Abstract
Stroke causes functional disabilities and reduces the quality of life of stroke survivors. This retrospective cohort study aimed to examine changes in health-related quality of life (HRQoL) six months after a stroke and the effect of stroke characteristics and sociodemographic factors on HRQoL. Participants completed a questionnaire that included the stroke characteristics, sociodemographic characteristics, and the 5-level European Quality of Life 5 dimensions (EQ-5D-5L) before discharge. Follow-up assessments of HRQoL were performed at one, three, and six months after discharge. Descriptive statistics and linear mixed models were used for data analyses. A total of 155 first-stroke patients were included, of which N = 152 patients completed follow-up assessments until six months. The mean EQ-5D-5L index score at discharge was 0.69 (SD 0.33). The trends of HRQoL significantly increased from discharge to three months, but there was no significant HRQoL improvement after three months. Considering stroke severity, mean HRQoL significantly improved for patients with no stroke symptoms, minor stroke, and moderate stroke (p < 0.05) but not those with severe stroke (p = 0.156). HRQoL among patients with sufficient monthly income significantly increased over six months (p < 0.05). HRQoL among patients with severe stroke and having insufficient income were poor. Supportive programs are required to improve their HRQoL.
Keywords: EQ-5D-5L, Health-related quality of life, Sociodemographic factors, Stroke, Thailand
Subject terms: Quality of life, Neuroscience, Neurology
Introduction
Stroke remains the second leading cause of death worldwide, accounting for 11.6% of total deaths. It is the third leading cause of disability combined (5.9% of total disability-adjusted life years (DALYs))1. Ischemic stroke had the highest incidence of all strokes (62.4%) in 2019, while the incidence of hemorrhagic stroke was 37.6%1. From 1990 to 2019, the incidence of stroke increased by 70.0%, the prevalence of stroke increased by 85.0%, and disability-adjusted life years due to stroke increased by 32.0%1. Major risk factors for stroke include higher age, hypertension, diabetes mellitus, metabolic syndrome, atrial fibrillation, and smoking2. Older patients with stroke often have worse outcomes than younger patients3,4.
Thailand is facing an older society. The proportion of the Thai population aged 60 years and over is projected to increase from 19.46% in 2022 to 31.37% in 20405. Stroke is a major leading cause of death and disability in Thailand6,7. It was reported as the highest rank of DALYs lost in Thai females and the third in Thai males8. Patients with stroke were estimated to lose 10.27 quality-adjusted quality of life years (QALYs), about 8.41 QALYs for ischemic stroke, and 16.15 QALYs for intracerebral hemorrhage patients9.
Advanced medical interventions could reduce the mortality rate after a stroke10. However, more than half of stroke patients currently experience disability or neurological deficits10–12. Neurological deficits from stroke are varied, such as cognitive, physical, or psychological impairments, depending on the location of the stroke lesion and the severity of the stroke13,14. Stroke consequences cause functional disabilities in performing basic or advanced daily activities or working abilities and mental disturbances. Those consequences could reduce the quality of life in stroke patients11,15,16. The optimizing recovery of stroke patients varies within the first few months and can continue for up to six months17. The suggested golden period of post-stroke recovery is within three months after a stroke18. The stroke recovery outcomes depend on the location of stroke lesion, stroke subtypes, stroke severity13,14,17, age, gender, and comorbidity3,4,19.
Quality of life (QoL) was often assessed to investigate improvements in health-related problems17,20,21. Health-related quality of life (HRQoL) is a multidimensional concept used to evaluate the impact of health status on quality of life, covering physical and mental health status20. Most studies have shown that the HRQoL in stroke patients decreased after they had a stroke9,21–23. Studies on HRQoL are beneficial to identify the burden of strokes on an individual’s life. Understanding the dynamic changes in HRQoL of stroke patients after hospital discharge may help manage appropriate supportive programs for stroke victims. This study assessed HRQoL of stroke patients from hospital discharge to one month, three months, and six months to investigate patterns of changes in HRQoL within 6 months. Moreover, this study examined effects of stroke characteristics and sociodemographic data and time on HRQoL. The findings would help to explain the burdens of stroke and develop supportive programs to improve quality of life in stroke patients.
Methods
This retrospective cohort study was approved by the Human Research Ethics Committee, Faculty of Medicine Ramathibodi Hospital, Mahidol University and usage of anonymized data of the primary project was granted on 19 January 2024 (COA. MURA2024/48). In the primary study, written informed consent was obtained from all participants after receiving approval from the Human Research Ethics Committee, Faculty of Medicine Ramathibodi Hospital (COA. MURA2020/193). All methods were performed in accordance with the principles outlined in the Declaration of Helsinki.
The primary study recruited patients with their first stroke who were admitted to an acute stroke unit in a tertiary hospital in Bangkok between April 2020 and February 2021. All participants were followed up until six months after hospital discharge. The inclusion criteria were as follows: (1) being 20 years of age and above; (2) being diagnosed with a first stroke by a physician with brain imaging confirmation; (3) being capable of cognitive communication; and (4) being willing to participate in the study. Patients were excluded from the study if they had: (1) other illnesses (e.g., cancers, heart failure, end-stage renal diseases) that could affect the patients’ quality of life; and (2) language-related limitations that prevented responses to evaluation; and (3) being admitted to the hospital due to recurrent stroke.
