Abstract
Background
Subarachnoid hemorrhage (SAH) remains a serious public health problem worldwide, especially in economically developed regions/countries. This study intends to thoroughly analyze the incidence, mortality, and disability-adjusted life years (DALYs) rate of SAH at the global, regional, and national levels. This study focused on the differences in SAH incidence between China and Japan from 1990 to 2019, and projected global, Chinese, and Japanese SAH incidence rates until 2030.
Methods
Data on the disease burden owing to SAH from 1990 to 2019 were obtained from the Global Burden of Disease (GBD) Study 2019. linear regression analysis was used to calculate the estimated annual percentage change (EAPC) and linear regression method was used to calculate the average annual percentage change (AAPC). Bayesian age-period-cohort (BAPC) model was used to predict the disease burden from 2020 to 2030.
Results
Globally, age-standardised incidence, mortality, and DALYs rates was declined from 1990 to 2019. In 1990–2019, the incidence of SAH decreased in China, while it increased in Japan, especially among middle-aged and elderly women. Projections suggest that the global incidence of SAH will decrease by 2.06% in 2030, with an increase of 6.24% in China and 13.82% in Japan, with the highest increase among Japanese women being 16.19%.
Conclusions
Global SAH incidence, mortality, and DALYs rates declined over the 1990–2019 period, with regional/national SAH mortality and DALYs rates negatively correlated with socio-demographic index (SDI), while SAH incidence was positively correlated with SDI. The incidence of SAH decreased in China and increased in Japan during this period. The predictions show that over the next 10 years, while the incidence of SAH continues to decline globally, the incidence of SAH in China and Japan has increased. Thus, SAH remains a serious disease burden that requires early intervention targeting risk factors and populations at risk that may have increased because of economic development.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-21227-9.
Keywords: Subarachnoid hemorrhage, Disease burden, China, Japan, Prediction
Introduction
Subarachnoid hemorrhage (SAH) is a type of stroke that usually results from a ruptured aneurysm [1]. According to the Global Burden of Disease (GBD) 2019 estimates, the number of people who will die from SAH in 2019 will be about 370,000 globally, about 90,736 in China, and about 14,508 in Japan [2]. The disease burden of SAH is more severe in China and Japan compared to the global average. In addition to this, there is a considerable difference in SAH incidence rates between China and Japan from 1990 to 2019. It has been reported that the incidence of SAH in China decreased by 39.3% from 1990 to 2019, whereas it increased by 77% in Japan [2]. The reasons for the large difference in the incidence of SAH between China and Japan are not known.
The GBD database has the advantage of systematically analyzing and integrating global disease and health data, and its use can provide policymakers, researchers, and the public with a comprehensive understanding of the SAH disease burden at the global, regional, and national levels [3]. In this study, we first assessed the global and regional/national SAH disease burden by combining the estimated annual percentage change (EAPC) and average annual percentage change (AAPC) [4, 5]. After finding significant differences in SAH incidence rates between China and Japan from 1990 to 2019, we comparatively analyzed the potential reasons for the differences in incidence rates between China and Japan. Finally, we attempted to predict the incidence of SAH in the next 10 years globally, in China, and in Japan using Bayesian model for age-period-cohort (BAPC) [6, 7]. Our results help policy makers to develop more effective policies targeting SAH risk factors and at-risk populations to reduce the risk of developing SAH.
Methods
GBD 2019
Data downloaded from GBD 2019 (https://vizhub.healthdata.org/gbd-results/). GBD 2019 estimates 369 cases of diseases and injuries in 7 GBD super-regions, 21 GBD regions, and all countries/ territories, and is a systematic, collaborative global database [3]. GBD 2019 contains many indicators, such as DALYs. We extracted information about SAH from the database and analyzed age-standardized incidence rate, age-standardized mortality rate and age-standardized DALYs.
