Abstract
Objective
This study created and evaluated the face validity of a novel, low-cost, three-dimensional printed pediatric laparoscopic trainer and compared it to a standard laparoscopic trainer (LT).
Design
We developed the Space Child Laparoscopic Trainer (SCLT) using fused deposition modeling technology with a Bambulab P1S 3D printer.
The cost per unit was five euros and the assembly time was 10 min. The printing time was 543 min for 434 g of polylactic acid filament (PLA). A smartphone was used as the camera.
The performance of experienced surgeons and surgical residents was evaluated on SCLT and LT using the Objective Structured Assessment of Technical Skill score (OSATS) and time spent. Two fundamental laparoscopic tasks, peg transfer and precision cutting, were randomly performed by each trainer. Participant satisfaction was assessed using a questionnaire. This study assessed the learning speed of surgical residents using the SCLT compared to a standard LT through a non-inferiority test. The test results were compared with those of a control group of experienced senior surgeons.
Setting
A medical training program was set up for first-year surgery residents from different French cities (Rouen, Caen, Amiens, and Lille) at the Medical Training Center of Rouen, in collaboration with the University Hospital of Rouen.
Participants
Ten pediatric surgeons with at least ten years of experience in laparoscopic surgery, 51 first-year surgical residents, and six external evaluators with at least five years of laparoscopic experience.
Results
In total, 200 exercises were performed by 50 residents. The estimated learning speed was +0.139 (95 % confidence interval [CI]: +0.053–+0.252, p = 0.01) for LT and +0.153 (95%CI: +0.035–+0.243, p = 0.004) for SCLT. The estimated learning speed ratio for the SCLT compared to that for the LT was 1.10 (95%CI: 0.35–3.46, p = 0.09 for non-inferiority to 0.50).
Conclusions
The results demonstrated a similar performance between the SCLT and standard LT for resident training in pediatric surgery. The widespread dissemination of this tool to residents and surgeons, especially in developing countries, may allow easier access to laparoscopic training.
Keywords: 3D-printing, Low-fidelity laparoscopic trainer, Education, Surgical resident
Abbreviations:
- 3D
three-dimensional
- CI
confidence interval
- FLS
Fundamentals of Laparoscopic Surgery
- LT
laparoscopic trainer
- OSATS
Objective Structured Assessment of Technical Skill score
- PLA
polylactic acid filament
- SCLT
Space Child Laparoscopic Trainer
- TPU
thermoplastic polyurethane
1. Introduction
Laparoscopy training is an essential component of residency training in pediatric surgery and other surgical specialties [1]. This training is mandatory for pediatric and general surgical residents in France. Laparoscopic training consists of practicing surgical procedures related to the digestive, urological, and gynecological systems using a simulator [2]. Constant practice of these operations requires the regular repetition of fundamental procedures using standard laparoscopic trainers (LTs) [3]. This necessitates easy access to laparoscopic simulators. However, laparoscopic simulators are less accessible due to high costs ranging between 69 and 1100 euros [4]. Furthermore, these simulators are often located in simulation centers, which are typically far from the hospital departments where students reside. In addition, simulators specifically designed for pediatric applications are rare.
Current solutions include a three-dimensional (3D)-printed laparoscopic trainer model with >20 components, which is only compatible with an iPad [5]. Other existing low-cost laparoscopic trainers do not meet current standards and do not account for the limitations associated with reduced working space such as children's abdomen [6]. The present study proposes a low-cost laparoscopic trainer readily available to all students irrespective of socioeconomic challenges: the Space Child Laparoscopic Trainer (SCLT). The SCLT was developed using 3D printing technology, which enables the easy reproduction of medical devices. Over the past decade, 3D printers have gained popularity in hospitals for the creation of low-fidelity implants and devices [7].
The primary objective of the SCLT is to replicate the volume of the abdominal cavity of a six-year-old child [8] to provide a realistic training environment for surgeons. The second objective was easy reproducibility using additive manufacturing. To meet these criteria, the SCLT was developed and optimized for easy reproducibility at home, with minimal components. The SCLT kit was adapted with smartphones to film the exercises, and multiple trocar sites were incorporated to simulate various procedures, including appendectomy and cholecystectomy.
