Abstract
The coexistence of fibrous dysplasia and aneurysmal bone cyst in the craniofacial region is extremely rare. This article presents a unique case involving the skull base, diagnosed using computed tomography and magnetic resonance. Imaging revealed a characteristic expansile mass with a ground-glass appearance alongside cystic areas exhibiting fluid-fluid levels, indicative of fibrous dysplasia and aneurysmal bone cyst. Surgical resection was performed successfully, although significant intraoperative hemorrhage was encountered, leading to hypovolemic shock and cardiorespiratory arrest. This case underscores the essential role of imaging in accurate diagnosis and highlights the bleeding risks associated with surgical treatment of fibrous dysplasia with aneurysmal bone cyst. Preoperative embolization is suggested as a strategy to mitigate bleeding risk during surgery.
Keywords: Fibrous dysplasia, Aneurysmal bone cyst, Skull base, Magnetic resonance imaging, Computed tomography
Introduction
Fibrous dysplasia (FD) is an uncommon congenital anomaly. It is characterized by a localized impairment in osteoblastic maturation, which replaces the normal bone with fibrous stroma and islands of immature woven bone. FD represents approximately 7% of all benign bone tumors and can affect any bone. It can occur as a single bone lesion (monostotic) or involve multiple bones (polyostotic) [1].
Aneurysmal bone cyst (ABC) is a non-neoplastic lesion consisting of cystic cavernous spaces filled with blood and devoid of lining endothelium. Typically, ABC occurs in long bones and the spinal column in teenagers and young adults. Its presentation can be primary or associated with other skeletal abnormalities such as FD, nonossifying fibroma, or chondromyxoid fibroma [1,2].
FD alongside ABC in the craniofacial area is uncommon, with only a few cases reported in the literature [1,3]. In this article, we describe a case of FD with associated ABC in the skull base, emphasizing the imaging findings that aid in the diagnosis.
Case presentation
An 11-year-old male patient presented to a neurosurgery control appointment describing a 1-year history of a painless, petrous, bulky mass sensation in the right retro auricular region. Physical examination revealed a hard, noncompressible retro auricular mass; auditory function was reduced. A hemogram and C-reactive protein were requested, but they showed unremarkable findings. Further imaging studies were ordered to evaluate the lesion.
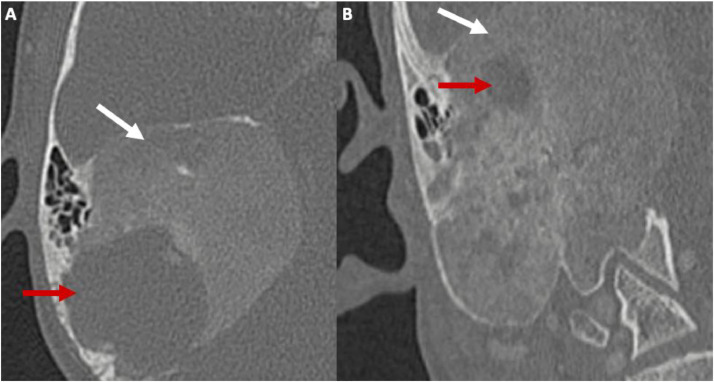
A non–contrast-enhanced computed tomography (CT) scan of the ear was performed to provide more details about the lesion. The scan showed a sizeable petromastoid mass with a ground-glass appearance and several cystic areas narrowing the external and internal auditory canals. This suggests FD coexisting with ABC as the primary differential diagnosis (Fig. 1).
Fig. 1.
Noncontrast CT scan of the ears in axial (A) and coronal (B) views showing a ground-glass appearance petromastoid expansive bony mass (white arrows) with multiple cystic areas (red arrows) measuring 60 × 50 × 40 mm, narrowing the internal and external auditory canals. The scutum, cochlea, vestibule, and semicircular canals appeared normal.
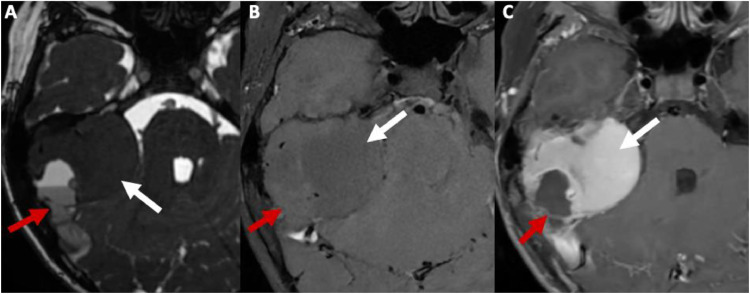
A magnetic resonance imaging (MRI) of the brain was performed to characterize the lesion further, showing that the right petromastoid mass had multiple cystic spaces with hematic content, some producing fluid-fluid levels, suggesting the presence of ABC within the FD (Fig. 2).
