Abstract
Background
The severe health challenge and financial burden of drug-resistant tuberculosis (DR-TB) continues to be an impediment in China and worldwide. This study aimed to explore the impact of Diagnosis-related group (DRG) payment on medical expenditure and treatment efficiency among DR-TB patients.
Methods
This retrospective cohort study included all DR-TB patients from the digitized Hospital Information System (HIS) of Wuhan Pulmonary Hospital and the TB Information Management System (TBIMS) with completed full course of National Tuberculosis Program (NTP) standard treatment in Wuhan from January 2016 to December 2022, excluding patients whose treatment spanned both before and after the DRG timepoint. These patients are all receiving standardized treatment specified by the NTP in designated tuberculosis hospitals. We performed the difference-in-differences (DID) model to investigate 6 primary outcomes. The cost-shifting behaviors were also examined using 4 outpatient and out-of-pocket (OOP) indicators. In the DID model, the baseline period is set from January 2016 to December 2020 before the DRG payment reform, while the treatment period is from January 2021 to December 2022. The payment reform only applied to individuals covered by Wuhan Municipal Medical Insurance, so the treatment group consists of patients insured by this plan, with other patients serving as the control group.
Results
In this study, 279 patients were included in the analysis, their average treatment duration was 692.79 days. We found the DRG payment implementation could effectively reduce the total medical expenditure, total inpatient expenditure, and inpatient expenditure per hospitalization by 28636.03RMB (P < 0.01), 22035.03 RMB (P < 0.01) and 2448.00 RMB (P < 0.05). We also found a reduction in inpatient frequency and inpatient length of stays per hospitalization by 1.32 and 2.63 days with significance. The spillover effects of the DRG payment on outpatient and OOP expenditure were statistically insignificant.
Conclusions
The DRG payment method can effectively control the increase of DR-TB patients’ medical expenditure and improve treatment efficiency with the guarantee of care quality. Furthermore, there was no evidence of spillover effects of DRG payment on outpatient and out-of-pocket expenditures.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12939-024-02368-0.
Keywords: Drug-resistant tuberculosis (DR-TB), Diagnosis-related group (DRG), Difference-in-differences (DID), Medical expenditure, Treatment efficiency
Introduction
Tuberculosis (TB) remains the second leading cause of mortality from a single infectious agent, only behind COVID-19, causing nearly twice as many deaths as HIV/AIDS [1]. Of particular concern is the 410,000 cases of drug-resistant tuberculosis (DR-TB) reported globally in 2022. DR-TB presents limited treatment options and has historically been associated with poor outcomes [2]. This challenges the World Health Organization’s (WHO) End TB Strategy [3]. China faces a significant TB burden [4, 5], with an estimated 748,000 new cases in 2022, making it the third highest among 30 high-burden countries [1], ending TB in China and globally requires robust control strategies [6].
Beyond its impact on health, TB is also directly linked to the Sustainable Development Goal (SDG) of ending poverty [7]. The financial burden faced by patients seeking TB diagnosis and treatment remains a global impediment, with numerous studies indicating that DR-TB patients incur higher medical expenditures compared to those with drug-susceptible TB, placing a heavier financial burden on them [8, 9], especially in developing countries [10–13]. This disproportionately affects economically and socially disadvantaged individuals [14, 15]. The high economic burden can hinder access and adherence to treatment, negatively impact health outcomes, and ultimately increase the risk of disease transmission [16, 17]. Consequently, the End TB approach must incorporate socioeconomic support and cost-reduction initiatives, such as financing, reimbursement, and payment methods [18–20]. The Diagnosis-related group (DRG) payment system, a case group payment scheme classified by medical resource consumption, has been adopted by many countries. By establishing a fixed payment rate for each case, the DRG payment system aims to reduce unnecessary medical services by altering provider incentives. China plans to implement DRG nationwide to replace fee-for-service (FFS) by 2024 after piloting in 30 cities in 2019.
Theoretically, the DRG payment system has the potential to incentivize healthcare providers to control expenditure and increase treatment efficiency by reducing unnecessary health service utilization [16, 21–23]. However, since DRG payment system applies only to inpatient care, some researchers have suggested that DRG may lead to a shift in the delivery of care towards less expensive settings [24], such as transfer of inpatients to unnecessary outpatient services to reduce incurred inpatient expenditures [25–27]. Moreover, many studies have shown that under DRG payment, issues such as fragmented hospitalizations and increased readmission rates may arise [28–30]. Some research have also found the negative impact of the DRG payment method on quality [31–33].
There are some unaddressed issues. First, research on the implications of the medical insurance payment methods for TB patients is limited. Previous studies were focused on financing and medical security [17, 34–38]. Second, no studies investigated the effect of the recently implemented DRG payment methods on TB patients, only some studies examined the implementation of case-based payment during the early phase of the program. Studies on combining increased reimbursement rates with case-based payment showed improved equity in TB service accessibility but increased inequality in out-of-pocket (OOP) [39, 40]cost. Outpatient costs also rose significantly with case-based payment [41]. A capitation reform for TB patients with a full period of treatment led to a notable reduction in medical expenses [42]. Third, the causal inference of impact of the DRG payment model on medical expenditure and treatment efficiency among TB patients remains unclear, these innovative payment methods have only been piloted on a small scale with a relatively short implementation period. Finally, the current understanding of the spillover effects of DRG payment on TB patients remains unclear.
In this study, we applied a quasi-experimental approach, difference-in-difference (DID) design, to investigate the impact of DRG payment reform on the medical expenditure and treatment efficiency of DR-TB patients with a full period of treatment. Additionally, we also investigated the spillover effect of DRG payment reform on outpatient costs, service utilization, and OOP expenditures, which could be potentially incentivized by DRG reform.