Our Hypotheses is that the SCLT is an inexpensive laparoscopic simulator that offers sufficient performance to effectively train novice surgeons. Its high accessibility allows trainees to engage in significantly longer training durations, compared to the limited access typically available at simulation centers. We hypothesize that this extended training time will ultimately enhance the experience level of young surgeons when they begin operating on real patients, despite the SCLT potentially having lower performance compared to the most advanced laparoscopic trainers. Given that the SCLT provides significantly greater accessibility (allowing for home training rather than training limited to medical centers) we hypothesize that the increased training duration (potentially more than double) could compensate for any potential reduction in learning speed compared to the standard LT. Therefore, demonstrating that the SCLT's learning speed is not inferior by than 50 % compared to the LT supports its utility in surgical training programs.
The primary goal of this study is to assess the learning speed of surgical residents using the SCLT compared to a standard LT through a non-inferiority test. The test results were compared with those of a control group of experienced senior surgeons.
2. Material and methods
2.1. Model design
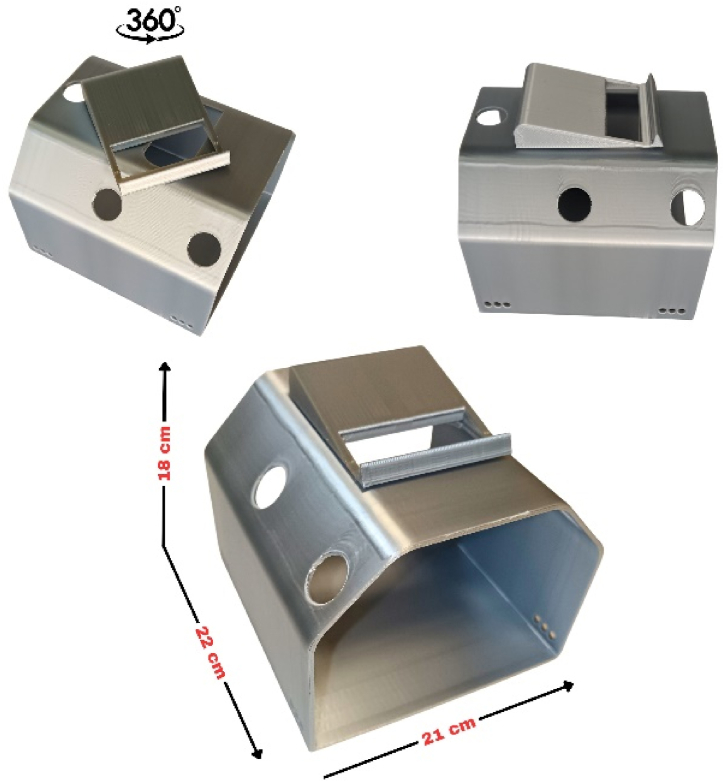
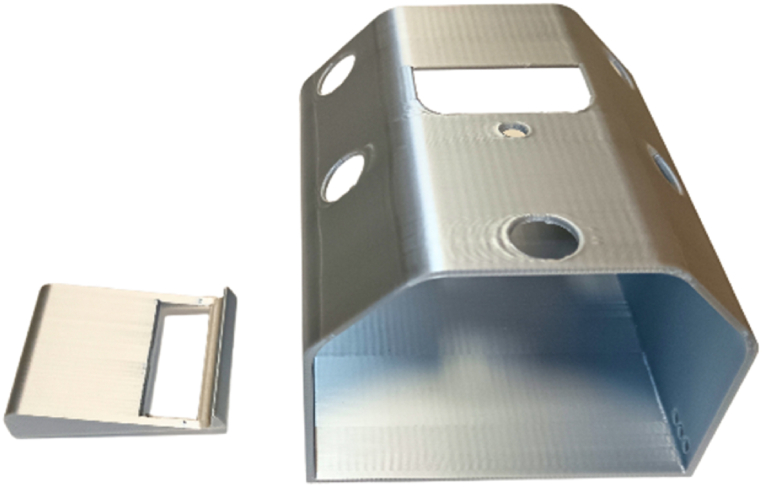
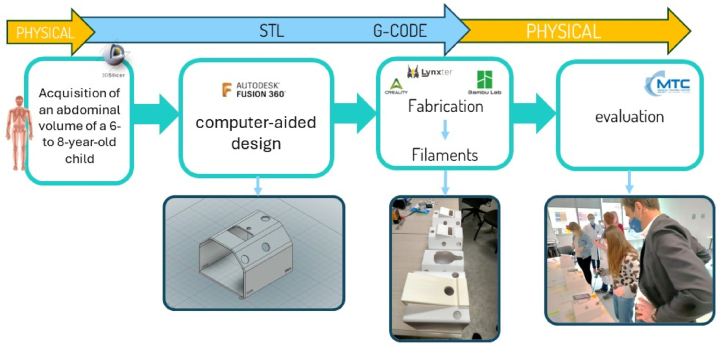
The SCLT is a low-cost, portable, and ergonomic laparoscopic device (Fig. 1, Fig. 2, Fig. 3). The SCLT utilized in this study is a model specifically designed and developed in-house by our team. The design was created using computer-aided design software (Fusion 360 Autodesk®) and printed using filament deposition technology, which is currently the least expensive option available [9]. Both parts of the SCLT are made of polylactic acid (PLA), derived from corn starch, making them biodegradable (Fig. 4). Thermoplastic