Abstract
Aim
The aim of this systematic review and meta-analysis was to explore the effects of different pulmonary rehabilitation on respiratory function in mechanically ventilated patients and to determine the optimal type of intervention.
Method
A comprehensive search was conducted using PubMed, Embase, Web of Science, Joanna Briggs Institute(JBI), and the Cochrane Library from their inception until September 16th, 2024. The search targeted randomized controlled trials (RCTs) comparing pulmonary rehabilitation or usual care, for improving respiratory function in mechanically ventilated patients. We performed a meta-analysis utilizing Endnote X9 and R 4.3.1.
Results
Twelve articles were included for systematic review and ten articles were analyzed in the meta-analysis.The primary outcomes such as Maximum inspiratory pressure(MIP)[n = 10 studies, sample size 216 (intervention) vs. 218 (control), MD = 7.45, 95% CI: 3.81 to 11.09], Maximum expiratory pressure(MEP)[n = 5 studies, sample size 115 (intervention) vs. 112 (control), MD = 13.98, 95% CI:7.41 to 20.54], Rapid shallow breathing index(RSBI)[n = 4 studies, sample size 96 (intervention) vs. 98 (control), MD = -33.85, 95% CI:-71.18 to 3.48] and Tidal volume(VT)[n = 4 studies, sample size 96 (intervention) vs. 98 (control), MD = 74.64, 95% CI:21.7 to 127.57] shows that MIP, MEP and VT significantly improved after the pulmonary rehabilitation.The random-effects models were employed because of the modest degree of heterogeneity present.
Conclusion
Pulmonary rehabilitation showed mixed effects on significantly improved the MIP, MEP, VT and DT. Pulmonary rehabilitation by inspiratory muscle training could administer the best therapeutic effect, followed by neuromuscular electrical stimulation.
Clinical trial number
Not applicable.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12890-024-03461-4.
Keywords: Pulmonary rehabilitation; MIP; MEP, REBI; VT
Mechanical ventilation(MV) is a life-saving therapy widely used in ICU patients to support oxygenation and ventilation [1]. However, its prolonged use is associated with complications such as pulmonary atelectasis, diaphragmatic dysfunction, and ventilator-associated pneumonia, resulting in decreased respiratory function, prolonged hospitalization as well as increased mortality [2]. Recently, there have been increasing number of studies showing that pulmonary rehabilitation(PR) can strengthen the patient’s muscles, stabilize or reduce pulmonary symptoms so that alleviate the adverse effects of mechanical ventilation [3, 4].
Clinical Practice Guideline demonstrated that PR is an individualized, comprehensive intervention therapy to help mechanically ventilated patients weaning from the machine as early as possible, reduce the incidence of pulmonary complications, and improve quality of life [5].An official American Thoracic Society and European Respiratory Society stated that there is increased evidence for use and efficacy of a variety of forms of exercise training as part of PR, which include interval training, strength training, extremity exercise training, and transcutaneous neuromuscular electrical stimulation [6].Rehabilitation in ICU patients was considered contraindicated in more than 40% of ICU bed days, mainly due to sedation and renal replacement issues [7]. However, treatment modalities, such as PR do not interfere with renal replacement or sedation [8]. Continuous passive motion prevents contractures in ICU patients and respiratory failure with prolonged inactivity [9].In acute critically ill individuals with respiratory failure, unable to move actively, reductions in muscle atrophy and critical illness neuropathy were observed when using NMES [10].
Maximum inspiratory pressure(MIP) and Maximum expiratory pressure(MEP) are non-invasive parameters used to assess respiratory muscle strength and appear to be distinct predictors of survival [11].While tidal volume (VT) is one of the unique lung volumes and most convenient indicator to measure [12].Rapid shallow breathing index (RSBI), defined as the ratio of breathing frequency to average tidal volume in 1 min (breaths/min/L), has been shown to be one of the most accurate predictors of weaning outcome [13].Obviously, these indicators are valid and sensitive indicators to detect pulmonary function, but there are a lack of studies discussing how PR affects respiratory function in mechanically ventilated patients.
Currently, there are numerous studies focusing on pulmonary rehabilitation in ICU worldwide [14, 15],but there are some weak points such as inconsistency of interventions, lack of multidisciplinary cooperation and variable indicators, which have caused that optimal PR protocol remains uncertain. The aim of this systematic review and meta-analysis was to explore the effects of different PR on respiratory function in mechanically ventilated patients and to determine the optimal rehabilitation type.
Method
The present study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and registered on PROSPERO (CRD42021243331; 2021/4/17).
Study selection
The study selection criteria were based on the Population, Intervention, Comparison, and Outcome (PICO) method. The PICO parameters for this article were as follows: Population, mechanical ventilation patients; Intervention, Pulmonary rehabilitation, which mainly includes respiratory exercises such as effective coughing, lip-contraction breathing, respiratory training, neuromuscular electrical stimulation, upper and lower extremity exercise training and physical therapy, and the experimental group may use one or more of the above measures [16]; Comparison, conventional treatment; Outcome, Pulmonary function parameters (e.g., tidal volume, respiratory rate, and rapid shallow respiration index), respiratory muscle strength (determined by maximal inspiratory and expiratory pressures), diaphragm thickness, diaphragm excursion.