Methods
Study site
This study selected Wuhan as the study site, which is a city situated in the central region that could be a representative city in China. Wuhan formally implemented the DRG payment scheme in January 2021, the payment reform was only applicable to individuals covered by the Wuhan Municipal Medical insurance, while other patients were still paid under the FFS scheme.
Study design
In this retrospective study, we used the DID analysis to investigate the changes in medical expenditure and treatment efficiency after the implementation of the DRG payment. The baseline period is from January 2016 to December 2020, before the DRG payment reform. And the treatment period is from January 2021 to December 2022. According to the DRG policy, in the DID model, the treatment group includes patients insured by Wuhan municipal medical insurance, while the control group includes other patients not insured by Wuhan municipal medical insurance [43, 44]. In our study, the study population is the DR-TB patients with a full period of treatment.
Data sources and sample selection
Wuhan Pulmonary Hospital serves as the sole treatment center for DR-TB in the city. In this study, we used data from the digitized Hospital Information System (HIS) of Wuhan Pulmonary Hospital and the TB Information Management System (TBIMS) spanning 2016 to 2022, encompassing 1303 DR-TB patients. These patients all received standardized treatment specified by the National TB Program (NTP) in Wuhan Pulmonary Hospital, the initial regimen usually lasts 24 months, and some patients take short-term chemotherapy regimens of 6 to 12 months. With this data source, this article only evaluates direct medical expenditure.
Patients completing the full treatment course during this period were selected. Exclusions were made for those with treatment outcomes categorized as “refusal” or “interruption” which could underestimate medical expenditure and treatment efficiency. According to WHO guidelines, both “cured” and “treatment completed” are considered successful outcomes for DR-TB treatment [45]. Hence, DR-TB patients with a full period of treatment in our study were defined as those whose treatment initiation and completion fell between 2016 and 2022, and whose treatment outcome was “cured” or “treatment completed”, excluding patients whose treatment spanned both before and after the DRG timepoint.
The reasons for selecting DR-TB patients with a full period of treatment was from the following aspects. First, while previous articles on the impact of the DRG payment system have indicated positive effects on costs and efficiency, many studies have shown that under DRG payment, issues such as fragmented hospitalizations and increased readmission rates may arise [28–30]. Moreover, compared to other diseases, DR-TB has a longer course and requires multiple hospitalizations. Since the DRG payment method only sets payment caps for single hospitalizations, healthcare institutions may increase the number of hospitalizations or extend treatment duration to gain more revenue. Therefore, the impact of the DRG payment method on the medical expenditure and treatment efficiency of DR-TB during the full period of treatment is highly significant.
Additionally, prior research indicates that the DRG payment may negatively affect service quality [31–33]. Thus, although this study focuses on medical expenditure and treatment efficiency, we are also concerned about whether the DRG payment method negatively affects service quality, specifically the treatment outcomes of DR-TB patients. Therefore, we selected only those DR-TB patients who successfully completed the full treatment course, ensuring that our study results are of high quality.
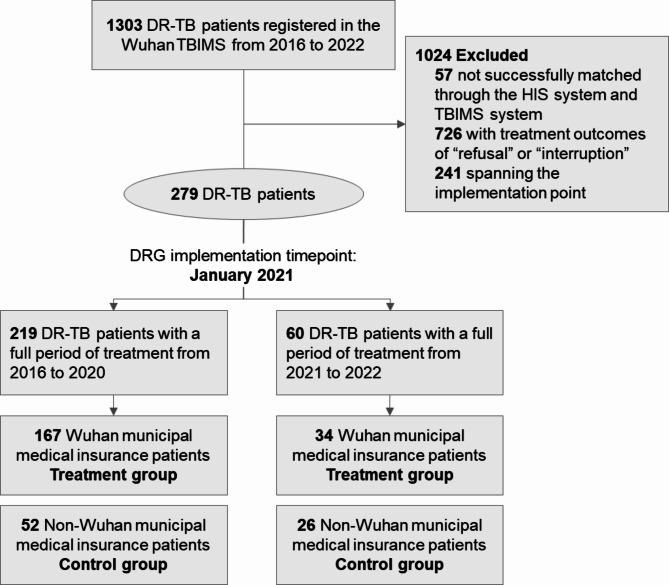
A total of 1303 DR-TB patients were registered at TBIMS in Wuhan. The study refined the cohort by excluding mismatches between HIS and TBIMS records and patients who did not complete treatment. Patients spanning the implementation point were excluded, resulting in a final sample of 279 patients (219 from 2016 to 2020, 60 from 2021 to 2022). The full process of sample selection is specified in Fig. 1.
Fig. 1.
Sample selection
Since each DR-TB patient with a full period of treatment has multiple outpatient and inpatient experiences, we integrated a summary database, included 279 patients’ demographic information, total medical expenditure, total inpatient expenditure, total outpatient expenditure, inpatient frequency, outpatient frequency, and treatment duration. Two separate databases for inpatient and outpatient records were integrated to analyze the impact of DRG payment on the inpatient expenditure, outpatient expenditure, and inpatient length of stay (LOS) on the case-level to supplement the main results, totaling 751 inpatient admissions and 6553 outpatient visits.