polyurethane (TPU) trocars can be added to the SCLT to facilitate grasper insertion. Laparoscopic optics are provided by a smartphone, and all conventional laparoscopic instruments can be used with the SCLT. The cost of producing one SCLT unit is €5 and it takes 10 min to assemble. The SCLT has been designed to be printable without print support, which makes printing easier, saves printing time, and reduces the quantity of PLA required to produce the SCLT.
Fig. 1.
Full assembled SCLT with the rotational base and dimension size.
Fig. 2.
Full assembled SCLT with instruments and Smartphone.
Fig. 3.
3D printed components with the base (left) and the body (right).
Fig. 4.
Flow-chart.
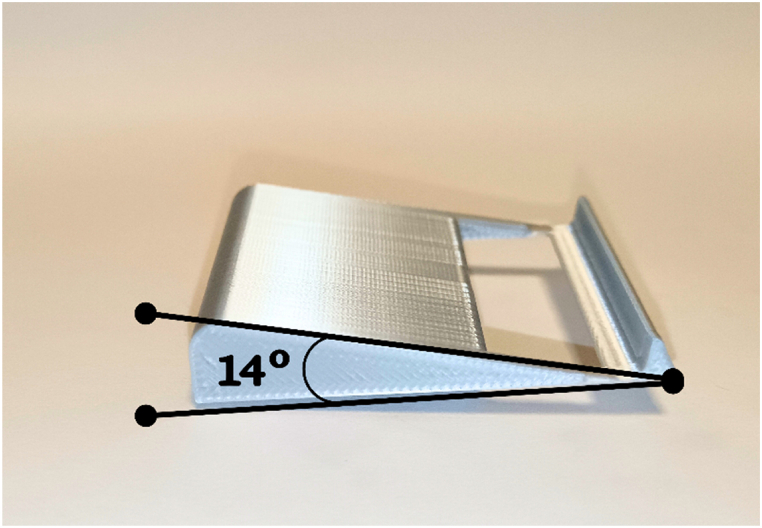
The SCLT can be printed in two parts: the body and the base. The base is designed to fit all phones and can be rotated around a fixed axis. After conducting several tests, we determined that the optimal inclination angle for the phone base is 14° (Fig. 5). This provides improved viewing ergonomics and optimal vision for the trainer. No specific app is required for this setup; users simply need to open the camera on their phone and activate the flash to illuminate the inside of the laparotrainer.”
Fig. 5.
The base with the 14° angle.
The SCLT is a simulation of the abdomen of a six-year-old child, measuring 18 cm in height, 22 cm in length, and 21 cm in width, with a volume of 5.67 L. It has seven trocar ports that can simulate different types of surgeries, including appendectomy and cholecystectomy.
2.2. Cost and feasibility
The SCLT model was designed with cost-effectiveness and accessibility in mind. It utilizes approximately 450 g of polylactic acid (PLA), which is the most commonly used polymer in 3D printing due to its biodegradability and ease of use. The cost of PLA ranges between 10 and 20 euros per kilogram, depending on the manufacturer. Consequently, the material cost of producing the SCLT is less than 5 euros.