Measures
Sociodemographic data of patients with first stroke were collected as follows: age (years), gender (male = 1, female = 0), marital status (married = 1, not married = 0), level of education (lower than bachelor’s degree = 0, bachelor’s degree or higher = 1), and family monthly income (sufficiency income = 1, insufficiency income = 0).
Clinical data included subtypes of stroke, comorbidity, and severity of stroke, were recorded from the patient’s medical records. Subtypes of stroke were classified as ischemic stroke and hemorrhagic stroke, which were confirmed with brain imaging. Participants were understood to have comorbidities if they responded that they had diabetes mellitus, hypertension, and dyslipidemia. The National Institutes of Health Stroke Scale (NIHSS) was collected on hospital discharge to identify stroke severity after acute stroke treatment. An NIHSS score of 0 point was considered a no-stroke symptom, 1 to 4 points a minor stroke, 5 to 15 points a moderate stroke, 16 to 20 points a severe stroke, and 21 to 42 points a very severe stroke24.
Health-related quality of life (HRQoL) was assessed using the European Quality of Life 5 dimensions (EQ-5D). It is a self-report instrument to assess health-related quality of life (HRQoL)25. The validated Thai-language version of the 5-level European Quality of Life 5 dimensions (EQ-5D-5L) questionnaire25–27 was used to assess the quality of life of participants. The EQ-5D-5L questionnaire has five dimensions to evaluate mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension is assigned to five levels: no problems, slight problems, moderate problems, severe problems, and extreme problems27. The responses of five dimensions were calculated to the index score using a scoring algorithm developed for Thailand28. The EQ-5D-5L index score indicates the utility value of a respondent’s health state where 1 refers to full health state, 0 refers to dead, and negative index scores suggest that one’s health state is worse than dead. Health state 11111 indicates no problems on any of the five dimensions. While levels 2 to 5 of any dimension refer to some problems. The EQ-5D-5L questionnaire had a good validity and reliability for measuring HRQoL among Thai population with chronic diseases29,30. The coefficient of Cronbach’s alpha for EQ-5D-5L from this study sample was 0.90.
Data collection and follow-up
Trained research nurses reviewed first-stroke patients for eligibility. Stroke patients who met the inclusion criteria were invited to participate in the study between April 2020 and February 2021. Full disclosure was provided to eligible participants, and informed consent was obtained before data collection. The initial data collection included sociodemographic, clinical, and health-related quality of life information. The research nurses conducted interviews and reviewed study participants’ medical records the day before their hospital discharge.
Follow-up: One, three, and six months after hospital discharge, all stroke participants received telephone interviews with their HRQoL using the EQ-5D-5L questionnaire. The last follow-up cases were in August 2021.
This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist for cohort study31.
Statistical analysis
The G*Power 3.1 software was used to determine sample size for repeated measures32, using a significance level of 5% and a statistical power of 80%, yielding a Cohen’s effect size of 0.2532,33. For four repeated times, the minimum sample size for two groups was 24 (12 samples per group) and for four groups was 36 (9 samples per group). The IBM SPSS Statistics version 29.0 (IBM Corp, Armonk, NY) was used for data analysis. Pairwise deletion was used to deal with the missing data. Categorical data were presented with frequency and percentage. Continuous variables were presented with mean, minimum, maximum, standard deviation (SD), and 95% confidence interval (CI). Linear mixed models were applied to investigate the effects of stroke characteristics and sociodemographic data (group), time, and interactions between each grouping variable and time (group*time) on EQ-5D-5L index scores. For variables with significant group*time interaction indicating different group effect over time, the simple main effect for each group was further evaluated between two time points using Bonferroni correction34. A p < 0.05 was considered statistically significant. Figures were generated to visualize patterns of change in HRQoL within 6 months after stroke.
Ethical approval and consent to participate
This study was reviewed and approved by the Human Research Ethics Committee, Faculty of Medicine Ramathibodi Hospital, Mahidol University (MURA2024/48). Informed consent was obtained from all individual participants included in the primary study (COA. MURA2020/193).
Results
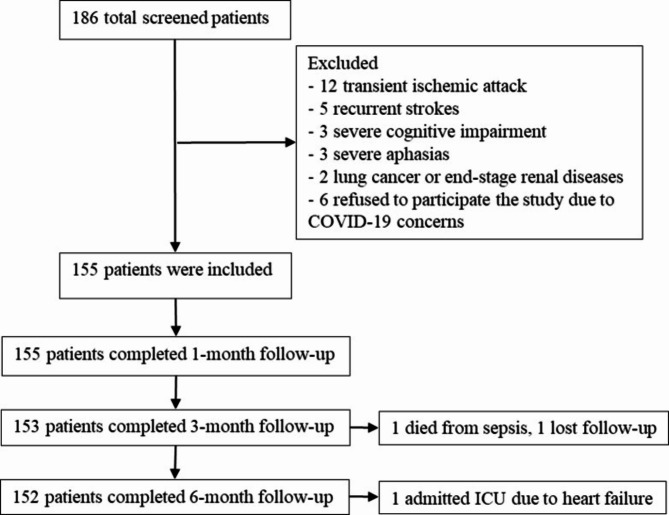
From April 2020 to February 2021, 155 of 186 hospitalized patients who met the inclusion criteria completed a telephone interview 1 month after discharge. Therefore, 155 patients were included in this study analysis. However, two participants lost follow-up at 3 months; a 72-year-old male died from sepsis, and a 64-year-old female lost follow-up and could not be contacted. Moreover, one 77-year-old male participant was not assessed quality of life at 6 months since he was admitted to ICU due to heart failure, resulting in 152 patients completed the last follow-up at 6 months after discharge (Fig. 1).
