Abstract
Background and Aims:
Both operating table height and patient level in relation to the anesthesiologist influence supraglottic airway device (SAD) insertion and task performance in terms of physical and mental workload. The aim of the study was to find out the appropriate table height during SAD insertion in terms of time taken for insertion, success rate, ease of insertion, and anesthesiologist comfort.
Material and Methods:
In this randomized controlled trial, 90 American Society of Anesthesiologists physical status I and II patients, aged between 18 and 60 years, scheduled for elective surgery were recruited. Patients were divided into three groups of 30 each. During SAD insertion, the table height was adjusted so that the patient’s forehead was at the level of 5 cm above the xiphoid process in group I, at the level of the xiphoid process in group II, and at the level of 5 cm below the xiphoid process in group III of the anesthesiologist. We measured SAD insertion time, first attempt success rate, ease of insertion, and anesthesiologist comfort during the procedure.
Results:
The SAD insertion time (in seconds) was lower in group III than in groups I and II, and a significant difference was found between the groups (P < 0.05). The mean ease of insertion score, anesthesiologist comfort, and the first-attempt success rate of SAD insertion were higher in group III than in groups I and II, and the difference among the groups was statistically significant (P < 0.05).
Conclusions:
We conclude that the lower table height with the patient’s forehead at the level of 5 cm below the xiphoid process of the anesthesiologist is ergonomically more efficient during SAD (I-gel) insertion. This table height is also more comfortable for the anesthesiologist during SAD placement.
Keywords: Anesthesiologist, operating table height, supraglottic airway devices
Introduction
Supraglottic airway devices (SADs) are used to maintain the airway during anesthesia. It is imperative to perform the insertion in the shortest possible time to avoid fatal complications. This can be achieved by the proper positioning of the patient’s head during the procedure.[1] Postural adjustments by the anesthesiologist at the neck, back, knee, and ankle during SAD insertion result in physical problems such as cervical disc pain, mental workload, and poor task performance.[2,3,4,5] The anesthesiologist’s discomfort was compensated by creating abnormal angles at the wrist, elbow, and shoulder joints. Lee et al.[6] found that higher table levels reduce discomfort during laryngoscopy and tracheal intubation by limiting the need to bend the neck or lower back. Successful insertion of the SAD depends upon many factors, such as the patient’s mouth opening, gender, the type of denture condition, and the size of the SAD. Table height in relation to the anesthesiologist’s xyphoid process is also a major factor influencing the successful SAD insertion. We could not find any studies on optimal table height for anesthesiologists while inserting the SAD. The aim of this study was to find out the appropriate table height during SAD insertion in terms of time taken for insertion, success rate, ease of insertion, and anesthesiologist comfort. We hypothesized that setting the table height with the patient’s forehead 5 cm below the anesthesiologist’s xiphoid process would reduce the SAD insertion time and increase the anesthesiologist’s comfort.
Material and Methods
This study was approved by the institutional ethical committee. Written informed consent was obtained from all subjects to participate in the trial. The trial was registered prior to patient enrollment at the Clinical Trial Registry of India (CTRI/2020/06/02603). This randomized control trial was conducted from August 2021 to January 2022. Ninety American Society of Anesthesiologists (ASA) physical status I and II patients, aged between 18 and 60 years, with mallampati of grade I and II, were recruited. Contraindications of SADs and difficult airways were excluded. The patients were randomized into three groups, with 30 patients in each group, by computer-generated random numbers. The randomly allocated sequence was concealed in opaque, sealed envelopes, and a group name was assigned as shown [Figure 1]. In group I, the table height was adjusted so that the