Variables
To assess the impact of DRG payment on medical expenditure, we selected three dependent variables from the database: total medical expenditure per patient, total inpatient expenditure per patient, and inpatient expenditure per hospitalization. Adjustments for inflation to 2016 were made using Wuhan’s annual consumer price index. Treatment efficiency was evaluated through three additional dependent variables: inpatient frequency, treatment duration, and inpatient LOS per hospitalization. We also analyzed total outpatient expenditure per patient, outpatient visit frequency, outpatient expenditure per visit, and total inpatient OOP expenditure per patient to examine potential spillover effects of DRG payment on outpatient and OOP expenditure. The independent variable was DRG payment implementation, represented by a dummy variable indicating whether the patient is in the DRG payment scheme. Control variables included age, sex, marriage status, living area, occupation, drug resistance type, and the Charlson Comorbidity Index (CCI) selected based on the behavior model of health service utilization [46–48]. Definitions for all the variables are detailed in eTable 1 (supplementary materials).
Statistical analyses
We used the DID model to evaluate the effect of the DRG payment on inpatient expenditure and treatment efficiency among DR-TB patients with a full period of treatment. The model is as follows:
 |
The dependent variable  denotes the outcome variables of patient i receiving treatment in year t. In this DID model, the key explanatory variable is
denotes the outcome variables of patient i receiving treatment in year t. In this DID model, the key explanatory variable is  , which denotes a dummy variable for the status of DRG implementation in Wuhan. It equals one if a patient from the treatment group and the time of discharge is after January 2021, otherwise, it equals zero. The coefficient
, which denotes a dummy variable for the status of DRG implementation in Wuhan. It equals one if a patient from the treatment group and the time of discharge is after January 2021, otherwise, it equals zero. The coefficient  is the core coefficient concerned in this study, which represents the average treatment effect of the DRG on a series of outcome variables.
is the core coefficient concerned in this study, which represents the average treatment effect of the DRG on a series of outcome variables.  is a set of covariates, which are mentioned in the variables sector, and
is a set of covariates, which are mentioned in the variables sector, and  is a random error term.
is a random error term.
We further performed validity tests and robustness checks to examine the reliability and sensitivity of our analytical results. First, the prerequisite for the application of DID is that the outcome variables of the treatment group and control group have a similar time trend before the DRG payment implementation. So, we applied an event study to check the common trend assumption, we added interactions between indicators for months relative to the DRG payment implementation and an indicator of treatment group instead of using the DRG payment implementation status in the model. The second concern on the validity of the results is that the DRG payment may have spillover effects on outpatient expenditure or OOP expenditure. Thus, we chose four variables in the database, total outpatient expenditure per patient, outpatient expenditure per visit, outpatient frequency, and total inpatient OOP expenditure per patient. We examined the impacts of the DRG payment on these variables to test whether the spillover effects exist.
We conducted two robustness checks. First, to mitigate selection bias and ensure comparability between treatment and control groups [49], we employed propensity score matching (PSM) combined with DID, following prior research [50, 51]. Control variables were used in logit regression to weight the propensity scores, reflecting the likelihood of a sample being in the treatment group. Nearest-neighbor matching was then used to select a comparable control group. After matching, propensity score distributions and kernel density curves (eFigure 1) demonstrated improved similarity between groups. We subsequently performed PSM-DID analysis under common support conditions to validate our DID findings. Second, acknowledging potential COVID-19 confounding effects during our study period in Wuhan [52–54], we excluded data from the pandemic’s peak (December 2019 to May 2020). We then re-assessed the impacts of DRG payment on medical expenditure and treatment efficiency among eligible patients.
Results
Overview of study
The final sample consisted of 279 DR-TB patients with full period treatment. Table 1 presents the summary statistics for patients from the treatment and control group. The number of patients in the treatment group and control group before and after the DRG payment implementation was 167, 52, 34 and 26, respectively.
Table 1.
Descriptive statistics of variables on patient-level
| Variables | Before DRG | After DRG | ||
|---|---|---|---|---|
| Treatment | Control | Treatment | Control | |
| Patient characteristics | ||||
| Observations, No. | 167 | 52 | 34 | 26 |
| Age, mean (SD) | 47.10 (14.39) | 44.27 (12.73) | 45.41 (17.59) |
41.15 (16.14) |
| Sex, No. (%) | ||||
| Male | 107 (64.07) | 28 (53.85) | 20 (58.82) | 15 (57.69) |
| Female | 60 (35.93) | 24 (46.15) | 14 (41.18) | 11 (42.31) |
| Marriage status, No. (%) | ||||
| Unmarried | 22 (13.17) | 3 (5.77) | 7 (20.59) | 6 (23.08) |
| Married | 126 (75.45) | 40 (76.92) | 26 (76.47) | 18 (69.23) |
| Divorced, widowed | 19 (11.38) | 9 (17.31) | 1 (2.94) | 2 (7.69) |
