Abstract
Background
Obtaining a full understanding of the anatomical structure of the eyeball and the contents within the eye plays a crucial role in learning eye diseases. However, it can be challenging for beginners to quickly learn, memorize, and apply this anatomical knowledge. To improve the teaching of ocular anatomy and help students overcome learning difficulties in ophthalmology clerkship, Zhongshan Ophthalmic Center developed an integrated ocular anatomy course comprising three main components: 'online preview,' 'lecture,' and 'wetlab dissection'.
Methods
Fifty-five fourth-year medical students from Sun Yat-sen University were recruited for this study. The impact of the integrated course was evaluated through three in-class quizzes (T1: pre-teaching assessment, T2: post-wetlab training, and T3: end of clerkship) and assessments of students' self-confidence levels. Additionally, students' course evaluations were gathered via a questionnaire survey. Statistical analyses were conducted via ANOVA and the Kruskal–Wallis test.
Results
The integration course significantly improved the mean scores of post-teaching tests (67.08 ± 10.27 vs. 74.36 ± 12.75 vs. 78.81 ± 12.70, P < 0.0001) and the students’ self-confidence scores (P < 0.0001). Fifty-four participants were satisfied with the integrated anatomy course (79.3% strongly agreed, 18.2% more agreed). Fifty-two participants agreed (76.4% strongly agreed, 18.2% more agreed) that the course could help them better understand the anatomy of the eye.
Conclusions
This integrated ocular anatomy course can aid students in better understanding and retaining the anatomy and function of ocular structures, serving as a valuable adjunct teaching strategy that can be further applied to ophthalmology clerkship.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-024-06611-8.
Keywords: Anatomy, Integration course, Ophthalmology, Clerkship
Background
Anatomy is considered one of the cornerstones of medical curricula, and a deep understanding of anatomy is essential for safe clinical practice, particularly in the discipline of surgery [1–4]. However, studies indicate that medical students' anatomy knowledge is not well retained when they enter clerkship, resulting in difficulties in further clinical study [5–8].
In most medical schools, students complete their basic sciences curricula within the first two years and have limited exposure to anatomical knowledge during the subsequent clinical training period [9–12]. Studies conducted in dentistry and psychiatry have demonstrated the advantages of integrating basic and clinical sciences. The results of these studies have further confirmed that additional anatomical learning beyond the first year can enhance students' clinical competency [13, 14]. However, few studies have focused specifically on ophthalmology.
Thus, to improve students’ understanding of eye anatomy and increase their competency for ophthalmological clerkship, we have developed an integrated anatomy course for the fourth-year medical students in their clerkship rotation at Zhongshan Ophthalmic Center, Sun Yat-sen University. Harden’s integration ladder model was used to guide the implementation of integrated curricula and integrate clinical aspects with anatomy [15]. The aim of this study was to assess the capacity of the new anatomy curriculum to meet the established learning outcomes and to evaluate students' perceptions regarding the integrated teaching paradigms.
Methods
Study participants
Medical students in Sun Yat-sen University receive one week of clerkship training in Zhongshan Ophthalmic Center in their fourth year. The one-week ophthalmology clerkship occurs approximately 18–20 times per year, and 15–20 students are involved in each rotation [16, 17].
Fifty-five students, including 32 boys and 23 girls from four rotations in the spring semester of the 2022–2023 academic year were enrolled in this study. The students had the same medical education background and had completed theoretical courses in ophthalmology in their third year. Students in each rotation were divided into 4 mini-groups (3–5 students each). Each mini-group was assigned a wetlab teaching assistant to guarantee teaching quality.
Informed consent was obtained from all students, and the research was approved by the Institutional Review Board of Zhongshan Ophthalmic Center.
Integration course
A two-hour eye anatomy integration course, including an online preview with video, lecture and wetlab porcine eye dissection, was performed at the beginning of the ophthalmology clerkship. Each part of the course is described in detail below.
Online preview with porcine eye dissection video
We presented the students with the online preview link (http://ypgxkc.gzzoc.com/Item/193.aspx) one day before the clerkship. It provided an approximately 10-min video of the porcine eye dissection with two different methods (described in detail in Table 1), and arranged a pre-study task. Students were required to watch the video and become familiar with the operating steps of the two dissection methods. Their engagement was verified prior to the class.
Table 1.