The following inclusion criteria were used for study selection: (1) The age of the participants was ≥ 18 years old, and the duration of mechanical ventilation in ICU was ≥ 24 h. (2)The interventions must compare the control groups with the implementation of PR with general therapy, or both groups applied PR but with higher intensity or frequency in the intervention groups (3) The outcome measures were focused on respiratory function, such as MIP or VT. (4) Randomized controlled trials (RCTs) in English published in peer-reviewed journals and the studies provided information on the intervention protocol and dosage. Unpublished manuscripts and conference abstracts were not eligible for study selection. The exclusion criteria were duplicate publications and studies from which outcome data could not be extracted.
Data sources and searches
The concatenation of keywords and synonyms by “OR” and “AND” were searched in the following five databases on September 16th, 2024: PubMed, Cochrane Library, EMBASE, Web of Science and Joanna Briggs Institute(JBI).The keywords included breathing exercise, pulmonary rehabilitation, neuromuscular electrical stimulation, NMES, respiratory training, mechanical ventilation, ICU, critically ill patients, intensive care unit.Medical Subject Headings (MeSH) terms, free words and Boolean operators were used to search for relevant studies.Additionally, the reference lists of retrieved studies were also screened to identify additional relevant articles. The original authors were contacted by email when necessary data were missing.The detailed search strategy is shown in Supplementary Material Table 2.
The data search were performed using Endnote X9.Two reviewers (XYX and DDZ) independently screened the titles and abstracts of the collected articles.Disagreements were decided by questioning a third researcher(SZC). Subsequently, full-text reading was conducted for rescreening. In addition, reference lists of the included literature and previously published reviews were searched manually.
Quality assessment
We used the risk-of-bias2 (RoB2), a revised Cochrane RoB tool to assess the quality of the study design and extent of potential bias [17]. Two reviewers (XYX., DDZ.) resolved disagreements through discussion, and a third reviewer (SZC) adjudicated.The assessment items included bias arising from the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in the measurement of outcome, and bias in the selection of the reported result.High, low, and some concerns was determined through formulated signaling questions in each domain.
Grading of recommendations Assessment, Development, and evaluation Approach
Two researchers(XYX.,DDZ.) independently assessed the quality of evidence and strength of recommendation, while a third reviewer (SZ C.) judged disagreement.The CoE evaluation was based on the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) tool.
Data extraction
The data and results from the included studies were extracted by using a standardized spreadsheet of Excel (Microsoft Excel 2016; Microsoft Corp., Redmond, WA, USA) that documented basic information regarding the study (e.g., first author, year of publication, country), characteristics of participants (e.g.,sample size, participants’ type, setting), type of intervention (e.g., pulmonary rehabilitation type, time, frequency, intensity, duration), type of control group and outcome (e.g., MIP, MEP, VT, REBI, RR, diaphragm thickness, diaphragm excursion).Outcomes reported as continuous variables were presented as means ± standard deviations. If only the median and interquartile range were reported, they were converted to mean and standard deviation using appropriate statistical formulas [18].All data were extracted independently by two reviewers (XYX and DDZ). When results were missing or not fully reported, efforts were made to contact the contributing authors to retrieve missing data.
Data synthesis and analyses
The statistical analyses were performed using R 4.3.1. Heterogeneity among studies was examined with Chi-squared test and statistics. When P < 0.01 andI2 > 50%, the statistics indicated high heterogeneity, and a random-effects model would be chosen; otherwise, a fixed-effects model was adopted.In our review, the outcomes were continuous variables so as Mean differences (MDs) with 95% CIs were used. Guided by Cochrane Statistical Methods Group (2022) recommendations: <40% signifies low, 30–60% moderate,50–90% substantial, and 75–100% considerable heterogeneity, considering p-values and confidence interval.Egger test was used to detect publication bias when studies were larger than 10, with P < 0.05 indicating the presence of bias.
Post hoc analysis
We performed subgroup analyses with type duration, setting, participations, and MV-duration as subsets by using R 4.3.1.Sensitivity analysis was also performed using the same software. The analysis was based on available data from the included studies, and the methods used are consistent with the overall approach outlined previously.
Results
Study recruitment
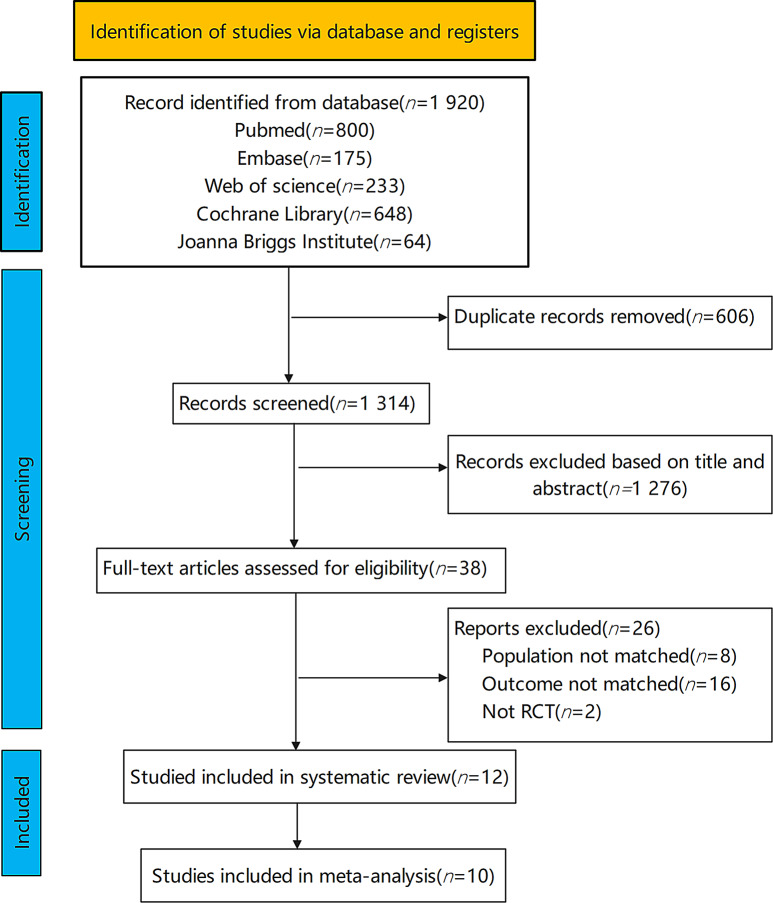
A total of 1920 records were obtained by searching five databases and manual search, of which 606 duplicated records by the Endnote X9 software were excluded. After screening the titles and abstracts, a total of 38 records were entered into the full-text screening. Two reviewers (YXX and DDZ) independently evaluated the full texts for eligibility and excluded 26 irrelevant records(population not matched = 8,outcome not matched = 16,not RCT = 2). Finally, 12 articles reporting 10 studies met our inclusion criteria and were included in this review [19–30].The specific PRISMA flow diagram is shown in Fig. 1.