patient’s forehead was at the level of 5 cm above the xiphoid process of the anesthesiologist; in group II, the table height was adjusted so that the patient’s forehead was at the level of the xiphoid process of the anesthesiologist; and in group III, the table height was kept so that the patient’s forehead was at the level of 5 cm below the xiphoid process of the anesthesiologist. In the operating room, patients were placed in a supine position with a 6-cm-thick pillow under their occiput, facilitating the flexion of the cervical spine. The initial table level was adjusted according to the group allocation. Standard monitoring devices such as non-invasive blood pressure, pulse oximeter, and electrocardiography were connected. SAD (size 3 was used for patients weighing between 30 and 60 kg, and size 4 was used for patients weighing between 50 and 90 kg) insertion was performed after administering anesthesia using propofol (2 mg/kg), fentanyl (2 mcg/kg), and vecuronium (0.1 mg/kg) intravenously. A 1:1 air-to-oxygen ratio and a minimum alveolar concentration of isoflurane were used to maintain anesthesia.[7] The primary objective of this study was SAD insertion time (in seconds). Secondary objectives were first-attempt success rate, ease of insertion (using a 5-point Likert scale where 1 is the hardest to use and 5 is the easiest), and anesthesiologist comfort. SAD insertion time was counted from the time when the supraglottic airway was picked up and the administration of the first breath until the appearance of the square wave capnography waveform, which is suggestive of adequate ventilation.[8] All SAD I gel insertions (intersurgical, Wokingham, Berkshire, RG412RZ, UK) were performed by five experienced anesthesiologists who had performed more than 100 successful SAD insertions and were earlier enrolled in the study on a voluntary basis.[9] Comfort was measured based on the presence or absence of movement at various joints (neck, lower back, ankle, and knee) of the anesthesiologist performing the procedure. A score of 0 meant no movement at either joint; a score of 1 meant movement at each joint (minimum score of 0 and a maximum score of 4).[10] Both the patient and the data analyst were blinded to the group assigned. According to Sharda et al.,[11] normal apnea time during gel insertion with the conventional insertion technique was 20.8 ± 5.9 s. In our study, the sample size was calculated by assuming a 25% variation in apnea time at different table heights considered statistically significant. The sample size came out to be 27, with an alpha error of 0.05 and a power of 90%. Considering a 10% dropout rate, we took a total of 90 patients, 30 in each group. Statistical analysis was performed using SPSS 22 software. Continuous variables are expressed as mean ± standard deviation and categorical variables as proportions (%). The analysis of variance (ANOVA) test was used for the comparison of patient characteristics and the differences in variables among the three groups. P values < 0.05 were considered statistically significant.
Figure 1.
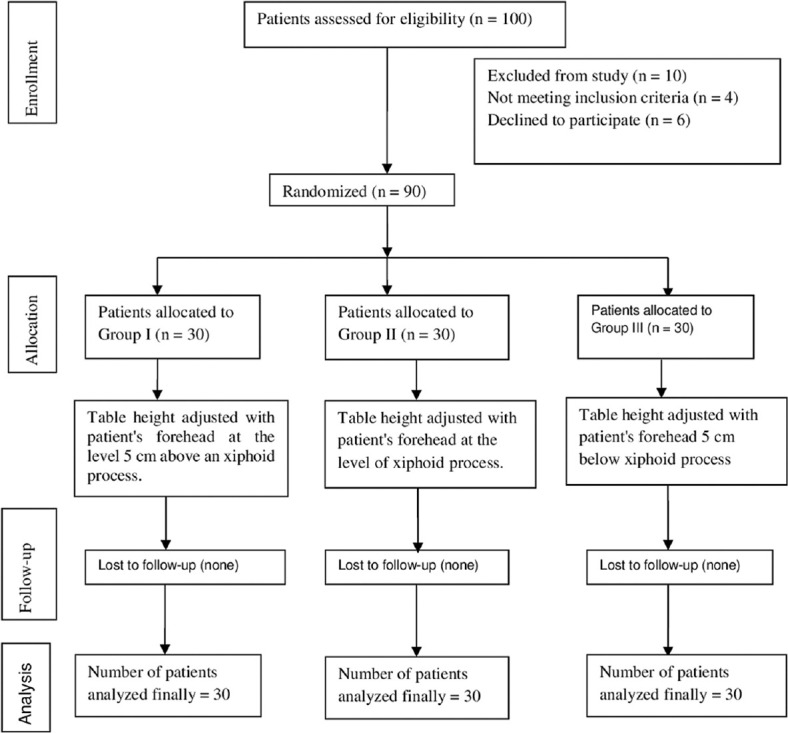
Consort flowchart
Results
We assessed the eligibility of 100 patients, out of which 10 were excluded from the study (4 did not meet the inclusion criteria for having a difficult airway, and 6 were not given consent to participate in the study). Figure 1 shows the CONSORT flow diagram of the patient’s progress through the study. All the patients enrolled in the study (group I: n = 30; group II: n = 30; group III: n = 30). Table 1 presents the patient demographic data of three groups that were comparable, and there was no clinically significant difference among the research groups. Our primary outcome was the SAD insertion time (in seconds), which was lower in group III than in groups I and II, and a significant difference was found between the groups [Table 2]. Our secondary outcomes were the mean ease of insertion score, anesthesiologist comfort, and the first-attempt success rate of SAD insertion, which was higher in group III than in group I and group II, and the difference among the groups was statistically significant [Table 2]. However, the requirement for more than one attempt was less in group III than in groups I and II. A significant difference was found between the groups [Table 2].