Guidelines for Wetlab Dissection of the Porcine Eye
| Method 1 | Method 2 |
|---|---|
| 1. Observe the outside of the eye (conjunctiva, cornea, sclera, limbus, extraocular muscles, optic nerve). Then, fix the porcine eye on the cutting board with pins | 1. Observe the outside of the eye (conjunctiva, extraocular muscles, optic nerve). Then, remove the conjunctiva and extraocular muscles, and observe the cornea and sclera, limbus, the insertion of extraocular muscles, optic nerve and vessels on the surface of the eyeball |
| 2. Measure the diameter of cornea. Perform the paracentesis from the limbus into the anterior chamber and observe the leaking aqueous humor | 2. Cut the eyeball along the equator and divide it into front and back parts |
| 3. Cut the cornea along with the limbus with the last quarter preserved. Observe corneal thickness and texture, and anterior chamber angle | 3. Front part: observe the position and structure of the iris, pupil, lens, ciliary body and pars plana. Remove the lens and identify the location of zonular suspension on the ciliary body |
| 4. Identify the position and structure of the iris, pupil, and lens | 4. Back part: Observe the overall fundus, including the vitreous body, retina, optic disk, and retinal vessels |
| 5. Detach the zonular and remove the lens out. Cut the lens in half and observe its structure and texture | |
| 6. Cut the sclera at 3:00, 6:00, 9:00, and 12:00 until the equator of the eyeball. Observe the overall fundus, including the vitreous body, retina, optic disk, and retinal vessels | |
| 7. Suck out the vitreous body, feel its texture. Then, detach the retina from the ora serrata, observe its shape and texture | |
| 8. Detach the choroid from the sclera and observe its color and structure | |
| 9. The underlying sclera was exposed. Feel its texture and identify the optic disc |
Lecture and anatomical demonstrations
A one-hour review lecture on the eye anatomy was given in a teaching room near the wetlab laboratory. The lecture focused on the surface structures of the globe and intraocular contents, demonstrating the structures with 3D videos, pictures and eyeball models. In addition to normal anatomy, common abnormal signs and crucial pathophysiological knowledge were also incorporated to elucidate the clinical relevance of the anatomy. This review lecture offered students a great opportunity to review eye anatomy and integrate basic anatomical knowledge with clinical training [1].
Wetlab porcine eye dissection
Following the lecture, every two students then dissected two fresh porcine eyes together, one eye with one dissection method as listed in Table 1. Fresh porcine eyes were collected from a local slaughterhouse in the morning of the course and stored in a refrigerator at 4℃ until usage. Each student was provided with dissection tools and given 60 min to dissect. One wetlab teaching assistant was responsible for guiding 4–5 students. All animal procedures were conducted in accordance with the ethical guidelines published by the International Council for Laboratory Animal Science (ICLAS) and Directive 2010/63/EU in Europe.
The students would observe the structure of the extraocular adnexa, the eyewall structures and the intraocular contents. Furthermore, they would be guided to measure some important structural parameters, distinguish the relative position relationship, and determine the texture of the internal and external components of the eyeball. The key points in the previous lecture were emphasized again in the dissection process. Figures 1 and 2 outline the steps of wetlab dissection and the main eye structures, respectively, that students were required to identify in the porcine eye.
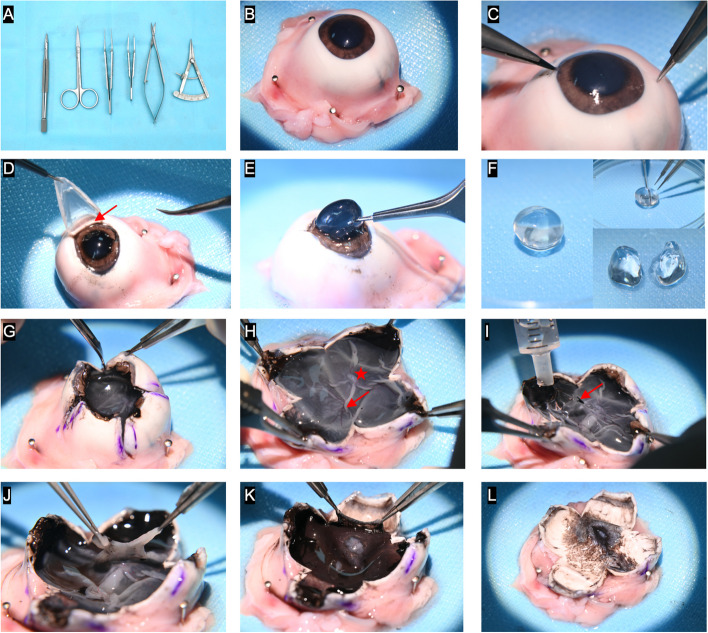
Fig. 1.