Fig. 1.
PRISMA flow diagram
Characteristics of included studies
Twelve RCTs including 547 participants in total were published between 2005 and 2024. Six studies were conducted in Asia regions (China) and Six in non-Asia regions (Brazil, Egypt). Eleven(91.67%) studies were two-arm parallel RCTs, while one study was a three-arm clinical trial [26]. However, considering the exercise type and study objective, we only included data from one selected intervention and control group in this three-arm study.Studies were held in different settings, with five studies being implemented in ICU [19, 23, 24, 28, 30], four in respiratory care center(RCC) [21, 22, 25, 27],two in surgical ICUs [20, 26], and one in neurosurgical department [29].The types of participants varied from the different studies, six studies with the most frequently included prolonged mechanical ventilation(PMV) [20–23, 25, 28].The included participants had varying mechanical ventilation duration, with the shortest being 24 h [26, 29] and the longest being 63 days [27]. None of the included studies reported related adverse events. The detailed summary characteristics of the included RCTs are shown in Table 1.
Table 1.
Detailed summary characteristics of the included RCTs
| Study | Country | Sample Size(Intervention/Control) | Pulmonary rehabilitation type | Intervention frequency | Intervention intensity | Intervention duration | Control group | Setting | Participants’ type | Mechanical ventilation Duration |
|---|---|---|---|---|---|---|---|---|---|---|
| Cader et al.2012 [19] | Brazil | 14/14 | IMT | twice a day, 7 days a week | Initial load of 30% of the MIP, increasing daily by 10% |
until extubation |
conventional physiotherapy |
ICU |
bed-ridden elderly intensive care patients |
≥ 48 h |
| Chen et al.2012 [21] | China | 12/15 | IMT + Extremity muscle training | 4–6 sessions a week | 60–80% of age-predicted maximal heart rate | 14 days | same treatment except for exercise training | RCC | Prolonged Mechanical Ventilation(PMV) | ≥ 21 days |
| Chiang et al.2006 [22] | China | 17/15 | Extremity muscle training | 5 times a week | Set at 10 to 11 for the first week and then progressed to 12 to 13 for the next 5weeks. | 42 days | standard therapy | RCC | PMV | ≥ 14 days |
| Condessa et al.2013 [23] | Brazil | 38/39 | IMT | twice a day, seven days a week |
with a load equal to 40% of the participant’s MIP |
until extubation |
usual care | ICU | PMV | ≥ 48 h |
| Dantas et al.2023 [24] | Brazil | 14/14 | Extremity muscle training | twice a day, every day of the week | / | 42 days | passive mobilization of the four limbs | ICU | Critical illness | ≥ 48 h |
| Hsin et al.2022 [25] | China | 29/30 | NMES | 5 days a week | Observed visible muscle contraction | 7 days | similar intervention, except that the stimulator power was off. | RCC | PMV | > 21 days |
| Leite et al.2018 [26] | Brazil | 17/26 | NMES | once a day | produced visible contractions | until ICU discharge | regular treatment | Surgical ICU | Critical illness | ≥ 24 h |
| Lin et al.2024 [27] | China | 17/14 | Abdominal sandbag training | twice a day, five days a week | maintain a tidal volume of 8 mL/kg | 90 days |
standard chronic weaning protocol |
RCC |
Chronic respiratory failure |
≥ 63 days |
| Reshia et al.2023 [28] | Egypt | 35/35 | Chest physiotherapy | / | / | / | standard nursing chest care | ICU | PMV | ≥ 48 h |
| Yang et al.2024 [29] | China | 40/40 | IMT | twice a day | vibration frequency of 40 Hz | 7 days | routine care | neurosurgical department |
Mechanically ventilated patients following brainstem hemorrhage |
≥ 24 h |
| Zhou et al.2024 [30] | China | 23/24 | NMES + IMT | twice a day | set at 50% of MIP | 5 days | routine care | ICU |
neurocritical patients with weaning failure |
≥ 48 h |
| Caruso et al.2005 [20] | Brazil | 12/13 | IMT | twice a day | 40% of MIP | 10 days | received no inspiratory muscle training, | Surgical ICU | PMV | > 72 h |
Abbreviations IMT, Inspiratory muscle training; NMES, Neuromuscular electrical stimulation; MIP, Maximum Inspiratory Pressure; ICU, Intensive care unit; RCC, Respiratory Care Center; PMV, Prolonged Mechanical Ventilation
Characteristics of the interventions
In our review, four included studies evaluated inspiratory muscle training(IMT) only [19, 20, 23, 29] ,two separate studies have utilized extremity muscle training(EMT) [22, 24], neuromuscular electrical stimulation(NMES) [25, 26] and combined interventions [21, 30],while the remaining study evaluated the effects of chest physiotherapy [28] and abdominal sandbags training [27]. The frequency, intensity and duration of PR varied across the studies, with intervention duration ranging from 5days to 90 days, and the most common(58.33%)frequency was twice a day [19, 20, 23, 24, 27, 29, 30]. Because of the different types of interventions, the intensity cannot be summarized or comparison directly. All studies report the monitoring of intervention and treatment of control group.Two articles [26, 28] lacked primary outcome data after contacting the authors therefore they were included in the systematic review but excluded in the meta-analysis.