Fig. 1.
Study flow diagram.
Characteristics of patients with stroke
A total of 155 patients with a stroke were initially included in the study. Baseline sociodemographic and clinical characteristics in the initial cohort and 6-month follow-up are shown in Table 1. The mean age was 63.98 years. Most participants were male (62.6%). About two-thirds of them were married (67.1%). 36.8% of participants were educated with a bachelor’s degree or higher. Most participants (83.9%) had a sufficient family monthly income for their living standard. Most participants’ medical expenses were covered by the government through the civil service medical benefits scheme (52.3%), followed by the universal coverage scheme (36.8%). Among the 155 stroke participants, ischemic stroke was the most prevalent (89.7%). Most of the participants were discharged with minor stroke (50.9%), followed by moderate stroke (23.9%), and no stroke symptoms (18.1%), while 7.1% had severe and very severe stroke symptoms after treatment. The most common comorbidity was hypertension (64.5%). The lost 3 cases at the 6-month follow-up did not possess significant characteristics (Table 1).
Table 1.
Baseline characteristics of patients with stroke.
| Variables | Initial cohort (n = 155) | 6-month follow-up (n = 152) |
|---|---|---|
| Number (%) | Number (%) | |
| Age in years, mean (SD); minimum - maximum | 63.98 (12.53); 29–91 | 63.84 (12.59); 29–91 |
| Gender | ||
| Male | 97 (62.6) | 95 (62.5) |
| Female | 58 (37.4) | 57 (37.5) |
| Marital status | ||
| Married | 104 (67.1) | 102 (67.1) |
| Not married | 51 (32.9) | 50 (32.9) |
| Level of education | ||
| Lower than bachelor’s degree | 98 (63.2) | 97 (63.8) |
| Bachelor’s degree or higher | 57 (36.8) | 55 (36.2) |
| Family monthly income | ||
| Sufficient income | 130 (83.9) | 128 (84.2) |
| Insufficient income | 25 (16.1) | 24 (15.8) |
| Medical payment source | ||
| Universal coverage scheme | 57 (36.8) | 54 (35.5) |
| Civil service medical benefits scheme | 81 (52.3) | 81 (53.3) |
| Social security scheme | 10 (6.5) | 10 (6.6) |
| Health insurance | 2 (1.3) | 2 (1.3) |
| Self-payment | 5 (3.2) | 5 (3.3) |
| Stroke subtypes | ||
| Ischemic | 139 (89.7) | 136 (89.5) |
| Hemorrhagic | 16 (10.3) | 16 (10.5) |
| Comorbidities* | ||
| Diabetes mellitus | 60 (38.7) | 58 (38.2) |
| Hypertension | 100 (64.5) | 99 (65.1) |
| Dyslipidemia | 84 (54.2) | 82 (53.9) |
| NIHSS at discharge, mean (SD); minimum - maximum | 4.18 (4.71); 0–23 | 4.12 (4.64); 0–23 |
| No stroke symptom (NIHSS = 0) | 28 (18.1) | 28 (18.4) |
| Minor stroke (NIHSS = 1–4) | 79 (50.9) | 77 (50.7) |
| Moderate stroke (NIHSS = 5–15) | 37 (23.9) | 37 (24.3) |
| Severe stroke (NIHSS = 16–20) | 9 (5.8) | 8 (5.3) |
| Very severe stroke (NIHSS = 21–42) | 2 (1.3) | 2 (1.3) |
*multiple responses; SD = standard deviation; NIHSS = National Institutes of Health Stroke Scale
Changes in HRQoL within 6 months after discharge from a stroke
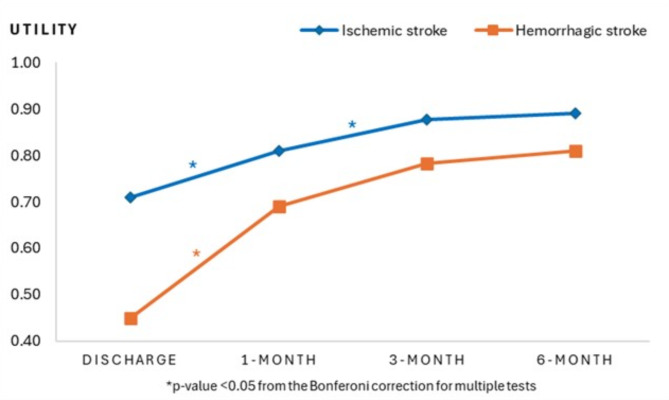
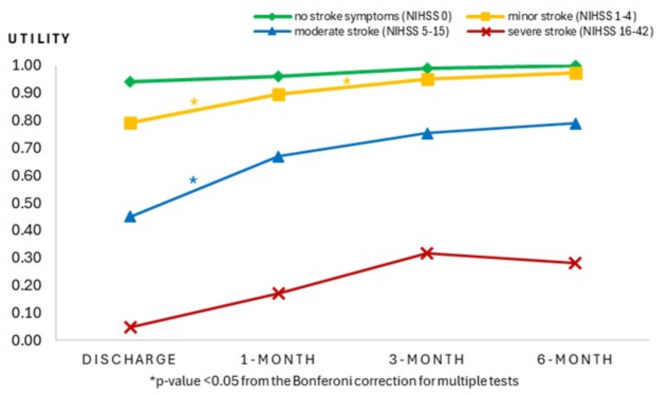
Overall, the EQ-5D-5L index score at discharge ranged from − 0.42 to 1.00, with a mean index score of 0.69 (SD 0.33). The trend toward improvement of EQ-5D-5L index scores in six months of stroke was identified for both stroke subtypes (Fig. 2). The EQ-5D-5L index scores among patients with ischemic stroke significantly increased from discharge to 1 month (p < 0.05) and from 1 month to 3 months (p < 0.05). For hemorrhagic stroke, a significant improvement was identified from discharge to 1 month (p < 0.05). However, both stroke subtypes had no significant improvement from 3 months to 6 months. Considering HRQoL changes by severity of stroke (Fig. 3), patterns of EQ-5D-5L index mean scores were increased from discharge to 6 months among patients with no stroke symptoms, minor stroke, and moderate stroke (p < 0.05), while the HRQoL trend among severe stroke patients seemed to increase after discharge and then decreased after three months.