Wetlab dissection of the porcine eye- Method 1. A Dissection tools. B Fix the porcine eye onto the cutting board with pins. C Perform a paracentesis from the limbus into the anterior chamber. D Cut the cornea along with the limbus with the last quarter preserved. Observe the corneal thickness, texture and the anterior chamber angle (arrow). E Separate the lens by detaching the zonular. F. Remove the lens. Cut the lens in half and observe its structure and texture. G Cut the eyewall at 3:00, 6:00, 9:00, and 12:00 until the equator of the eyeball. H Observe the overall fundus, including the vitreous body, retina, optic disk (star), and retinal vessels (arrow). I Suck out the vitreous body and feel its texture. The arrow indicates posterior vitreous detachment. J Detach the retina from the ora serrata and observe its shape and texture. K Detach the choroid and observe its color and texture. L Expose the sclera, feel its texture and identify the optic disc
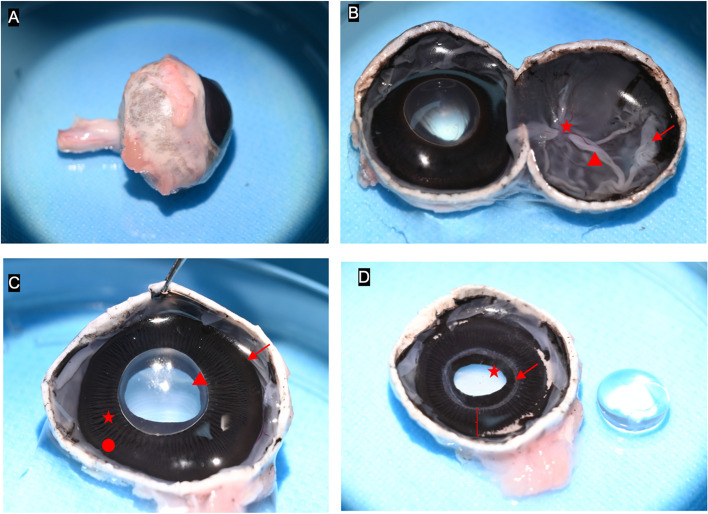
Fig. 2.
Wetlab dissection of the porcine eye- Method 2. A Observe the external structure of the eye, including the cornea and sclera, limbus, the insertion of extraocular muscles and the optic nerve. B Cut the eyeball along the equator and divide it into front and back parts. Back part: Observe the overall fundus, including the vitreous body, retina (arrow), optic disk (star), and retinal vessels (triangle). C Front part: observe the position and structure of the iris, pupil, lens (triangle), pars plicata (star), pars plana (circle) and the ora serrata (arrow). D Remove the lens, observe the iris (star) and ciliary body (parentheses), and identify the location of the zonular attachment to the ciliary body (arrow)
Assessment
This study is a self-controlled study. To evaluate the teaching effectiveness, we conducted three assessments on eye anatomy: a pre-teaching assessment (T1), and two post-teaching assessments (T2 following wetlab training, and T3 after the clerkship). Each assessment comprised 10 multiple-choice questions, designed to assess three levels of knowledge mastery: direct recall of ocular anatomy, classification and synthesis of ocular structures, and comprehension of the vital functions corresponding to these structures. Each question was awarded a score of 10 out of 100. Notably, while the questions across the three assessments were identical in content, the answer option order was varied. The students were given one minute to answer each question.
Each question was accompanied by a self-assessed confidence level score utilizing a Likert 4-point scale, widely employed in measuring opinions, attitudes, or behaviors [18, 19]. Specifically, the scale was as follows: 4 = very certain, 3 = quite certain, 2 = quite uncertain, and 1 = very uncertain [20].
A questionnaire including five dimensions (difficulty, interest, innovation, practicality, and popularity) was designed to evaluate students’ satisfaction with the anatomy course (Supplementary Table 1). In addition, open-ended questions were designed to capture students' opinions, attitudes and suggestions on this teaching modality.
Statistics
Statistical analyses were conducted with SPSS software version 22.0 (SPSS Inc., Chicago, IL, USA). Differences in T1, T2, and T3 scores were compared via ordinary one-way ANOVA test. The self-confidence scores of T1, T2 and T3 were compared via the Kruskal–Wallis test. The validity of the questionnaire was assessed via logical analysis and testing, while reliability was primarily evaluated through a re-test method. A cumulative histogram was used to analyze the results of the questionnaire. A P value < 0.05 was considered statistically significant for all tests.
Results
Pre- and post-teaching tests and self-confidence levels
The test response rate and self-confidence level evaluation were 100%. The total scores of T1, T2, and T3 were 67.08 ± 10.27, 74.36 ± 12.75, and 78.81 ± 12.70, respectively, which showed significantly difference (P < 0.0001). An analysis of the test performance of T1, T2, and T3 revealed significant differences in the texture of the eye structure (P < 0.0001), the cornea (P = 0.0155), the uvea (P < 0.0001), and the vitreous (P = 0.0173) in addition to the total score. (Table 2).
Table 2.