Fig. 2.
Brain MRI in T2 (A), T1 (B), and T1 with contrast enhancement (C). The images reveal a petromastoid mass that appears hypointense in T2 and T1 with avid contrast enhancement, indicating fibrous tissue (white arrows). Additionally, there are internal T2 and T1 hyperintense cystic areas with peripheral rim enhancement and fluid-fluid levels consistent with hematic content (red arrows). These findings collectively indicate FD with associated ABC.
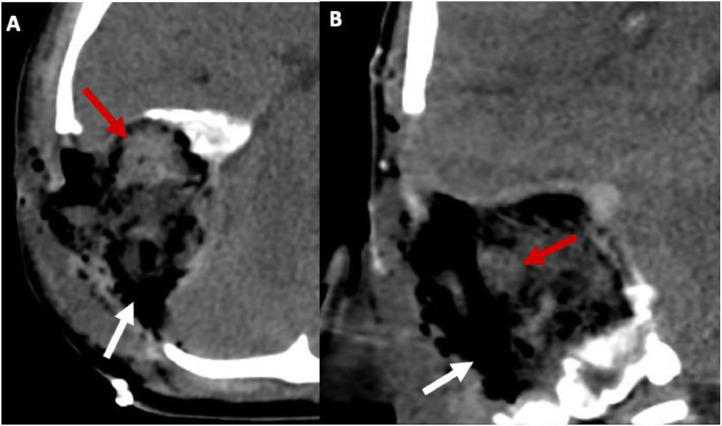
The tumor was surgically resected via a suboccipital retromastoid approach. During the procedure, a major hemorrhage occurred due to arterial bleeding from intratumoral vessels, resulting in hypovolemic shock and cardiorespiratory arrest, which required resuscitation. Tumor segments were sent to pathology, showing irregular and curvilinear bony trabeculae with a “Chinese letter” appearance, arranged on a fibrous connective tissue stroma associated with vascular proliferation, confirming the diagnosis of FD and associated ABC. A CT scan performed 1-day postsurgery showed changes consistent with the mastoidectomy (Fig. 3).
Fig. 3.
Noncontrast CT scan of the brain in axial (A) and coronal (B) views showing a right postsurgical cavity due to mastoidectomy, containing air bubbles (white arrows) and residual blood (red arrows).
Postoperatively, the patient experienced partial involvement of the right cranial nerves VII, VIII, IX, X, and XI, manifesting as conductive hearing loss, peripheral facial paresis, dysphonia, and dysphagia. After 1 year and multiple rehabilitation sessions, the patient achieved significant symptom resolution, although hearing loss persists.
Discussion
The association of FD with ABC is rare, with only 36 reported cases in the literature, of which 15 occurred in the skull base [4]. According to Rau et al., FD with concomitant ABC is diagnosed in patients with a mean age of 18.8 years, more commonly affecting men (60%) than women (40%) [4].
ABC within a pre-existing lesion such as FD may be caused by a local circulatory disturbance that causes a significant elevated venous pressure and the formation of enlarged vascular spaces within the affected bone [4]. This hemodynamic disturbance could be secondary to the pre-existing bone lesion or local trauma [4].
The symptoms of FD associated with ABC depend on the lesion's location and rate of growth [5]. In cases where the lesion involves the petromastoid region, as in our case, symptoms may include headache, ear pain, hearing loss, tinnitus, and vertigo, mainly due to extrinsic compression of adjacent structures [6].
FD is typically considered a slow-growing, painless lesion. In contrast, ABC is characterized by rapidly growing and painful lesions [4]. In cases where FD is accompanied by ABC, the usual clinical course involves a pre-existing FD that grows more quickly and becomes painful due to the emergence of the ABC; however, in our case, this presentation was not evident [4].