Evaluation of SAH-related burdens
Incidence, mortality and DALY are used in the GBD database to assess the burden of SAH in this study. Incidence was defined as the number of new SAH cases in a region or country at a specific time (one year) divided by the population of the region or country. The mortality rate is the proportion of SAH deaths per 100,000 population and is determined by the number of deaths caused by SAH each year. Years of life lost (YLLs) are calculated as the difference in standard life expectancy minus age at death. While years lived with Disability (YLDs) refers to the number of years lived with disability. DALYs is the sum of YLLs and YLDs, use population total health loss as the variable to estimate the total burden of SAH [8]. This study used age-standardized rate to eliminate the influence of population age structure is different, to ensure the comparability of statistical indicators [8].
Socio-demographic index (SDI)
The SDI, which ranges from 0 (worst) to 1 (best), is a composite of the total fertility rate under 25 years of age, the average educational attainment of the population aged 15 years and older, and per capita income with lagged distribution [9]. Pearson analysis of the correlation of age-standardized incidence, mortality, and DALYs rates with the SDI can better reveal the association between the disease burden of SAH and the economic development of a country or region.
Statistical analyses
All statistical analyses were performed using R Studio software (version 4.2.2) and Joinpoint Software (version 5.0.2, National Cancer Institute, USA) and the two-tailed P value < 0.05 was considered statistically significant. In assessing temporal trends in SAH disease burden, we combined two mainstream metrics for our analyses, the AAPC and the EAPC. The AAPC is a geometrically weighted average of the annual percentage change computed in Joinpoint software. AAPC and its 95% confidence interval (CI) > 0 indicated an upward trend, while AAPC and its 95% CI < 0 indicated a downward trend [4]. The EAPC was calculated based on a regression model, specifically: [ln (age-standardized rate) =α + β× (calendar year) +ε]. The EAPC and its 95% CI were calculated from the model of [100×(exp (β)- 1)]. An upward trend is indicated when the lower limit of the 95% CI of the EAPC is > 0, while a downward trend is indicated when the upper limit of the 95% CI of the EAPC is < 0 [5]. In addition, to predict the disease burden of SAH to 2030, we used the BAPC. The BAPC model is expressed as follows: nij = log(λij) = µ + αi + βj + γk, where λij denotes the number of cases, µ denotes the intercept, and αi, βj, and γk represent the effects of age, period and cohort [6, 7]. The model was implemented in R Studio software using the INLA and BAPC packages. The projected population was taken from World Population Prospects 2022 [10].
Results
Global trends
The age-standardised incidence rate due to subarachnoid hemorrhage in 2019 was 14.46 (95% uncertain interval (UI), 12.33–16.94) per 100,000 population (Table S1), the age-standardised mortality rate in 2019 was 4.66 (95%UI, 4.13–5.17) per 100,000 population (Table S2) and the age-standardised DALYs rate in 2019 was 136.47 (95%UI, 120.83-154.66) per 100,000 population (Table S3). The EAPC of incidence rate in global was − 0.81 (95% confidence interval (CI), -0.86–0.76) (Table S1). The EAPC of mortality rate in global was − 3.52 (95% CI, -3.83–3.2) (Table S2). The EAPC of DALYs rate in global was − 3.13 (95% CI, -3.39–2.88) (Table S3). The AAPC of incidence rate in global was − 0.63 (95% CI, -0.65–0.61) (Table S4). The AAPC of mortality rate in global was − 2.91 (95% CI, -2.94–2.87) (Table S4). The AAPC of DALYs rate in global was − 2.65 (95% CI, -2.68–2.63) (Table S4).
Global subarachnoid hemorrhage mortality and DALYs rates have been declining, and the incidence reached an inflection point in 2014 after a sustained decline. Although not statistically significant, the annual percentage changes from 2014 to 2019 were greater than zero for the first time (Fig. 1A-C).
Fig. 1.