| Living area, No. (%) | ||||
| Inside Wuhan | 163 (97.60) | 13 (25.00) | 33 (97.06) | 9 (34.62) |
| Outside Wuhan | 4 (2.40) | 39 (75.00) | 1 (2.94) | 17 (65.38) |
| Occupation, No. (%) | ||||
| Students | 7 (4.19) | 1 (1.92) | 1 (2.94) | 3 (11.54) |
| Employed | 23 (13.77) | 2 (3.85) | 19 (55.88) | 19 (73.08) |
| Farmers | 13 (7.78) | 9 (17.31) | 0 (0) | 1 (3.85) |
| Unemployed | 83 (49.70) | 30 (57.69) | 1 (2.94) | 0 (0) |
| Retired | 12 (49.70) | 2 (3.85) | 6 (17.65) | 1 (3.85) |
| Others | 29 (17.37) | 8 (15.38) | 7 (20.59) | 2 (7.69) |
| Drug resistance type, No. (%) | ||||
| HR-TB | 4 (2.40) | 1 (1.92) | 5 (14.71) | 2 (7.69) |
| RR-TB | 5 (2.99) | 9 (17.31) | 12 (35.29) | 12 (46.15) |
| MDR-TB | 158 (94.61) | 42 (80.77) | 17 (50.00) | 12 (46.15) |
| CCI, mean (SD) |
0.36 (0.71) |
0.27 (0.60) |
0.65 (0.98) |
0.77 (1.27) |
| Outcomes | ||||
| Total medical expenditure per patient, mean (SD), RMB | 53381.57 (23940.91) |
49629.35 (38173.51) |
44485.78 (30518.44) | 68365.97 (47601.53) |
| Total inpatient expenditure per patient, mean (SD), RMB |
17682.89 (20316.92) |
34795.14 (39907.91) |
18514.91 (15205.11) |
54682.13 (41976.48) |
| Inpatient frequency, mean (SD) |
2.03 (2.20) |
3.83 (2.77) |
2.26 (1.69) |
5.23 (3.87) |
| Treatment duration per patient, mean (SD), day |
700.74 (116.13) |
667.29 (175.34) |
552.07 (101.35) |
544.51 (116.00) |
| Total outpatient expenditure per patient, mean (SD), RMB | 35698.68 (16631.80) | 14834.20 (12304.35) | 25970.87 (23005.94) | 13683.83 (17497.35) |
| Outpatient frequency, mean (SD) |
29.60 (8.56) |
18.25 (8.71) |
13.32 (7.65) |
7.96 (5.46) |
| Total inpatient OOP expenditure per patient, mean (SD), RMB |
6736.12 (7512.43) |
24334.43 (27640.64) |
7139.85 (4916.05) |
27741.28 (20908.67) |
SD Standard deviation; RMB Chinese Yuan; Before the DRG payment implementation: 2016–2020; After the DRG payment implementation: 2021–2022
DRG: Diagnosis-related group; HR-TB: isoniazid resistant tuberculosis; RR-TB: rifampicin resistant tuberculosis; MDR-TB: multiple drug-resistant tuberculosis; CCI: Charlson Comorbidity Index; OOP: Out-of-pocket
Medical expenditures
Table 2 shows the estimated effects of the DRG payment on medical expenditures. Compared with patients reimbursed under the FFS scheme, total medical expenditure was significantly reduced by 28636.03RMB (P < 0.01) in patients reimbursed under the DRG payment scheme after the DRG implementation. And the DRG payment implementation is significantly associated with a decrease in total inpatient expenditure (DID=-22035.03, P < 0.01). Moreover, we used the inpatient database to evaluate the effect of the DRG payment on inpatient expenditure for a single admission. We found the DRG payment implementation could effectively reduce the inpatient expenditure per hospitalization, which could be reduced by 2448.00RMB (P < 0.05) per hospitalization compared with those not insured by Wuhan municipal medical insurance.
Table 2.
Impacts of the DRG payment on medical expenditures among DR-TB patients
| Total medical expenditure per patient | Total inpatient expenditure per patient | Inpatient expenditure per hospitalization | |
|---|---|---|---|
| DID (RMB, Yuan) |
-28636.03*** (9622.04) |
-22035.03*** (8369.80) |
-2448.00** (1202.59) |
| Control variables | YES | YES | YES |
| Observations | 279 | 279 | 751 |
Standard errors are shown in parentheses. The significance levels of 1%, 5%, and 10% are denoted by ***, **, and *, respectively. All regressions controlled individual fixed effects, year fixed effects, and covariates. Covariates include age, sex, marriage status, living area, occupation, drug resistance type, and CCI
DRG: Diagnosis-related group; DID: difference-in-differences; DR-TB: drug-resistant tuberculosis
Treatment efficiency
Table 3 presents the estimated results for the treatment efficiency. The results show that after the DRG payment implementation, the inpatient frequency of full period treatment was significantly decreased by 1.32. We also found a reduction in treatment duration by 25.84 days, but this effect was statistically insignificant. In addition, the DRG payment implementation could effectively reduce the inpatient LOS per hospitalization, which could be reduced by 2.63 (P < 0.05) days per hospitalization compared with those not insured by Wuhan municipal medical insurance.
Table 3.
Impacts of the DRG payment on treatment efficiency among DR-TB patients
| Inpatient frequency | Inpatient LOS per hospitalization | Treatment duration per patient | |
|---|---|---|---|
| DID |
-1.32* (0.75) |
-2.63 days** (1.06) |
-25.84 days (39.82) |
| Control variables | YES | YES | YES |
| Observations | 279 | 751 | 279 |
Standard errors are shown in parentheses. The significance levels of 5%, and 10% are denoted by **, and *, respectively. All regressions controlled individual fixed effects, year fixed effects, and covariates. Covariates include age, sex, marriage status, living area, occupation, drug resistance type, and CCI
DRG: Diagnosis-related group; DID: difference-in-differences; DR-TB: drug-resistant tuberculosis; LOS: length of stay
Test for spillover effects
We used the patient-level data from the summary database and case-level data from the outpatient database to test whether the DRG payment has spillover effects on outpatient and OOP expenditure. The results are presented in Table 4. All estimates of medical expenditure are statistically insignificant, suggesting no evidence of spillover effects on outpatient and OOP expenditures. Furthermore, we found a reduction in outpatient visit frequency by 4.31 with significance, which suggested that the DRG payment may improve the efficiency of outpatient treatment to some extent.
Table 4.
