Abstract
Localized bladder amyloidosis is a rare disorder mimicking bladder tumor, with merely over 200 reported cases. Here, we report a case of a 67-year-old female presented with painless gross hematuria. A positive Congo red staining of the cystoscopy biopsy raised suspicion of bladder amyloidosis, and transurethral resection of the mass was performed. Interestingly, the histopathology of the excised mass showed pink-staining material under Hematoxylin and Eosin staining, but negative Congo red staining. This case demonstrates that a negative Congo red staining doesn't exclude amyloidosis. An accurate diagnosis should rely on a comprehensive evaluation of clinical, laboratory, radiological, and histopathological findings.
Keywords: Congo red staining, Localized bladder amyloidosis, Pink-staining material
1. Introduction
Localized amyloidosis can manifest in any organ, often without accompanying systematic diseases.1 The bladder, an uncommon site for this condition, requires clinical attention as it can present symptoms indistinguishable from those of urinary malignancies. Histopathological examination plays a pivotal role in differential diagnosis, with Congo red staining serving as a key diagnostic indicator for amyloid deposits.2 However, negative Congo red staining doesn't necessarily rule out amyloidosis. Here, we report a case of localized bladder amyloidosis with a literature review. Notably, this patient was still diagnosed with localized bladder amyloidosis despite the postoperative histopathology showing a negative Congo red staining, highlight that Congo red staining isn't the exclusive diagnostic standard for amyloidosis.
2. Case presentation
A 67-year-old non-smoker female with a 6-month history of painless gross hematuria was admitted to our hospital. The hematuria was intermittent and red in color with no clotting. Accompanying symptoms included occasional irritative voiding symptoms and lower abdominal pain. She denied fever and joint pain. Physical examination revealed no abnormalities. Computed tomography (CT) showed normal bladder wall thickness with no evidence of masses or lesions (Fig. 1). Upon cystoscopy, a 2 × 2 cm dark-red lesion was identified on the posterior bladder wall. Histopathology examination demonstrated uniformly pink-staining material in the specimen. Further analysis with Congo red staining under polarized light microscopy revealed a characteristic “apple-green” birefringence, which is indicative of amyloidosis. Evaluation concerning systematic amyloidosis all returned negative. The patient denied any history of chronic inflammatory conditions (including rheumatoid arthritis, systemic lupus erythematosus, tuberculosis, etc.) that could lead to secondary amyloidosis. Transurethral resection of the bladder tumor (TURBT) was then performed (Fig. 2), and histologic sections displayed chronic inflammation in the urothelial mucosa and edema in the submucosal layer with pink-staining material deposition and thickening of the vascular walls via Hematoxylin and Eosin (H&E) staining (Fig. 3). However, Congo red staining of the specimen yielded a negative result. Still, considering the patient's clinical symptoms, the histopathological findings from the preoperative cystoscopy biopsy, and the identification of pink-staining material in the tissue excised through TURBT, a diagnosis of localized bladder amyloidosis was made. The patient's symptoms quickly relieved after the surgery. A subsequent cystoscopy conducted approximately 3 months following TURBT showed smooth bladder mucosa with no evidence of recurrence (Fig. 4).
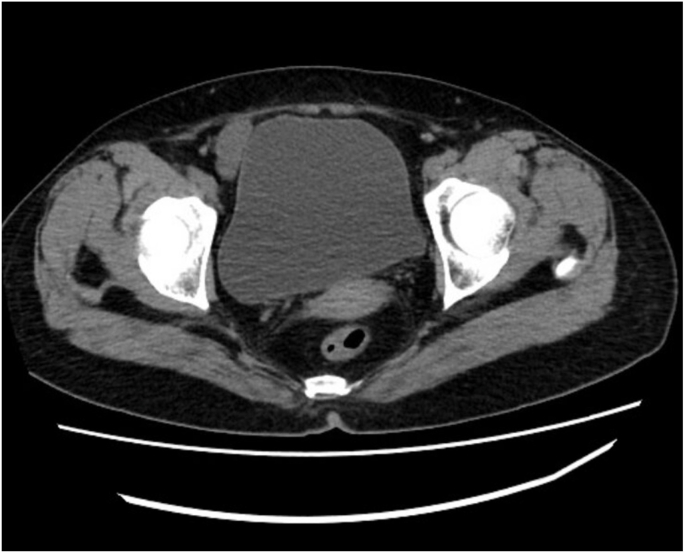
Fig. 1.
CT scan revealed a normal bladder wall without identifiable pathological changes.