Risk of bias and quality assessment
Overall, five studies were rated as having some concerns [20, 24, 26, 27, 29] ,two studies were at high risk of bias [21, 22], and five studies were rated as low risk [19, 23, 25, 28, 30].Most of bias caused by deviations from intended interventions.Detailed risk of bias assessment for each study is shown in Supplementary Fig. 1.
Meta-analysis outcomes
Primary outcomes
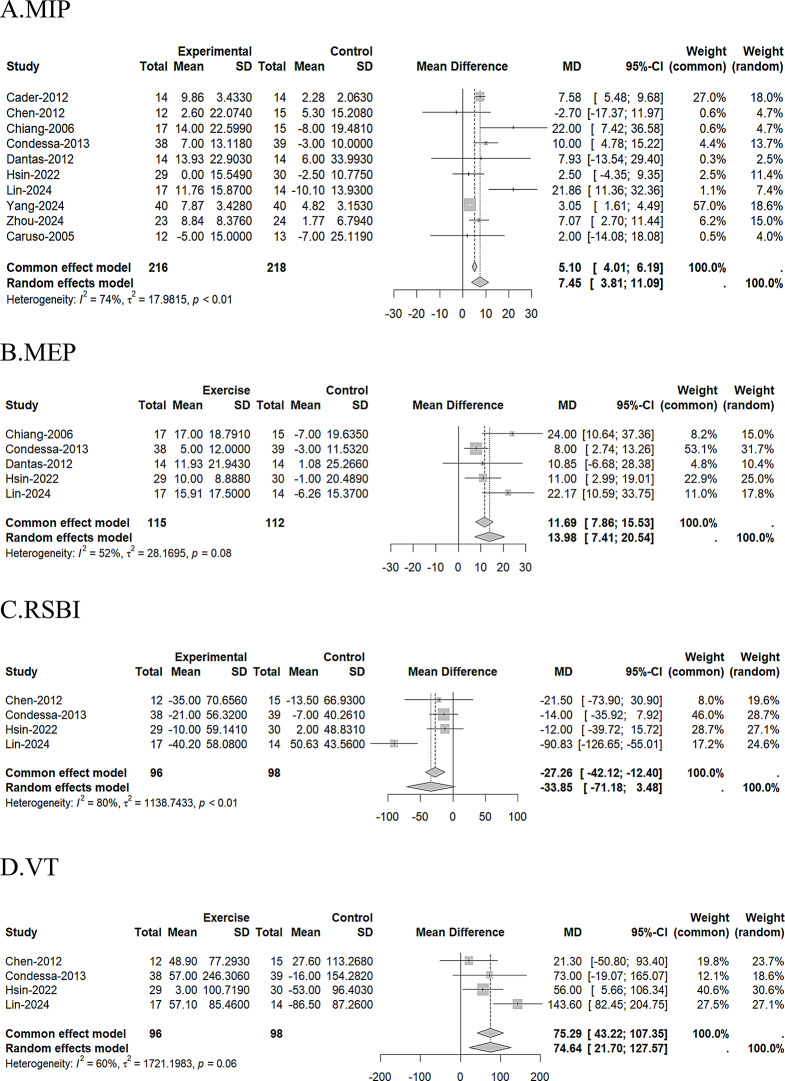
Among these analyses, The primary outcomes such as MIP[n = 10 studies, sample size 216 (intervention) vs. 218 (control), MD = 7.45, 95% CI: 3.81 to 11.09,I2 = 74%], MEP[n = 5 studies, sample size 115 (intervention) vs. 112 (control), MD = 13.98, 95% CI:7.41 to 20.54,I2 = 52%], RSBI[n = 4 studies, sample size 96 (intervention) vs. 98 (control), MD = -33.85, 95% CI:-71.18 to 3.48,I2 = 80%] and VT[n = 4 studies, sample size 96 (intervention) vs. 98 (control), MD = 74.64, 95% CI:21.7 to 127.57,I2 = 60%] shows that MIP, MEP and VT significantly improved after the pulmonary rehabilitation, yet RSBI have no significance, this may be due to the heterogeneity as well as the small number of included studies.The random-effects models were employed because of the modest degree of heterogeneity present.The results of the meta-analyses are presented in Fig. 2.
Fig. 2.