Comparison of test performance and self-confidence
| Test scores (mean ± SD) | P value | Self-confidence scores (Median) | P value | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T1 vs. T2 vs. T3 | T1 vs. T2 | T1 vs. T3 | T2 vs. T3 | T1 | T2 | T3 | T1 vs. T2 vs. T3 | T1 vs. T2 | T1 vs. T3 | T2 vs. T3 | |
| Total Score | 67.08 ± 10.27 | 74.36 ± 12.75 | 78.81 ± 12.70 | < 0.0001 | 0.0015 | < 0.0001 | 0.0685 | 26 | 30 | 30 | < 0.0001 | 0.0006 | < 0.0001 | 0.1391 |
| Eye structure, texture | 3.59 ± 4.84 | 8.00 ± 4.04 | 7.68 ± 4.26 | < 0.0001 | < 0.0001 | < 0.0001 | 0.6842 | 2 | 3 | 3 | < 0.0001 | < 0.0001 | < 0.0001 | 0.6526 |
| Eye structure, position | 10.00 ± 0.00 | 10.00 ± 0.00 | 10.00 ± 0.00 | NA | NA | NA | NA | 4 | 4 | 4 | 0.2115 | 0.0828 | 0.5211 | 0.2655 |
| Cornea | 5.66 ± 1.40 | 6.46 ± 1.50 | 6.34 ± 1.65 | 0.0155 | 0.0053 | 0.0227 | 0.7008 | 2 | 3 | 3 | < 0.0001 | < 0.0001 | < 0.0001 | 0.0373 |
| Uvea | 7.36 ± 2.00 | 8.85 ± 1.72 | 9.11 ± 1.49 | < 0.0001 | < 0.0001 | < 0.0001 | 0.3992 | 3 | 4 | 3 | < 0.0001 | < 0.0001 | < 0.0001 | 0.7963 |
| Ciliary body | 9.53 ± 1.77 | 9.55 ± 1.45 | 9.38 ± 1.67 | 0.8331 | 0.9561 | 0.6427 | 0.5672 | 2.5 | 3 | 3 | 0.0253 | 0.0452 | 0.0095 | 0.6061 |
| Choroid | 9.06 ± 1.89 | 9.52 ± 1.35 | 9.35 ± 1.34 | 0.2986 | 0.1488 | 0.3576 | 0.5063 | 3 | 3 | 3 | 0.0323 | 0.1083 | 0.0096 | 0.3411 |
| Retina | 3.01 ± 4.64 | 4.75 ± 4.89 | 5.00 ± 5.05 | 0.1011 | 0.4251 | 0.0353 | 0.1856 | 2 | 3 | 3 | 0.0002 | 0.0099 | < 0.0001 | 0.1173 |
| Lens | 3.96 ± 4.94 | 4.55 ± 5.03 | 4.82 ± 5.04 | 0.6603 | 0.5444 | 0.3711 | 0.7733 | 2 | 3 | 3 | 0.0002 | 0.0492 | < 0.0001 | 0.0288 |
| Aqueous humor | 6.60 ± 4.78 | 6.00 ± 4.94 | 7.86 ± 4.14 | 0.1011 | 0.5205 | 0.1458 | 0.034 | 2 | 3 | 3 | 0.0006 | 0.0301 | 0.0002 | 0.0646 |
| Vitreous | 8.30 ± 2.39 | 8.18 ± 2.43 | 9.29 ± 1.77 | 0.0173 | 0.7962 | 0.0158 | 0.0071 | 3 | 3 | 3 | 0.0121 | 0.0089 | 0.0131 | 0.7333 |
Further analysis revealed significant differences in the total scores between T1 and T2 (P = 0.0015), and between T1 and T3 (P < 0.0001), but no differences between T2 and T3 (P = 0.0685). The same trend was observed in the texture of the eye structure, the cornea and the uvea. Although there was no difference in the T1 and T2 scores of the vitreous body, there was a significant difference between T1 and T3 (P = 0.0158), or between T2 and T3 (P = 0.0071). (Table 2).
No significant differences were found in the retina and aqueous humor among the scores of T1, T2, and T3. However, test performance in both structures improved gradually, and there were significant differences in the retina between T1 and T3 (P = 0.0353), and in the aqueous humor between T2 and T3 (P = 0.034).
The overall self-confidence in understanding eye anatomy significantly improved across the three tests (P < 0.0001), with notable progress observed between T1 and T2 (P = 0.0006), and between T1 and T3 (P < 0.0001). Considerable enhancements were observed in nearly all the structures (P < 0.05), excluding the relative position relationships of the eye structures (P = 0.2115). For the relative position relationship, the students consistently demonstrated high accuracy in answering related questions throughout the three tests, approaching a perfect score of 100%. Although no significant difference was obtained in the scores of the ciliary body and lens, the students’ self-confidence in understanding the anatomy and function of these two structures improved (P < 0.05), (Table 2).
Students’ feedback questionnaire
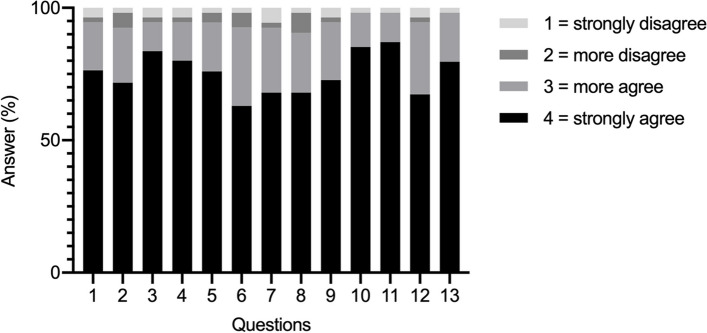
Validity and reliability of the questionnaire were ensured, and it had a high level of reliability with a total reliability coefficient of 0.951. Morever, the Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy yielded a value of 0.822, indicating strong scale validity. All respondents completed the questionnaire (Supplementary Table 1). For their satisfaction with the integrated course, 80.0% (44/55) strongly agreed and 18.2% (10/55) agreed. Moreover, 76.4% (42/55) strongly agreed that the course significantly enhanced their understanding of eye anatomy. The course effectively strengthened comprehension of three-dimensional positioning (83.6% strongly agreed), ocular structure attributes (80.0% strongly agreed), and functions (76.3% strongly agreed). The course was well-organized (72.7% strongly agreed), with instructors demonstrating prompt responsiveness (85.5% strongly agreed) and facilitating the learning process (87.3% strongly agreed) in wetlab dissections. Owing to their level of satisfaction, the participants were willing to recommend the course to other students and teaching hospitals (69.1% strongly agreed with both). (Fig. 3).