Testing spillover effects of the DRG payment on outpatient and OOP expenditure
| Total outpatient expenditure per patient | Outpatient expenditure per visit | Outpatient frequency |
Total inpatient OOP expenditure | |
|---|---|---|---|---|
| DID |
-6601.00 (5119.17) |
-199.35 (210.58) |
-4.31* (2.45) |
-3980.10 (4577.85) |
| Control variables | YES | YES | YES | YES |
| Observations | 279 | 6553 | 279 | 279 |
Standard errors are shown in parentheses. The significance levels of 10% are denoted by *. All regressions control for individual fixed effects, year fixed effects, and covariates. Covariates include age, sex, marriage status, living area, occupation, drug resistance type, and CCI
DRG: Diagnosis-related group; DID: difference-in-differences; DR-TB: drug-resistant tuberculosis; OOP: out-of-pocket
Tests for pre-trends
As it was mentioned before, we chose the variables of inpatient expenditure per hospitalization and inpatient LOS in the inpatient database to examine the pre-trends with the event study framework. eFigure 2 reports the results of the tests for pre-trends. The results show that no pre-existing differential change in outcomes between the treatment and control group, which suggests the estimated effects are not attributable to a continuation of pre-existing trends. These pieces of evidence reinforce our findings that the DRG payment is responsible for the changes in medical expenditure and treatment efficiency per hospitalization.
Robustness checks
eTable 2 in supplementary materials reports the results of PSM-DID, the effect of the DRG payment on medical expenditure and treatment efficiency after matching is similar to the results before matching. As expected, the results show that total medical expenditure and total inpatient expenditure were significantly reduced by 23688.42RMB and 18877.39RMB, respectively. We also found a reduction in inpatient frequency and treatment duration by 1.12 and 38.60 days, respectively, but the negative effect was statistically insignificant. eTable 3 and eTable 4 in supplementary materials show the results of the impacts of the DRG payment on medical expenditure and treatment efficiency excluding the potential confounding effect of COVID-19. The results are almost consistent with the main results. The results of the robustness check suggested the reliability and sensitivity of the main analysis results.
Discussion
The present study investigated the impact of the DRG payment reform, implemented by the Chinese government in 2021, on medical expenditure and treatment efficiency among DR-TB patients who completed a full course of treatment. The findings revealed that the implementation of this policy was associated with significant reductions in total medical expenditure, total inpatient expenditure, and inpatient expenditure per hospitalization. Moreover, the policy implementation led to substantial decreases in both inpatient frequency and LOS. The implementation of this policy was not found to be associated with adverse consequences, such as cost shifting to outpatient or OOP expenditure.
The DRG policy aimed to standardize the clinical pathway and control the medical expenditure by improving treatment efficiency. Results reveal its effectiveness in controlling total medical expenditure, total inpatient expenditure and the inpatient expenditure per hospitalization in DR-TB patients, consistent with previous studies [16, 22, 55, 56]. DRG payment establishes payment standards based on disease classification. Institutions can retain surpluses from efficient practices but cover deficits if costs exceed standards. Consequently, institutions strategically manage expenses to increase revenues. Moreover, China has issued documents such as the National Guidelines for Performance Assessment of Tier-III Public Hospitals, and Guidelines for High-Quality Development of Public Hospitals, the inpatient expenditure per hospitalization of public hospitals is included in the regulatory and assessment indicators system, so it has been effectively controlled.
Implementation of DRG has demonstrated a significant decrease of 1.32 inpatient frequencies alongside the reduction in inpatient LOS in DR-TB patients. This trend is noteworthy as DRG is known to reduce only one of them in prior research. A cross-sectional study in Hong Kong, China, has associated the introduction of DRG with shorter hospital stays and increased inpatient rates [29]. Due to DR-TB’s airborne nature and transmission risk during hospitalization [57], physicians prioritize treatment efficiency to mitigate transmission risks associated with prolonged stays. Furthermore, Wuhan’s DRG payment scheme emphasizes incentive alignment and constraints on medical insurance payment methods, discouraging unnecessary hospitalizations. Designated institutions must implement internal assessment systems tailored to DRG, standardizing healthcare professionals’ practices.
Previous studies on DRG indicated a cost-minimization behavior by shifting care from inpatient to outpatient or OOP settings. Encouragingly, there were no significant changes in these indicators among DR-TB patients covered by the Wuhan municipal medical insurance after the implementation of DRG, compared to non-Wuhan municipal medical insurance patients. Additionally, outpatient visits have significantly decreased by 4.31, contrary to previous findings [25, 39, 41, 56]. The standardization of outpatient clinical pathways for TB patients has been emphasized worldwide [58]. The Chinese Society for Tuberculosis, Chinese Medical Association released the Chinese expert consensus on multidrug-resistant tuberculosis and Rifampicin-resistant tuberculosis treatment in 2019 [59], based on the WHO’s consolidated guidelines on drug-resistant tuberculosis treatment, which standardizes the diagnostic and treatment pathways for DR-TB. The implementation of case-based payment can make service provision more aligned with clinical pathways [40], thus effectively reduce unnecessary outpatient service utilization and control the individual payments. Additionally, DR-TB has contagious negative externalities compared to other diseases. Under the DRG payment system, the shift of patients to outpatient services increases the likelihood of transmission. Moreover, after the COVID-19 pandemic, the management of respiratory infectious diseases has been further standardized [60], leading to a decrease in the number of outpatient visits for DR-TB patients under the DRG payment system.
To the best of our knowledge, this study is the first to investigate changes in medical expenditure and treatment efficiency among Chinese DR-TB patients following the implementation of DRG payment. Additionally, we examined the spillover effects of DRG payment on TB patients. A further strength of our study is that it includes only patients who completed treatment or were cured, ensuring that all analyses are based on quality-assured data.
