Abstract
Introduction
There is evidence of a gap between individuals with intellectual and developmental disabilities (IDD) who need treatment for self-injurious behavior (SIB) and those who receive treatment. The purpose of this study (n=15) was to begin to understand the treatment gap from the perspective of family caregivers.
Methods
In semi-structured virtual interviews, family caregivers discussed their experiences of working with providers to treat their child’s or sibling’s self-injury. Through a systematic process of quasi-inductive thematic analysis, researchers transcribed and analyzed the interviews and developed a working model of treatment pathways.
Results
Caregivers described many barriers to treatment access. Themes include Caregiver Driven, Importance of the Provider-Caregiver Relationship, Beliefs and Perceptions about SIB, Practical Constraints, Knowledge Gaps, and Wait Until Crisis.
Conclusion
The findings highlight the power of providers to support families coping with SIB in IDD. Specific ways providers can better facilitate treatment access are suggested. Future research directions should include provider interviews and focus groups and, ultimately, the development of interventions that consider access pathways as a key feature of any effective treatment plan.
Keywords: qualitative, self-injurious behavior, caregivers, treatment access
“Nobody wants to help you until the ambulance comes. You know, until you reach a crisis point… that to me is- that’s the real tragedy here, because I have been crying out, to everybody who will listen to me: I need help. I need help. I need help. And all of them go- wow, yes you do. But I can’t help you. So good luck with that.”
Lifetime prevalence estimates indicate that 5–20% of individuals with intellectual and developmental disabilities (IDD) and as many as 30–50% of individuals with autism spectrum disorder engage in self-injurious behaviors (SIB) such as headbanging, eye poking, biting, or skin gouging (Dimian & Symons, 2022). The tremendous negative impacts of these behaviors on quality of life for individuals and their families are well-documented (e.g.,Turnbull & Reuf, 1997), yet there is a paucity of research on the development of SIB or the experiences of caregivers seeking treatment for SIB.
There is, however, evidence that caregivers cannot reliably access treatments for challenging behaviors like SIB, despite advances in biobehavioral treatment options (Griffith & Hastings, 2014; Lunsky et al., 2014; Ruddick et al., 2015; Toms et al., 2015). Ruddick et al. described a significant discrepancy between the prevalence of challenging behaviors such as SIB in children with severe intellectual developmental disabilities (IDD) and those who were referred for, or received, services. Autistic adults involved in a participatory study described being dismissed for mental health services because “people like me don’t get support” (Camm-Crosbie et al., 2019, p. 1434). Healthcare disparities for people with disabilities are especially pronounced for individuals with IDD and mental health needs (Hall & Kurth, 2019; Iezzoni, 2011).
Outcomes for both caregivers and individuals with disabilities are poor without treatment. Without treatment, SIB is likely to continue and become more difficult to manage. Self-injury may become a chronic, intractable problem. For example, Taylor et al. (2011) reported that 84% of a study sample from 1987 still engaged in SIB in 2011. In a prospective cohort study, self-injury persisted in 44% of autistic individuals over ten years (Laverty et al., 2020). Family caregivers for individuals who engage in challenging behavior like SIB experience increased caregiver burden and stress and are vulnerable to lower well-being; unsurprisingly, these negative effects are worse without adequate access to information and services (e.g., Griffith & Hastings, 2014; Resch et al., 2010; Symons et al., 1999; Unwin & Deb, 2011). In the absence of support, caregivers may engage in dangerous practices to cope with SIB, such as physical restraint without safety training (Allen et al., 2006).
In addition to a lack of research on long-term treatment for severe challenging behavior, there is insufficient research on both access to SIB-specific treatment for individuals with IDD and the nature of treatment experiences. Frequently, researchers include SIB in the category of ‘challenging behavior’ or ‘problem behavior,’ typically defined as “self-injurious behaviour, physical and/or verbal aggression, destructiveness, inappropriate sexual behaviour, antisocial behaviour, disturbed sleep and overactivity” (James, 2013, p. 14). It is unknown whether SIB treatment access specifically differs from access for other challenging behaviors, or from other service delivery experiences, such as the experience of getting a diagnosis and services for autism (an area with a considerable research literature; Makino et al., 2019; Snijder et al., 2021).
A potential reason for the gap in SIB treatment services may be the everyday experiences of caregivers of individuals with SIB and IDD. The family caregiver perspective is crucial to understanding why the treatment gap exists and how researchers and practitioners can support family caregivers who are caring for a child or adult with SIB. The role of parent and family systems in developmental outcomes is robustly recognized by the research literature (Head & Abbeduto, 2007). This suggests that the knowledge and attitudes that a parent or a caregiver has about SIB and available treatments would influence the child’s developmental outcomes.
The primary goal of this study was to explore the experience of accessing treatment for SIB in individuals with IDD from the family caregiver perspective. The central research question for this study is: What are the treatment experiences of family caregivers for individuals with IDD for SIB? The subquestion of this analysis is: What are the experiences of family caregivers in interactions with providers for the treatment of SIB in individuals with IDD? The term ‘provider’ may refer to any service provider from across the medical, educational, and allied health disciplines providing services to address the issue of SIB. These research questions are broadly articulated and focused on the essence of an experience in the tradition of phenomenological research (Creswell & Poth, 2018). By harnessing the lived experience of family caregivers who cope with SIB each day, we aim to better understand the treatment gap, why it exists, and what can be done to close it.
Methods
We chose a qualitative interview approach, to gather a depth of experiential knowledge. Qualitative methods are especially suited to capture the complexities of disability in the social context; specifically, they are ideally suited to “illuminating the often hidden interactions of cultural attitudes, institutional processes, public policies, and individual lives” (O’Day & Killeen, 2002, p. 10). In the following sections, our approach is described in detail in pursuit of transferability (Anfara et al., 2002; Lewis et al., 2014).
Philosophical Assumptions
There are three primary epistemological and ontological assumptions underlying this work. In accordance with critical disability theory, the researchers believe that disability is a dimension of human difference and not a defect, the meaning of a disability depends upon the social context, and systemic ableism exists and influences participant experiences. Relatedly, the researchers accept the social constructivist idea that individuals construct subjective meaning of their experiences and it is the researchers’ duty to value and accept a complexity of viewpoints co-constructed by historical and cultural norms (Creswell and Poth, 2018). For example, in accordance with our philosophical assumptions, we allowed the participant to self-define what qualifies as a chronic case of SIB, given the guideline that we were interested in SIB severe enough to interfere with daily life. Finally, this work is oriented toward pragmatism, with real-world applications a primary goal of this research.