Fig. 3.
Students’ evaluation of the integrated course with a four-point scale. The scale was as follows: 1 = strongly disagree (light gray), 2 = more disagree (dark gray), 3 = more agree (gray), 4 = strongly agree (black). The X-axis represents each survey question, while the Y-axis indicates the percentage of responses for each choice
Students’ comments on the integrated course on anatomy
In the open-ended questions, the students listed several advantages of the integration course of anatomy as follows: i, It facilitated an intuitive understanding of the anatomy of the eyeball, especially its texture and tactility. ii, Theoretical lessons combined with wetlab training were highly efficient. iii, Wetlab training improved their hands-on skills. Their suggestions were focused on more porcine eyes for each student and more time for wetlab dissection. Our study has certain limitations, notably, its sample size and limited generalizability.
Discussion
In this study, we implemented an integrated ocular anatomy course within the ophthalmology clerkship, resulting in a significant improvement in the overall anatomy test score (P < 0.0001) and students' confidence in ophthalmic anatomy (P < 0.0001), with a high student satisfaction rate.
Qualified clinicians, especially surgeons, need an in-depth understanding of anatomy to perform safe clinical procedures [2, 21–26]. However, within traditional medical curricula, most medical students finish basic sciences, including anatomy lessons, in their preliminary years in medical school and have limited exposure to anatomy during clinical training [7–10, 27, 28]. There is a concern that medical students are ill-prepared in anatomy when they enter clerkships and residency programs [29, 30]. Therefore, in future clinical training, attention should continuously be given to anatomy and other basic sciences.
The method and extent of integration of basic and clinical sciences can vary widely [8, 15]. Bass, et al. [31] developed a pancreatic cancer team-based learning (TBL) module to integrate topics from abdominal anatomy, radiology, and clinical decision-making to teach abdominal anatomy. Barry, et al. [32] designed a vertical integration curriculum in the preclerkship, where students used foundational anatomy concepts in conjunction with modern imaging and diagnostic techniques to enhance important clinical concepts.
Ophthalmology clerkship requires a firm grasp of ocular anatomy. Only with a full understanding of the normal structure and function of the eye can students better understand the pathophysiology and symptomatology of ocular diseases [33–37]. However, few studies have investigated eye anatomy in ophthalmology clerkship. Our investigation comprehensively evaluated a novel integrated anatomy course for medical students’ ophthalmology clerkship.
The pre- and post-teaching test results showed that this integrated course could enhance students’ understanding of eye anatomy. The course effectively deepened participants' comprehension of the texture of the eye structure. The score of the texture question was low in T1, but was greatly improved in T2 and T3. Wetlab dissection of the porcine eye can quickly and effectively enhance students' perceptual understanding of the texture of the eye structures. The course also helped students better understand the eye’s structural composition, specifically focusing on elucidating the textural intricacies of key components such as the cornea, uvea, retina, aqueous humor and vitreous body. The acquisition of ophthalmic anatomical knowledge has a distinct learning curve, poised to facilitate the subsequent learning of ophthalmic surgical procedures, notably cataract and eyelid ptosis surgeries [38, 39].
Since the uvea is the middle layer of the eyewall, while the retina is the innermost layer, their positional relationship and functions are intricate, rendering them consistently challenging aspects for teaching ocular anatomy that students often find difficult to understand [40, 41]. Although no difference was obtained in the test scores of the questions about the ciliary and the lens, the students’ self-confidence in their understanding of these structures significantly improved. The number of multiple-choice questions, plus the corresponding scores, were appropriately increased. The integrated course allowed the students to review anatomy theory and immediately observe the structures in porcine eyes, which would be highly helpful for their understanding and memory, particularly for structures that are difficult to explain in theoretical courses.
Interestingly, for question No.3, which focused on the eye structures and their position relationships, 100% of the students answered correctly and the confidence score was high. Thus, students are proficient in layering the eyewall and their relative relationships, and it is unnecessary to spend more time on this part in the course.