Pairwise meta-analysis of direct comparisons. A. Forest plot of MIP. B. Forest plot of MEP. C. Forest plot of RSBI. D. Forest plot of VT
Secondary outcome
The meta-analyses results are presented in Supplementary Fig. 2.Respiratory rate(RR)[n = 3 studies, sample size 58 (intervention)vs 59 (control), MD = -1.82, 95% CI:-6.4 to 2.76,I2 = 70%], Diaphragm thickness(DT)[n = 2 studies, sample size 40 (intervention)vs 38 (control), MD = 0.51, 95% CI:0.19 to 0.83,I2 = 1%] and Diaphragm Motion(DM))[n = 2 studies, sample size 40 (intervention)vs 38 (control), MD = -0.06, 95% CI:-0.27 to 0.14,I2 = 0%] were secondary outcome indicators in which only DT reached statistical significance, in contrast DM and RR seemed no different after rehabilitation. RR shown to be heterogeneous, while VT and VD had low heterogeneity.
Publication bias
The results of the test are shown in Supplementary Table 3,Egger’s test provided no evidence of publication bias (p value of MIP = 0.6835).
Sensitivity analysis
Sensitivity analysis is shown in Supplementary Fig. 3. The combined results of MIP, MEP and VT remained statistically different after sequential exclusion.However RSBI and VT only become consistently after elimination 1 article [27],and their conclusion remained unchanged, possibly related to only this study utilized the abdominal sandbag training method. After the majority of the literature was excluded, the combined results of the remaining studies did not differ significantly, demonstrating the robustness of the results of the meta-analysis.
Subgroup analysis
The result of the subgroup analysis is presented in supplementary Table 4.According to the characteristics of included studies, we performed subgroup analyses for each of the primary outcomes, which showed that the source of MIP heterogeneity was likely to be intervention type and MV duration.This is consistent with the theory that MIP declines with the reduction of diaphragmatic contractility in the early stages of MV, and further reduction is caused by hyperinflation of the lungs as well as reduced inspiratory muscle strength [31].The results of MEP were provisionally non-significant.Therefore, we suggest that IMT for patients with MV ≥ 48 h is the optimal method of PR, while the rest of the results have provided hypotheses for further studies that could potentially confirm the efficacy of the specific measures.However, subgroup analysis concerning different intervention frequency, intensity and duration could not be undertaken due to insufficient data as well as non-harmonized units.
GRADE evidence quality evaluation
The quality of evidence for all outcomes was scored using the GRADE method and was characterized by a high degree of heterogeneity between studies due to the absence of blinding, inadequate allocation concealment, and small number of study subjects.MIP, MEP and RR were moderate-quality evidence, VT, DT, and DM were low-quality evidence, while RSBI were very low-quality evidence. Detailed evidence quality evaluation is summarized in Supplementary Table 5.
Discussion
This systematic review and meta-analysis highlighted the benefits of PR on respiratory function in mechanically ventilated patients, which could significantly improve MIP, MEP, VT, diaphragm thickness and diaphragm motion.However, there was little difference in the RSBI and very uncertain evidence on RR.Furthermore, our findings demonstrated that PR by IMT could administer the best therapeutic effect, followed by NMES.Training could be applies using an inspiratory threshold device with the frequency of twice a day, 7 days a week, while initial intensity load of 30% of the MIP, increasing daily by 10%.Moreover, these measures were more effective in patients who have been mechanically ventilated in the ICU for more than 48 h.Regarding the duration of the intervention, the effect of the 7-day program was not significantly different from the 42-day option.Only one study [30] investigated the effect of NMES combined with IMT on the Oxygen indicator(OI).This indicates that further RCTs are necessary to obtain more data.
Although MV is lifesaving, ventilator-associated events still presented certain impairments in lung function and even higher mortality ( [32].Compared to other outcomes, MIP, MEP, VT, RSBI, etc. are directly visible indicators that can clearly reflect the changes in respiratory function, increasing the ICU team’s awareness and acceptance of PR. In accordance with the GOLD guideline [33], the outcomes of pulmonary function tests can assess patient’s airway obstruction as well as limitation, which include MIP and MEP, at the same time VT, RR and RSBI values can indicate respiratory recovery which are often used as a reference for extubation tests. It has been reported ( [34, 35] that prognostic degree is directly proportional to diaphragm thickness and diaphragm motion. The diaphragm is the main respiratory muscle, and mechanical ventilated suffer from diaphragm fatigue or weakness, leading to respiratory function undergoing attenuation.Our findings proved that PR methods such as IMT and NMES can significantly improve the mentioned indexes, so as to enhance the respiratory muscle level, accelerate the time of weaning, and improve the patients’ quality of life.
Regarding intervention type, our meta-analysis indicated that PR was evenly beneficial for respiratory function, including greater spirometry and shorter ventilator duration, which is in largely accordance with previous findings ( [36, 37].However, these studies focused on prevention or reversal of weaning failure and other clinical outcomes. It remains unknown which is the best intervention among the various protocols.Clinical application still be blocked due to the high heterogeneity of the intervention. In our study, we found that IMT improved MIP and MEP yet had no significant effect on RSBI or VT.This is probably related to the fact that IMT is difficult to monitor and control to meet the rigorous criteria. A meta-analysis showed that although NMES appears to be a straightforward and safe modality for critically ill, when combined with physical therapy (PT), it significantly improved the extubation success rate and showed a better ranking over PT or NMES alone ( [38]. Our results also showed that though NMES had influence on MEP and VT, it was statistically difference on MIP only when combined NMES with IMT, therefore NMES combined with other training may be a superior rehabilitation strategy. Abdominal sandbag training had a remarkable effect on all outcome indicators, but there was a few studies and sample sizes that could be supported as evidence so that further confirmation is needed. There are fewer studies integrating two or more measures, and present results pointed to a non-significant effect of comprehensive PR.As increasing evidence confirms the benefits of PR, exploring a comprehensive PR measure is necessary.