Positionalities
We, the first and second authors, engaged in reflection on our personal orientations toward the issue of SIB and discussed with each other how our positionalities (i.e., our personal positioning in relation to the study topic and context) might influence our analysis (Braun & Clarke, 2021). The first author identifies as a semi-insider perspective in some ways; she is a caregiver for her brother, who has intellectual and developmental disabilities and engages in severe, entrenched SIB, though she is not currently his primary caregiver. The second author identifies as an outsider perspective, though she has experience as an educator for individuals with IDD who engage in SIB.
Ethics
This study was approved by the University of Minnesota Institutional Review Board. Eligible participants (see below) completed an informed consent process which included the purpose of the study and explanation of the right of participants to terminate their participation at any time. Prior and during the interview process, the researchers engaged in reflexivity regarding the ethical issues inherent in qualitative health research with sensitive topics, including issues of therapeutic interviewing, relational boundaries, and emotional impact for both researcher and participant (Kendall & Halliday, 2014). In this context, reflexivity refers to an intentional process of reflection and self-awareness through journaling and peer debriefing intended to enhance methodological and ethical rigor in the interview process. During the interviews, the researcher worked to cultivate an interview environment in which participants felt comfortable and used active listening skills. When participants became emotional, the researcher responded with empathy and a reminder that they could end their participation or take breaks at any time. Following data collection, the data was deidentified and stored securely on a Box server (including journaling documents).
Participants
Participants were recruited through convenience and snowball sampling via online support groups and personal networks. For example, this process included e-mailing parent support group listservs and asking participants for referrals from their social networks. An eligibility screening determined if they met the inclusion criteria: immediate family members over the age of 18 or legal guardians with direct involvement in the care for an individual with IDD who engages in SIB that is significant and pervasive enough to interfere with daily life. As this is an initial inquiry with a broad aim, a specific sample population, and an expectation of high-quality dialogue given the interviewer’s semi-insider status, n=15 was determined as the sample size according to the concept of information power (Malterud et al., 2016).
The participants were primarily mothers with one sibling and one father (Table 1). They were primarily white, non-Hispanic, well-educated, employed, and with an annual income greater than $50,001 (Table 1). They were located in Colorado, Minnesota, Idaho, Florida, and California. The family members they cared for were primarily white and the most common diagnoses were autism and developmental delay (Table 2). All but one caregiver indicated their family member had multiple IDD diagnoses. Nine individuals with IDD were male and four were female. Participants reported a variety of SIB topographies and all but one reported multiple topographies of SIB (Table 2). Two participants did not report demographic information.
Table 1.
Caregiver demographics
| Characteristic | n(13) | % |
|---|---|---|
|
| ||
| Gender | ||
| Male | 1 | 8% |
| Female | 12 | 92% |
| Nonbinary/other | 0 | 0% |
| Caregiver Relationship | ||
| Mother | 11 | 85% |
| Father | 1 | 8% |
| Sister | 1 | 8% |
| Race | ||
| white | 12 | 92% |
| Black or African American | 1 | 8% |
| Ethnicity | ||
| Non-Hispanic | 13 | 100% |
| Hispanic | 0 | 0% |
| Education level | ||
| Less than high school degree | 0 | 0% |
| High school graduate | 1 | 8% |
| Some college but no degree | 3 | 23% |
| Associates degree | 1 | 8% |
| Bachelor’s degree | 3 | 23% |
| Master’s degree | 4 | 31% |
| Doctoral degree | 0 | 0% |
| Professional degree | 1 | 8% |
| Employment status | ||
| Working (paid employee) | 7 | 54% |
| Working (self-employed) | 2 | 15% |
| Not working | 4 | 31% |
| Income | ||
| Less than $10,000 | 1 | 8% |
| $10,001-$50,000 | 1 | 8% |
| $50,001-$100,000 | 3 | 23% |
| $100,001-$149,999 | 4 | 31% |
| Prefer not say | 4 | 31% |
Note: Two participants did not provide demographic information. Participants were permitted to select more than one race. Percentages are based on reported data.
Table 2.
Individual with IDD demographics
| Characteristic | n(13) | % |
|---|---|---|
|
| ||
| Gender | ||
| Male | 9 | 69% |
| Female | 4 | 31% |
| Nonbinary/other | 0 | 0% |
| Race | ||
| white | 12 | 92% |
| Black or African American | 1 | 8% |
| Asian | 1 | 8% |
| Ethnicity | ||
| Non-Hispanic | 12 | 92% |
| Hispanic | 1 | 8% |
| Diagnosis | ||
| Developmental delay | 11 | 85% |
| Autism | 10 | 77% |
| Chromosomal or genetic linked syndrome | 1 | 8% |
| Visual impairment or blindness | 2 | 15% |
| Deaf or hard of hearing | 1 | 8% |
| Other | 9 | 69% |
| SIB Topographies | ||
| Hits self with body part | 12 | 92% |
| Hits self against surface or object | 9 | 69% |
| Hits self with object | 5 | 38% |
| Bites self | 8 | 62% |
| Pulls hair or skin | 7 | 54% |
| Rubs or scratches self | 7 | 54% |
| Inserts finger or object | 5 | 38% |
| Skin picking | 6 | 46% |
Note: All information about the individual with IDD is caregiver-reported. Respondents were permitted to select more than one race, diagnosis, and SIB topography. The SIB topography information was collected via the Self-Injurious Behavior Subscale of the Repetitive Behavior Scale-Revised (RBS-R; Bodfish et al., 1999). Two participants did not complete survey information for their family member. Percentages are based on reported data.
Procedure
Upon first contact with the researchers, participants completed an eligibility screening via Qualtrics. The first author followed up via e-mail to confirm their eligibility, gain informed consent, and schedule the virtual interview. Participants completed a survey before or after the interview, which included demographic data and the Repetitive Behavior Scale-Revised (Bodfish et al., 1999; reported in Tables 1 and 2). The survey had a response rate of 87%; two participants did not complete the survey, despite reminders.
The interviews were conducted virtually, using Zoom, between March and July 2021 and lasted between 45 min and 2.5 hr. We used the automatic transcription and recording features of Zoom for data collection. The first author conducted fourteen interviews and the second author conducted one interview, because of previously established trust between the second author and the participant (i.e., the second author was previously the participant’s son’s teacher). At the start of the interview, the researcher re-introduced herself and the project, reminded the participant of their right to end the interview at any time, and alerted them that Zoom was recording. The interviews were semi-structured. See Table 3 for an excerpt from the interview protocol, noting that the term ‘providers’ was intentionally ambiguous to allow participants to discuss the types of providers most relevant to their circumstance. The first author disclosed her positionality as a semi-insider when she felt it was appropriate to earn the trust of the participant, but did so sparingly and thoughtfully, taking care not to deter the interview focus from the participant.