Fig. 2.
Health-related quality of life by stroke subtypes. Figure 2 shows mean EQ-5D-5L index scores of patients with stroke at discharge, 1-month, 3-month, and 6-month after discharge.
Fig. 3.
Health-related quality of life by stroke severity. Figure 1 shows mean EQ-5D-5L index scores of patients with stroke at discharge, 1-month, 3-month, and 6-month after discharge.
Effects of stroke and sociodemographic characteristics on HRQoL over 6 months
Table 2 shows results for analyses of the effects of individual factors, time, and their interaction on health-related quality of life. Mixed model analysis indicated significant main effects of time on HRQoL index scores among stroke patients for all factors, including stroke subtypes, stroke severity, age group, gender, marital status, education level, and monthly income (p < 0.001). Average HRQoL index scores showed an increasing trend from 0.69 at discharge to 0.80 (1 month), 0.87 (3 months), and 0.89 (6 months).
Table 2.
Effects of stroke and sociodemographic characteristics on HRQoL over 6 months.
| Factors | Mean EQ-5D-5L index scores (SD) | P-value | |||||
|---|---|---|---|---|---|---|---|
| Discharge (n = 155) | 1-month (n = 155) | 3-month (n = 153) | 6-month (n = 152) |
Group | Time | Group*Time | |
| All | 0.69 (0.33) | 0.80 (0.28) | 0.87 (0.26) | 0.89 (0.26) | < 0.001 | ||
| Stroke subtypes | |||||||
| IS | 0.71 (0.30) | 0.81 (0.27) | 0.88 (0.25) | 0.89 (0.26) | 0.074 | < 0.001 | 0.003 |
| ICH | 0.45 (0.46) | 0.69 (0.35) | 0.78 (0.29) | 0.81 (0.27) | |||
| Stroke severity | |||||||
| No symptoms | 0.94 (0.09) | 0.96 (0.07) | 0.99 (0.03) | 1.00 (0.01) | < 0.001 | < 0.001 | < 0.001 |
| Minor | 0.79 (0.21) | 0.90 (0.11) | 0.95 (0.08) | 0.97 (0.08) | |||
| Moderate | 0.45 (0.30) | 0.67 (0.31) | 0.75 (0.33) | 0.79 (0.30) | |||
| Severe | 0.05 (0.25) | 0.17 (0.37) | 0.32 (0.38) | 0.28 (0.46) | |||
| Age group | |||||||
| ≤ 60 years | 0.70 (0.36) | 0.81 (0.30) | 0.87 (0.26) | 0.88 (0.27) | 0.753 | < 0.001 | 0.862 |
| > 60 years | 0.68 (0.31) | 0.80 (0.27) | 0.86 (0.26) | 0.89 (0.25) | |||
| Gender | |||||||
| Male | 0.71 (0.33) | 0.83 (0.27) | 0.89 (0.23) | 0.91 (0.23) | 0.141 | < 0.001 | 0.842 |
| Female | 0.64 (0.32) | 0.76 (0.30) | 0.82 (0.30) | 0.85 (0.30) | |||
| Marital status | |||||||
| Married | 0.72 (0.31) | 0.80 (0.30) | 0.86 (0.27) | 0.88 (0.27) | 0.713 | < 0.001 | 0.001 |
| Non-married | 0.62 (0.35) | 0.80 (0.25) | 0.87 (0.23) | 0.89 (0.25) | |||
| Education attainment | |||||||
| < Bachelor’s degree | 0.69 (0.33) | 0.77 (0.32) | 0.85 (0.29) | 0.86 (0.30) | 0.104 | < 0.001 | 0.303 |
| ≥Bachelor’s degree | 0.70 (0.33) | 0.85 (0.20) | 0.90 (0.20) | 0.93 (0.16) | |||
| Monthly income | |||||||
| Insufficient income | 0.60 (0.43) | 0.70 (0.40) | 0.76 (0.34) | 0.74 (0.38) | 0.024 | < 0.001 | 0.719 |
| Sufficient income | 0.70 (0.31) | 0.82 (0.25) | 0.89 (0.24) | 0.91 (0.22) | |||
The main effect of stroke subtypes was not statistically significant (p = 0.074), but there was significant time by subtype interaction (p = 0.003). Thus, mean HRQoL index scores over six months differed for different stroke subtypes. There were significant main effects of stroke severity and time*stroke severity interaction (p < 0.001), meaning that changes in EQ-5D-5L index score over time differed by level of stroke severity. There was no significant effect of age group, gender, and education level on the linear trend of EQ-5D-5L index score over six months. There was an interaction effect between time and marital status (p = 0.001). Thus, trends of mean EQ-5D-5L index score over six months differed by marital status. The main effect of monthly income was statistically significant (p = 0.024). Participants with sufficient income had a higher mean score of EQ-5D-5L than those with insufficient income (p < 0.05). Moreover, the trend of mean EQ-5D-5L index score among participants with sufficient income increased over six months, while it decreased after three months among those with insufficient income (Table 2).