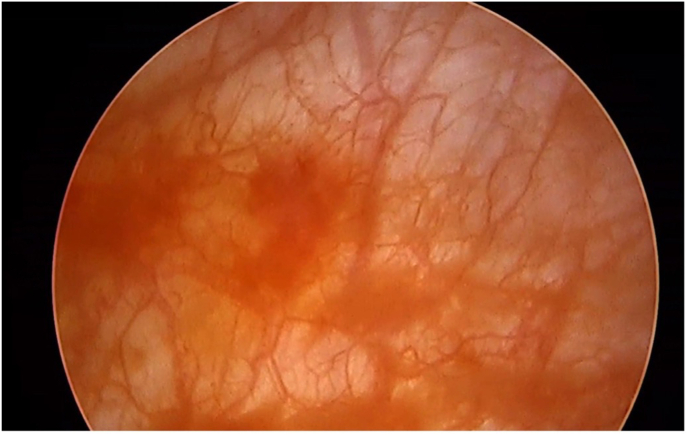
Fig. 2.
Cystoscopy image of the dark-red lesion during TURBT.
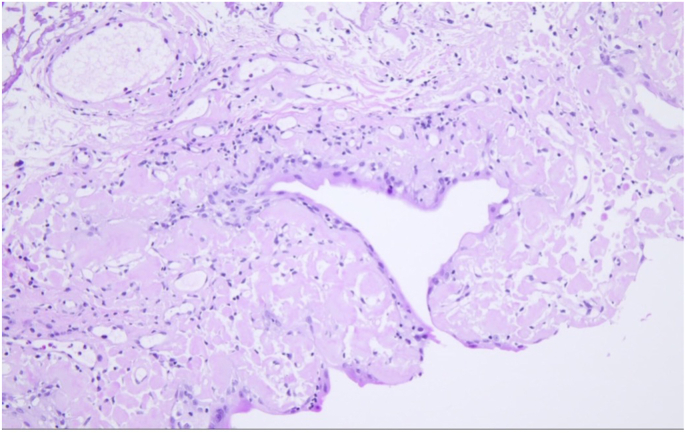
Fig. 3.
Histopathological finding of the excised specimen showed pink-staining material accumulation through H&E staining (200 × ).
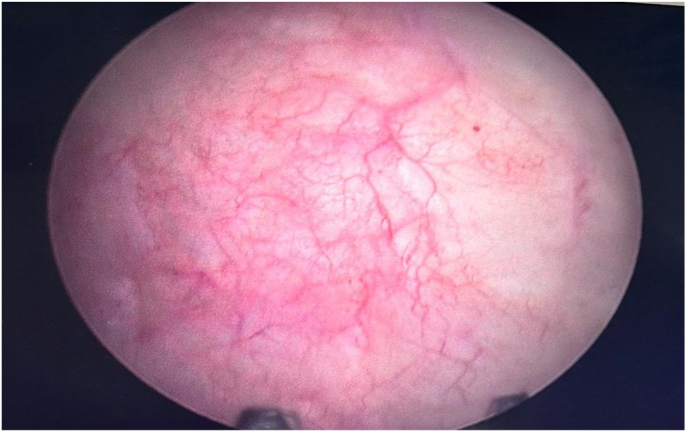
Fig. 4.
Cystoscopy image of the 3-month follow-up examination.
3. Discussion
Amyloidosis is a group of symptoms characterized by gradual tissue deterioration owing to abnormal extracellular protein deposition.3 Localized amyloidosis limits to a single tissue or organ, while systematic amyloidosis affects multiple organs.4 Patients with localized amyloidosis typically don't progress into systematic disease and thus don't require chemotherapy. Bladder amyloidosis is a rare clinical manifestation with merely more than 200 cases worldwide.5 The disease is nearly uniformly distributed across the fifth, sixth and seventh decades for male patients, while for most female patients, diagnosis typically occur during the sixth decade. The posterior and posterolateral walls are most primarily targeted, followed by the trigone.6 Distinguishing this disease from urinary malignancies is challenging, as they share similar clinical, imaging and cystoscopy findings.7 Patients usually present with intermittent, painless macroscopic hematuria and urinary irritation. CT often reveals signs of bladder wall thickening, mass lesions and filling defects. Cystoscopy frequently suggests nodular or polypoidal lesions within the bladder, bearing a resemblance to bladder carcinomas.
Histopathology examination, which is usually positively Congo red stained that exhibits a distinctive apple-green birefringence under polarized light microscope, is the golden standard for the diagnosis of the disease.8 Yet, it should be noted that negative Congo-red staining doesn't necessarily rule out amyloidosis, as is in our case. Several factors may account for this situation. For starters, the pathological transformation of the native protein structure into a predominantly antiparallel β-sheet conformation is similar to that of physiologic protein folding. Secondly, different ways of amyloid fibrils generation may have various reaction to Congo red staining. Thirdly, the false-negative Congo red staining may be attributed to technical issues such as fixation. Lastly, some atypical amyloidosis cases have been reported to be lack of Congo red staining.9 Nevertheless, electron microscopy can discern amyloid fibrils even in the absence of positive Congo red staining, thus serving as an adjunctive diagnostic approach for suspected cases of amyloidosis that do not yield to traditional Congo red staining.10 Other staining techniques such as Alcian blue, Thioflavin T and Azan Mallory trichrome stain are also valuable for identifying amyloid deposits. However, we were unable to utilize these methods owing to our limited facilities.