Table 3.
Interview protocol excerpt
| Questions | Additional probes |
|---|---|
|
| |
| When did you first realize that your family member was self-harming? Tell me about this realization and what came next. | If you initiated treatment, how did you know that it was time to seek treatment for your family member’s self-harm? If you initiated treatment, how did you go about seeking treatment? Who did you turn to? |
| Are you satisfied with the treatment your family member has received for self-harm? | If you are not satisfied, what do you wish you or providers had done differently? If you are satisfied, what treatment experiences have made you feel this way? |
| Imagine you have a friend who has a family member with similar disabilities as your own. This friend comes to you with concerns that their family member has begun engaging in self-harm. What would you suggest they do? | What would be the best way to inform people about how to find help? |
Data Analysis
The researchers edited the Zoom transcriptions for clarity, according to the video recording of the interview and uploaded the files into NVIVO software for qualitative coding. By conducting, viewing, editing, and transcribing the interviews, both researchers thoroughly familiarized themselves with the data (Braun & Clarke, 2006). The researchers engaged in an iterative process, involving open coding separately (a process of initial generation of concepts from the data), collaboratively discussing the data and developing a codebook, and continuing to gather and transcribe interviews while analyzing previously collected data. Codes and categories were added, renamed, and reorganized throughout the analytical process, consistent with an iterative and quasi-inductive approach. Discussion between the first and second authors aimed to deepen analysis rather than achieve consensus (Braun & Clarke, 2021).
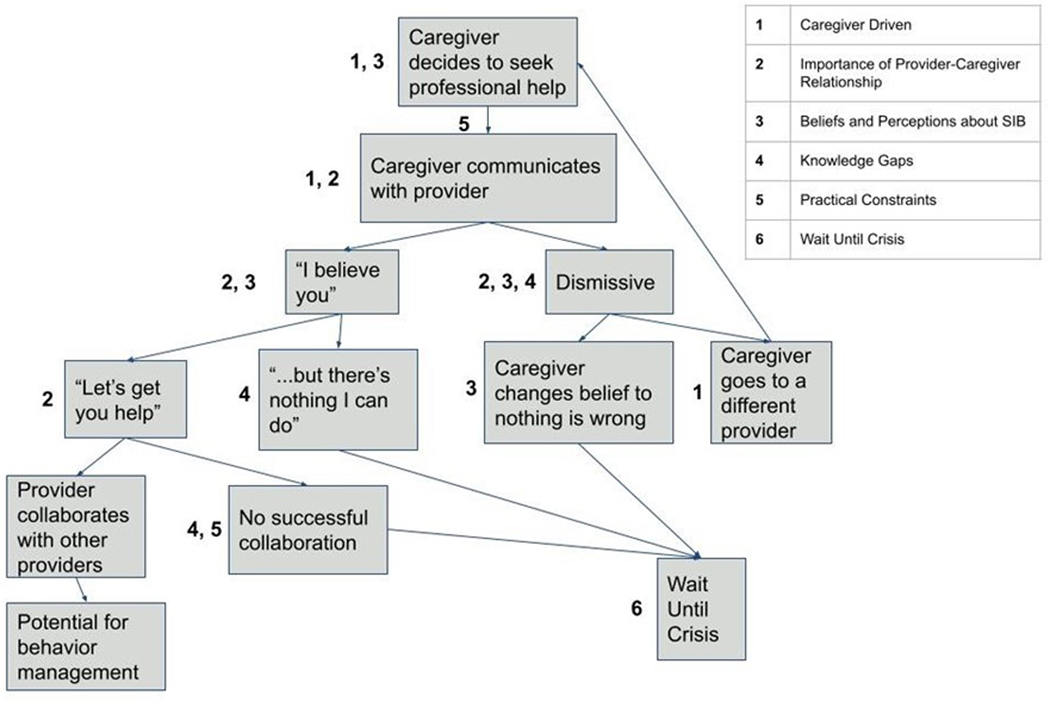
Following data collection and open coding of all 15 transcripts, the first and second authors visualized the codebook of categories and codes with a concept map (i.e., we conceptualized connections between codes and working themes on a whiteboard). The data included a richness beyond the initial research question, such as exploration of the caregiving experience and family stress. It was at this point that we decided to focus on interactions with providers for the initial analysis. We began a second stage of coding in which we individually wrote memos for each code under the category of Interactions with Providers. Each researcher, independently, re-read the coded data and wrote reflections, connections, and other thoughts; we then met and deepened our analyses through conversation. This systematic process led to revising and reworking potential themes. At this stage, we understood the data deeply enough to apply what we had learned to our second variable, the process of accessing treatment. We then developed the working model of treatment pathways, presented in Figure 1. We presented our findings to our research team for peer debriefing. Throughout the process, we maintained a thorough audit trail, revisited philosophical assumptions as needed, and engaged in ongoing reflexivity.
Figure 1.
This working model represents caregiver pathways to treatment from the decision to seek professional help for self-injury. Numbers along the pathways correspond to themes as described in the legend.
Results
Participants described substantial barriers to effective treatment access at multiple levels. Our analysis led to the development of six themes to describe the participants’ treatment experiences as they relate to interactions with providers. The themes are described in detail in the following sections. In summary, (a) primary caregivers tend to shoulder the responsibility of treatment access (Caregiver Driven), (b) treatment access tends to be a relational process (Importance of the Provider-Caregiver Relationship), (c) the caregiver’s and the provider’s beliefs and perceptions of the SIB influence each other and treatment (Beliefs and Perceptions about SIB), (d) there are multiple gaps in treatment knowledge and case knowledge (Knowledge Gaps), (e) systemic practical constraints influence the caregiver-provider interaction (Practical Constraints), and (f) there is a tendency to put-off intervention until the SIB leads to a crisis such as severe injury (Wait Until Crisis). We found that although we did not ask participants to discuss a certain type of provider, participants tended to focus on interactions with providers in a medical context, particularly pediatricians and other primary care providers, and psychiatrists and psychologists.
Caregiver Driven
The Caregiver Driven theme describes the assumption of caregiver responsibility to initiate, coordinate, follow-up, follow-through, and ensure the treatment of the individual with SIB. This came up either implicitly or explicitly in all interviews. Some participants described the isolation and burden of the responsibility to procure and sustain treatment directly (e.g., “I definitely feel that it has all been mother-driven”). Other participants described more implicit barriers: they did not expect or anticipate proactive support from providers as they experientially learned that treatment access required persistent and ongoing “pushing.” The word pushing, or similar words, occurred repeatedly across interviews: “about three years ago is when we started doing the medication intervention. And that was mostly because I pushed for it,” “so I kept pushing and [name redacted] received the diagnosis of autism spectrum disorder at about nine years old.”