In CT scans, FD with associated ABC appears as a ground-glass expansive mass with multiple cystic areas within it [5]. In MRI scans, the cystic spaces can show high signal intensity on T2 and T1 sequences due to hemorrhage, and fluid-fluid levels may be observed [5,7]. When fluid-fluid levels within FD are present, sarcomatous transformation or concomitant ABC must be suspected [7].
The treatment is based on surgical resection. The surgical approach depends on the mass localization; for example, if the lesion is in the petro-mastoid region, suboccipital retromastoid approach surgery may be performed, as in our case. [8]. Some authors advocate performing preoperative embolization to reduce tumor vascularity [5].
In our case, the patient experienced intraoperative bleeding during resection, leading to hypovolemic shock and cardiorespiratory arrest, which could have been prevented by performing preoperative embolization of the tumor's vascularity.
Other adjuvant therapies being studied include radiotherapy, sclerotherapy, argon beam coagulation, and drugs like denosumab [5].
The recurrence of primary ABC ranges from 10% to 50%; however, there are no reports about the recurrence of secondary ABC [9].
Conclusions
Though rare, the coexistence of FD and ABC in the craniofacial region can be accurately diagnosed with CT and MRI. Surgical resection, despite the risk of significant intraoperative bleeding, can be successfully performed, underscoring the importance of detailed preoperative planning. Preoperative embolization may offer a valuable strategy to mitigate bleeding risks during surgery. Further research is warranted to refine treatment approaches and determine the recurrence rate of secondary ABC.
Patient consent
Informed consent was obtained from the patient.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments: None.
References
- 1.Joshi DrAR, Hosamani DrS, Kapadia DrJ. Craniofacial fibrous dysplasia with aneurysmal bone cyst: a rare coexistence. Int J Radio Diagnos Imaging. 2022;5(3):31–33. doi: 10.33545/26644436.2022.v5.i3a.273. [DOI] [Google Scholar]
- 2.Kransdorf MJ, Sweet DE. Aneurysmal bone cyst: concept, controversy, clinical presentation, and imaging. Am J Roentgenol. 1995;164(3):573–580. doi: 10.2214/ajr.164.3.7863874. [DOI] [PubMed] [Google Scholar]
- 3.Swed S, Kremesh MI, Alshareef L, Katnaji J, Abd W, Ayoub K. Secondary aneurysmal bone cyst with benign fibro-osseous lesions: case report. Ann Med Surg. 2021;72 doi: 10.1016/j.amsu.2021.103024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rau LH, Reinheimer A, Meurer MI, Marodin AL, Espezim CS, Klüppel LE, et al. Fibrous dysplasia with secondary aneurysmal bone cyst—A rare case report and literature review. Oral Maxillofac Surg. 2019;23(1):101–107. doi: 10.1007/s10006-019-00741-w. [DOI] [PubMed] [Google Scholar]
- 5.Sharma G, Sharma P, Shankar SG, Gupta R. Fibrous dysplasia with aneurysmal bone cyst presenting as sinonasal mass. Cureus. 2022;14(4):e24485. doi: 10.7759/cureus.24485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Razek AA, Huang BY. Lesions of the petrous apex: classification and findings at CT and MR imaging. RadioGraphics. 2012;32(1):151–173. doi: 10.1148/rg.321105758. [DOI] [PubMed] [Google Scholar]
- 7.Lin Wen-Chiung, Wu Hung-Ta Hondar, Wei Chao-Jung, Chang Cheng-Yen. Aneurysmal bone cyst arising from fibrous dysplasia of the frontal bone. Eur Radiol. 2004;14(5):930–932. doi: 10.1007/s00330-003-2181-4. [DOI] [PubMed] [Google Scholar]
- 8.Pasquini E, Compadretti GC, Sciarretta V, Ippolito A. Transnasal endoscopic surgery for the treatment of fibrous dysplasia of maxillary sinus associated to aneurysmal bone cyst in a 5-year-old child. Int J Pediatr Otorhinolaryngol. 2002;62(1):59–62. doi: 10.1016/S0165-5876(01)00593-6. [DOI] [PubMed] [Google Scholar]
- 9.Baek S, Kim BJ. Aneurysmal bone cyst arising from the surgically removed craniofacial fibrous dysplasia in the long-term follow-up: a case report. Arch Craniofac Surg. 2023;24(5):244–249. doi: 10.7181/acfs.2023.00255. [DOI] [PMC free article] [PubMed] [Google Scholar]