Abstract
Introduction
Fournier's gangrene, a polymicrobial infection affecting the scrotum and perineal area, predominantly affects elderly males, presenting challenges in diagnosis and management. This report examines two cases, with a focus on the rare outcome of bilateral orchidectomy.
Case presentation
A 69-year-old diabetic male presented with severe penile and scrotal pain, leading to the diagnosis of Fournier's gangrene. In another case, a 91-year-old male with a history of Benign Enlargement of the Prostate experienced scrotal pain and ulcerative lesions, resulting in a rapid progression of gangrene. The surgical approaches encompassed multiple debridement and bilateral orchidectomy, underscoring the intricate nature of managing Fournier's gangrene.
Discussion
Fournier's gangrene typically originates as a polymicrobial infection in the genitourinary or perianal regions, with common risk factors including diabetes, immunosuppression, and advanced age. Diagnosis often relies on clinical assessment, though imaging aids in complex cases. Early intervention with broad-spectrum antibiotics and repeated debridement remains the cornerstone of treatment.
Conclusion
Fournier's gangrene, a rare condition, poses diverse clinical presentations, management strategies, and outcomes. Early recognition, aggressive surgical debridement, and a multidisciplinary approach are essential in managing this condition.
Keywords: Fournier's gangrene, Necrotizing fasciitis, Scrotum, Surgical debridement
Highlights
-
•
Fournier's gangrene is a rare, severe infection of the scrotum and perineum, challenging to diagnose and manage in elderly males.
-
•
This report discusses two elderly males with Fournier's gangrene, both requiring the rare intervention of bilateral orchidectomy.
-
•
A 69-year-old diabetic male with severe scrotal pain underwent multiple debridements and bilateral orchidectomy for management.
-
•
A 91-year-old male with BPH experienced rapid progression of Fournier's gangrene, necessitating bilateral orchidectomy.
-
•
Treatment includes aggressive debridement, broad-spectrum antibiotics, medical resuscitation, and reconstructive surgery post-debridement.
1. Introduction
Fournier's gangrene is a perianal-origin polymicrobial infection that evolves into necrotizing fasciitis affecting the scrotum and perineal area, characterized by rapid necrotic expansion along fascial planes towards the abdominal wall and flank region [1]. It predominantly affects males over females, exhibiting a notable 10 to 1 ratio, with an incidence of 1.6 cases per 100,000 men [2]. Fournier's gangrene is most frequently observed in men aged 50 to 79, with an incidence rate of 3.3 cases per 100,000 men [3,4]. Although Fournier's gangrene may manifest in healthy individuals, it is commonly linked to a debilitated or immunocompromised condition.
The mortality rate of this disease remains elevated, varying between 20 % and 50 % [5]. Fournier's Gangrene constitutes an uncommon and life-threatening soft tissue infection, capable of swiftly escalating to systemic toxicity if not promptly addressed [2]. Complications associated with Fournier's gangrene can manifest in both the short and long term.
This case report aims to present two distinct cases of Fournier's gangrene in elderly male patients, emphasizing the diverse clinical presentations, management strategies, and outcomes. The rarity of bilateral orchidectomy as an outcome in Fournier's gangrene underscores the need for a thorough exploration of the cases presented herein. This case report adheres to the SCARE checklist [6].
2. Case presentation
2.1. Case 1
A 69-year-old man presented to the emergency room with complaints of pain and swelling in the penile region and scrotum for four days. The swelling had insidious onset, and there was no history of trauma, malignancy, insect bites, or other injuries. The swelling was accompanied by fever and foul-smelling discharge, extending from the underside of the scrotum to the dorsal portion of the penis. The patient, a chronic smoker who occasionally consumes alcohol, was found to have Diabetes Mellitus after admission (random blood sugar: 332 mg/dL).