Although a few participants mentioned partners, professionals, or other family members who shared this responsibility, for most participants, there was a primary caregiver (most often a mother) who consistently held the responsibility of treatment access. In some cases, the primary caregiver went to remarkable lengths in pursuit of treatment, including in-depth research of medications and treatments in medical libraries (pre-internet), lawsuits and legislation, parenting classes, and traveling long distances for specialty care (particularly for participants from rural areas). For some caregivers, particularly older caregivers who had been seeking treatment for many years, advocacy had become a deep part of their identity and extended beyond their own adult child to the needs of their community.
This theme was inextricable from descriptions of individual, dyadic, and family stress. Ongoing pursuit of care was often stressful in and of itself, as well as motivated by the urgency of enormous family stress: “there’s only so much we can take on in terms of supporting her,” “I just remember thinking, I don’t want to live my life this way…I just pictured myself at eighty trying to restrain my big fifty-five-year-old,” “he was starting to get more violent towards us,” “when he has these fits I’m just trying to protect the two-year-old.”
This led to a paradox for caregivers of limited physical and emotional energy: as the SIB became more severe, the need for treatment and support from outside the family increased, but the energy of caregivers was depleted by coping with the severe SIB. Caregivers had little remaining energy to drive access to treatment, which required mental, physical, and emotional labor. Specifically, this labor involved logistically coordinating visits with new providers and also re-living the chronic trauma of SIB in every conversation seeking help.
Caregivers had varying reactions to this paradox, which seemed to align with where they were in the process of acquiring care. If the onset of the SIB was relatively new (within the last few years), caregivers were in the midst of going through multiple providers and multiple treatment types. Although they may have been angry and frustrated, they still retained enough energy and hopefulness to try new approaches and see new providers. Conversely, caregivers for adults who had entrenched SIB that occurred for many years frequently exhibited symptoms of burnout and described their efforts to drive treatment access in the past. However, these caregivers tended to have a sense of hopelessness about new treatments in the present. Although the SIB was frequently still an ongoing, sometimes severe, problem, older caregivers had little interest or energy to try new treatment approaches beyond what they had already found helped to manage the behavior. One caregiver summarized this sense of stagnation in the following way:
“Parents become… they’re disconnected from what they’re doing in relation to managing their child and their child’s injury and the genesis of the problem…They stop seeking solutions, because they get either shunned or ridiculed or put off or their insurance won’t pay or- you know, people are disrespectful or whatever it might be, you know, the bureaucracy doesn’t understand what they need, you know, and it just becomes- they’re resigned to taking care of this. Rather than, how am I going to get out of this? How am I going to get my child served without me, you know, being the heart and soul of every single act and action?”
In the last sentence above, this participant succinctly summarizes the Caregiver Driven theme and expresses one of its great dangers: when a primary caregiver is unable to drive treatment access for an individual with IDD who self-injures, what then?
Importance of Caregiver-Provider Relationship
Positive experiences came from positive caregiver-provider relationships, regardless of type of provider. When caregivers described positive experiences with providers, they tended to report that the provider made them feel listened to and supported, rather than the provider having special sort of expertise. When talking about a positive experience with a provider, caregivers emphasized a sense of feeling listened to (“he just listens to me,” “he listened to me…he would take my calls”) and lucky (“extremely lucky… I mean we’re talking really lucky,” “it’s very lucky,” “we’re probably lucky,”) as well as validated in their sense of urgency (“Dr. [name redacted] gets it. He understands that it can kill you.”) Their favorite providers tended to be those they had known a long time and who they felt knew their family well (they held case knowledge; see Knowledge Gaps theme). They were willing to go above and beyond when necessary, such as one family’s experience of a doctor helping them to access Medicaid.
Likewise, many descriptions of negative experiences emphasized how the provider made the participant feel: dismissed, reprimanded, hopelessly unusual, judged, like a burden, or a general sense of being misunderstood. They described bringing in pictures of injuries as “proof,” because the provider didn’t believe the SIB was as severe as the caregiver said. Multiple caregivers described “panicked” phone calls and crying, out of desperation to make the provider believe them and adopt their sense of urgency. One mother described relief at her son’s meltdown in the primary care doctor’s office, in which he headbanged on the wall of the waiting room: “at least the doctor saw it.”
Relationships also had the power to open-up or limit care options. One caregiver described when a neurologist refused to see her as he had heard from other providers that she was a “hysterical parent.” Getting an appointment with a provider was sometimes the result of social capital: “we are actually personal friends with [name redacted],” “I finally got him into a psychiatrist, after I served on this board of directors,” “one of my friends had worked for five years at [name redacted].” This demonstrates privileged interaction with the care system for well-connected individuals, particularly given the high socioeconomic status and educational levels of the participants (see Table 1). One mother, who was also a leader in her local disability community, described how her son’s care relied upon her status:
“The only way that I’ve been able to get anything is by doing the research myself. And then researching and talking to, I don’t know how many people, because I’m really well- connected. I mean I’m in meetings all the time with all these different people who are in this business. So, my ability to find somebody to help him is like, probably 100 times better than the typical family. And I still haven’t succeeded.”
Beliefs and Perceptions about SIB
As discussed in the methods section, the researchers assumed a philosophy of social constructivism. The researchers aimed to honor the complexity of meanings of SIB, treatment, or management, and other ambiguous concepts. This theme describes how those beliefs and perceptions play a role in treatment access.
Across families, the meaning of SIB varied, in terms of topography of behavior (skin picking versus headbanging; see Table 2), and also in more subtle ways, such as the delineation between a behavior which is injurious and a behavior that is restricted, repetitive, or nonnormative. For many caregivers, restricted and repetitive behaviors were typical for their child or sibling with disabilities. There was not a clear distinction between a behavior that was of little concern and a dangerous behavior that was likely to become a strong part of their behavioral repertoire. Caregiver judgment was therefore paramount.
Often, the caregiver’s personal beliefs and perceptions of the behavior(s) were dynamic, changing across time and susceptible to influence by professionals, particularly at the early stages of behavior onset and diagnosis. At the point at which the caregiver first sought help from outside the family system, a belief change had occurred: the behavior was no longer ‘nothing to worry about,’ but perceived as (potentially) an issue in need of treatment. It was at this critical point that a provider’s own beliefs and perceptions had the power to shift the caregiver’s beliefs and perceptions one way or another.