Temporal trend in incidence, mortality, and DALYs of subarachnoid hemorrhage. (A-C): Joinpoint regression analysis of Global. (APC, annual percentage change; DALYs, disability-adjusted life-years)
Regional trends
The incidence of EAPC in most regions showed a downward trend, and the decline was most obvious in East Asia, EAPC=-2.56 (95% CI, -2.93–2.17) (Table S1), By GBD region, East Asia mainly includes (China, Taiwan (province of China) and the democratic people’s republic of Korea). The incidence of EAPC in High-income Asia Pacific increased by 1.88 (95% CI, 1.52–2.24) (Table S1). According to GBD, the High-income Asia Pacific region mainly includes (Brunei Darussalam, Japan, Republic of Korea, Singapore). Mortality declined in most regions, with the largest decline in East Asia EAPC=-7.57 (95% CI, -8.43- -6.71) (Table S2). Only in Central Asia was the mortality rate increased by 0.58 (95% CI, 0.45–0.71) (Table S2), Including (Armenia, Azerbaijan, Georgia, Kazakhstan, Kyrgyzstan, Mongolia, Tajikistan, Turkmenistan, Uzbekistan). DALYs showed a downward trend in all regions, and the largest decline was in East Asia (-6.9 (95% CI, -7.67–6.12)) (Table S3).
The incidence of AAPC decreased, and the decrease was most obvious in East Asia − 1.67(95% CI, -1.72–1.6) (Table S4). AAPC of High-income Asia Pacific is increased 1.2 (95% CI, 1.15–1.25) (Table S4). The lowest mortality of AAPC is -6.04(95% CI, -6.12–5.95) (Table S4) in East Asia and the highest is 0.48 (95% CI, 0.4–0.57) (Table S4) in Central Asia. AAPC of DALYs in East Asia decreased by a maximum of -5.56(95% CI, -5.63–5.49) (Table S4). Eastern Europe has an increase of up to 0.16(95% CI, 0.07–0.25) (Table S4), according to the GBD subregion Eastern Europe includes Belarus, Estonia, Latvia, Lithuania, Republic of Moldova, Latvia, Latvia, Latvia, Latvia, and the Republic of Moldova. Russian federation and Ukraine.
Regional SDI is positively correlated with incidence rate, with person coefficient = 0,40 (Fig. 2A); regional SDI is negatively correlated with mortality rate, with person coefficient =-0.17(Figure S1A); regional SDI is negatively correlated with DALYs rate, with person coefficient =-0.15 (Figure S2 A).
Fig. 2.
Age-standardised incidence rates for subarachnoid hemorrhage by Socio-demographic Index. (A): 21 GBD regions; (B): 204 countries and territories
Nation trends
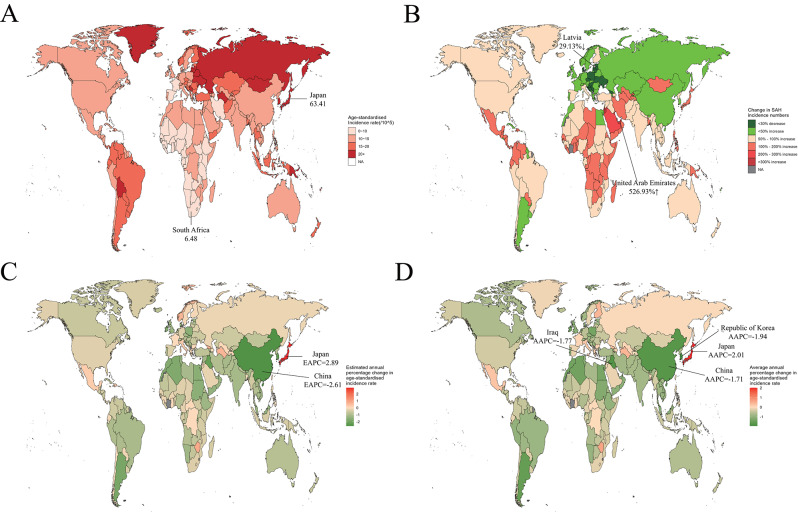
The country with the highest decrease in EAPC incidence is china-2.61(95% CI, -3–2.22), the highest increase is japan2.89(95% CI, 2.43–3.36) (Fig. 3C) (Table S5). The lowest mortality rate is china-7.7(95% CI, -8.56–6.82), the highest in the Philippines is 2.7(95% CI, 2.06–3.35) (Figure S3 C) (Table S6). The lowest EAPC in DALYs is -7.03(95% CI, -7.82–6.23) in China, and the highest is 2.99(95% CI, 2.35–3.64) in Philippines (Figure S4 C) (Table S7).