Upon admission, the patient was attentive and febrile, with stable vital signs and no symptoms of respiratory distress or dehydration. Local examination revealed a five cm lesion on the dorsal aspect of the penis and a yellowish slough extending to the undersurface of the scrotum. The yellowish-sloughed scrotum was reddened. Systemic examination findings were unremarkable. Laboratory findings revealed leukocytosis (WBC: 18,500/μL) and elevated CRP (185 mg/L).
His blood sample was sent for antibiotic sensitivity testing and microbiological culture. The blood culture showed no bacterial growth. Urine analysis indicated the presence of >10^5 CFU/ML of Escherichia coli. Escherichia coli was also identified during the microbiological culture of the tissue sample, confirming the diagnosis of Fournier's Gangrene. The patient received empiric broad-spectrum antibiotic therapy, including carbapenems (1 g IV every 6 h) in combination with Clindamycin (600 mg IV every 8 h) and Vancomycin (20 mg/kg IV every 8 h).
Emergency surgical debridement was performed in the inguinal region surrounding the wound. The procedure was performed under general anesthesia. The patient was positioned in lithotomy to optimize surgical access to the perianal and perineal regions. A diverting colostomy was performed to prevent fecal contamination of the wound bed. Hemostasis was ensured, and negative pressure wound therapy was applied postoperatively. In total, surgical debridement was performed five times. During the debridement process, the patient also experienced a urethral injury. Buccal Mucosa Graft (BMG) urethroplasty technique was utilized to address the urethral injury (Fig. 1). Foley's catheter was kept in the urethra to make the urethra patent, which also prevented complications like stricture formation. A suprapubic catheter was administered to drain urine (Fig. 2A). To manage his diabetes, the patient was prescribed 1800 Kcal/day diet and given Metformin 500 mg twice a day. After one month, bilateral orchidectomy, urethroplasty and split-thickness skin graft of the penis from the medial region of the thigh of the left leg were performed (Fig. 2B). Bilateral orchidectomy was performed due to extensive involvement of the testicular tissues. The decision for orchidectomy was made based on the clinical assessment, which revealed significant testicular compromise as part of the necrotizing infection. The patient was kept under evaluation for some days. Postoperative recovery was uneventful, and the patient was discharged with proper wound care instructions. At the final follow-up visit, six months post-discharge, the patient showed complete wound healing and no evidence of recurrence.
Fig. 1.
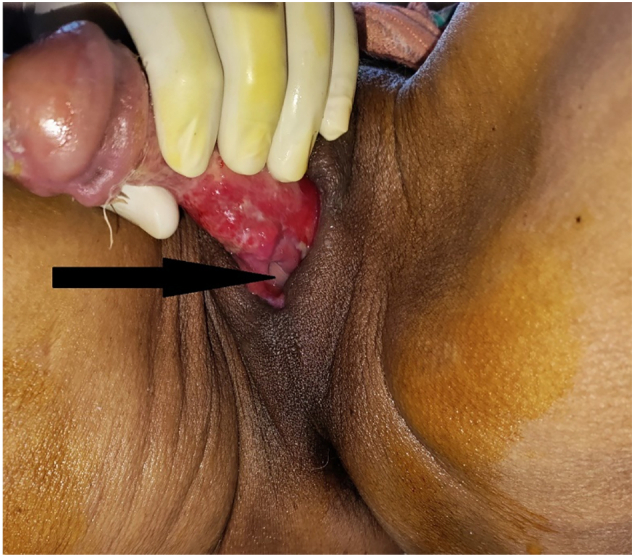
The black arrow indicates Foley's catheter, signifying urethral injury during debridement.
Fig. 2.
A. Preoperative view of penis and scrotum with debrided skin before undergoing orchidectomy, skin graft and urethroplasty.