Limitations
The study has several limitations. First, only one DRG pilot city in central China was considered as the sample area, there is a lack of horizontal comparative analysis among different pilot regions. Future studies are encouraged to acquire horizon data to extend to a comparative study among different pilot regions. Secondly, the relatively short duration post-reform has resulted in a limited sample size, necessitating further long-term follow-up studies to validate findings conclusively. Thirdly, this study solely investigates changes in total expenditure after the DRG payment reform, details of medical expenditure such as drug expenses and diagnostic expenses need to be explored in future studies. Moreover, this article only evaluates direct medical expenditure, the indirect medical expenditure and indirect medical expenditure were not analyzed because of data cannot be obtained.
Conclusions
The DRG payment reform can effectively control the increase of medical expenditures for DR-TB patients with a full period of treatment, achieved by regulating the inpatient expenditure per hospitalization, and the frequency and duration of inpatient service utilization, without adverse consequences of cost shifting towards outpatient or OOP expenditures. This study provides crucial empirical evidence on the impact of DRG payment on medical expenditures and treatment efficiency for DR-TB, offering valuable insights for China and other countries in providing TB care and implementing payment reform strategies.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We are grateful to Shenglan Tang from Duke University for his valuable comments. We thank Wuhan Pulmonary Hospital for providing historical data in the study. We are also thankful to those who reviewed drafts of this paper.
Abbreviations
- TB
Tuberculosis
- DR-TB
Drug-resistant tuberculosis
- WHO
World Health Organization
- DRG
Diagnosis-related group
- SDG
Sustainable Development Goal
- FFS
Fee-for-service
- NHSA
National Healthcare Security Administration
- OOP
Out-of-pocket
- HIS
Hospital Information System
- TBIMS
TB Information Management System
- NTP
National Tuberculosis Program
- LOS
Length of stay
- DID
Difference-in-differences
- PSM
Propensity score matching
- CCI
Charlson Comorbidity Index
- HR-TB
Isoniazid resistant tuberculosis
- RR-TB
Rifampicin resistant tuberculosis
- MDR-TB
Multiple drug-resistant tuberculosis
Author contributions
Yuehua Li had full access to all the data in the study. Xiong and Yao contributed equally to this work. Concept and design: All authors.Acquisition, analysis, or interpretation of data: Yuehua Li, Xiong, Yao.Drafting of the manuscript: Xiong, Yao.Critical revision of the manuscript for important intellectual content: Chen, Yunfei Li.Statistical analysis: Xiong, Yao.Obtained funding: Xiang, Lin.
Funding
This research was supported by the National Natural Science Foundation of China (grant 72174068 to L.X.) and the Fundamental Research Funds for the Central Universities (NO. YCJJ20242228).
Data availability
The data that support the findings of this study are available from HIS and TBIMS of Wuhan Pulmonary Hospital but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the corresponding author upon reasonable request and with permission of Wuhan Pulmonary Hospital.
Declarations
Ethics approval and consent to participate
Research involving human data has been performed in accordance with the Declaration of Helsinki. All methods were carried out in accordance with relevant guidelines and regulations in the declaration. The study was approved by the institutional review board at each participating site and by the biomedical ethics review committee of Huazhong University of Science and Technology (S170. June 30, 2021). The need for informed consent was waived by the ethics institutional review board of Huazhong University of Science and Technology because of the retrospective nature of the study. All authors confirm that this research caused no harm (physical or mental) to any participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that there were no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yingbei Xiong and Yifan Yao contributed equally to this work.
References
- 1.Global tuberculosis report 2023. Geneva: World Health Organization; 2023.
- 2.Conradie F, Diacon AH, Ngubane N, Howell P, Everitt D, Crook AM, et al. Treatment of highly drug-resistant pulmonary tuberculosis. N Engl J Med. 2020;382(10):893–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mirzayev F, Viney K, Linh NN, Gonzalez-Angulo L, Gegia M, Jaramillo E et al. World Health Organization recommendations on the treatment of drug-resistant tuberculosis, 2020 update. Eur Respir J 2021;57(6). [DOI] [PMC free article] [PubMed]
- 4.Li T, Zhang B, Du X, Pei S, Jia Z, Zhao Y. Recurrent pulmonary tuberculosis in China, 2005 to 2021. JAMA Netw Open. 2024;7(8):e2427266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jiang H, Liu M, Zhang Y, Yin J, Li Z, Zhu C, et al. Changes in incidence and epidemiological characteristics of Pulmonary Tuberculosis in Mainland China, 2005–2016. JAMA Netw Open. 2021;4(4):e215302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feng Q, Zhang G, Chen L, Wu H, Yang Y, Gao Q, et al. Roadmap for ending TB in China by 2035: the challenges and strategies. Biosci Trends. 2024;18(1):11–20. [DOI] [PubMed] [Google Scholar]