For participants, provider beliefs at this stage frequently shut-down treatment. There was an overall lack of a sense of urgency by providers. Caregivers recounted dismissive comments from healthcare providers at early consults: “no no no he’s not autistic in any way,” “they don’t see it as a big issue,” “most of them don’t take it very seriously,” “oh no he’s just a little boy… that’s just what boys do,” “oh he’ll just knock himself out eventually,” “well that’s just autism,” and even “I don’t care.” These comments clearly remained with participants, who often relayed them years after they were uttered. Generalizations of providers such as “they don’t take it very seriously” tended to come from caregivers of older individuals who had emitted SIB for a long time.
Another crucial belief was the extent to which the caregiver believed SIB is treatable, curable, or manageable. Again, these beliefs were susceptible to influence by providers and often changed across time. As discussed in the Caregiver Driven theme, the time since SIB onset seemed to play a role in these beliefs. Caregivers newer to SIB tended to believe in the treatability and even curability of the SIB more than caregivers who had been managing SIB for many years, who often had witnessed years of SIB and many failed treatment interventions, which likely influenced their beliefs.
Culpability, and fears of misplaced culpability, were another relevant belief. Caregivers described fears of being accused of abuse; they proactively overexplained bruises and feared misunderstandings that could lead to the involvement of law enforcement or Child Protective Services: “Who wants to bring your kid to the doctor worrying that the doctor is gonna call the ambulance and the cops?” This fear was especially pronounced for caregivers of nonverbal individuals who expressed themselves idiosyncratically: “things could be interpreted in different ways, like I have a neighbor who…she called me, she’s like, is everything okay? And my daughter actually had been laughing hysterically. She was really happy, but she thought she was screaming, like crying and upset.” These fears exist within a context of isolation. Although caregiving for someone with IDD is already an isolating, stigmatizing experience for many, SIB exacerbates the feeling of isolation: “I mean there are families that are fearing for their lives. I mean they’re- I mean I’m sure you understand this, they’re so isolated in their homes. You know, even before the pandemic. They couldn’t go out, you know, they have to lock children in their rooms to keep themselves safe and they’re afraid.” Perceptions of SIB as very rare, shameful, and even impossible, lead to a context of stigma, isolation, and fear of caregivers and providers attempting treatment.
Knowledge Gaps
This theme represents gaps in knowledge and knowledge translation as they relate to the treatment of SIB, both in general and in specific cases. We identified five gaps in knowledge or knowledge translation that impeded treatment: (1) Providers lack the necessary knowledge or training to provide care (“they had no clue about autism”); (2) The belief that the knowledge does not exist (as stated in the previous theme, a belief that SIB is not treatable; i.e. science has not advanced enough to treat SIB); (3) Providers have the necessary knowledge, but they will not pass it on to caregivers (a caregiver perception that the providers don’t care, or are unwilling to speak frankly with caregivers); (4) Providers do not have the case knowledge of the caregivers necessary to treat an individual (see below); and (5) Providers do not share knowledge with other providers involved in an individual’s care (collaboration is minimal or nonexistent).
These knowledge gaps refer to two necessary types of knowledge: treatment knowledge and case knowledge. Treatment knowledge includes knowledge of the treatment options available, what will work best in a given case, and medical and behavioral expertise. Case knowledge is the in-depth understanding of the individual and their needs, including who they are, their behaviors, and their family and caregiver context. Both types of knowledge are necessary for effective intervention.
The case knowledge gap is exemplified by the following quote:
“It’s not like you can ask the medical community or the educational community, the therapy community, none of them have the answers. They just all will try to help from their individual discipline, but they are not the family who sees the whole picture and who is trying to have a semi-decent life day to day.”
This mother describes how providers from different disciplines miss the reality of daily life with SIB and severe disability. To connect back to previously discussed themes, understanding of the daily reality of caregivers of individuals with SIB and IDD (case knowledge) comes from positive relationships between caregivers and providers and alignment of beliefs and perceptions of SIB. Without these, the third knowledge gap tends to occur, in which caregivers believe that providers are unwilling to pass on critical knowledge about treatment. Over time, this tends to lead to caregiver burnout and a resulting stagnation of treatment access, as discussed in the Caregiver Driven theme. It may also lead to the second knowledge gap, the belief that treatment for SIB does not exist, particularly when a provider insists that SIB is not treatable: “And the doctors couldn’t do anything about that. Yeah that’s just how [people with intellectual disabilities] are, that’s just, you know, that’s just what you get.”
Practical Constraints
The Practical Constraints theme describes systemic and practical constraints that impede treatment access including insurance issues, bureaucratic red-tape, inflexibility of treatments, unreasonable distances to travel for specialists, and provider workforce shortages. These broader issues influence the dyadic interaction of caregivers and providers, as providers must operate within systems of care such as hospitals or clinics, and caregivers receive care within those systems and interact with other systems, such as insurance companies and social services.
A parent described the barrier of apparent inflexibility of intensive Applied Behavior Analysis (ABA) treatment, often provided at a dosage of 40 hours per week: “So if we continue with ABA, can I survive?… that problem is much more complicated because I’m navigating this thing as basically an unemployed and unemployable single parent.” Many caregivers echoed frustrations of getting appointments with providers, child psychiatrists in particular, a field with a well-documented workforce shortage (Harris, 2018): “We couldn’t get an appointment with a psychiatrist,” “it took five months to get in to see the developmental pediatrician which I guess nowadays is amazing,” “I would drive an hour and a half north of here to do video appointments,” “we were like, number 628 on the waitlist.”. A caregiver reported difficulties with the standard 20-min appointments being sufficient for the exchange of case and treatment knowledge: “I don’t think they have enough time to gather enough information.” Families who had experienced emergency room or in-patient services sometimes found themselves stuck within a system of care ill-fit to their needs: “They said, you can just take him back home, or continue to languish in the ER for weeks on end.” Although systemic issues are not the focus of this study, these quotes demonstrate how practical constraints influence the dyadic level of caregiver and provider interactions.
Wait Until Crisis
The culmination of the preceding themes is the caregiver perception that, more often than not, they do not receive help proactively. This theme is exemplified by these quotes: “Nobody wants to help you until the ambulance comes,” “It’s like a secret, you know? No one really wants to help until it gets really bad.” Wait Until Crisis refers to the pattern of delaying intervention, the urge to “wait and see,” sometimes on the part of both the provider and the caregiver, and ultimately leading to moments of family crisis. These moments of crisis were typically moments of especially severe SIB or aggression to others, that resulted in severe, sometimes permanent injury, hospitalization, or the involvement of law enforcement.