Fig. 3.
The global disease burden of subarachnoid hemorrhage. (A): The age- standardissed incidence rate of subarachnoid hemorrhage in 2019; (B): The change in subarachnoid hemorrhage incidence numbers in 2019; (C): The estimated annual percentage change in age- standardised incidence rate of subarachnoid hemorrhage in 2019; (D): The average annual percentage change in age- standardised incidence rate of subarachnoid hemorrhage in 2019
At the national level, the highest reduction of AAPC in the Republic of Korea is 1.94(95% CI, -1.97–1.91), China is -1.71(95% CI, -1.76–1.64), ranking the third, and the highest is Japan (2.01(95% CI, 1.96–2.06)) (Fig. 3D) (Table S8). China has the lowest mortality rate − 6.12(95% CI, -6.24–5.96), the highest is Philippines1.76(95% CI, 1.65–1.91) (Figure S3 D) (Table S8). The lowest AAPC of DALYs was China (-5.66(95% CI, -5.75–5.52)) and the highest was Philippines (2.01(95% CI, 1.88–2.16)) (Figure S4 D) (Table S8).
There is a positive correlation between national SDI and incidence (person coefficient = 0.31) (Fig. 2B), and a negative correlation between national SDI and mortality (person coefficient =-0.14) (Figure S1B). There is no current correlation between national SDI and DALYs (Figure S2 B).
Although the EAPC and AAPC with the lowest incidence reduction are not exactly the same, we can still find a large difference in incidence between China and Japan. Next, we plan to analyze this difference in more detail.
The burden of SAH in China and Japan from 1990 to 2019
Combining the results of EAPC and AAPC, we found that China and Japan showed a decreasing trend in both mortality and DALYs rates (Table S6,7,8), but there was a huge difference in incidence rate, with China’s SAH incidence decreasing from 1990 to 2019, while Japan’s SAH incidence increased from 1990 to 2019 (Table S5,8). There were four join points in the incidence rate in China during 1990–2019, which were 1993, 1996, 2005 and 2014, among which the most obvious decrease was − 5.85 (95% CI, -5.98–5.71) during 1996–2005(Fig. 4A). From 1990 to 2019, the incidence in Japan showed five turning points in 1993, 1996, 2000, 2004 and 2007, among which the fastest increase in 2000–2004 was 11.07 (95% CI, 2.01–11.47) (Fig. 4B). By age stratification of patients, it was found that in 1990, China had more patients over 80 years old than Japan, 174.38 (95% UI, 130.79-226.88) vs. 148.91 (95% UI, 107.38-197.93) (Fig. 4C). In 2019, the incidence increased in all age groups in Japan, surpassing that in China, with the largest increase in the 55–59 age group, which increased by about 1.75 times in 1990 (Fig. 4D). Compared with 1990, in 2019, the incidence rate of male and female of all ages in China was declining, while the incidence rate of male over 30 years old in Japan was rising, among which the increase rate of male aged 55–59 was the highest 2.02 times, and the incidence rate increased in female over the age of 30, with the highest increase in female aged 50–54, which was 2.08 times that of 1990 (Fig. 4E-F).
Fig. 4.