Table 3 shows the results of simple main effect analyses for variables having significant effects of group*time interaction on the HRQoL index score. Significant changes were identified between discharge and 1-month, 3-month, and 6-month (p < 0.05), but there was no significant change from 3 months to 6-months for all strokes. Stratified analysis for each stroke subtype found that mean EQ-5D-5L index scores between discharge and 1-month, discharge and 3-month, and discharge and 6-month were significantly different at 0.10, 0.17, and 0.18 scores for ischemic stroke patients, and 0.24, 0.33, and 0.36 scores for hemorrhagic stroke patients (p < 0.05). There were significant increases in EQ-5D-5L scores over six months for patients with no stroke symptoms, minor stroke, and moderate stroke (p < 0.001) but not severe stroke (p = 0.156). Mean EQ-5D-5L index scores among minor stroke and moderate stroke patients significantly increased from discharge to 1-month (0.11 and 0.22 points, respectively). At six months, means of EQ-5D-5L index scores among patients with no stroke symptoms, minor stroke, and moderate stroke significantly increased 0.06, 0.18, and 0.34 scores from discharge. Considering married and non-married patients, changes in EQ-5D-5L mean scores from discharge were 0.08 vs. 0.18 (1-month), 0.14 vs. 0.25 (3-month), and 0.16 vs. 0.27 (6-month).
Table 3.
Mean EQ-5D-5L index changes at each time point by stroke subtypes, severity, and marital status.
| Variables | P-value | Mean change (95% CI) | |||
|---|---|---|---|---|---|
| Discharge to 1-month | Discharge to 3-month | Discharge to 6-month | 3-month to 6-month | ||
| All | < 0.001 | 0.12 (0.07, 0.16)** | 0.18 (0.13, 0.22)** | 0.20 (0.15, 0.24)** | 0.02 (-0.03, 0.07) |
| Stroke subtypes | |||||
| IS | < 0.001 | 0.10 (0.05, 0.15)** | 0.17 (0.11, 0.20)** | 0.18 (0.13, 0.22)** | 0.01 (-0.03, 0.06) |
| ICH | < 0.001 | 0.24 (0.05, 0.44)* | 0.33 (0.14, 0.53)** | 0.36 (0.17, 0.56)** | 0.03 (-0.16, 0.23) |
| Stroke severity | |||||
| No symptoms | < 0.001 | 0.02 (-0.02, 0.05) | 0.05 (0.01, 0.08)* | 0.06 (0.02, 0.09)** | 0.01 (-0.03, 0.05) |
| Minor | < 0.001 | 0.11 (0.06, 0.15)** | 0.16 (0.11, 0.20)** | 0.18 (0.13, 0.22)** | 0.02 (-0.02, 0.07) |
| Moderate | < 0.001 | 0.22 (0.09, 0.35)** | 0.30 (0.17, 0.43)** | 0.34 (0.21, 0.47)** | 0.04 (-0.09, 0.17) |
| Severe | 0.156 | 0.12 (-0.20, 0.44) | 0.27 (-0.08, 0.58) | 0.23 (-0.11, 0.55) | -0.04 (-0.37, 0.30) |
| Marital status | |||||
| Married | < 0.001 | 0.08 (0.03, 0.13)** | 0.14 (0.09, 0.19)** | 0.16 (0.11, 0.21)** | 0.02 (-0.03, 0.07) |
| Non-married | < 0.001 | 0.18 (0.09, 0.28)** | 0.25 (0.17, 0.36)** | 0.27 (0.18, 0.37)** | 0.02 (-0.08, 0.11) |
P-value corresponds to simple main effect test for each group
*p < 0.05, **p < 0.001 corresponds to simple main effect for each group at each time point using Bonferroni post-hoc adjustments
Discussion
The self-reported health state reflected the perception of stroke patients on their HRQoL25. This study showed dynamic changes in HRQoL among patients with stroke within six months. It is important information to indicate patterns of HRQoL changes over time in stroke patients. HRQoL was likely to improve from discharge to one month and three months after discharge. These findings were consistent with previous studies35,36. The results from this study showed that patterns of HRQoL over time differed by stroke subtypes. The HRQoL scores among patients with ischemic stroke were significantly improved from discharge to 1 month and from 1 month to 3 months. In comparison, hemorrhagic stroke patients found significant increases in HRQoL from discharge to 1 month, but there was no significant change after 1 month, although the slope seemed to be similar to ischemic stroke. Small sample sizes in hemorrhagic stroke might affect the power of the statistical test. Besides, the HRQoL scores among patients with ischemic stroke were higher than those of hemorrhagic stroke from the start through the end of follow-up. These results indicated that hemorrhagic stroke had lower HRQoL16,19 due to worse outcomes than ischemic stroke9.