Table 1.
Demographic parameter
| Variant | Group I | Group II | Group III | P | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| Mean | SD | Mean | SD | Mean | SD | ||
| Age | 39.81 | 8.02 | 43.09 | 11.34 | 40.32 | 7.23 | >0.05 |
| BMI | 21.5 | 4.89 | 22.48 | 5.41 | 22.93 | 5.99 | >0.05 |
Age and weight in the above table are in terms of mean±SD
Table 2.
SAD insertion time, ease of insertion, anesthesiologist comfort, and number of attempts
| Value | Group I Mean±SD | Group II Mean±SD | Group III Mean±SD | P |
|---|---|---|---|---|
| SAD insertion time (in seconds) | 21.53±6.21 | 17.1±2.83 | 13.43±2.87 | <0.05 |
| Ease of insertion | 3.9±0.75 | 4.7±0.46 | 4.83±0.37 | <0.05 |
| Anesthesiologist comfort | 1.43±0.56 | 0.4±0.56 | 0.16±0.37 | <0.05 |
| Number of attempts (%) | ||||
| First attempt | 36.66 | 66.66 | 93.33 | <0.05 |
| More than one attempt | 63.33 | 33.33 | 06.66 | <0.05 |
Values in the above table are in terms of mean±SD *P<0.05 statistically significant
Discussion
In this study, we found that significantly less time was required for SAD insertion when the operating table height was adjusted with the patient’s forehead kept at the level of 5 cm below the xiphoid process of the anesthesiologist. The first-attempt success rate of SAD placement was higher when the operating table height was adjusted with the patient’s forehead kept at a level of 5 cm below the xiphoid process of the anesthesiologist [Figure 2]. The ease of insertion and the anesthesiologist’s comfort were also higher when the operating table height was adjusted with the patient’s forehead kept at a level of 5 cm below the xiphoid process of the anesthesiologist. In our study, we found that higher levels of operating table height in relation to the anesthesiologist (at the xiphoid process, 5 cm above the xiphoid process) were least comfortable for the anesthesiologist during SAD insertion because more postural adjustments were required at the neck, back, knee, and ankle. For this, anesthesiologists compensated by creating uncomfortable angles at the joints of the wrists, elbows, and shoulders, leading to discomfort. This study had a 100% success rate for SAD insertion. A report stated that inexperienced anesthesiologists had more movements in their upper body to compensate for trolly height during laryngoscopy as compared to experienced anesthesiologists, who maintained their erect posture.[10] There are few studies published highlighting the appropriate operating table height in relation to the anesthesiologist during bag and mask ventilation, during laryngoscopy and endotracheal intubation, and during chest compression.[12] There is a lack of clear-cut guidelines regarding operating table height in relation to the anesthesiologist during SAD insertion. SAD has been inserted in various positions, such as neutral, sniffing, and prone.[9,13] We performed SAD insertion in the sniffing position. Proper positioning of the patient’s head and the level of the patient in relation to the anesthesiologist is vital. It is well understood that anesthesiologists tend to adopt poor postures during various procedures, with movements at various joints affecting them.[14] Hongi et al.[12] evaluated the effect of bed height on airway procedure outcomes such as bag mask ventilation, endotracheal intubation, and routine airway procedures in their study. Contrary to our result, they found that table height does not affect the outcome.
Figure 2.