Comparison of subarachnoid hemorrhage incidence in China and Japan. (A): Joinpoint regression analysis of China; (B): Joinpoint regression analysis of Japan; (C): Age distribution of China and Japan in 1990; (D): Age distribution of China and Japan in 2019; (E): Age and sex distribution of China and Japan in 1990; (F): Age and sex distribution of China and Japan in 2019
SAH burden predictions for global, China, and Japan
The incidence of SAH worldwide is projected to decline from 14.39 per 100,000 people in 2020 to 14.09 per 100,000 people in 2030, a decrease of 2.06% (Figure S5). However, the age-standardised incidence rate of SAH is expected to increase in China and Japan between 2020 and 2030. Among them, the incidence of SAH in China increased from 11.37 per 100,000 people in 2020 to 12.08 per 100,000 people, an increase of 6.24% (Fig. 5A); The incidence in Japan increased from 73.08 per 100,000 people in 2020 to 83.18 per 100,000 people, an increase of 13.82% (Fig. 5D). According to the forecast data, the incidence rate of Japan is higher than that of China. In China, the male incidence rate increased from 10.53 per 100,000 in 2020 to 11.37 per 100,000 in 2030, an increase of 7.92% (Fig. 5B); The incidence in female increased from 12.11 per 100,000 in 2020 to 13.05 per 100,000 in 2030, an increase of 7.76% (Fig. 5C). According to the predicted data, the incidence rate of Chinese male is higher than that of female. In Japan, the male incidence rate increased from 51.82 per 100,000 in 2020 to 54.65 per 100,000 in 2030, an increase of 5.47% (Fig. 5E); The incidence rate in female will increase from 90.78 per 100,000 people in 2020 to 105.49 per 10,000 people in 2030, an increase of 16.19% (Fig. 5F), and according to the projected data, the increase is greater in Japanese female than in male.
Fig. 5.
Prediction of incidence of subarachnoid hemorrhage in 2020–2030. (A): China; (B): China Male; (C): China Female; (D): Japan; (E): Japan Male; (F): Japan Female
Discussion
This study analyzed the magnitude and temporal trends of SAH-related disease burden in the world, China and Japan from 1990 to 2019, and made projections up to 2030. Our results showed that the age-standardized incidence rate, mortality rate and DALYs rate of SAH have decreased globally (including China) in the past three decades, while the age-standardized incidence rate of SAH in Japan has increased while the age-standardized mortality rate and DALYs rate have decreased. We also found an increase in age-standardized incidence rates in China and Japan by 2030, and the trends suggest that SAH remains and will continue to be a serious disease burden in China and Japan for some time, and that more targeted measures should be taken in a timely manner to reduce this burden [11].
We found that age-standardized mortality and DALYs rates were negatively associated with SDI across countries/regions globally, whereas age-standardized morbidity rates were positively associated with SDI. Consistent with our results, SAH was also found to be more than twice as likely among new stroke cases in the World Bank’s high-income group as in the low-income to upper-middle-income groups in other reports (19.7% vs. 7.9%) [12]. This may be because populations in areas with higher SDI are more likely to be exposed to hypertension and smoking, two major risk factors for SAH [1, 13]. For example, the age-standardized prevalence rates EAPC and AAPC were the highest in this study Japan is the world’s fourth largest consumer of smoking and has a higher prevalence of smoking than other high-income countries [14]. Moreover, Japan has a high prevalence of hypertension, which, according to the 2016 Japan National Health and Nutrition Survey, is 60% in men and 41% in women aged 40–74 years, and 74% in men and 77% in women aged 75 years and older [15].