This study revealed that patterns of changes in HRQoL among patients with a stroke over six months varied by severity of stroke. The comparisons of HRQoL over 6 months were significantly different for stroke patients with no stroke symptoms, minor stroke, and moderate stroke. However, we found no significant HRQoL changes among severe stroke patients. These results explained that patients with less severe stroke were more likely to have significantly improved HRQoL19,37. These results indicated that the burden of stroke among patients with severe stroke is intense, and the chance of improving is low. Severe stroke patients could expect permanent disability and low HRQoL19,37.
Moreover, HRQoL seemed stable after three months for all stroke subtypes and severity levels. The improvement of HRQoL found in this study might be explained by the recovery in motor function after strokes, which suggested the maximum possible recovery was within three months18,37–40. It might be recommended that rehabilitation and supportive programs should be implemented within three months after stroke40,41. The study in China also found that the quality of life among stroke patients significantly increased at one month for physical functioning and general health16. However, the rehabilitation and supportive programs should be continued for 6 or 12 months since several studies identified physical functioning and HRQoL improvement at 6 months17,36 and 12 months38,42. Although this study did not find significant differences in HRQoL among severe stroke patients, the increasing trends of HRQoL were presented till three months and decreased afterward. These findings indicated poor outcomes in patients with severe stroke symptoms. Rehabilitation and appropriate care programs should also be provided to improve their HRQoL and prevent complications35,43,44.
Furthermore, this study found that family monthly income had a significant effect on HRQoL among patients with stroke over six months. Stroke patients with sufficient family monthly income tended to have better HRQoL than those with insufficient income for their standard of living. This finding was consistent with the results from previous studies11,19,45. Most of this study population’s medical expenses for acute stroke treatment and post-discharge rehabilitation were covered by the government and their health insurance (96.8%). However, stroke patients and their families might face an economic burden from informal care costs and productivity losses due to stroke46. Financial support from the community or related organizations for medical or general expenses may help reduce stroke burdens and increase HRQoL in stroke patients.
To the best of our knowledge, this is the first study in Thailand conducted to examine patterns of changes in health-related quality of life among post-stroke patients over six months based on stroke subtypes, stroke severity, and sociodemographic factors. Moreover, this study had a remarkedly low attrition rate (1.9%). HRQoL information from this study could be used to explain the burdens of stroke for different subtypes and severity levels. The timing of starting supportive programs is essential for patients to achieve the maximum possible recovery and quality of life. Stroke patients with severe stroke symptoms and insufficient monthly income had poor quality of life over time. Long-term supportive care plans are required to improve their quality of life. Multidisciplinary teams could use these findings to prepare patients and their families in the long run.
This study has some limitations. Although the self-report EQ-5D-5L questionnaire is easy to use and reflects an individual’s perception of their health state, respondents need to be able to communicate effectively. This study excluded stroke patients who were unable to assess themselves due to major neurological problems such as aphasia, cognitive impairment, or critical conditions. The burdens of stroke from this study might be underestimated, and the HRQoL might be overestimated. These may compromise the representativeness of all strokes. Second, EQ-5D-5L is a generic measure of HRQoL consisting of only five dimensions. The information obtained might be limited. Third, a small sample size from one tertiary hospital, especially hemorrhagic patients, may limit the data analysis and generalizability of the results. Future studies are needed using more stroke-specific instruments, recruiting large sample sizes, and collecting data from several settings. Finally, economic evaluations should be performed after stroke discharge since some stroke survivors may be unable to fully return to work or may have extra care costs due to a stroke.
Conclusions
This study found that not all stroke patients regained full health state after six months. The means of HRQoL index scores from discharge to 6 months were between 0.69 and 0.89. The patterns of mean HRQoL scores significantly increased from discharge to three months. There were positive slopes in HRQoL from 3 to 6 months, but no significant changes were identified. HRQoL means differed by stroke subtypes and severity. Ischemic stroke showed better results in HRQoL than hemorrhagic stroke. Patients with minor and moderate stroke had significant changes in HRQoL over six months. HRQoL scores among patients with severe stroke also improved from discharge to 6 months, but not statistically significant. Moreover, monthly income sufficiency significantly affected HRQoL improvements over six months. Rehabilitation or supportive programs in Thailand should be started within the first three months after stroke to achieve the maximum possible outcomes. Moreover, supportive care plans should be prepared for patients with severe stroke symptoms and insufficient monthly income.
Acknowledgements
The authors extend their gratitude to all patients who participated in this study.
Author contributions
N.B., J.G.V., J.K., and N.T. contributed to the study concept and design. N.B., J.K., and N.T. acquired the participants and data. N.B. and J.G.V. performed data analysis and interpretation. N.B. wrote the first draft of the manuscript, and all authors reviewed and edited the manuscript. All the authors read and approved the final manuscript.
Funding
This study was supported by Ramathibodi School of Nursing, Faculty of Medicine Ramathibodi Hospital, Mahidol University.
Data availability
The datasets used and analyzed in the current study are available from the corresponding author on reasonable request.