Regarding intervention duration, there is a lack of consensus since the protocol would change with disease category.For instance, neurocritical patients had a shorter duration of rehabilitation (5 days) ( [30],Although our meta-analysis showed PR trended to improve respiratory function regardless of the intervention duration, the protocol with short periods (< 7days) was rarely used in our included studies.More research is required in future to prove what the optimal duration of intervention is.In the clinic, the ICU team needs to constantly consider whether the treatment dose is sufficient or not.Therefore, calculating the type and frequency of intervention may be appropriate to quantify. A cohort study implemented this concept. They used a quantitative activity score (MQS) that combined the intensity and duration of rehabilitation then noted that high doses of activity were independent predictors of patients’ functional ability ([39]. However, relevant data are too scarce to synthesize. We recommend utilizing a scale to quantify PR in forthcoming studies.In addition, a clinical trial, in which both intervention and usual care groups had a long periods of PR, indicated that an increase in intervention was not associated with a better function ([40].The findings were similar to our meta-analysis that performing intervention until ICU discharge may not have a favorable impact on patient functioning even decreased MIP.The excessive treatment may exceed the tolerance and become a burden on ICU patients. Clinical staff should consider the optimal dose of PR for mechanical ventilator rather than lengthen the treatment duration meaninglessly.
In summary, some types of PR could enhance pulmonary function, improve the quality of life, which is consistent with the findings of a number of studies ( [41–43].
Limitation
There were several limitations to this study: (1)Only 10 studies including 504 individuals were eligible to be included in the meta analysis, publication bias and small sample sizes caused a substantial amount of bias.(2) Among the included articles with a low-to-moderate quality, the major risk of bias was a lack of blinding and deviations from intended intervention. Thus, more high-quality RCTs with larger sample sizes in this field are essential. (3) Considering the diversity of respiration-related outcome indicators and the small number of included studies, only the studies reporting the MIP, MEP, RESBI and VT were included in the meta-analysis to ensure the reliability of the study and comparison. (4) Analyses of moderator variables on the effects of pulmonary rehabilitation programs (e.g., age, sex, sample size, comorbidities, and sedation level) were not performed.Meanwhile there were lack of reporting on adverse events.Lesser clinical therapeutic factors could be identified for the treatment plan. (5) Although we used the random-effects model for pooling, the high heterogeneity of intervention duration might not be neglected and should be considered in clinical practice. (6) During the meta-analysis, There was 1 study that directly provide author-calculated mean difference and we did not receive a response from the authors after contact via email ( [27]. In this study, We used the data from the article directly instead of calculating it through the harmonized formula; however, some data extraction bias remains inevitable.(7)The exclusion of non-English studies, which might have introduced selection bias.
Conclusion
This meta-analysis compared the figures of MIP, MEP, RSBI, VT, RR, DM and DT with various PR methods in MV patients.Different types have different benefits while IMT might be the most recommended method, following by the NMES. Moreover, depending on clinical resources and the tolerance of patients, the duration of MV should reach greater than or equal to 24 h. The study results may serve as an empirical basis for devising intervention plans to develop pulmonary rehabilitation in clinical units.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like thank all the people who participated in primary studies.
Author contributions
X conceived and designed the study. X and Z contributed to the literature search, and participated in data collection and statistical analyses. C performed the interpretation and X wrote the manuscript. All authors read and approved the final manuscript.
Funding
Guangzhou Science and Technology Program, provided by, The First Affiliated Hospital of Sun Yat-Sen University(K0220090).
