Abstract
How to cite this article: Kumar R, Singh AK. “Right Lower Lobe Lung Pathology”: A Potential Mimic of Pneumoperitoneum. Indian J Crit Care Med 2024;28(12):1182–1183.
Keywords: Linear basal atelectasis, Pneumoperitoneum, Pseudo-pneumoperitoneum
A 75-year-old male presented to the emergency room in a lethargic state with ventricular tachycardia requiring unsynchronized cardioversion and cardio-pulmonary resuscitation. He was intubated, started on nor-epinephrine for hemodynamic support, and diagnosed with typhoid fever based on positive Typhi-dot IgM. Further investigations revealed mild anemia, acute kidney injury, and dilated cardiomyopathy with severe left ventricular dysfunction (EF 25%) and moderate tricuspid regurgitation on echocardiogram. Broad-spectrum antibiotics, supportive care, and antiplatelet therapy were initiated. His condition remained critical in the ICU.
Chest X-ray A-P view in supine position was done, clearly showing gas under the diaphragm (Fig. 1). Ultrasound abdomen was done, which showed no sign of pneumoperitoneum like a peritoneal strip sign or reverberation artifact. As the abdominal examination did not reveal any signs of peritonitis, and history was not consistent with bowel perforation, a CT abdomen was done to confirm the X-ray findings, which did not reveal any pneumoperitoneum, or bowel perforation or any intra-abdominal pathology. To evaluate further, a CT chest was done, which deciphered bilateral centriacinar and paraseptal emphysema with a large bulla in the right lower lobe posterior segment with underlying basal linear atelectasis (Fig. 2).
Fig. 1.
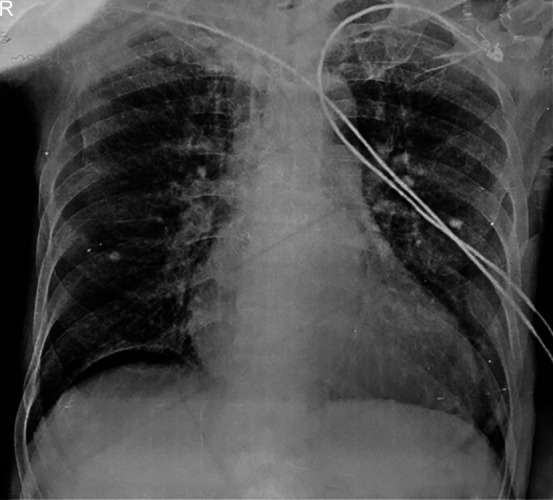
Chest X-ray supine A-P view showing gas under right hemidiaphragm
Fig. 2.
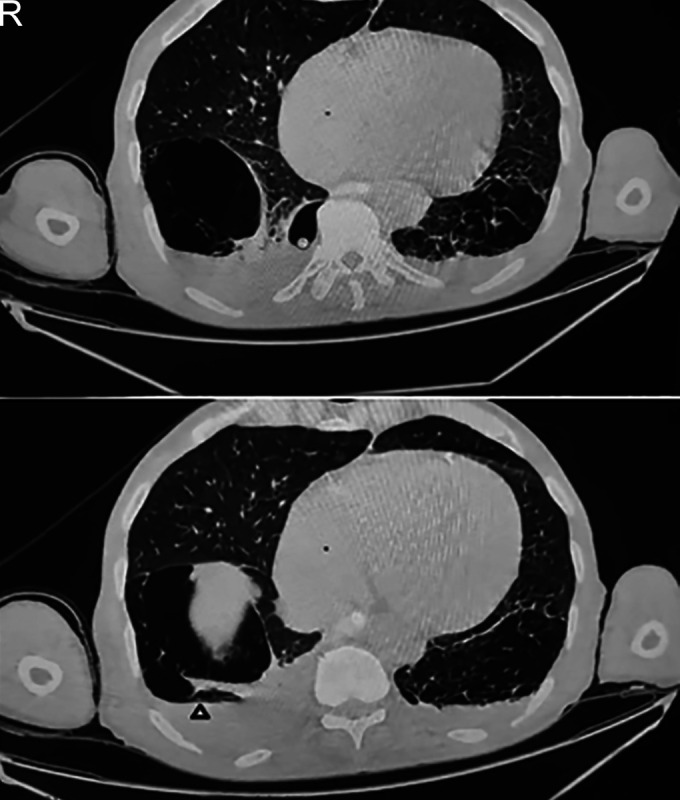
CT chest showing right lower lobe bullous lesion with underlying basal linear atelectasis (arrowhead)
Conservative management continued, cultures were negative and patient improved with time and discharged from hospital.
Discussion
Gas under the diaphragm on a chest X-ray is most commonly due to hollow viscus perforation. However, in 10% of cases can also be caused by various conditions such as pneumatosis coli, post-surgical status, or Chilaiditi syndrome etc.1–3
In this particular case, initially, X-ray findings showed gas under the diaphragm, whereas history and examination were not consistent with the same. An erect chest X-ray is considered highly sensitive for detecting free intraperitoneal gas because air naturally ascends, creating a distinct boundary between the diaphragm and the liver. In contrast, when the patient is supine, the air disperses across the abdomen and liver, making detection more challenging. In critically ill patients, a supine AP chest or abdomen X-ray is often the only feasible option. Therefore, a CT scan of the chest and abdomen was performed, which did not reveal any evidence of pneumoperitoneum or any colonic loops under the right hemidiaphragm (Chilaiditi syndrome) in the abdomen. Instead, it detected basal linear atelectasis in the CT chest, which can mimic gas under the diaphragm seen on an X-ray.
Despite an extensive review of the medical literature, no similar cases were identified. It is acknowledged that right lower lobe basal linear atelectasis, or bulla can sometimes mimic gas under the diaphragm. In such instances, the bulla exerts pressure on the basal lung, creating an appearance resembling free intra-abdominal air typically observed beneath the diaphragm.2,4 This underscores the importance of cautious interpretation of imaging findings and the necessity for thorough clinical evaluation to accurately differentiate between pneumoperitoneum and pseudopneumoperitoneum induced by bullous lung pathology. Further research and detailed case studies could provide additional insights into this unusual diagnostic challenge.
So when clinical suspicion is low for abdominal pathology despite X-ray findings, supplementary CT imaging is advisable to confirm the diagnosis and guide appropriate management, thereby avoiding unnecessary surgical interventions.
Orcid
Rishabh Kumar https://orcid.org/0000-0003-2574-3575
Ashutosh Kumar Singh https://orcid.org/0000-0002-4421-8090
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Ramachar Sreevathsa M, Melanta K. R gas under diaphragm. Int J Surg Case Rep. 2016;28:314–316. doi: 10.1016/j.ijscr.2016.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campos A, Johari A, Walizai T, Sharma R, Shah V, Botz B, et al. Pneumoperitoneum. Reference article, Radiopaedia.org. [online]https://radiopaedia.org/articles/pneumoperitoneum Available from: [Last accessed November, 2024] [Google Scholar]
- 3.Orangio GR, Fazio VW, Winkelman E, McGonagle BA. The Chilaiditi syndrome and associated volvulus of the transverse colon. An indication for surgical therapy. Dis Colon Rectum. 1986;29(10):653–656. doi: 10.1007/BF02560330. [DOI] [PubMed] [Google Scholar]
- 4.Lo BM. Radiographic look-alikes: Distinguishing between pneumoperitoneum and pseudopneumoperitoneum. J Emerg Med. 2010;38(1):36–39. doi: 10.1016/j.jemermed.2008.01.011. [DOI] [PubMed] [Google Scholar]