Declarations
Consent for publication
Not required.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the global burden of disease study 2019. Lancet Neurol.20(10), 795–820. 10.1016/S1474-4422(21)00252-0 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Samuthpongtorn, C., Jereerat, T. & Suwanwela, N. C. Stroke risk factors, subtypes and outcome in elderly Thai patients. BMC Neurol.21(1), 322. 10.1186/s12883-021-02353-y (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Long, X. et al. Mortality, recurrence, and dependency rates are higher after acute ischemic stroke in elderly patients with diabetes compared to younger patients. Front. Aging Neurosci.8, 142. 10.3389/fnagi.2016.00142 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bártlová, S. et al. Quality of life of post-stroke patients. Zdr. Varst.61(2), 101–108. 10.2478/sjph-2022-0014 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Statista Research Department. Share of total population older than 60 years old in Thailand in 2022 with a forecast to 2040 [Graph]. (2023). https://www.statista.com/statistics/713667/thailand-forecast-aging-population/
- 6.Chantkran, W., Chaisakul, J., Rangsin, R., Mungthin, M. & Sakboonyarat, B. Prevalence of and factors associated with stroke in hypertensive patients in Thailand from 2014 to 2018: A nationwide cross-sectional study. Sci. Rep.11(1), 17614. 10.1038/s41598-021-96878-4 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rao, C. et al. Verifying causes of death in Thailand: Rationale and methods for empirical investigation. Popul. Health Metr.8, 11. 10.1186/1478-7954-8-11 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bundhamcharoen, K., Odton, P., Phulkerd, S. & Tangcharoensathien, V. Burden of disease in Thailand: Changes in health gap between 1999 and 2004. BMC Public. Health11, 53. 10.1186/1471-2458-11-53 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Butsing, N., Tipayamongkholgul, M., Wang, J. D. & Ratanakorn, D. Combined quality of life and survival for estimation of long-term health outcome of patients with stroke. Health Qual. Life Outcomes20(1), 46. 10.1186/s12955-022-01959-1 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Powers, W. J. et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke50(12), e344–e418. 10.1161/STR.0000000000000211 (2019). [DOI] [PubMed] [Google Scholar]
- 11.Butsing, N., Tipayamongkholgul, M., Ratanakorn, D., Suwannapong, N. & Bundhamcharoen, K. Social support, functional outcome and quality of life among stroke survivors in an urban area. J. Pac. Rim Psychol.13, e4. 10.1017/prp.2019.2 (2019). [Google Scholar]
- 12.Sennfält, S., Norrving, B., Petersson, J. & Ullberg, T. Long-term survival and function after stroke: A longitudinal observational study from the Swedish Stroke Register. Stroke50(1), 53–61. 10.1161/STROKEAHA.118.022913 (2019). [DOI] [PubMed] [Google Scholar]
- 13.Pantoni, L. & Salvadori, E. Location of infarcts and post-stroke cognitive impairment. Lancet Neurol.20(6), 413–414. 10.1016/S1474-4422(21)00107-1 (2021). [DOI] [PubMed] [Google Scholar]
- 14.Lim, J. S., Lee, J. J. & Woo, C. W. Post-stroke cognitive impairment: Pathophysiological insights into brain disconnectome from advanced neuroimaging analysis techniques. J. Stroke23(3), 297–311. 10.5853/jos.2021.02376 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kainz, A. et al. Changes of health-related quality of life within the 1st year after stroke-results from a prospective stroke cohort study. Front. Neurol.12, 715313. 10.3389/fneur.2021.715313 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen, Q., Cao, C., Gong, L. & Zhang, Y. Health related quality of life in stroke patients and risk factors associated with patients for return to work. Medicine98(16), e15130. 10.1097/MD.0000000000015130 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duncan, P. W., Lai, S. M. & Keighley, J. Defining post-stroke recovery: Implications for design and interpretation of drug trials. Neuropharmacol39(5), 835–841. 10.1016/s0028-3908(00)00003-4 (2000). [DOI] [PubMed] [Google Scholar]
- 18.Lee, K. B. et al. Six-month functional recovery of stroke patients: A multi-time-point study. Int. J. Rehabil Res.38(2), 173–180. 10.1097/MRR.0000000000000108 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kariyawasam, P. N., Pathirana, K. D. & Hewage, D. C. Factors associated with health related quality of life of patients with stroke in Sri Lankan context. Health Qual. Life Outcomes18(1), 129. 10.1186/s12955-020-01388-y (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yin, S., Njai, R., Barker, L., Siegel, P. Z. & Liao, Y. Summarizing health-related quality of life (HRQOL): Development and testing of a one-factor model. Popul. Health Metr.14, 22. 10.1186/s12963-016-0091-3 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wong, H. J., Lua, P. L., Harith, S. & Ibrahim, K. A. Health-related quality of life profiles and their dimension-specific associated factors among Malaysian stroke survivors: A cross sectional study. Health Qual. Life Outcomes19(1), 210. 10.1186/s12955-021-01847-0 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xie, J. et al. Impact of stroke on health-related quality of life in the noninstitutionalized population in the United States. Stroke37(10), 2567–2572. 10.1161/01.STR.0000240506.34616.10 (2006). [DOI] [PubMed] [Google Scholar]
- 23.Kwon, S. et al. Health-related quality of life and related factors in stroke survivors: Data from Korea National Health and Nutrition Examination Survey (KNHANES) 2008 to 2014. PLoS One13(4), e0195713. 10.1371/journal.pone.0195713 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hage, V. The NIH stroke scale: A window into neurological status. Nurs. Spectr.24(15), 44–49 (2011). [Google Scholar]
- 25.EuroQol Group. EuroQol–a new facility for the measurement of health-related quality of life. Health Policy16(3), 199–208. 10.1016/0168-8510(90)90421-9 (1990). [DOI] [PubMed] [Google Scholar]
- 26.Rabin, R. & de Charro, F. EQ-5D: A measure of health status from the EuroQol Group. Ann. Med.33(5), 337–343. 10.3109/07853890109002087 (2001). [DOI] [PubMed] [Google Scholar]
- 27.EuroQol Research Foundation. EQ-5D-5L user guide. Rotterdam: EuroQol Group (2019). https://euroqol.org/publications/user-guides (2019).