The students also provided positive feedback in the questionnaire; 79.3% of them strongly agreed that they were satisfied with the integration course of anatomy, and 18.2% of them more agreed. Over 90% of the participants agreed (76.4% strongly agreed, 18.2% more agreed) that the course could help them understand the anatomy of the eye structure, which is consistent with the test results. In their clerkship in other clinical sciences, they had not previously tried such integrated courses and they suggested that such an integrated course on anatomy should be recommended to other teaching hospitals, especially surgery-related subjects. Moreover, students were willing to recommend the integrated course on anatomy to others; therefore, we believe that, compared with teaching the theory of eye anatomy in the classroom, this teaching format can effectively mobilize students' enthusiasm for learning.
The participants exhibited considerable enthusiasm for wetlab dissection and requested additional time to engage in the activity. Owing to its comparable size and anatomical structures to the adult human eye [42], the porcine eye serves as an advantageous substitute. Furthermore, fresh porcine eyes are more accessible to acquire, and porcine models have been extensively utilized in ocular anatomy training [43–47]. Students can explore small anatomical structures and feel the texture of the components that are often unrecognizable in embalmed human cadavers and have a more visual and perceptual understanding of the structures of the human eye. Therefore, the anatomical teaching effect of the fresh porcine eye is much better than that of the human eye removed from the dehydrated corpse.
Our study has limitations. This was a self-controlled study without comparison group and a small sample size. A randomized control study design would have been ideal. However, this was not possible due to logistic constraints. Future large-scale trials are necessary to corroborate our findings and strengthen the evidentiary foundation for implementing an integrated anatomy course within ophthalmology clerkship programs.
In summary, the students in this study showed significant improvements in post-teaching test scores and confidence levels as compared with those in pre-teaching test. The students’ overall satisfaction with the course was high. This course enables students to review and reinforce eye anatomy and improve their proficiency in clinical clerkships, and holds significant potential for widespread application in ophthalmology clerkship. Although the course is designed for ophthalmology clerkship, integrating anatomy or other basic sciences in clinical training can be adapted to serve other medical students and professionals.
Supplementary Information
Acknowledgements
We thank the effort of the teaching team and all of the internship tutors (Ying Yang, Jing Wu, Xue Bai, Dan Li, Chong Liu) at Zhongshan Ophthalmic Center for this study.
Authors’ contributions
LH and ZM contributed to the primary manuscript text, while XLiu, YZ and XLin assisted with data collection and analysis. ZM provided valuable insights and guidance throughout the research process. LH and ZM coordinated the study, oversaw data interpretation, and prepared the manuscript. All authors participated in reviewing and revising the manuscript for publication.
Funding
This research was supported by Teaching Quality Project of Sun Yat-sen University in 2024.
Data availability
The data and materials supporting the findings herein are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
All animal procedures were conducted in accordance with the ethical guidelines published by the International Council for Laboratory Animal Science (ICLAS) and Directive 2010/63/EU in Europe. Informed consent was obtained from all study participants. Ethical approval (2021KYPJ084) was obtained from the Institutional Review Board of Zhongshan Ophthalmic Center (IRB-ZOC-SYSU). To protect participant anonymity, no identifying information was collected.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Li Huang and Xinyu Liu contributed equally to this work.
Contributor Information
Xianchai Lin, Email: linxch7@mail.sysu.edu.cn.
Zhen Mao, Email: maozh5@mail.sysu.edu.cn.
References
- 1.Kivell TL, Doyle SK, Madden RH, Mitchell TL, Sims EL. An interactive method for teaching anatomy of the human eye for medical students in ophthalmology clinical rotations. Anat Sci Educ. 2009;2(4):173–8. [DOI] [PubMed] [Google Scholar]
- 2.Estai M, Bunt S. Best teaching practices in anatomy education: A critical review. Ann Anat. 2016;208:151–7. [DOI] [PubMed] [Google Scholar]
- 3.Fenesi B, Mackinnon C, Cheng L, Kim JA, Wainman BC. The effect of image quality, repeated study, and assessment method on anatomy learning. Anat Sci Educ. 2017;10(3):249–61. [DOI] [PubMed] [Google Scholar]