Fabrication of the SCLT is achieved using Fused Deposition Modeling (FDM) 3D printing technology. FDM printers are the most accessible, widely available, and affordable type of 3D printers, typically costing less than 500 euros. These printers are suitable for use at home, in simulation centers, hospital departments, and educational institutions. The widespread availability and ease of use of FDM printers facilitate the replication of the SCLT model in various settings without the need for specialized equipment.
We tested printing on Creality Cr-6 SE, Lynxter S600D, and Mingda Magician Pro systems, all with the same printing capabilities.
2.3. Assessing performance and satisfaction
This study evaluated two groups with different levels of experience; namely, 51 first-year surgical residents and 10 surgeons with experience in pediatric surgeries. The participants were from various French cities, including Caen, Lille, Amiens, and Rouen. The residents were in their first year of training in either pediatric or adult surgery.
This study evaluated the performance by calculating an Objective Structured Assessment of Technical Skills (OSATS) score [10] for two fundamental laparoscopic skill tasks: peg transfer and precision cutting. The evaluation was conducted by six external evaluators, each with at least five years of laparoscopic experience. To be considered successful, each task had to be completed within 7 min.
Each resident and expert was assessed using both a standard LT and the SCLT, in random order. The order of passage for each LT was recorded.
All participants attending the training day were included in the study, with none declining to participate. Data were collected by two independent evaluators present during the event, who were not otherwise involved in the study. Each resident and senior surgeon was evaluated once per exercise on each laparotrainer, resulting in two exercises assessed on the SCLT and two on the standard LT. A pseudo-randomization was implemented in the assignment to the LT or SCLT based on the availability of the two stations, aiming to alternate the conditions whenever possible.
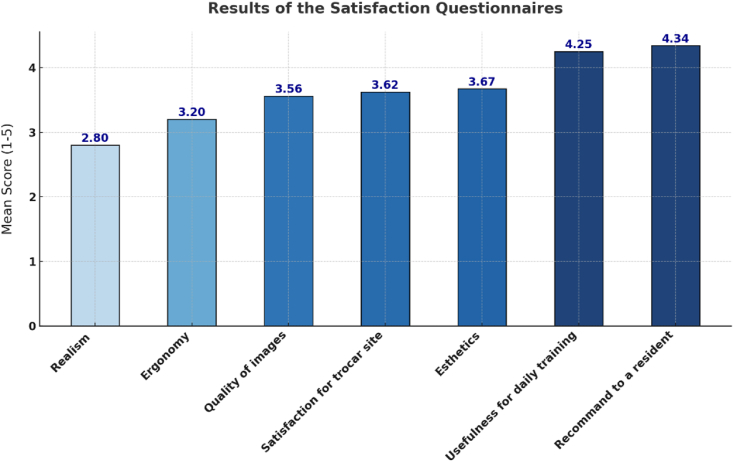
In addition to the OSATS score, the participants were asked to complete a seven-question satisfaction questionnaire on the quality of the SCLT, including image quality, realism, ergonomics, and usefulness. Finally, the participants were asked whether they would recommend the SCLT to their colleagues.
2.4. Participants and settings
All assessments were conducted at the Medical Training Center in Rouen, France, during a national training day that brought together surgical residents from Caen, Rouen, Amiens, and Lille. The participant cohort included first-year surgical residents as well as seven pediatric surgery residents. Additionally, ten senior pediatric surgeons from Rouen, Caen, Amiens, and Lille, each with at least 5 years of experience in laparoscopy, participated in the study.
In the context of surgical training in France, residents choose their surgical specialty at the end of their sixth year of medical school. Since 2017, the general surgery residency program has been discontinued, requiring residents to select their specific surgical field at the beginning of their residency.
2.5. Statistical analysis
The primary statistical analysis was non-inferiority analysis. The objective of this study was to demonstrate that the learning speed with the SCLT was not slower than that with the standard LT.
Global performance was calculated by averaging the OSATS scores for each of the four exercises. The learning speed was defined as the progress between two successive exercises, expressed in score points per exercise. Non-inferiority of the SCLT laparotrainer compared to the LT laparotrainer was defined by a ratio of learning speeds ≥0.50 between SCLT and LT. Non-inferiority was tested using a one-sided Wald's test on log-transformed learning speeds. The learning speeds of the LT and SCLT laparotrainers were simultaneously assessed in a linear mixed-effects model with random effects for the cumulative number of LT exercises performed by the resident, cumulative number of SCLT exercises performed, and type of exercise (compress or TP).