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Perkins GD, Mistry D, Gates S, et al. Effect of Protocolized Weaning with Early Extubation to Noninvasive Ventilation vs Invasive Weaning on Time to Liberation from mechanical ventilation among patients with respiratory failure the Breathe Randomized Clinical Trial. JAMA-J Am Med Assoc. 2018;320(18):1881–8. 10.1001/jama.2018.13763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ries AL, Bauldoff GS, Carlin BW, et al. Pulmonary rehabilitation - joint ACCP/AACVPR evidence-based clinical practice guidelines. Chest. 2007;131(5):S4–42. 10.1378/chest.06-2418. [DOI] [PubMed] [Google Scholar]
- 3.Muñoz-Cofré R, Del Valle MF, Marzuca-Nassr GN, et al. A pulmonary rehabilitation program is an effective strategy to improve forced vital capacity, muscle strength, and functional exercise capacity similarly in adults and older people with post-severe COVID-19 who required mechanical ventilation. BMC Geriatr. 2024;24(1):313. 10.1186/s12877-024-04910-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feng Y, Sun Q, Guan C, Wang S, Wang P, Hu D. [Effect of early pulmonary rehabilitation training on the prognosis of patients with acute respiratory distress syndrome after weaning of invasive mechanical ventilation in the intensive care unit]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2024;36(3):286–92. 10.3760/cma.j.cn121430-20231009-00856. [DOI] [PubMed] [Google Scholar]
- 5.Girard TD, Alhazzani W, Kress JP, et al. An official American Thoracic Society/American College of Chest Physicians Clinical Practice Guideline: Liberation from Mechanical Ventilation in critically ill adults. Rehabilitation Protocols, Ventilator Liberation protocols, and Cuff Leak tests. Am J Respir Crit Care Med. 2017;195(1):120–33. 10.1164/rccm.201610-2075ST. [DOI] [PubMed] [Google Scholar]
- 6.Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–64. 10.1164/rccm.201309-1634ST. [DOI] [PubMed] [Google Scholar]
- 7.Bourdin G, Barbier J, Burle JF, et al. The feasibility of early physical activity in intensive care unit patients: a prospective observational one-center study. Respir Care. 2010;55(4):400–7. [PubMed] [Google Scholar]
- 8.Burtin C, Clerckx B, Robbeets C, et al. Early exercise in critically ill patients enhances short-term functional recovery. Crit Care Med. 2009;37(9):2499–505. 10.1097/CCM.0b013e3181a38937. [DOI] [PubMed] [Google Scholar]
- 9.Griffiths RD, Palmer TE, Helliwell T, MacLennan P, MacMillan RR. Effect of passive stretching on the wasting of muscle in the critically ill. Nutr Burbank Los Angel Cty Calif. 1995;11(5):428–32. [PubMed] [Google Scholar]
- 10.Routsi C, Gerovasili V, Vasileiadis I, et al. Electrical muscle stimulation prevents critical illness polyneuromyopathy: a randomized parallel intervention trial. Crit Care Lond Engl. 2010;14(2):R74. 10.1186/cc8987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wanger J, Clausen JL, Coates A, et al. Standardisation of the measurement of lung volumes. Eur Respir J. 2005;26(3):511–22. 10.1183/09031936.05.00035005. [DOI] [PubMed] [Google Scholar]
- 12.Bhakta NR, McGowan A, Ramsey KA, et al. European Respiratory Society/American Thoracic Society technical statement: standardisation of the measurement of lung volumes, 2023 update. Eur Respir J. 2023;62(4). 10.1183/13993003.01519-2022. [DOI] [PubMed]
- 13.Rittayamai N, Ratchaneewong N, Tanomsina P, Kongla W. Validation of rapid shallow breathing index displayed by the ventilator compared to the standard technique in patients with readiness for weaning. BMC Pulm Med. 2021;21(1):310. 10.1186/s12890-021-01680-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumar Khurana A, Hussain A, Goyal A, et al. Six-Week Hospital-based Pulmonary Rehabilitation in Covid Pneumonia ICU survivors: experience from a Tertiary Care Center in Central India. Turk Thorac J. 2022;23(2):89–96. 10.5152/TurkThoracJ.2022.21159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang Y, Zhang RJ, Yuan XN, et al. Clinical effect of pulmonary rehabilitation in patients with mechanical ventilation: a meta-analysis. Int J Artif Organs. 2024;47(2):96–106. 10.1177/03913988231218116. [DOI] [PubMed] [Google Scholar]
- 16.Liu S, Wang LW, Wang SM, Qin X, Zhang Q, Guan CH. Meta-analysis of the effect of pulmonary rehabilitation in mechanically ventilated patients. Chin J Acute Crit Care Nurs. 2021;2(2):140–5. [Google Scholar]
- 17.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 18.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cader SA, de Souza Vale RG, Zamora VE, Costa CH, Martin Dantas EH. Extubation process in bed-ridden elderly intensive care patients receiving inspiratory muscle training: a randomized clinical trial. Clin Interv AGING. 2012;7:437–43. 10.2147/CIA.S36937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caruso P, Denari SDC, Ruiz SAL, et al. Inspiratory muscle training is ineffective in mechanically ventilated critically ill patients. Clin Sao Paulo Braz. 2005;60(6):479–84. [DOI] [PubMed] [Google Scholar]
- 21.Chen YH, Lin HL, Hsiao HF, et al. Effects of Exercise training on pulmonary mechanics and functional status in patients with prolonged mechanical ventilation. Respir CARE. 2012;57(5):727–34. 10.4187/respcare.01341. [DOI] [PubMed] [Google Scholar]
- 22.Chiang LL, Wang LY, Wu CP, Wu HD, Wu YT. Effects of physical training on functional status in patients with prolonged mechanical ventilation. Phys Ther. 2006;86(9):1271–81. 10.2522/ptj.20050036. [DOI] [PubMed] [Google Scholar]
- 23.Condessa RL, Brauner JS, Saul AL, Baptista M, Silva ACT, Vieira SRR. Inspiratory muscle training did not accelerate weaning from mechanical ventilation but did improve tidal volume and maximal respiratory pressures: a randomised trial. J Physiother. 2013;59(2):101–7. 10.1016/S1836-9553(13)70162-0. [DOI] [PubMed] [Google Scholar]