When gender was not considered, we found that the incidence of SAH in both China and Japan showed an increasing trend with age, which is in line with the world trend [13]. This indicates that the burden of SAH is still very serious among middle-aged and elderly people. We speculate that this phenomenon may be because the older people are, the worse their blood vessels are, and the aneurysm is more likely to rupture. About 85% of SAH originates from aneurysm rupture, which may cause the incidence of SAH to increase with age [16, 17]. When gender factors are taken into account, studies have shown that the incidence rate for Japanese women is 22.9/100,000 person-years (95% CI, 15.7–33.5), and for men it is 19.5 (95% CI, 14.2–26.8), with a relative risk of 1.3 for women (95% CI, 0.8–2.1), which is consistent with our findings that the incidence rate of SAH in Japanese women is higher than that in men, especially in middle-aged and elderly women [13]. Gender is also a risk factor for aneurysm formation and rupture. Women have a much higher risk of new aneurysm formation, and the decline in estrogen levels after menopause may also lead to an increased risk of aneurysm formation in older women. In addition, activation of various estrogen subtypes and receptors can affect the formation and rupture of intracranial aneurysms in mice [18, 19]. A combination of many complex factors may contribute to the higher incidence of SAH in Japanese women.
In this study, we also predicted the age-standardized incidence rates of SAH in the world, China, and Japan by 2030. Unlike the continued decline in the age-standardized incidence rates of SAH worldwide, the age-standardized incidence rates of SAH in China and Japan continued to rise. This may be attributed to the population structure of China and Japan by 2030 (Figure S6 B). The aging population will lead to a further increase in the number of hypertensive patients, which has been confirmed in related studies in Japan [15]. Moreover, studies have reported that the prevalence of hypertension, average systolic blood pressure, and pulse pressure among the elderly in China increased significantly from 2008 to 2018 [20]. In addition, although China’s smoking rate has declined, it is worth noting that the use of e-cigarettes in China has increased in recent years. The toxic components of e-cigarettes also have adverse effects on endothelial function and cardiovascular disease [21]. In 2030, the incidence rate increase among men in China was slightly higher than that among women, while the incidence rate increase among women in Japan was 2.96 times that of men (16.19% vs. 5.47%). From the observation of Japan’s population structure in 2030, we found that the number of elderly women in Japan is significantly higher than that of men of the same age (Figure S6 B). The elderly, women and Japanese women over 75 years old have a higher proportion of hypertension, which may be the potential reasons for the prediction results in this study that the incidence of SAH in Japanese women in 2030 will be higher than that of men [15–19].
In conclusion, despite the significant decline in the incidence of SAH globally, the burden of SAH is likely to continue to increase in the absence of interventions for risk factors, with a particularly severe impact on middle- and high-income countries, such as China and Japan, which are the focus of this study. Hypertension and smoking are major risk factors for SAH [1, 13]. Studies have found that for every 1 mmHg decrease in systolic blood pressure, the overall age-adjusted and sex-adjusted incidence of SAH decreased by 7.1% (95% CI, 5.8–8.4). For every 1% point decrease in smoking rate, the age-adjusted and sex-adjusted overall incidence of SAH decreased by 2.4% (95% CI, 1.6–3.3) [13]. Therefore, primary prevention targeting the major risk factors for SAH, such as reducing the prevalence of hypertension by reducing salt intake and obesity rates, and controlling smoking prevalence through comprehensive legislation, may contribute to reducing the burden of SAH [21–23]. In addition to the major risk factors for SAH, other risk factors such as demographic structure, air pollution, lead exposure, and hyperglycemia also need to be intervened with efforts from governmental departments [11].
Previous studies have always categorized SAH as a small category of stroke and have not specifically focused on SAH as a disease. The present study is, to our knowledge, one of the very few studies that focuses solely on the disease burden of SAH. In addition, we innovatively compare and discuss the potential reasons for the large gap in SAH incidence between China and Japan. Despite the efforts made in this study, the following limitations still need to be considered. First, the GBD database is limited by the quality of disease registries in each country/area. Lower-income countries/areas may have missing data on the burden of disease compared to higher-income countries/areas, resulting in inaccurate data. This could lead to an underestimation of the burden of disease. Second, this study assessed the trend of SAH and predicted the disease burden of SAH based on the GBD 2019 database, but the prediction results may not be accurate enough due to the lagging information in this database. Third, economic development does not fully explain differences across countries/regions. Fourth, there are many factors that affect the disease burden of SAH, such as hypertension, smoking, BMI, hyperglycemia, etc., and in this study, we focused only on the major factors: hypertension and smoking. Finally, the combined effects of multiple risk factors for SAH are unknown and require further study. Despite these limitations, our results are generally consistent with previous studies related to SAH disease burden, thus supporting the validity of our results.