B. Postoperative view showing bilateral orchidectomy and split thickness skin graft of penis.
2.2. Case 2
A 91-year-old man with a medical history of Benign Enlargement of Prostate (BEP), under medication for 8 years, presented to our surgical department due to pain over the right scrotum for 1 month. Additionally, he had an ulcerative lesion over the right scrotum for 15 days with foul-smelling discharge. The pain was insidious, dull in nature, non-radiating, with no aggravating or relieving factors. The scrotum initially swelled, followed by the formation of a gradually increasing wound measuring approximately 3*5 cm. Laboratory investigations revealed elevated white blood cell (WBC) count of 22,000/μL, C-reactive protein (CRP) of 245 mg/L, direct bilirubin (0.34 mg/dL), reduced hemoglobin (10.7 g/dL), and a PT/INR ratio of 12.4 s.
The patient underwent scrotal and pubic exploration in the operative room. Under saddle block, supine position, painting, and draping were performed. Full debridement of necrotic fascia and subcutaneous tissue was carried out. A protective diverting colostomy was created to minimize contamination. After thorough irrigation with saline and antiseptic solutions, a vacuum-assisted closure (VAC) system was applied. The patient underwent a total of four surgical debridement procedures. Group A Streptococci was identified during the microbiological culture of the tissue sample. In spite of the implementation of aggressive drainage and broad-spectrum antibiotic therapy, the progression of gangrene was rapid, worsening the patient's general condition within hours. Subsequently, due to the rapid deterioration, a secondary extensive debridement was undertaken, involving bilateral orchidectomy (Fig. 3).
Fig. 3.

Postoperative view of open scrotum after debridement and bilateral orchidectomy.
The patient underwent intravenous antibiotic therapy, which consisted of Flucloxacillin (500 mg, four times a day for 3 days) and Ceftriaxone (1 g, twice a day for 4 days). Additionally, Intravenous Paracetamol was administered at a dose of 1 g, thrice a day for 4 days, and Intravenous Pantoprazole at a dose of 40 mg, once a day for 2 days. Metronidazole, 500 mg, was given intravenously thrice a day for 4 days. Subsequently, the patient transitioned to oral medications, including tablet metronidazole (400 mg, thrice a day), tablet Flucloxacillin (500 mg, four times a day), tablet Pantoprazole (40 mg, once a day), and tablet Paracetamol (500 mg for two days). At the time of discharge, the patient was hemodynamically stable. The patient remained regular on follow-ups, and no adverse events were encountered. At the one-year follow-up, the patient demonstrated complete wound healing, and no recurrence of infection.
3. Discussion
Fournier's gangrene typically arises as a polymicrobial infection with origins in the genitourinary or perianal region. However, determining the precise portal of entry is often challenging. The primary origin often involves a polymicrobial source, with Group A streptococcus being the most frequently identified organism, yet the fundamental cause remains inadequately understood [7]. Numerous predisposing factors have been documented in the literature, with common occurrences including diabetes, alcoholism, old age, paraplegia, obesity, renal insufficiency, underlying neoplasms and chronic vascular disease [8,9].
Our Case 1 involved a patient with diabetes who was also a chronic smoker and occasional alcohol consumer. The Case 2 had a history of Benign Enlargement of the Prostate (BEP). These cases highlight the diverse predisposing factors and underscore the importance of recognizing and managing these risks for optimal patient outcomes.
The initial indicators of potential Fournier gangrene encompass pruritus, localized soreness, swelling, and redness affecting the perineal, scrotal, or labial skin, along with systemic manifestations like fever, chills, nausea, vomiting, urinary retention, and malaise [10]. A classic hallmark of Fournier's gangrene is the presence of severe pain that is disproportionately intense compared to the observable physical findings [3]. In alignment with this characteristic, our Case 1, a 69-year-old male, experienced intense pain and sought emergency medical attention due to pain and swelling in the penile and scrotal region.