- 7.Carter DJ, Glaziou P, Lonnroth K, Siroka A, Floyd K, Weil D, et al. The impact of social protection and poverty elimination on global tuberculosis incidence: a statistical modelling analysis of sustainable development goal 1. Lancet Glob Health. 2018;6(5):E514–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Portnoy A, Yamanaka T, Nguhiu P, Nishikiori N, Garcia Baena I, Floyd K, et al. Costs incurred by people receiving tuberculosis treatment in low-income and middle-income countries: a meta-regression analysis. Lancet Glob Health. 2023;11(10):e1640–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Menzies NA, Allwood BW, Dean AS, Dodd PJ, Houben RMGJ, James LP, et al. Global burden of disease due to rifampicin-resistant tuberculosis: a mathematical modeling analysis. Nat Commun. 2023;14(1):6182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oga-Omenka C, Tseja-Akinrin A, Sen P, Mac-Seing M, Agbaje A, Menzies D, et al. Factors influencing diagnosis and treatment initiation for multidrug-resistant/rifampicin-resistant tuberculosis in six sub-saharan African countries: a mixed-methods systematic review. BMJ Global Health. 2020;5(7):e002280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muttamba W, Tumwebaze R, Mugenyi L, Batte C, Sekibira R, Nkolo A, et al. Households experiencing catastrophic costs due to tuberculosis in Uganda: magnitude and cost drivers. BMC Public Health. 2020;20(1):1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kilale AM, Pantoja A, Jani B, Range N, Ngowi BJ, Makasi C, et al. Economic burden of tuberculosis in Tanzania: a national survey of costs faced by tuberculosis-affected households. BMC Public Health. 2022;22(1):600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaswa M, Minga G, Nkiere N, Mingiedi B, Eloko G, Nguhiu P, et al. The economic burden of TB-affected households in DR Congo. int j Tuberc lung dis. 2021;25(11):923–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Assebe LF, Negussie EK, Jbaily A, Tolla MTT, Johansson KA. Financial burden of HIV and TB among patients in Ethiopia: a cross-sectional survey. BMJ Open. 2020;10(6):e036892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li H, Cheng B, Chen Y. What causes high costs for rural tuberculosis inpatients? Evidence from five counties in China. BMC Infect Dis. 2020;20(1):501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang Y, Chen Y, Wang J, Lao Y. The impacts of medical insurance payment methods on medical bills and medical service quality: evidence from Xiangtan, China. J Bus Res. 2023;169:114292. [Google Scholar]
- 17.Liu X, Lin KH, Li YH, Jiang JN, Zhong ZD, Xiong YB, et al. Impacts of Medical Security Level on Treatment outcomes of Drug-resistant tuberculosis: evidence from Wuhan City, China. Patient Prefer Adherence. 2022;16:3341–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carter DJ, Daniel R, Torrens AW, Sanchez MN, Maciel ELN, Bartholomay P, et al. The impact of a cash transfer programme on tuberculosis treatment success rate: a quasi-experimental study in Brazil. BMJ Global Health. 2019;4(1):e001029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duran D, Bauhoff S, Berman P, Gaudet T, Konan C, Ozaltin E, et al. The role of health system context in the design and implementation of performance-based financing: evidence from Cote d’Ivoire. BMJ Global Health. 2020;5(9):e002934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghazy RM, El Saeh HM, Abdulaziz S, Hammouda EA, Elzorkany AM, Khidr H, et al. A systematic review and meta-analysis of the catastrophic costs incurred by tuberculosis patients. Sci Rep. 2022;12(1):558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meng Z, Hui W, Cai Y, Liu J, Wu H. The effects of DRGs-based payment compared with cost-based payment on inpatient healthcare utilization: a systematic review and meta-analysis. Health Policy. 2020;124(4):359–67. [DOI] [PubMed] [Google Scholar]
- 22.Ma W, Qu J, Han H, Jiang Z, Chen T, Lu X, et al. Statistical insight into China’s indigenous diagnosis-related-Group System Evolution. Healthcare. 2023;11(22):2965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Qiao D, Zhang Y, Rehman A, ur, Khosravi MR. Big Data-enabled analysis of DRGs-Based payment on stroke patients in Jiaozuo, China. J Healthc Eng. 2020;2020:e6690019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Milstein R, Schreyögg J. The end of an era? Activity-based funding based on diagnosis-related groups: a review of payment reforms in the inpatient sector in 10 high-income countries. Health Policy. 2024;141:104990. [DOI] [PubMed] [Google Scholar]
- 25.Kim TH, Park EC, Jang SI, Jang SY, Lee SA, Choi JW. Effects of diagnosis-related group payment system on appendectomy outcomes. J Surg Res. 2016;206(2):347–54. [DOI] [PubMed] [Google Scholar]
- 26.Kim SJ, Han K, Kim W, Kim SJ, Park E. Early impact on outpatients of mandatory adoption of the diagnosis-related Group‐based reimbursement system in Korea on Use of Outpatient Care: differences in medical utilization and Presurgery Examination. Health Serv Res. 2018;53(4):2064–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee C, Kim JM, Kim YS, Shin E. The effect of diagnosis-related groups on the Shift of Medical Services from Inpatient to Outpatient settings: a National claims-based analysis. Asia-Pac J Public Health. 2019;31(6):499–509. [DOI] [PubMed] [Google Scholar]
- 28.Kutz A, Gut L, Ebrahimi F, Wagner U, Schuetz P, Mueller B. Association of the Swiss diagnosis-related group reimbursement system with length of Stay, Mortality, and Readmission Rates in Hospitalized Adult patients. JAMA Netw Open. 2019;2(2):e188332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu Y, Fung H, Shum HM, Zhao S, Wong ELY, Chong KC, et al. Evaluation of length of Stay, Care volume, In-Hospital mortality, and Emergency Readmission Rate Associated with Use of diagnosis-related groups for Internal Resource Allocation in Public Hospitals in Hong Kong. JAMA Netw Open. 2022;5(2):e2145685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chang WF, Yan XY, Ling H, Liu T, Luo AJ. A study of the types and manifestations of physicians’ unintended behaviors in the DRG payment system. Front Public Health. 2023;11:1141981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peng LN, Chou YJ, Chen LK, Huang N. Post-acute Use of opioids and psychotropics in patients after hip fracture: unintended consequences of implementing diagnosis-related grouping payment. J Nutr Health Aging. 2020;24(7):745–51. [DOI] [PubMed] [Google Scholar]