Conclusion
In summary, SAH remains a disease of high global concern, with significant variations between regions and countries. Although the global incidence of SAH declined from 1990 to 2019, it has increased in certain countries with economic development and ageing demographics. In this study we focused on identifying a large difference in SAH incidence rates between China and Japan during 1990–2019, with a Chinese incidence rate EAPC of -2.61 (95% CI, -3–2.22) and an AAPC of -1.71 (95% CI, -1.76–1.64). In Japan, the EAPC was 2.89 (95% CI, 2.43–3.36) and the AAPC was 2.01 (95% CI, 1.96–2.06). However, from the results of SAH incidence rate prediction, the increase of SAH incidence rate in China in the next ten years is 7.92% for male and 7.76% for female. In Japan, the increase of SAH incidence rate in the next ten years is 5.47% in male and 16.19% in female. Contributing to the change in prevalence in China and Japan may be hypertension, smoking, and ageing demographics brought about by economic development. Regions and countries should develop effective interventions and strategies to prevent the rise in SAH incidence based on local conditions.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank the reviewers for their guidance.
Author contributions
P.D and C.X desigened the study and P.D, C.X and Y.G analyzed the data and P.D and C.H provied discussion and P.D, Z.Z and W.L wrote and revised the manuscript. All authors reviewed the manuscript.
Funding
This work was supported by a Special Fund of Drum Tower Hospital Clinical Research, Nanjing, China (2022-LCYJ-PY-38 for Wei Li, and 2022-LCYJ-MS-37 for Chun-Hua Hang).
Data availability
The datasets generated during the current study are available in the Global Health Data Exchange query tool (https://ghdx.healthdata.org/gbd-results-tool).
Declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Peng-Fei Ding, Chen-Jie Xing and Yong-Yue Gao contributed equally to this work.
Contributor Information
Chun-Hua Hang, Email: hang_neurosurgery@163.com.
Zong Zhuang, Email: zhuangzong@126.com.
Wei Li, Email: wei.li@nju.edu.cn.
References
- 1.Claassen J, Park S. Spontaneous subarachnoid haemorrhage. Lancet. 2022;400:846–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feigin VL, Stark BA, Johnson CO, Roth GA, Bisignano C, Abady GG, Abbasifard M, Abbasi-Kangevari M, Abd-Allah F, Abedi V, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet Neurol. 2021;20:795–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Global burden. Of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396:1204–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li C, Fu Y, Liu S, Yu H, Yang X, Zhang M, Liu L. The global incidence and disability of eye injury: an analysis from the Global Burden of Disease Study 2019. EClinicalMedicine 2023, 62:102134. [DOI] [PMC free article] [PubMed]
- 5.Zhang T, Yin X, Chen H, Li Y, Chen J, Yang X. Global magnitude and temporal trends of idiopathic developmental intellectual disability attributable to lead exposure from 1990 to 2019: results from global burden of Disease Study. Sci Total Environ. 2022;834:155366. [DOI] [PubMed] [Google Scholar]
- 6.Chen J, Chen H, Zhang T, Yin X, Man J, Yang X, Lu M. Burden of pancreatic cancer along with attributable risk factors in China from 1990 to 2019, and projections until 2030. Pancreatology. 2022;22:608–18. [DOI] [PubMed] [Google Scholar]
