, FL. (Drs. Horton, Coombs, and Cardenas-Trowers).
Yooree Ha, Mayo Clinic College of Medicine & Science, Jacksonville, FL. (Ms. Ha).
Zhen Wang, Mayo Clinic Evidence-based Practice Center, Rochester, MN. (Dr. Wang).
Tara J. Brigham, Mayo Clinic Libraries, Jacksonville, FL. (Ms. Brigham).
Zenobia E. Ofori-Dankwa, Department of OB/GYN, University of Louisville School of Medicine, Louisville, KY. (Dr. Ofori-Dankwa).
Olivia O. Cardenas-Trowers, Department of Medical and Surgical Gynecology, Mayo Clinic College of Medicine & Science, Jacksonville, FL. (Drs. Horton, Coombs, and Cardenas-Trowers).
References:
- 1.Simms KT, Yuill S, Killen J, et al. Historical and projected hysterectomy rates in the USA: implications for future observed cervical cancer rates and evaluating prevention interventions. Gynecol Oncol. 2020;158(3):710–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Falcone T, Walters MD. Hysterectomy for benign disease. Obstet Gynecol. 2008;111(3):753–767. [DOI] [PubMed] [Google Scholar]
- 3.Jaiswal A, Huang KG. Energy devices in gynecological laparoscopy - Archaic to modern era. Gynecol Minim Invasive Ther. 2017;6(4):147–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lyons SD, Law KS. Laparoscopic vessel sealing technologies. J Minim Invasive Gynecol. 2013;20(3):301–307. [DOI] [PubMed] [Google Scholar]
- 5.Chekan EG, Davison MA, Singleton DW, Mennone JZ, Hinoul P. Consistency and sealing of advanced bipolar tissue sealers. Med Devices (Auckl). 2015;8:193–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–46. [DOI] [PubMed] [Google Scholar]
- 8.Clark JM, Sanders S, Carter M, et al. Improving the translation of search strategies using the polyglot search translator: a randomized controlled trial. J Med Libr Assoc. 2020;108(2):195–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.EndNote. Version 20. Clarivate Analytics. 2023.
- 10.Covidence systematic review software. 2023. Veritas health innovation. Melbourne, Australia. Available at www.covidence.org. [Google Scholar]
- 11.Sterne J, Savović J, Page M, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 12.Sterne J, Hernán M, Reeves B, et al. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ. 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shiber LDJ, Ginn DN, Jan A, Gaskins JT, Biscette SM, Pasic R. Comparison of industry-leading energy devices for use in gynecologic laparoscopy: articulating ENSEAL versus LigaSure energy devices. J Minim Invasive Gynecol. 2018;25(3):467–473.e1. [DOI] [PubMed] [Google Scholar]
- 14.Rothmund R, Kraemer B, Brucker S, et al. Laparoscopic supracervical hysterectomy using EnSeal vs standard bipolar coagulation technique: randomized controlled trial. J Minim Invasive Gynecol. 2013;20(5):661–666. [DOI] [PubMed] [Google Scholar]
- 15.Rothmund R, Szyrach M, Reda A, et al. A prospective, randomized clinical comparison between UltraCision and the novel sealing and cutting device BiCision in patients with laparoscopic supracervical hysterectomy. Surg Endosc. 2013;27(10):3852–3859. [DOI] [PubMed] [Google Scholar]
- 16.Holub Z, Voracek J, Jun LK, Lukac J. Laparoscopic hysterectomy: randomized study of harmonic scalpel and electrosurgery. J Gynecol Surg. 2000;16(1):33–39. [Google Scholar]
- 17.Choi C, Do I-G, Song T. Ultrasonic versus monopolar energy-based surgical devices in terms of surgical smoke and lateral thermal damage (ULMOST): a randomized controlled trial. Surg Endosc. 2018;32(11):4415–4421. [DOI] [PubMed] [Google Scholar]
- 18.Aykan Yuksel B, Karadag B, Mulayim B. Comparison of the efficacy and safety of two advanced vessel sealing technologies in total laparoscopic hysterectomy. J Obstet Gynaecol Res. 2019;45(11):2220–2227. [DOI] [PubMed] [Google Scholar]
- 19.Janssen PF, Brolmann HAM, van Kesteren PJM, et al. Perioperative outcomes using LigaSure compared with conventional bipolar instruments in laparoscopic hysterectomy: a randomised controlled trial. BJOG. 2011;118(13):1568–1575. [DOI] [PubMed] [Google Scholar]
- 20.Wong C, Goh A, Merkur H. Comparison of surgical outcomes using Gyrus PKS™ vs LigaSure™ in total laparoscopic hysterectomy: a randomised controlled trial. Aust N Z J Obstet Gynaecol. 2020;60(5):790–796. [DOI] [PubMed] [Google Scholar]
- 21.Aytan H, Nazik H, Narin R, Api M, Tok EC. Comparison of the use of LigaSure, HALO PKS cutting forceps, and ENSEAL tissue sealer in total laparoscopic hysterectomy: a randomized trial. J Minim Invasive Gynecol. 2014;21(4):650–655. [DOI] [PubMed] [Google Scholar]
- 22.Hasanov M, Denschlag D, Seemann E, Gitsch G, Woll J, Klar M. Bipolar vessel-sealing devices in laparoscopic hysterectomies: a multicenter randomized controlled clinical trial. Arch Gynecol Obstet. 2018;297(2):409–414. [DOI] [PubMed] [Google Scholar]