- 24.Dantas CM, Silva PFDS, de Siqueira FHT, et al. Influencia Da Mobilizacao precoce na forca muscular periferica e respiratoria em pacientes criticos. Rev Bras Ter Intensiva. 2012;24(2):173–8. [PubMed] [Google Scholar]
- 25.Hsin YF, Chen SH, Yu TJ, Huang CC, Chen YH. Effects of transcutaneous electrical diaphragmatic stimulation on respiratory function in patients with prolonged mechanical ventilation. Ann Thorac Med. 2022;17(1):14–20. 10.4103/atm.atm_158_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leite MA, Osaku EF, Albert J, et al. Effects of Neuromuscular Electrical Stimulation of the quadriceps and Diaphragm in critically ill patients: a pilot study. Crit Care Res Pract. 2018;2018:4298583. 10.1155/2018/4298583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin TK, Chen MY, Cheng HH, Chow J, Chen CM, Chou W. Effectiveness of abdominal sandbag training in enhancing diaphragm muscle function and exercise tolerance in patients with chronic respiratory failure. J Formos Med Assoc. 2024;123(10):1087–92. 10.1016/j.jfma.2024.01.021. [DOI] [PubMed] [Google Scholar]
- 28.Reshia FAA, Salameh B, Alsadaan N, et al. Enhancing pulmonary function and arterial blood gas readings through immediate chest physiotherapy among extubated patients in ICU. J Int Med Res. 2023;51(11):03000605231208600. 10.1177/03000605231208600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang W, Xu B, Zhao L, Guo A, Zhang M, Lin Z. Assessing the efficacy of a graded pulmonary rehabilitation protocol in mechanically ventilated patients following brainstem hemorrhage. Med (Baltim). 2024;103(27):e38783. 10.1097/MD.0000000000038783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhou Q, Zhang Y, Yao W, Liang S, Feng H, Pan H. Effects of proprioceptive neuromuscular facilitation combined with threshold inspiratory muscle training on respiratory function in neurocritical patients with weaning failure: a randomized controlled trial. Int J Rehabil Res. 2024;47(3):164–8. 10.1097/MRR.0000000000000627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spadaro S, Marangoni E, Ragazzi R, et al. A methodological approach for determination of maximal inspiratory pressure in patients undergoing invasive mechanical ventilation. Minerva Anestesiol. 2015;81(1):33–8. [PubMed] [Google Scholar]
- 32.Muscedere J, Sinuff T, Heyland DK, et al. The clinical impact and preventability of Ventilator-Associated conditions in critically ill patients who are mechanically ventilated. Chest. 2013;144(5):1453–60. 10.1378/chest.13-0853. [DOI] [PubMed] [Google Scholar]
- 33.Halpin DMG, Criner GJ, Papi A, Prevention of Chronic Obstructive Lung Disease. Global Initiative for the Diagnosis, Management, and. The 2020 GOLD Science Committee Report on COVID-19 and Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2021;203(1):24–36. 10.1164/rccm.202009-3533SO [DOI] [PMC free article] [PubMed]
- 34.Goligher EC, Fan E, Herridge MS, et al. Evolution of Diaphragm thickness during mechanical ventilation. Impact of Inspiratory Effort. Am J Respir Crit Care Med. 2015;192(9):1080–8. 10.1164/rccm.201503-0620OC. [DOI] [PubMed] [Google Scholar]
- 35.Grosu HB, Ost DE, Lee YI, et al. Diaphragm muscle thinning in subjects receiving mechanical ventilation and its Effect on Extubation. Respir CARE. 2017;62(7):904–11. 10.4187/respcare.05370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Salcedo PA, Lindheimer JB, Klein-Adams JC, Sotolongo AM, Falvo MJ. Effects of Exercise training on pulmonary function in adults with chronic lung disease: a Meta-analysis of Randomized controlled trials. Arch Phys Med Rehabil. 2018;99(12):2561–e25697. 10.1016/j.apmr.2018.03.014. [DOI] [PubMed] [Google Scholar]
- 37.Wu RYE, Yeh HJE, Chang KJE, Tsai MWE. Effects of different types and frequencies of early rehabilitation on ventilator weaning among patients in intensive care units: a systematic review and meta-analysis. PLoS ONE. 2023;18(4):e0284923. 10.1371/journal.pone.0284923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Effect of neuromuscular electrical stimulation in critically ill adults with mechanical ventilation: a systematic review and network meta-analysis | BMC Pulmonary Medicine | Full Text. Accessed August 31. 2024. https://bmcpulmmed.biomedcentral.com/articles/10.1186/s12890-024-02854-9 [DOI] [PMC free article] [PubMed]
- 39.Scheffenbichler FT, Teja B, Wongtangman K, et al. Effects of the level and duration of mobilization therapy in the Surgical ICU on the loss of the ability to live independently: an international prospective cohort study. Crit Care Med. 2021;49(3):e247–57. 10.1097/CCM.0000000000004808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu W, Mu X, Wang X, Zhang P, Zhao L, Li Q. Effects of comprehensive pulmonary rehabilitation therapy on pulmonary functions and blood gas indexes of patients with severe pneumonia. Exp Ther Med. 2018;16(3):1953–7. 10.3892/etm.2018.6396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu Y, Gong Y, Zhang C, et al. Effect of neuromuscular electrical stimulation combined with early rehabilitation therapy on mechanically ventilated patients: a prospective randomized controlled study. BMC Pulm Med. 2023;23(1):272. 10.1186/s12890-023-02481-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shaaban L, Abdeen A, Saleh HM, Mahran SA, Farghaly S. Early rehabilitation program and weaning outcomes in critically ill chronic obstructed airway disease patients: a randomized trial. Egypt J Bronchol. 2022;16(1):32. 10.1186/s43168-022-00128-8. [Google Scholar]
- 43.Zheng MH, Liu WJ, Yang J. Effect of early stepwise cardiopulmonary rehabilitation on function and quality of life in sepsis patients. World J Clin Cases. 2024;12(4):729–36. 10.12998/wjcc.v12.i4.729. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.