All other statistical tests were two-tailed and conducted at a 5 % significance level without correction for multiple testing.
Statistical analyses were performed using R software version 4.1.
3. Results
3.1. Participants
Fifty-one residents (32 women and 19 men) and 10 senior surgeons (four women and six men) participated in the SCLT evaluation. Among the residents, 49 (96 %) were <30 years of age, 14 (27.4 %) played video games, and 18 (35.3 %) performed laparoscopies at least once a month. Among the experts, eight (80 %) were >30 years old, two (20 %) played video games, and eight (80 %) performed laparoscopies at least once a month.
The mobile phone brands used during the study were as follows: 42 (68.8 %) Iphones, 7 (11.5 %) Samsung, and six (9.8 %) Huawei/Oppo. Nine participants (14.8 %) reported having access to a 3D printer.
3.2. Main results
A total of 200 exercises were performed by the 50 residents. Each of the ten senior surgeons performed a total of four exercises, two on the SCLT and two on the standard LT. This resulted in a total of 40 evaluations collected for the senior surgeons. The 10 experts were excluded because they expected an almost immediate learning speed. One participant was excluded because the order of the exercise performance was unknown. The estimated learning speed was +0.139 (95 % confidence interval [CI]: +0.053–+0.252, p = 0.01) for the LT and +0.153 (95 % CI: 0.035–0.243, p = 0.004) for the SCLT. The estimated learning speed ratio for the SCLT compared with the LT was 1.10 (95%CI: 0.35–3.46, p = 0.09 for non-inferiority to 0.50).
3.3. Secondary results
Table 1, Table 2, Table 3 present the OSATS scores obtained by residents and expert surgeons for the peg transfer and precision cutting exercises, respectively. Each participant performed each exercise once on the SCLT and once on the standard LT, resulting in four exercises per participant (two exercises on each trainer). For the residents, this amounted to a total of 200 exercises performed (50 residents × 4 exercises each), and for the expert surgeons, a total of 40 exercises (10 surgeons × 4 exercises each).
Table 1.
Results of surgical residents.
| Peg transfer | |||
|---|---|---|---|
| SCLT (n = 50) | LT (n = 50) | P value | |
| Failure | 5 | 3 | |
| Mean OSATS score (Maximum score = 25) | 17.9 | 18.5 | 0.80 |
| Mean Time (seconds) | 188 | 183 | 0.77 |
| Precision cutting | |||
| SCLT (n = 50) | LT (n = 50) | P value | |
| Failure | 29 | 19 | |
| Mean OSATS score (Maximum score = 25) | 16.21 | 17.05 | 0.2 |
| Mean Time (seconds) | 330 | 338 | 0.57 |
LT: laparoscopic trainer, OSATS: Objective Structured Assessment of technical skills, SCLT: Space Child Laparoscopic Trainer.
Table 2.
Results of experienced surgeons.
| Peg transfer | |||
|---|---|---|---|
| SCLT (n = 10) | LT (n = 10) | P value | |
| Failure | 1 | 0 | |
| Mean OSATS score (Maximum score = 25) | 23.2 | 24.3 | 0.211 |
| Mean Time (seconds) | 167.2 | 94.6 | 0.08 |
| Precision cutting | |||
| SCLT (n = 10) | LT (n = 10) | P value | |
| Failure | 1 | 0 | |
| Mean OSATS score (Maximum score = 25) | 21.6 | 23 | 0.09 |
| Mean Time (seconds) | 266 | 290 | 0.824 |
LT: laparoscopic trainer, OSATS: Objective Structured Assessment of technical skills, SCLT: Space Child Laparoscopic Trainer.
Table 3.
Results of experienced surgeons and surgical residents.
| Experienced surgeons (N = 10) | Surgical residents (N = 50) | P value | ||
|---|---|---|---|---|
| Peg transfer SCLT | OSATS score | 23.2 | 17.9 | <0.05 |
| Mean time | 167.2 | 188 | 0.05 | |
| Precision cutting SCLT | OSATS score | 21.6 | 17.2 | <0.05 |
| Mean time | 266 | 330 | 0.22 |
OSATS: Objective Structured Assessment of technical skills, SCLT: Space Child Laparoscopic Trainer.