Caregivers resign themselves to the understanding that the emphasis on early intervention for other areas of their child or sibling’s life has not reached SIB. They encounter providers who have little to offer until the SIB is severe enough to warrant emergency hospitalization, heavy psychotropic medications, a padded room, or mechanical restraints. Caregivers, in some cases, do not feel ready to try certain treatments until the SIB is severe enough that they feel they have no other option:
“[Interviewer:]: If you had tried risperidone a little bit sooner, that might have changed things.
[Participant:]: That’s true. That’s true. But then would I have been as willing?”
In this way, the perceptions of severity can influence the tendency to postpone interventions, from both the provider and the caregiver. So can knowledge gaps, if providers do not know of treatment interventions other than the most invasive. Practical constraints may lead to a tendency to delay intervention, such as waitlists or insurance issues. Through no fault of their own, the exhaustion from having to strenuously push for care may lead caregivers to tend to wait. Each of the preceding themes are connected to the overall tendency to Wait Until Crisis, as described in Figure 1.
Discussion
The primary research question of this study was: What are the treatment experiences of family caregivers for individuals with IDD for SIB? This analysis focused on the subquestion: What are the experiences of family caregivers in interactions with providers for the treatment of SIB in individuals with IDD? We aimed to address these questions through the thematic analysis of fifteen semi-structured interviews with family caregivers.
The interviews were rife with negative emotionality, including sadness, anger, and expressions of chronic stress. Caregivers expressed the exhaustion of daily coping combined with the frustration of inadequate treatment access and effectiveness. Stress was compounded by negative interactions with treatment providers and alleviated by positive interactions. This overall impression and the participants’ descriptions seemed to confirm the treatment gap and the power of the provider to either bring relief to families struggling with SIB or deepen their frustrations.
In the analysis process, we noticed connections between themes and how the data fit into pathways of acquiring treatments. Figure 1 describes a working model of treatment pathways from the point of the caregiver’s initial decision to seek professional help for SIB for their family member. Figure 1 is intended to integrate the themes from our analysis and reflect how treatment acquisition is an ongoing and dynamic process. Further, we believe the complexity of treatment access is better represented with a pathway model such as Figure 1 rather than as a dichotomous variable (i.e., treatment is either accessed or not accessed). Figure 1 was developed through in-depth analysis of the many stories and experiences shared in interviews. Participants described traveling these pathways many times; their frustrations came from getting stuck with dismissive or unhelpful providers over and over again. This left caregivers in a seemingly endless loop of fruitless help-seeking until they reached crisis. They then returned to help-seeking when short-term crisis interventions ended (e.g., emergency room visits).
The first stage of treatment acquisition is not necessarily behavior onset, but onset of the caregiver’s belief that professional help is needed (Beliefs and Perceptions about SIB). The distinction acknowledges that many caregivers attempt to cope with challenging behaviors within the family system before seeking help from professionals. When the caregiver seeks a provider, they may encounter various barriers, such as the long waitlists and unreturned phone calls many participants described (Practical Constraints). Finding an appropriate provider and getting an appointment likely requires perseverance and persistence by the primary caregiver (Caregiver Driven). In the initial consultation, the caregiver and provider must develop rapport and trust, despite the sensitive nature of the presenting problem and possible systemic barriers, such as short appointments (Importance of the Caregiver-Provider Relationship, Practical Constraints). Crucially, the provider must believe the caregiver and perceive the behavior as in need of treatment (Beliefs and Perceptions about SIB). The provider must have sufficient treatment and case knowledge (Knowledge Gaps). The provider must be willing and able to collaborate with others (Practical Constraints, Knowledge Gaps), as treatment for SIB usually involves a combination of biological and behavioral approaches. The caregiver repeats this process with other providers who are able to offer complementary treatments or begins again if they are dismissed upon initial consultation (Caregiver Driven). As evident in Figure 1, if this process does not progress past each of these stages, the result is to Wait Until Crisis.
These findings are consistent with other areas of research on treatment access not specific to SIB. In focus groups with parents of children with fragile X syndrome, Down syndrome, or autism, Minnes and Steiner found common stressors in “dealing with the healthcare system,” “negotiating relationships with practitioners,” and a unanimous concern about clinician’s lack of knowledge of IDD (2009, p. 255). In our framework, these findings would map onto the Practical Constraints, Importance of the Caregiver-Provider Relationship, and Knowledge Gaps themes, respectively.
Wright et al.’s (2015) meta-analysis of pathways to care for Attention Deficit Hyperactivity Disorder (ADHD) is a model paper in this area because of its well-developed evidence base and comprehensive representation of the complexity of treatment access+. Barriers and facilitators identified in 27 papers in the categories of Wider Determinants, Identification of Need, Entry and Continuity of Care, and Interventions to Improve Access to Care contribute to a thorough, mixed methods description of ADHD care pathways at multiple levels (Wright et al., 2015). Many of Wright et al.’s findings align with the results of the current study, yet also demonstrate a complexity of treatment systems that is not captured in this initial inquiry. For example, Wright et al. identified the importance of parent perception in the process of identification of need; in ADHD, this manifested as parental perceptions of hyperactivity as a serious problem (e.g. Sayal, Taylor, Beecham & Byrne, 2002). Two studies in this meta-analysis found that parent race and ethnicity influenced this perception. For example, Black mothers endorsed hyperactivity, impulsivity, and concentration more frequently than white mothers (Hillemeier et al., 2007 as cited in Wright et al., 2015). This is just one example of the many variables yet to be explored for SIB in IDD and treatment access. Following significant further research, it may be beneficial to model an analysis of treatment access for SIB in IDD after the Wright et al. meta-analysis of ADHD treatment access.
Practical Implications
This research demonstrates the power of the provider to support families affected by SIB by preventing crisis and promoting coping. There are multiple potential points of intervention in Figure 1 to increase access to prevention-oriented, collaborative, effective, family-oriented treatment.
At the dyadic level, providers can evaluate their beliefs and perceptions of SIB, strive for positive relationships with caregivers and their family members with disabilities, and build their expertise on the topic. Providers can recognize and address threats to caregiver morale by acknowledging the stress and complexity of seeking care for a family member with IDD and SIB. As discussed in the theme Importance of the Caregiver-Provider Relationship, active listening and validation can help establish trust. To establish productive and consistent beliefs and perceptions about SIB, providers can build and communicate treatment knowledge and actively seek case knowledge. This is consistent with existing research on health disparities for individuals with intellectual disabilities, which emphasizes the need for improved knowledge and skills related to serving patients with IDD, multidisciplinary approaches, and the particular importance of communication between caregivers, providers, and individuals with IDD (Krahn et al., 2006).