Fournier's gangrene is primarily diagnosed clinically; however, in challenging situations where uncertainty persists, radiological assessment becomes valuable for confirmation. Ultrasound imaging and X-rays are instrumental in detecting subcutaneous gas or emphysema within the underlying soft tissue, aiding in diagnostic visualization [11]. Yet, among all diagnostic modalities, a CT scan holds superior value for assessing the extent of the disease [12]. While CT and MRI are often employed to delineate the spread of infection, imaging was not performed in our cases due to the patient's critical condition upon arrival. The diagnosis was made clinically based on the rapid spread of infection and systemic instability. Elevated WBC is often observed in CBC, while the comprehensive metabolic panel (CMP) may reveal electrolyte abnormalities such as hyponatremia or metabolic acidosis [13]. Both of our cases revealed elevated WBC in CBC.
Aggressive surgical debridement of necrotic tissue, combined with the use of broad-spectrum antibiotics, constitutes the cornerstone in the treatment of Fournier's gangrene [13]. Critical medical resuscitation is imperative, given that patients often present with sepsis and shock [10]. Medical intervention centers on promptly initiating empiric broad-spectrum antibiotics while awaiting culture sensitivities. While essential, the antibiotic and resuscitative measures should not impede the urgent, early, and aggressive surgical exploration and debridement, which constitutes the definitive therapy [14].
After surgical debridement, the crucial phase of local wound care involves employing methods such as vacuum-assisted closure devices (VAC dressing) and wet-to-dry dressings [15]. Patients often require reconstructive surgery with adequate tissue coverage for the affected area following the development of granulation tissue [16].
4. Conclusion
Fournier's gangrene, a rare condition poses a formidable challenge, necessitating a multidisciplinary approach for optimal patient care. Managing underlying risk factors, as exemplified in the presented cases, is equally crucial for preventing and addressing the recurrence of Fournier's gangrene. The elevated mortality rates associated with this condition underscore the continued need for research, awareness, and collaborative efforts in managing this rare but severe soft tissue infection.
Consent
Written informed consent was obtained from the patient for publication of this case report. A copy of the written consent is available for review by the editor-in-chief of this journal on request.
Ethical approval
This is a case report, therefore, it did not require ethical approval from ethics committee.
Guarantor
Suchit Thapa Chhetri.
Research registration number
Not applicable.
Provenance and peer review
Not commissioned, externally peer reviewed.
Funding
The study did not receive any grant from funding agencies in the public, commercial or not-for-profit sectors.
CRediT authorship contribution statement
Suchit Thapa Chhetri: Conceptualization, Data curation, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. Sumit Kumar Sah: Data curation, Validation, Visualization, Writing – original draft, Writing – review & editing. Indra Dev Pathak: Validation, Visualization, Writing – original draft, Writing – review & editing. Niraaz Pokhrel: Validation, Visualization, Writing – original draft, Writing – review & editing. Prem Khadka Thyayat: Validation, Visualization, Writing – original draft, Writing – review & editing. Nitesh Kumar Shah: Validation, Visualization, Writing – original draft, Writing – review & editing.
Declaration of competing interest
The authors report no conflicts of interest.
Acknowledgment
None.