- 7.Xu Q, Zhang T, Xia T, Jin B, Chen H, Yang X. Epidemiological trends of kidney Cancer along with attributable risk factors in China from 1990 to 2019 and its projections until 2030: an analysis of the global burden of Disease Study 2019. Clin Epidemiol. 2023;15:421–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kong X, Tao X, Li L, Zhao X, Ren J, Yang S, Chen X, Xiang H, Wu G, Li Y, Dong D. Global trends and partial forecast of adverse effects of medical treatment from 1990 to 2019: an epidemiological analysis based on the global burden of disease study 2019. BMC Public Health. 2024;24:295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jiang W, Li X, Wang R, Du Y, Zhou W. Cross-country health inequalities of four common nutritional deficiencies among children, 1990 to 2019: data from the global burden of Disease Study 2019. BMC Public Health. 2024;24:486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hu W, Fang L, Zhang H, Ni R, Pan G. Global disease burden of COPD from 1990 to 2019 and prediction of future disease burden trend in China. Public Health. 2022;208:89–97. [DOI] [PubMed] [Google Scholar]
- 11.Global regional. National burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet Neurol. 2021;20:795–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Owolabi MO, Sarfo F, Akinyemi R, Gebregziabher M, Akpa O, Akpalu A, Wahab K, Obiako R, Owolabi L, Ovbiagele B. Dominant modifiable risk factors for stroke in Ghana and Nigeria (SIREN): a case-control study. Lancet Glob Health. 2018;6:e436–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Etminan N, Chang HS, Hackenberg K, de Rooij NK, Vergouwen MDI, Rinkel GJE, Algra A. Worldwide Incidence of Aneurysmal Subarachnoid Hemorrhage according to Region, Time Period, blood pressure, and Smoking Prevalence in the Population: a systematic review and Meta-analysis. JAMA Neurol. 2019;76:588–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tanaka H, Mackenbach JP, Kobayashi Y. Widening socioeconomic inequalities in smoking in Japan, 2001–2016. J Epidemiol. 2021;31:369–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, Horio T, Hoshide S, Ikeda S, Ishimitsu T, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481. [DOI] [PubMed] [Google Scholar]
- 16.Li S, Zhang J, Li N, Wang D, Zhao X. Predictive nomogram models for unfavorable prognosis after aneurysmal subarachnoid hemorrhage: analysis from a prospective, observational cohort in China. CNS Neurosci Ther. 2023;29:3567–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Macdonald RL, Schweizer TA. Spontaneous subarachnoid haemorrhage. Lancet. 2017;389:655–66. [DOI] [PubMed] [Google Scholar]
- 18.Hu S, Yu N, Li Y, Hao Z, Liu Z, Li MH. A Meta-analysis of risk factors for the formation of de novo intracranial aneurysms. Neurosurgery. 2019;85:454–65. [DOI] [PubMed] [Google Scholar]
- 19.Fuentes AM, Stone McGuire L, Amin-Hanjani S. Sex differences in cerebral aneurysms and subarachnoid hemorrhage. Stroke. 2022;53:624–33. [DOI] [PubMed] [Google Scholar]
- 20.Tan S, Liu D, Zhang Y, Li S, Zhang K, Zuo H. Trends in blood pressure and hypertension among older adults and oldest-old individuals in China between 2008–2018. Hypertens Res. 2023;46:1145–56. [DOI] [PubMed] [Google Scholar]
- 21.Xi B, Magnussen CG. Smoking control in China: a need for comprehensive national legislation. PLoS Med. 2022;19:e1004065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mozaffarian D, Fahimi S, Singh GM, Micha R, Khatibzadeh S, Engell RE, Lim S, Danaei G, Ezzati M, Powles J. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371:624–34. [DOI] [PubMed] [Google Scholar]
- 23.Nagai M, Ohkubo T, Murakami Y, Takashima N, Kadota A, Miyagawa N, Saito Y, Nishi N, Okuda N, Kiyohara Y, et al. Secular trends of the impact of overweight and obesity on hypertension in Japan, 1980–2010. Hypertens Res. 2015;38:790–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during the current study are available in the Global Health Data Exchange query tool (https://ghdx.healthdata.org/gbd-results-tool).