Of particular concern is the issue of diagnostic overshadowing, which in this context refers to the tendency to attribute SIB to the intellectual or developmental disability (e.g. “yeah that’s just how [people with ID] are, that’s just, you know, that’s just what you get.”) The diagnostic overshadowing bias has been shown with psychiatrists and clinical psychologists providing services for individuals with IDD and can contribute to the underdiagnosis of mental-health difficulties (Mason & Scior, 2004). Providers can overcome this bias through further education on the diagnosis, assessment, and treatment of SIB and reflections on their beliefs about the meaning of an IDD diagnosis.
Many of the barriers described in the Practical Constraints theme must be addressed at a systems level. Systemic intervention will promote positive provider-caregiver interactions and treatment provision for all healthcare needs of individuals with IDD. However, there is a particular urgency for this issue given the many barriers to treatment described in Figure 1 and the burden placed on caregivers to navigate the care system. For providers, changes in educational training systems are particularly needed, to prepare healthcare professionals for the complexity of caring for individuals with severe IDD and behavioral health needs. Primary care physicians, which many participants identified as their first point of contact, often lack experience with individuals with IDD and feel they are “operating without a map” (Wilkinson et al., 2012, p. 243).
Limitations
Despite these outcomes, there are several limitations to this qualitative analysis. First, we had limited sample diversity (Tables 1 and 2). The sample was primarily caregivers who are highly educated, white, of high socioeconomic status, and mothers. Some caregivers may have been less likely to volunteer for an unpaid interview, such as those with lower socioeconomic status, those who had encountered little difficulty in treatment acquisition, or those for whom SIB had resolved. This limits the generality of the findings, as it is likely that caregivers of different backgrounds may experience different barriers to, or more difficulty with, accessing treatment.
Second, it is important to acknowledge that this research was conducted during the COVID-19 pandemic. Although most participants reflected on events that happened prior to the pandemic, there is evidence that individuals with IDD and their family members were significantly more impacted by the pandemic than those without IDD (Courtenay & Perera, 2020). The impact of the pandemic on treatment access was not explored directly in this study, though some participants commented on ways the pandemic had exacerbated existing treatment barriers or created new barriers (such as lack of in-person therapy).
Third, although reflexivity was practiced, the first author’s lived experience with the issue of SIB in IDD may have produced bias in her interpretations of interview data, based on her experiences accessing treatment for her brother’s SIB. Fourth, the methods focused on the dyadic level of caregiver and provider interactions. The issue of SIB occurs in more complex systems that were not fully captured, such as the triadic interactions of individuals with IDD and their caregivers and providers, the interactions of co-caregivers such as parents, the complexities of a family system, or the contributions of professional caregivers. Fifth, the choice of qualitative interviews with family caregivers prioritized a depth of knowledge over breadth; future studies with mixed methodologies, across diverse samples and contexts, are needed to fully understand this issue, as are researchers with a variety of positionalities. Finally, we prioritized the voice of the caregiver. Caregivers can play an important role by giving voice to individuals with complex communication needs who otherwise may not be represented in research. However, when available, the voice of individuals with IDD should be included in research according to the tenet of disability justice: nothing about us without us.
Research Implications and Future Directions
Given the results of this qualitative analysis, there are several important areas of future research. First, it will be important to scale to the collection of survey data and provider interviews and focus groups, to facilitate the development of interventions to improve treatment access. These findings could be foundational for survey development specific to documenting the breadth of the treatment gap issue and enhance sample heterogeneity. Second, it will be important to examine the provider perspective, through provider interviews coupled with focus groups. This will be critical for the development of interventions that close the treatment gap for SIB in IDD. Finally, it will be important to examine caregiver interactions with specific provider types, such as providers from medical or educational settings. This could identify impacts unique to specific provider types, such as the provider’s ability to meet the needs of caregivers and family members with IDD. With this information, future interventions could be grounded in an implementation science approach, with attention to sustainment, scale-up, and spread in a public health or educational context (Hamilton & Mittman, 2018).
Conclusion
The issue of SIB in individuals with IDD is of urgent clinical significance. It is clear that for the families interviewed, the strain of coping with SIB is heightened by the inaccessibility of treatment. The treatment gap is complex, but this research also clearly points to the power of providers in facilitating treatment access and supporting families.
Acknowledgements
Support provided, in part, from Eunice Kennedy Shriver NICHD Grant No. 44763. We wish to acknowledge the contributions of the participants.
This study has been approved by the University of Minnesota Institutional Review Board STUDY0012016.
Footnotes
Conflict of Interest Statement
The authors report there are no competing interests to declare.