References
- 1.Hartzell TL, Orgill DP. Fournier gangrene. In: Téot L, Meaume S, Akita S, Ennis WJ, del Marmol V, eds. Skin Necrosis. Springer; 2015:187–194. doi: 10.1007/978-3-7091-1241-0_32 [Google Scholar] [Full Text]. [DOI]
- 2.Hasham S., Matteucci P., Stanley P.R.W., Hart N.B. Necrotising fasciitis. BMJ. 2005;330(7495):830–833. doi: 10.1136/bmj.330.7495.830. (PubMed, Google Scholar, Full Text) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Auerbach J., Bornstein K., Ramzy M., Cabrera J., Montrief T., Long B. Fournier gangrene in the emergency department: diagnostic dilemmas, treatments and current perspectives. Open Access Emerg Med. 2020;12:353–364. doi: 10.2147/OAEM.S238699. (PubMed, Google Scholar, Full Text) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gadler T., Huey S., Hunt K. Recognizing Fournier’s gangrene in the emergency department. Adv. Emerg. Nurs. J. 2019;41(1):33–38. doi: 10.1097/TME.0000000000000221. (PubMed, Google Scholar, Full Text) [DOI] [PubMed] [Google Scholar]
- 5.Montrief T., Long B., Koyfman A., Auerbach J. Fournier gangrene: a review for emergency clinicians. J. Emerg. Med. 2019;57(4):488–500. doi: 10.1016/j.jemermed.2019.06.023. (PubMed, Google Scholar, Full Text) [DOI] [PubMed] [Google Scholar]
- 6.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg Lond Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. (PubMed, Google Scholar, Full Text) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leitch H.A., Palepu A., Fernandes C.M. Necrotizing fasciitis secondary to group A streptococcus. Morbidity and mortality still high. Can. Fam. Physician. 2000;46:1460–1466. (PubMed, Google Scholar, Full Text) [PMC free article] [PubMed] [Google Scholar]
- 8.Singh G., Sinha S.K., Adhikary S., Babu K.S., Ray P., Khanna S.K. Necrotising infections of soft tissues—a clinical profile. Eur. J. Surg. 2002;168(6):366–371. doi: 10.1080/11024150260284897. (PubMed, Google Scholar, Full Text) [DOI] [PubMed] [Google Scholar]
- 9.White N.R., Fowler L.L. Retroperitoneal and cutaneous necrotizing fasciitis secondary to necrotizing pancreatitis. J. Emerg. Med. 2014;47(2):147–149. doi: 10.1016/j.jemermed.2014.02.009. (PubMed, Google Scholar, Full Text) [DOI] [PubMed] [Google Scholar]
- 10.Chernyadyev S.A., Ufimtseva M.A., Vishnevskaya I.F., et al. Fournier’s gangrene: literature review and clinical cases. Urol. Int. 2018;101(1):91–97. doi: 10.1159/000490108. (PubMed, Google Scholar, Full Text) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Di Serafino M., Gullotto C., Gregorini C., Nocentini C. A clinical case of Fournier’s gangrene: imaging ultrasound. J. Ultrasound. 2014;17(4):303–306. doi: 10.1007/s40477-014-0106-5. (PubMed, Google Scholar, Full Text) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rajan D.K., Scharer K.A. Radiology of Fournier’s gangrene. AJR Am. J. Roentgenol. 1998;170(1):163–168. doi: 10.2214/ajr.170.1.9423625. (PubMed, Google Scholar, Full Text) [DOI] [PubMed] [Google Scholar]
- 13.Leslie SW, Rad J, Foreman J. Fournier gangrene. In: StatPearls. StatPearls Publishing; 2023. Accessed December 29, 2023. http://www.ncbi.nlm.nih.gov/books/NBK549821/ [PubMed] [Google Scholar] [Full Text]. [PubMed]
- 14.Wong C.H., Wang Y.S. The diagnosis of necrotizing fasciitis. Curr. Opin. Infect. Dis. 2005;18(2):101. doi: 10.1097/01.qco.0000160896.74492.ea. (PubMed, Google Scholar, Full Text) [DOI] [PubMed] [Google Scholar]
- 15.Birnbaum D.J., D’Journo X.B., Casanova D., Thomas P.A. Necrotizing fasciitis of the chest wall. Interact. Cardiovasc. Thorac. Surg. 2010;10(3):483–484. doi: 10.1510/icvts.2009.222323. (PubMed, Google Scholar, Full Text) [DOI] [PubMed] [Google Scholar]
- 16.Black P.C., Friedrich J.B., Engrav L.H., Wessells H. Meshed unexpanded split-thickness skin grafting for reconstruction of penile skin loss. J. Urol. 2004;172(3):976–979. doi: 10.1097/01.ju.0000133972.65501.44. (PubMed, Google Scholar, Full Text) [DOI] [PubMed] [Google Scholar]