- 28.Pattanaphesaj, J. et al. The EQ-5D-5L valuation study in Thailand. Expert Rev. Pharmacoecon Outcomes Res.18(5), 551–558. 10.1080/14737167.2018.1494574 (2018). [DOI] [PubMed] [Google Scholar]
- 29.Pattanaphesaj, J. & Thavorncharoensap, M. Measurement properties of the EQ-5D-5L compared to EQ-5D-3L in the Thai diabetes patients. Health Qual. Life Outcomes13, 14. 10.1186/s12955-014-0203-3 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sakthong, P., Sonsa-Ardjit, N., Sukarnjanaset, P. & Munpan, W. Psychometric properties of the EQ-5D-5L in Thai patients with chronic diseases. Qual. Life Res.24(12), 3015–3022. 10.1007/s11136-015-1038-z (2015). [DOI] [PubMed] [Google Scholar]
- 31.Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth.13(Suppl 1), S31–S34. 10.4103/sja.SJA_543_18 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Faul, F., Erdfelder, E., Lang, A. G. & Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods39(2), 175–191 (2007). [DOI] [PubMed] [Google Scholar]
- 33.Bakeman, R. Recommended effect size statistics for repeated measures designs. Behav. Res. Methods37(3), 379–384. 10.3758/BF03192707 (2005). [DOI] [PubMed] [Google Scholar]
- 34.Tabachnick, B. G. & Fidell, L. S. Using Multivariate Statistics 5th edn (Allyn & Bacon/Pearson Education, 2007).
- 35.Yeoh, Y. S. et al. Health-related quality of life loss associated with first-time stroke. PLoS One14(1), e0211493. 10.1371/journal.pone.0211493 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wongsa, D., Soivong, P., Chaiard, J. & Davidson, P. M. Patterns of health-related quality of life among stroke survivors: A longitudinal study. West. J. Nurs. Res.45(6), 511–519. 10.1177/01939459231151385 (2023). [DOI] [PubMed] [Google Scholar]
- 37.Guggisberg, A. G., Nicolo, P., Cohen, L. G., Schnider, A. & Buch, E. R. Longitudinal structural and functional differences between proportional and poor motor recovery after stroke. Neurorehabil Neural Repair.31(12), 1029–1041. 10.1177/1545968317740634 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Balkaya, M. & Cho, S. Optimizing functional outcome endpoints for stroke recovery studies. J. Cereb. Blood Flow. Metab.39(12), 2323–2342. 10.1177/0271678X19875212 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wee, S. K., Hughes, A. M., Warner, M. & Burridge, J. H. Trunk restraint to promote upper extremity recovery in stroke patients: A systematic review and meta-analysis. Neurorehabil. Neural Repair.28(7), 660–677. 10.1177/1545968314521011 (2014). [DOI] [PubMed] [Google Scholar]
- 40.Xu, J. et al. Separable systems for recovery of finger strength and control after stroke. J. Neurophysiol.118(2), 1151–1163. 10.1152/jn.00123.2017 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zeiler, S. R. Should we care about early post-stroke rehabilitation? Not yet, but soon. Curr. Neurol. Neurosci. Rep.19(3), 13. 10.1007/s11910-019-0927-x (2019). [DOI] [PubMed] [Google Scholar]
- 42.Algurén, B., Fridlund, B., Cieza, A., Sunnerhagen, K. S. & Christensson, L. Factors associated with health-related quality of life after stroke: A 1-year prospective cohort study. Neurorehabil Neural Repair.26(3), 266–274. 10.1177/1545968311414204 (2012). [DOI] [PubMed] [Google Scholar]
- 43.Bindawas, S. M. & Vennu, V. S. Stroke rehabilitation. A call to action in Saudi Arabia. Neurosciences (Riyadh)21(4), 297–305. 10.17712/nsj.2016.4.20160075 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shahid, J., Kashif, A. & Shahid, M. K. A comprehensive review of physical therapy interventions for stroke rehabilitation: Impairment-based approaches and functional goals. Brain Sci.13(5), 717. 10.3390/brainsci13050717 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mei, Y. X. et al. Health-related quality of life and its related factors in survivors of stroke in rural China: A large-scale cross-sectional study. Front. Public. Health10, 810185. 10.3389/fpubh.2022.810185 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Barral, M. et al. Patients’ productivity losses and informal care costs related to ischemic stroke: A French population-based study. Eur. J. Neurol.28(2), 548–557. 10.1111/ene.14585 (2021). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed in the current study are available from the corresponding author on reasonable request.