References
- Allen D, Hawkins S, & Cooper V. (2006). Parents’ use of physical interventions in management of their children’s severe challenging behaviour. Journal of Applied Research in Intellectual Disabilities, 19(4), 356–363. [Google Scholar]
- Anfara VA, Brown KM & Mangione TL (2002). Qualitative analysis on stage: Making the research process more public. Educational Researcher, 31(7), 28–38. [Google Scholar]
- Bodfish JW, Symons FJ, Parker DE, & Lewis MH (1999). Repetitive Behavior Scale–Revised. Journal of Autism and Developmental Disorders. [DOI] [PubMed] [Google Scholar]
- Braun V. & Clarke V. (2021). Thematic analysis: A practical guide. Sage. [Google Scholar]
- Braun V. & Clarke V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. [Google Scholar]
- Camm-Crosbie L, Bradley L, Shaw R, Baron-Cohen S, & Cassidy S. (2019). ‘People like me don’t get support’: Autistic adults’ experiences of support and treatment for mental health difficulties, self-injury and suicidality. Autism, 23(6), 1431–1441. 10.1177/1362361318816053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JW, & Poth CN (2018). Qualitative inquiry and research design (4th ed). Thousand Oaks, CA: Sage. [Google Scholar]
- Courtenay K, & Perera B. (2020). COVID-19 and people with intellectual disability: impacts of a pandemic. Irish Journal of Psychological Medicine, 37(3), 231–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimian AF, & Symons FJ (2022). A systematic review of risk for the development and persistence of self-injurious behavior in intellectual and developmental disabilities. Clinical Psychology Review, 94, 102158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith GM & Hastings RP (2014). ‘He’s hard work, but he’s worth it’. The experience of caregivers of individuals with intellectual disabilities and challenging behaviour: A meta-synthesis of qualitative research. Journal of Applied Research in Intellectual Disabilities, 27(5), 401–419. [DOI] [PubMed] [Google Scholar]
- Hall, & Kurth NK (2019). A Comparison of Health Disparities Among Americans With Intellectual Disability and/or Autism Spectrum Disorder and Americans With Other Disabilities. Inclusion (Washington, D.C.), 7(3), 160–168. 10.1352/2326-6988-7.3.160 [DOI] [Google Scholar]
- Hamilton AS & Mittman BS (2018). Implementation science in healthcare. Dissemination and implementation research in health: translating science to practice, 2, 385–400. [Google Scholar]
- Harris JC (2018). Meeting the workforce shortage: toward 4-year board certification in child and adolescent psychiatry. Journal of the American Academy of Child and Adolescent Psychiatry, 57(10), 722–724. [DOI] [PubMed] [Google Scholar]
- Hillemeier MM, Foster M, Heinrichs B, Heier B, & The Conduct Problems Prevention Research Group. (2007). Racial differences in parental reports of attention- deficit/hyperactivity disorder behaviours. Journal of Developmental and Behavioural Pediatrics, 28, 353–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laverty C, Oliver C, Moss J, Nelson L, & Richards C. (2020). Persistence and predictors of self-injurious behaviour in autism: a ten-year prospective cohort study. Molecular autism, 11(1), 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makino A, Hartman L, King G, Wong PY, & Penner M. (2021). Parent experiences of autism spectrum disorder diagnosis: A scoping review. Review Journal of Autism and Developmental Disorders, 8(3), 267–284. [Google Scholar]
- Iezzoni LI (2011). Eliminating health and health care disparities among the growing population of people with disabilities. Health affairs, 30(10), 1947–1954. [DOI] [PubMed] [Google Scholar]
- Kendall S, & Halliday LE (2014). Undertaking ethical qualitative research in public health: are current ethical processes sufficient? Australian and New Zealand Journal of Public Health, 38(4), 306–310. [DOI] [PubMed] [Google Scholar]
- Krahn GL, Hammond L. & Turner A. (2006). A cascade of disparities: Health and health care access for people with intellectual disabilities. Mental Retardation and Developmental Disabilities Research Reviews, 12(1), 70–82. [DOI] [PubMed] [Google Scholar]
- Lewis J, Ritchie J, Ormston R, & Morrell G. (2014). Generalising from qualitative research. In Ritchie J, Lewis J, McNaughton Nicholls C. & Ormston R. (Eds.), Qualitative research practice: A guide for social science students and researchers (2nd ed., pp. 347–366). London: SAGE. [Google Scholar]
- Lunsky Y, Tint A, Robinson S, Gordeyko M, & Ouellette-Kuntz H. (2014). System-wide information about family carers of adults with intellectual/developmental disabilities—a scoping review of the literature. Journal of Policy and Practice in Intellectual Disabilities, 11(1), 8–18. [Google Scholar]
- Malterud K, Siersma VD & Guassora AD (2016). Sample size in qualitative interview studies: guided by information power. Qualitative Health Research, 26(13), 1753–1760. [DOI] [PubMed] [Google Scholar]
- Mason J, & Scior K. (2004). ‘Diagnostic overshadowing’amongst clinicians working with people with intellectual disabilities in the UK. Journal of Applied Research in Intellectual Disabilities, 17(2), 85–90. [Google Scholar]
- Minnes P, & Steiner K. (2009). Parent views on enhancing the quality of health care for their children with fragile X syndrome, autism or Down syndrome. Child: care, health and development, 35, 250–256. [DOI] [PubMed] [Google Scholar]
- O’Day B. & Killeen M. (2002). Research on the lives of persons with disabilities: The emerging importance of qualitative research methodologies. Journal of Disability Policy Studies 13(1), 9–15. [Google Scholar]
- Resch JA, Mireles G, Benz MR, Grenwelge C, Peterson R, & Zhang D. (2010). Giving parents a voice: A qualitative study of the challenges experienced by parents of children with disabilities. Rehabilitation Psychology, 55(2), 139–150. [DOI] [PubMed] [Google Scholar]
- Ruddick L, Davies L, Bacarese-Hamilton M, & Oliver C. (2015). Self-injurious, aggressive and destructive behaviour in children with severe intellectual disability: Prevalence, service need and service receipt in the UK. Research in Developmental Disabilities, 45, 307–315. [DOI] [PubMed] [Google Scholar]
- Sayal K, Taylor E, Beecham J, & Byrne P. (2002). Pathways to care in children at risk of attention-deficit hyperactivity disorder. British Journal of Psychiatry, 181, 43–48. [DOI] [PubMed] [Google Scholar]
- Snijder MI, Langerak IP, Kaijadoe S, Buruma ME, Verschuur R, Dietz C, … & Oosterling IJ (2021). Parental Experiences with Early Identification and Initial Care for their Child with Autism: Tailored Improvement Strategies. Journal of Autism and Developmental Disorders, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Symons FJ, Koppekin A, & Wehby JH (1999). Self-injurious behavior and quality of life for persons with developmental disabilities. Mental Retardation, 37, 297–307. [DOI] [PubMed] [Google Scholar]
- Toms G, Totsika V, Hastings R, & Healy H. (2015). Access to services by children with intellectual disability and mental health problems: population-based evidence from the UK. Journal of Intellectual and Developmental Disability, 40(3), 239–247. [Google Scholar]
- Taylor L, Oliver C, & Murphy G. (2011). The chronicity of self-injurious behaviour: a long-term follow-up of a total population study. Journal of Applied Research in Intellectual Disabilities, 24(2), 105–117. [Google Scholar]
- Turnbull AP & Ruef MB (1997). Family perspectives on inclusive lifestyle issues for people with problem behavior. Exceptional Children, 63(2), 211–227. [Google Scholar]
- Unwin G. & Deb S. (2011). Family caregiver uplift and burden: Associations with aggressive behavior in adults with intellectual disability. Journal of Mental Health Research in Intellectual Disabilities, 4(3), 186–205. [Google Scholar]
- Wilkinson J, Dreyfus D, Cerreto M, & Bokhour B. (2012). “Sometimes I feel overwhelmed”: Educational needs of family physicians caring for people with intellectual disability. Intellectual and Developmental Disabilities, 50(3), 243–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright N, Moldavsky M, Schneider J, Chakrabarti I, Coates J, Daley D, … & Sayal K. (2015). Practitioner review: pathways to care for ADHD–a systematic review of barriers and facilitators. Journal of Child Psychology and Psychiatry, 56(6), 598–617. [DOI] [PMC free article] [PubMed] [Google Scholar]