In Table 1, Table 2, the values presented are the average scores of these exercises for both residents and expert surgeons on each device (SCLT and LT). The averages are calculated based on all individual exercise performances by the participants on each trainer. Similarly, Table 3 provides the average values for each exercise type (either on the SCLT or the LT) for both residents and expert surgeons.
No significant differences were found in the results obtained between the LT and the SCLT in either group, indicating comparable performance across both devices.
However, in the expert group, the duration of the peg transfer tended to be longer in the SCLT group than in the LT group, and the OSATS score for precision cutting tended to be lower in the SCLT group, although the difference was not significant.
The comparison of the performance of the two groups on the SCLT showed that the expert group performed significantly better on both exercises (Table 3).
3.4. Satisfaction questionnaire
Fig. 6 summarizes the detailed results of the satisfaction questionnaire. Overall, the residents expressed high satisfaction with the SCLT, with 43 participants indicating that they would recommend it to their colleagues. The questionnaire responses highlighted the suitability of the SCLT for daily laparoscopic training but also identified a weakness in its lack of realism.
Fig. 6.
Satisfaction questionnaire.
4. Discussion
This study introduces the SCLT, a novel 3D-printed LT that approximates the abdominal size of a six-year-old child. The SCLT was tested by more than 50 surgical residents who performed basic tasks using the low-cost training model. The results indicated that the performance of the residents on the SCLT was equivalent to that of traditional LTs. Among the 51 residents, the failure rate and task completion times were similar between the SCLT and standard LT. This implies that the low-cost laparoscopic trainer can be used as a substitute for a standard LT for laparoscopic training. This study demonstrated a significant learning speed with the SCLT, which was comparable for both LTs.
The learning speed analysis was based on the average progression of OSATS scores. This provided a detailed understanding of the impact of the training. Moreover, the use of OSATS scores allows for an objective evaluation of technical skill. We selected this methodology for two reasons. First, the study acknowledged the steep learning speed experienced by first-year residents during the initial exercises, reflecting the significant skill acquisition that occurs at this stage [11]. The analysis focused on a homogeneous group of residents with similar levels of experience to ensure data consistency. Experts were excluded from the analysis because of their minimal progress, which would not have contributed significantly to the results.
In comparing the SCLT to existing models [5], our device stands out for its affordability and innovation. At just 5 euros, the SCLT is significantly less expensive than the previously published laparoscopic trainers, which can cost around 20 dollars. Unlike these models that often require extra parts, our trainer is fully 3D-printed, simplifying its assembly and reducing costs. Moreover, the SCLT is designed for use with a smartphone, making it more accessible than trainers requiring an iPad. This feature, along with its pediatric scale and closed design, not only makes it more realistic for users but also highlights the SCLT's adaptability and potential for enhancing surgical training in a cost-effective manner.
The SCLT has several limitations. One of the main drawbacks of this model is that it does not accurately represent the working space available for pediatric laparoscopy. The internal space of the model corresponds to that of a six-year-old child's abdomen, which is already quite large compared with that of a newborn. This is problematic for pediatric surgeons who must operate on newborns' abdomens [13]. However, the SCLT is a step towards pediatric practices as the working area is smaller than that of a standard LT. Nonetheless, the SCLT is an ideal tool for adult surgical trainees who wish to perform surgeries such as appendectomy and cholecystectomy on children as part of their continuity of care. Some ergonomic issues were identified based on the height of the LT, which was not suitable for all participants. Some students were inconvenienced by their inability to change the position of the trocars. In contrast, the SCLT provides optimal ergonomics for the proposed exercises, with multiple trocar ports and camera support that can be rotated 360°. The setup size was ideal for easy transportation and storage. In terms of the environmental impact, the SCLT materials are biosourced, biodegradable, and recyclable polymers with minimal footprints [14].