TURBT is the principal treatment for localized bladder amyloidosis with a recurrence rate of approximately 50 %.6 Alternative therapeutic approaches include oral colchicine, intravesical installation of dimethyl sulfoxide and laser therapy.1,11,12 Systematic treatment is not advised in localized bladder amyloidosis patients. Given the high relapse risk, long-term follow-up by cystoscopy examination is recommended.
4. Conclusion
This article reported a rare case of localized bladder amyloidosis with the removed sample through TURBT exhibiting negative response to Congo red staining, demonstrating that a definite diagnosis of amyloidosis should be confirmed by multiple diagnostic approaches.
CRediT authorship contribution statement
Yuchong Qiu: Writing – review & editing, Writing – original draft, Conceptualization. Sicheng Wu: Resources. Jianyang Lv: Resources. Zhigang Ji: Writing – review & editing, Supervision, Project administration. Jie Dong: Writing – review & editing, Project administration, Conceptualization.
Ethnics approval and consent to participate
Written, informed consent was obtained from the patients to use the content and imaging material for submission and publication of this case report.
Funding
This study was supported by grants from the National High Level Hospital Clinical Research Funding (No. 2022-PUMCH-A-150).
Declaration of competing interest
The authors declare no competing interests.
Acknowledgement
Not applicable.
References
- 1.Biewend M.L., Menke D.M., Calamia K.T. The spectrum of localized amyloidosis: a case series of 20 patients and review of the literature. Amyloid. 2006 Jul 06;13(3):135–142. doi: 10.1080/13506120600876773. [DOI] [PubMed] [Google Scholar]
- 2.Al-Obaidy K.I., Grignon D.J. Primary amyloidosis of the genitourinary tract. Arch Pathol Lab Med. 2021 Jun 1;145(6):699–703. doi: 10.5858/arpa.2020-0102-RA. [DOI] [PubMed] [Google Scholar]
- 3.Picken M.M. The pathology of amyloidosis in classification: a review. Acta Haematol. 2020 May 11;143(4):322–334. doi: 10.1159/000506696. [DOI] [PubMed] [Google Scholar]
- 4.Buxbaum J.N., Dispenzieri A., Eisenberg D.S., et al. Amyloid nomenclature 2022: update, novel proteins, and recommendations by the international society of amyloidosis (ISA) nomenclature committee. Amyloid. 2022 Nov 24;29(4):213–219. doi: 10.1080/13506129.2022.2147636. [DOI] [PubMed] [Google Scholar]
- 5.Varghese S., Wong N.C., Shayegan B. Images in urology: localized primary amyloidosis of the urinary bladder. Can Urol Assoc J. 2018 Jan;12(1):E42–E44. doi: 10.5489/cuaj.4825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tirzaman O., Wahner-Roedler D.L., Malek R.S., Sebo T.J., Li C.Y., Kyle R.A. Primary localized amyloidosis of the urinary bladder: a case series of 31 patients. Mayo Clin Proc. 2000 Dec;75(12):1264–1268. doi: 10.4065/75.12.1264. [DOI] [PubMed] [Google Scholar]
- 7.Regmi A., Mehta M., Farooq A.V., Turk T.M., Wojcik E.M., Picken M.M. Localized urinary bladder amyloidosis as urothelial cancer mimicker. Arch Pathol Lab Med. 2024 May;10 doi: 10.5858/arpa.2023-0559-OA. [DOI] [PubMed] [Google Scholar]
- 8.Glenner G.G. The pathogenetic and therapeutic implications of the discovery of the immunoglobulin origin of amyloid fibrils. Hum Pathol. 1972 Jun;3(2):157–162. doi: 10.1016/s0046-8177(72)80069-8. [DOI] [PubMed] [Google Scholar]
- 9.Rosenmann E., Eliakim M. Nephrotic syndrome associated with amyloid-like glomerular deposits. Nephron. 1977 May 11;18(5):301–308. doi: 10.1159/000180846. [DOI] [PubMed] [Google Scholar]
- 10.Cheng Z., Cui Q., Tian Z., Zhao D., Zhu K., Fang Q. Electron microscopy in patients with clinically suspected of cardiac amyloidosis who underwent endomyocardial biopsy and negative Congo red staining. Int J Cardiol. 2013 Oct 3;168(3):3013–3015. doi: 10.1016/j.ijcard.2013.04.054. [DOI] [PubMed] [Google Scholar]
- 11.Malek R.S., Wahner-Roedler D.L., Gertz M.A., Kyle R.A. Primary localized amyloidosis of the bladder: experience with dimethyl sulfoxide therapy. J Urol. 2002 Sep;168(3):1018–1020. doi: 10.1016/S0022-5347(05)64564-8. [DOI] [PubMed] [Google Scholar]
- 12.Livingstone R.R., Sarembock L.A., Barnes R.D., Folb P.I. Colchicine therapy in primary amyloidosis of the bladder: a case report. J Urol. 1989 Dec;142(6):1570–1571. doi: 10.1016/s0022-5347(17)39168-1. [DOI] [PubMed] [Google Scholar]