- 23.Caltekin MD, Aydogmus S, Yalcin SE, et al. Comparison of three different new bipolar energy modalities and classic bipolar in vivo for tissue thermal spread. Turkish J Pathol. 2017;33(2):144–149. 10.5146/tjpath.2016.01377 [DOI] [PubMed] [Google Scholar]
- 24.Batra S, Bhardwaj P, Dagar M. Comparative analysis of peri-operative outcomes following total laparoscopic hysterectomy with conventional bipolar-electrosurgery versus high-pressure pulsed LigaSure use. Gynecol Minim Invasive Ther. 2022;11(2):105–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Holloran-Schwartz MB, Gavard JA, Martin JC, Blaskiewicz RJ, Yeung PP., Jr. Single-use energy sources and operating room time for laparoscopic hysterectomy: a randomized controlled trial. J Minim Invasive Gynecol. 2016;23(1):72–77. [DOI] [PubMed] [Google Scholar]
- 26.Jung H, Lim JS, Cho HJ. Comparison of bipolar coagulator and ultrasonic surgical system on laparoscopy-assisted vaginal hysterectomy. J Gynecol Surg. 2005;21(2):73–79. [Google Scholar]
- 27.Wang C-J, Yuen L-T, Yen C-F, Lee C-L, Soong Y-K. Comparison of the efficacy of the pulsed bipolar system and conventional bipolar electrosurgery in laparoscopically assisted vaginal hysterectomy. J Laparoendosc Adv Surg Tech A. 2005;15(4):361–364. [DOI] [PubMed] [Google Scholar]
- 28.Holub Z, Jabor A, Sprongl L, Kliment L, Fischlová D, Urbánek S. Inflammatory response and tissue trauma in laparoscopic hysterectomy: comparison of electrosurgery and harmonic scalpel. Clin Exp Obstet Gynecol. 2002;29(2):105–109. [PubMed] [Google Scholar]
- 29.Ou C-S, Joki J, Wells K, et al. Total laparoscopic hysterectomy using multifunction grasping, coagulating, and cutting forceps. J Laparoendosc Adv Surg Tech A. 2004;14(2):67–71. [DOI] [PubMed] [Google Scholar]
- 30.Yalcin Y, Yalcin SE. Perioperative outcomes of bipolar energy instruments in total laparoscopic hysterectomy. Ginekol Pol. 2019;90(11):640–644. [DOI] [PubMed] [Google Scholar]
- 31.Cho H-Y, Choi K-J, Lee Y-L, Chang KH-J, Kim H-B, Park S-H. Comparison of two bipolar systems in laparoscopic hysterectomy. JSLS. 2012;16(3):456–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Demirturk F, Aytan H, Caliskan AC. Comparison of the use of electrothermal bipolar vessel sealer with harmonic scalpel in total laparoscopic hysterectomy. J Obstet Gynaecol Res. 2007;33(3):341–345. [DOI] [PubMed] [Google Scholar]
- 33.Talwar P, Kumarachar SH, Velayudam L, Fathima T. Efficacy and safety of electrothermal bipolar vessel sealer vs enseal in total laparoscopic hysterectomy for large uterus: a comparative study in Mysuru, South India. World J Laparosc Surg. 2021;14(1):5–9. [Google Scholar]
- 34.Nouri K, Ott J, Demmel M, Promberger R, Huber JC, Mayerhofer K. Bipolar vessel sealing increases operative safety in laparoscopic-assisted vaginal hysterectomy. Arch Gynecol Obstet. 2011;283(1):91–95. [DOI] [PubMed] [Google Scholar]
- 35.English EM, Bell S, Kamdar NS, Swenson CW, Wiese H, Morgan DM. Importance of estimated blood loss in resource utilization and complications of hysterectomy for benign indications. Obstet Gynecol. 2019;133(4):650–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zorzato PC, Ferrari FA, Garzon S, et al. Advanced bipolar vessel sealing devices vs conventional bipolar energy in minimally invasive hysterectomy: a systematic review and meta-analysis. Arch Gynecol Obstet. 2024;309(4):1165–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Long CY, Fang JH, Chen WC, Su JH, Hsu SC. Comparison of total laparoscopic hysterectomy and laparoscopically assisted vaginal hysterectomy. Gynecol Obstet Invest. 2002;53(4):214–219. [DOI] [PubMed] [Google Scholar]
- 38.Jenkins TR. Laparoscopic supracervical hysterectomy. Am J Obstet Gynecol. 2004;191(6):1875–1884. [DOI] [PubMed] [Google Scholar]
- 39.Catanzarite T, Saha S, Pilecki MA, Kim JY, Milad MP. Longer operative time during benign laparoscopic and robotic hysterectomy is associated with increased 30-day perioperative complications. J Minim Invasive Gynecol. 2015;22(6):1049–1058. [DOI] [PubMed] [Google Scholar]
- 40.Kim EK, Applebaum JC, Kravitz ES, et al. Every minute counts: association between operative time and post-operative complications for patients undergoing minimally invasive sacrocolpopexy. Int Urogynecol J. 2023;34(1):263–270. [DOI] [PubMed] [Google Scholar]
- 41.Singh S, Swarer K, Resnick K. Longer operative time is associated with increased post-operative complications in patients undergoing minimally-invasive surgery for endometrial cancer. Gynecol Oncol. 2017;147(3):554–557. [DOI] [PubMed] [Google Scholar]
- 42.Childers CP, Maggard-Gibbons M. Understanding costs of care in the operating room. JAMA Surg. 2018;153(4):e176233. [DOI] [PMC free article] [PubMed] [Google Scholar]