SCLT is a low-cost and accessible tool for surgical residents and their departments, owing to its low cost and 3D printing technology. This facilitates laparoscopic training for students, helping them to overcome the learning speed of basic procedures. The SCLT can be used regularly in departments or at home and can be produced using several models of 3D printers, including the Mingda Magician Pro and Creality CR 6-SE, as used in the present study. Both printers had short printing times of approximately 20 h, and the postprint assembly of the various parts was straightforward, requiring only approximately 10 min. Furthermore, although image quality may vary between devices, the SCLT is compatible with all smartphones. The image resolution was sufficient for performing basic gestures as provided in the Fundamentals of Laparoscopic Surgery (FLS). These advantages are important for the easy adaptability of SCLT among surgical residents, surgeons, and students in developing countries. When comparing SCLT with other low-cost LTs available in the market, the performance of the residents appears to be similar [12].
Several experts tested the SCLT on residents and performed the required tasks. The experts achieved a higher success rate than the residents for the two laparoscopy trainers, supporting the idea that both simulators are equivalent and suitable for basic skill training. The experts performed the worst on the SCLT exercises. One hypothesis for this observation was the lack of ergonomics or a constrained working area in the SCLT. Mobile phones have virtually no depth of field, which may have influenced senior surgeons who are accustomed to viewing images on wider screens connected to high-resolution cameras.
This study has several limitations. First, although the study included 51 residents and 10 senior surgeons, the sample size, particularly for the expert group, may not have been sufficient to detect small but meaningful differences. Second, all participants were recruited from a single setting during a national training day. This homogeneity may limit the generalizability of our findings to other institutions or broader populations with different training backgrounds and resource availability. Third, we did not control for prior experience with video games or the frequency of performing laparoscopic procedures, both of which could affect proficiency and learning speed. Although some participants reported playing video games or performing laparoscopies regularly, these factors were not adjusted for in our analysis, potentially confounding the results. The use of pseudo-randomization based on the availability of training stations might not have fully eliminated selection bias, which could influence the outcomes. Additionally, the non-inferiority margin of 0.50 used in our analysis, while established a priori, is somewhat arbitrary and may not correspond to a significant threshold. Lastly, the study focused on immediate performance outcomes without assessing long-term skill retention or the transferability of skills to actual surgical procedures. Future research should include longitudinal assessments to determine the lasting impact of training with the SCLT and its effectiveness in improving operative performance. In the future, the SCLT will be evaluated nationally among all first-year pediatric surgery residents, which will require regular training at home.
After receiving evaluation and feedback, the SCLT improved. The shape of the laparotrainer was rounded, and its size was reduced to better simulate a child's abdomen. Two additional trocar ports were added, and the smartphone base was enlarged to accommodate larger tablets and smartphones. Currently, new neonatal laparotrainers are being designed.
5. Conclusions
This study provided data showing that the developed low-cost 3D-printed SCLT was comparable to a standard LT for training in basic laparoscopic procedures. The SCLT is a valuable tool that can greatly benefit surgical residents, including those in developing countries. Using this trainer, residents can gain access to regular training in basic laparoscopic procedures. This is particularly important in regions where resources and opportunities for surgical training may be limited. A key advantage of the SCLT is that it provides a working environment that closely mimics a pediatric environment.
These preliminary results require confirmation in larger studies. Assessments of the effectiveness of daily home-based SCLT for learning basic laparoscopic procedures would also be valuable.
The STL of the SCLT is freely available on both the Thingiverse and Cults3D platforms.
CRediT authorship contribution statement
Alexis Lubet: Writing – original draft, Visualization, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Mariette Renaux-Petel: Writing – review & editing, Supervision, Project administration, Methodology, Formal analysis, Data curation, Conceptualization. Jean-Baptiste Marret: Visualization, Validation, Investigation, Data curation. Julien Rod: Validation, Supervision, Investigation, Data curation. Louis Sibert: Writing – review & editing, Supervision, Resources, Project administration, Methodology, Investigation. Laurent Delbreilh: Writing – review & editing, Supervision, Resources, Project administration, Methodology, Investigation, Conceptualization. Agnès Liard: Writing – review & editing, Validation, Supervision, Resources, Project administration, Methodology, Investigation, Funding acquisition, Data curation.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon request. Please feel free to contact us via email for any inquiries.
Ethics statement
This study was approved by the local ethics committee. All participants provided their informed consent. In accordance with French regulations, a notification was made to the French Data Protection Authority (CNIL).