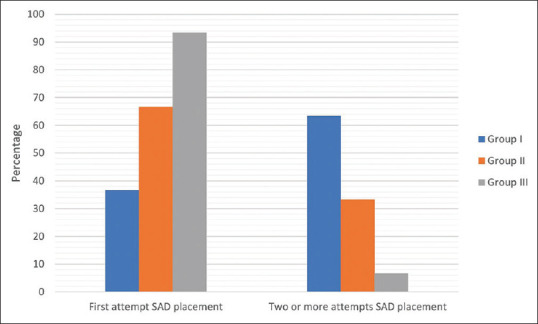
First-attempt success rate among the three groups
Limitations
Anesthesiologists could not be blinded to different table levels. The intensity of joint motion was not measured. We were unable to determine the sample size based on the primary outcome. We could not measure the number of manipulations. These limitations could be considered while designing future studies.
Conclusions
We conclude that the lower table height with the patient’s forehead at the level of 5 cm below the xiphoid process of the anesthesiologist is ergonomically more efficient during SAD (I-gel) insertion. This table height is also more comfortable for the anesthesiologist during SAD placement.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
There are no conflicts of interest.
Funding Statement
Nil
References
- 1.El-Orbany M, Woehlck H, Salem M. Head and neck position for direct laryngoscopy. Anesth Analg. 2011;113:103–9. doi: 10.1213/ANE.0b013e31821c7e9c. [DOI] [PubMed] [Google Scholar]
- 2.Hunningher A. A pain in the neck. RCoA Bull. 2009;58:13–4. [Google Scholar]
- 3.McNeill JM. Cervical disc problems. RCoA Bull. 2010;59:53. [Google Scholar]
- 4.Berquer R, Smith W, Davis S. An ergonomic study of the optimum operating table height for laparoscopic surgery. Surg Endosc. 2001;16:416–21. doi: 10.1007/s00464-001-8190-y. [DOI] [PubMed] [Google Scholar]
- 5.Hanna G, Shimi S, Cuschieri A. Task performance in endoscopic surgery is influenced by location of the image display. Ann Surg. 1998;227:481–4. doi: 10.1097/00000658-199804000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee H, Yun M, Hwang J, Na H, Kim D. Park Higher operating tables provide better laryngeal views for tracheal intubation. Br J Anaesth. 2014;112:749–55. doi: 10.1093/bja/aet428. [DOI] [PubMed] [Google Scholar]
- 7.Fujiwara A, Komasawa N, Nishihara I, Miyazaki S, Tatsumi S, Nishimura W, et al. Muscle relaxant effects on insertion efficacy of the laryngeal mask ProSeal(®) in anesthetized patients: A prospective randomized controlled trial. J Anesth. 2015;29:580–4. doi: 10.1007/s00540-015-1982-3. [DOI] [PubMed] [Google Scholar]
- 8.Castle N, Pillay Y, Spencer N. Insertion of six different supraglottic airway devices whilst wearing chemical, biological, radiation, nuclear-personal protective equipment: A manikin study. Anaesthesia. 2011;66:983–8. doi: 10.1111/j.1365-2044.2011.06816.x. [DOI] [PubMed] [Google Scholar]
- 9.Kim GW, Kim JY, Kim SJ, Moon YR, Park EJ, Park SY. Conditions for laryngeal mask airway placement in terms of oropharyngeal leak pressure: A comparison between blind insertion and laryngoscope-guided insertion. BMC Anaesthesiol. 2019;19:4. doi: 10.1186/s12871-018-0674-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Puri K, Udupi S, Shenoy K, Shenoy A. Influence of operating table height on laryngeal view during direct laryngoscopy: A randomized prospective crossover trial. Trends Anaesth Crit. 2019;28:14–8. [Google Scholar]
- 11.Sharda M, Kapoor MC, Atray R, Garg S. Insertion of i-gel™by the reversed technique improves the success rate and reduces the time taken for its placement: A prospective, randomized, controlled, interventional trial. J Anaesthesiol Clin Pharmacol. 2017;33:226–30. doi: 10.4103/joacp.JOACP_395_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hongi JY, Oh JH, Kim CW, Kim SE, Lee DH, Shin JH. Effects of bed height on the performance of endotracheal intubation and bag mask ventilation. Signa Vitae. 2016;12:47–51. [Google Scholar]
- 13.Kundra P. Securing of supraglottic airway devices during position change and in prone position. Indian J Anaesth. 2018;62:159–61. doi: 10.4103/ija.IJA_164_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walker JD. Posture used by anaesthetists during laryngoscopy. Br J Anaesth. 2002;89:772–4. [PubMed] [Google Scholar]