- 4.Sánchez-Ferrer ML, Grima-Murcia MD, Sánchez-Ferrer F, Hernández-Peñalver AI, Fernández-Jover E, Sánchez Del Campo F. Use of Eye Tracking as an Innovative Instructional Method in Surgical Human Anatomy. J Surg Educ. 2017;74(4):668–73. [DOI] [PubMed] [Google Scholar]
- 5.Bouwer HE, Valter K, Webb AL. Current integration of dissection in medical education in Australia and New Zealand: Challenges and successes. Anat Sci Educ. 2016;9(2):161–70. [DOI] [PubMed] [Google Scholar]
- 6.Bandiera G, Kuper A, Mylopoulos M, Whitehead C, Ruetalo M, Kulasegaram K, Woods NN. Back from basics: integration of science and practice in medical education. Med Educ. 2018;52(1):78–85. [DOI] [PubMed] [Google Scholar]
- 7.Willey JM, Lim YS, Kwiatkowski T. Modeling integration: co-teaching basic and clinical sciences medicine in the classroom. Adv Med Educ Pract. 2018;9:739–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khalil MK, Giannaris EL, Lee V, Baatar D, Richter S, Johansen KS, Mishall PL. Integration of clinical anatomical sciences in medical education: Design, development and implementation strategies. Clin Anat. 2021;34(5):785–93. [DOI] [PubMed] [Google Scholar]
- 9.Major CA, Burnham KD, Brown KA, Lambert CD, Nordeen JM, Takaki LAK. Evaluation of an online case-based learning module that integrates basic and clinical sciences. The Journal of chiropractic education. 2021;35(2):192–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van der Hoeven D, Zhu L, Busaidy K, Quock RL, Holland JN, van der Hoeven R. Integration of Basic and Clinical Sciences: Student Perceptions. Medical science educator. 2020;30(1):243–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van der Hoeven D, van der Hoeven R, Zhu L, Busaidy K, Quock RL. Integration of Basic and Clinical Sciences: Faculty Perspectives at a U.S. Dental School. Journal of dental education. 2018;82(4):349–55. [DOI] [PubMed]
- 12.Elangovan S, Venugopalan SR, Srinivasan S, Karimbux NY, Weistroffer P, Allareddy V. Integration of Basic-Clinical Sciences, PBL, CBL, and IPE in U.S. Dental Schools' Curricula and a Proposed Integrated Curriculum Model for the Future. Journal of dental education. 2016;80(3):281–90. [PubMed]
- 13.Wilkins KM, Moore D, Rohrbaugh RM, Briscoe GW. Integration of Basic and Clinical Science in the Psychiatry Clerkship. Acad Psychiatry. 2017;41(3):369–72. [DOI] [PubMed] [Google Scholar]
- 14.Walker AN, Collins BR, Topping D, Pierre K, Raviprasad AG, Nonabur V, et al. Going back to anatomy roots: Exploring the integration of anatomy sessions during clinical clerkships. Anat Sci Educ. 2024;17(9):1719–30. [DOI] [PubMed] [Google Scholar]
- 15.Harden RM. The integration ladder: a tool for curriculum planning and evaluation. Med Educ. 2000;34(7):551–7. [DOI] [PubMed] [Google Scholar]
- 16.Tang F, Chen C, Zhu Y, Zuo C, Zhong Y, Wang N, et al. Comparison between flipped classroom and lecture-based classroom in ophthalmology clerkship. Med Educ Online. 2017;22(1):1395679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang Z, Li M, Zhou Y, Ao Y, Xin W, Jia Y, et al. Modified Team-Based Learning in an Ophthalmology Clerkship in China. PLoS ONE. 2016;11(4):e0154250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fainstad T, Mann A, Suresh K, Shah P, Dieujuste N, Thurmon K, Jones CD. Effect of a Novel Online Group-Coaching Program to Reduce Burnout in Female Resident Physicians: A Randomized Clinical Trial. JAMA Netw Open. 2022;5(5):e2210752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mazzo A, Martins JC, Jorge BM, Batista RC, Almeida RG, Henriques FM, et al. Validation of the self-confidence scale of nursing care in urinary retention. Rev Lat Am Enfermagem. 2015;23(5):814–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mircioiu C, Atkinson J. A Comparison of Parametric and Non-Parametric Methods Applied to a Likert Scale. Pharmacy (Basel). 2017;5(2):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Drake RL, Pawlina W. Multimodal education in anatomy: The perfect opportunity. Anat Sci Educ. 2014;7(1):1–2. [DOI] [PubMed] [Google Scholar]
- 22.Meyer JJ, Obmann MM, Gießler M, Schuldis D, Brückner AK, Strohm PC, et al. Interprofessional approach for teaching functional knee joint anatomy. Ann Anat. 2017;210:155–9. [DOI] [PubMed] [Google Scholar]
- 23.So S, Patel RM, Orebaugh SL. Ultrasound imaging in medical student education: Impact on learning anatomy and physical diagnosis. Anat Sci Educ. 2017;10(2):176–89. [DOI] [PubMed] [Google Scholar]
- 24.Roxburgh M, Evans DJR. Assessing Anatomy Education: A Perspective from Design. Anat Sci Educ. 2021;14(3):277–86. [DOI] [PubMed] [Google Scholar]
- 25.Gasmalla HEE, Mossa AH, Taha MH, Wadi MM, Shehzad K, Abdalla ME, Hadie SNH. Promoting more future-ready anatomy education after the Covid-19 pandemic: A scoping review. Anat Sci Educ. 2022;15(6):1120–37. [DOI] [PubMed] [Google Scholar]