Funding
This work was supported by the French Society of Pediatric Surgery (SFCP).
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Alexis LUBET reports financial support, statistical analysis, and writing assistance were provided by French Society of Pediatric surgery. Alexis LUBET reports a relationship with French Society of Pediatric Surgery that includes: funding grants. If there are other authors, they declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We thank Dr Quôc Peyrot for his support in designing the SCLT, Dr André Gillibert for his statistical analysis expertise, and Loic Avegnon for reviewing the English manuscript.
References
- 1.Zhou X., Shao Y., Wu C., et al. Application of a highly simulated and adaptable training system in the laparoscopic training course for surgical residents: experience from a high-volume teaching hospital in China. Heliyon. 2023;9 doi: 10.1016/j.heliyon.2023.e13317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Breaud J., Talon I., Fourcade L., et al. The National Pediatric Surgery Simulation Program in France: a tool to develop resident training in pediatric surgery. J. Pediatr. Surg. 2019;54:582–586. doi: 10.1016/j.jpedsurg.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 3.McCluney A.L., Vassiliou M.C., Kaneva P.A., et al. FLS simulator performance predicts intraoperative laparoscopic skill. Surg. Endosc. 2007;21:1991–1995. doi: 10.1007/s00464-007-9451-1. [DOI] [PubMed] [Google Scholar]
- 4.Li M.M., George J. A systematic review of low-cost laparoscopic simulators. Surg. Endosc. 2017;31:38–48. doi: 10.1007/s00464-016-4953-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parkhomenko E., Yoon R., Okhunov Z., et al. Multi-institutional evaluation of producing and testing a novel 3D-printed laparoscopic trainer. Urology. 2019;124:297–301. doi: 10.1016/j.urology.2018.06.034. [DOI] [PubMed] [Google Scholar]
- 6.Knowlin L.T., Laskay N.M.B., Jules N.P., Godzik J., Chang T.P., Spurrier R.G. Advances in pediatric surgery simulation-based training. Children. 2023 December 28;11:34. doi: 10.3390/children11010034. PMID: 38255348, PMCID: PMC10813955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kamio T., Onda T. Fused deposition modeling 3D printing in oral and maxillofacial surgery: problems and solutions. Cureus. 2022;14 doi: 10.7759/cureus.28906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou R., Cao H., Gao Q., et al. Abdominal wall elasticity of children during pneumoperitoneum. J. Pediatr. Surg. 2020;55:742–746. doi: 10.1016/j.jpedsurg.2019.05.025. [DOI] [PubMed] [Google Scholar]
- 9.Andronov V., Beránek L., Krůta V., Hlavůňková L., Jeníková Z. Overview and comparison of PLA filaments commercially available in Europe for FFF technology. Polymers. 2023;15:3065. doi: 10.3390/polym15143065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin J.A., Regehr G., Reznick R., et al. Objective structured assessment of technical skill (OSATS) for surgical residents. Br. J. Surg. 1997;84:273–278. doi: 10.1046/j.1365-2168.1997.02502.x. [DOI] [PubMed] [Google Scholar]
- 11.Rahimi A.M., Hardon S.F., Uluç E., Bonjer H.J., Daams F. Prediction of laparoscopic skills: objective learning speed analysis. Surg. Endosc. 2023;37:282–289. doi: 10.1007/s00464-022-09473-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hardon S.F., van Gastel L.A., Horeman T., Daams F. Assessment of technical skills based on learning speed analyses in laparoscopic surgery training. Surgery. 2021;170:831–840. doi: 10.1016/j.surg.2021.04.024. [DOI] [PubMed] [Google Scholar]
- 13.Heinrich M., Tillo N., Kirlum H.J., Till H. Comparison of different training models for laparoscopic surgery in neonates and small infants. Surg. Endosc. 2006;20:641–644. doi: 10.1007/s00464-004-2040-7. [DOI] [PubMed] [Google Scholar]
- 14.Sola A., Trinchi A. Recycling as a key enabler for sustainable additive manufacturing of polymer composites: a critical perspective on fused filament fabrication. Polymers. 2023;15:4219. doi: 10.3390/polym15214219. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon request. Please feel free to contact us via email for any inquiries.