- 26.Chytas D, Salmas M, Demesticha T, Troupis T. Technological resources in anatomy education: Are there any which are worth the effort more than others? Anat Sci Educ. 2023;16(2):187–8. [DOI] [PubMed] [Google Scholar]
- 27.Vink S, van Tartwijk J, Verloop N, Gosselink M, Driessen E, Bolk J. The articulation of integration of clinical and basic sciences in concept maps: differences between experienced and resident groups. Adv Health Sci Educ Theory Pract. 2016;21(3):643–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Konno SI. Integrating basic knowledge and clinical ability. Journal of orthopaedic science : official journal of the Japanese Orthopaedic Association. 2019;24(5):763. [DOI] [PubMed] [Google Scholar]
- 29.Bergman EM, van der Vleuten CP, Scherpbier AJ. Why don’t they know enough about anatomy? A narrative review Med Teach. 2011;33(5):403–9. [DOI] [PubMed] [Google Scholar]
- 30.Schneid SD, Pashler H, Armour C. How much basic science content do second-year medical students remember from their first year? Med Teach. 2019;41(2):231–3. [DOI] [PubMed] [Google Scholar]
- 31.Bass RZ, Morgan DE, Brooks WS. A Case of Pancreatic Cancer: Abdominal Anatomy Team-Based Learning Module for Medical Students. MedEdPORTAL : the journal of teaching and learning resources. 2018;14:10700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barry DS, Dent JM, Hankin M, Moyer D, Shah NL, Tuskey A, Soukoulis V. The Clinical Anatomy and Imaging Laboratory: Vertical Integration in the Preclerkship Curriculum. MedEdPORTAL : the journal of teaching and learning resources. 2019;15:10824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.De La Hoz PM, Torramilans Lluís A, Pozuelo Segura O, Anguera Bosque A, Esmerado Appiani C, Caminal Mitjana JM. Ocular ultrasonography focused on the posterior eye segment: what radiologists should know. Insights Imaging. 2016;7(3):351–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marchese A, Cicinelli MV, Amato A, Bandello F, Gupta V, Miserocchi E, Agarwal A. The Next Steps in Ocular Imaging in Uveitis. Ocul Immunol Inflamm. 2023;31(4):785–92. [DOI] [PubMed] [Google Scholar]
- 35.Ramachandran A, Das T, Pathengay A, Pappuru RR, Dave VP. Surgical approach to endophthalmitis: an overview. Eye (Lond). 2024;38(13):2516–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Spaide RF, Fujimoto JG, Waheed NK, Sadda SR, Staurenghi G. Optical coherence tomography angiography. Prog Retin Eye Res. 2018;64:1–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Waheed NK, Rosen RB, Jia Y, Munk MR, Huang D, Fawzi A, et al. Optical coherence tomography angiography in diabetic retinopathy. Prog Retin Eye Res. 2023;97:101206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mangan MS, Atalay E, Arici C, Tuncer I, Bilgec MD. Comparison of Different Types of Complications in the Phacoemulsification Surgery Learning Curve According to Number of Operations Performed. Turk J Ophthalmol. 2016;46(1):7–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mangan MS, Cakir A, Imamoglu S. Cumulative Sum Analysis of the Learning Curve of Ptosis Surgery: External Levator Advancement versus Muller Muscle-conjunctival Resection. Korean J Ophthalmol. 2021;35(5):383–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tan B, Chua J, Wong D, Liu X, Ismail M, Schmetterer L. Techniques for imaging the choroid and choroidal blood flow in vivo. Exp Eye Res. 2024;247:110045. [DOI] [PubMed] [Google Scholar]
- 41.Zhang W, Kaser-Eichberger A, Fan W, Platzl C, Schrödl F, Heindl LM. The structure and function of the human choroid. Ann Anat. 2024;254:152239. [DOI] [PubMed] [Google Scholar]
- 42.Middleton S. Porcine ophthalmology. Vet Clin North Am Food Anim Pract. 2010;26(3):557–72. [DOI] [PubMed] [Google Scholar]
- 43.Nakashizuka H, Wakatsuki Y, Machida Y, Okubo Y, Shinojima A, Hattori T, et al. Wet laboratory training using porcine eyes with eyelids. Can J Ophthalmol. 2017;52(4):398–402. [DOI] [PubMed] [Google Scholar]
- 44.Kyllar M, Štembírek J, Danek Z, Hodan R, Stránský J, Machoň V, Foltán R. A porcine model: surgical anatomy of the orbit for maxillofacial surgery. Lab Anim. 2016;50(2):125–36. [DOI] [PubMed] [Google Scholar]
- 45.Kuo MX, Sarris M, Coroneo MT. Cadaveric Porcine Model for Teaching and Practicing Conjunctival Autograft Creation. Cornea. 2015;34(7):824–8. [DOI] [PubMed] [Google Scholar]
- 46.Machuk RWA, Arora S, Kutzner M, Damji KF. Porcine cataract creation using formalin or microwave treatment for an ophthalmology wet lab. Can J Ophthalmol. 2016;51(4):244–8. [DOI] [PubMed] [Google Scholar]
- 47.Sun X, Chen D, Liu X, Yan X, Wu Y. Effect of enzyme-induced collagen crosslinking on porcine sclera. Biochem Biophys Res Commun. 2020;528(1):134–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data and materials supporting the findings herein are available from the corresponding author upon reasonable request.