- 32.Jian W, Lu M, Liu G, Chan KY, Poon AN. Beijing’s diagnosis-related group payment reform pilot: impact on quality of acute myocardial infarction care. Soc Sci Med. 2019;243:112590. [DOI] [PubMed] [Google Scholar]
- 33.Jeon MJ, Choo SP, Kwak YH, Kim DW, Kim EH. The effect of diagnosis-related group payment system on the quality of medical care for pelvic organ prolapse in Korean tertiary hospitals. PLoS ONE. 2019;14(8):e0220895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Long Q, Jiang WX, Zhang H, Cheng J, Tang SL, Wang WB. Multi-source financing for tuberculosis treatment in China: key issues and challenges. Infect Dis Poverty. 2021;10(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pan Y, Chen S, Chen M, Zhang P, Long Q, Xiang L, et al. Disparity in reimbursement for tuberculosis care among different health insurance schemes: evidence from three counties in central China. Infect Dis Poverty. 2016;5(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhou C, Long Q, Chen J, Xiang L, Li Q, Tang S, et al. The effect of NCMS on catastrophic health expenditure and impoverishment from Tuberculosis care in China. Int J Equity Health. 2016;15(1):172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jia X, Chen J, Zhang S, Dai B, Long Q, Tang S. Implementing a free tuberculosis (TB) care policy under the integrated model in Jiangsu, China: practices and costs in the real world. Infect Dis Poverty. 2016;5(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xiang L, Pan Y, Hou S, Zhang H, Sato KD, Li Q, et al. The impact of the new cooperative medical scheme on financial burden of tuberculosis patients: evidence from six counties in China. Infect Dis Poverty. 2016;5:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jiang WX, Long Q, Lucas H, Dong D, Chen JY, Xiang L, et al. Impact of an innovative financing and payment model on tuberculosis patients’ financial burden: is Tuberculosis care more affordable for the poor? Infect Dis Poverty. 2019;8(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dong D, Jiang WX, Long Q, Huang F, Zhang H, Chen JY, et al. Impact of an innovative tuberculosis financing and payment model on health service utilization by Tuberculosis patients in China: do the poor fare better than the rich? Infect Dis Poverty. 2019;8(1):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang XX, Chen JY, Jiang H, Zhu AN, Long Q, Ji JS. Utilization and expenses of outpatient services among tuberculosis patients in three Chinese counties: an observational comparison study. Infect Dis Poverty. 2019;8(1):79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hu XY, Gao GY. Evaluation of the effect of the capitation compensation mechanism among pulmonary tuberculosis patients with a full period of treatment. Infect Dis Poverty. 2021;10(1):78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lai Y, Fu H, Li L, Yip W. Hospital response to a case-based payment scheme under regional global budget: the case of Guangzhou in China. Soc Sci Med. 2022;292:114601. [DOI] [PubMed] [Google Scholar]
- 44.Zhang L, Sha W, Lin Q, Fang Y. Can single disease payment impact hospitalization expenses and quality in district hospital? A case study in Fujian, China. Int J Equity Health. 2024;23(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wen S, Yin J, Sun Q. Impacts of social support on the treatment outcomes of drug-resistant tuberculosis: a systematic review and meta-analysis. BMJ Open. 2020;10(10):e036985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Andersen RM. National Health Surveys and the behavioral model of Health services Use. Med Care. 2008;46(7):647. [DOI] [PubMed] [Google Scholar]
- 47.Wolinsky FD, Johnson RJ. The Use of Health services by older adults. J Gerontol. 1991;46(6):S345–57. [DOI] [PubMed] [Google Scholar]
- 48.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. [DOI] [PubMed] [Google Scholar]
- 49.Becker SO, Ichino A. Estimation of Average Treatment effects based on propensity scores. Stata J. 2002;2(4):358–77. [Google Scholar]
- 50.Qian M, Zhang X, Chen Y, Xu S, Ying X. The pilot of a new patient classification-based payment system in China: the impact on costs, length of stay and quality. Soc Sci Med. 2021;289:114415. [DOI] [PubMed] [Google Scholar]
- 51.Boeckerman P, Ilmakunnas P. Unemployment and self-assessed health: evidence from Panel Data. Health Econ. 2009;18(2):161–79. [DOI] [PubMed] [Google Scholar]
- 52.Li Q, Wang L, Wang B, Lu H. The COVID-19-designated hospitals in China: preparing for public health emergencies. Emerg Microbes Infect. 2021;10(1):998–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sun S, Xie Z, Yu K, Jiang B, Zheng S, Pan X. COVID-19 and healthcare system in China: challenges and progression for a sustainable future. Global Health. 2021;17(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhang X, Tang S, Wang R, Qian M, Ying X, Maciejewski ML. Hospital response to a new case-based payment system in China: the patient selection effect. Health Policy Plann. 2024;39(5):519–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jian W, Lu M, Chan KY, Poon AN, Han W, Hu M, et al. The impact of a pilot reform on the diagnosis-related-groups payment system in China: a difference-in-difference study. Lancet. 2015;386:S26. [Google Scholar]
- 56.Zhang T, Lu B, Yan Z, Huang X, Lu W. Impacts of a New Episode-based payment Scheme on volume, expenditures, and Efficiency in Public hospitals: a quasi-experimental interrupted time-series study in Jinhua. China RMHP. 2022;15:1659–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Edlin Brian R, Tokars Jerome I, Grieco Michael H, Crawford Jack T, Julie W, Emelia S. An outbreak of Multidrug-resistant tuberculosis among hospitalized patients with the Acquired Immunodeficiency Syndrome. N Engl J Med. 1992;326(23):1514–21. [DOI] [PubMed] [Google Scholar]
- 58.Brown RE, Miller B, Taylor WR, Palmer C, Bosco L, Nicola RM, et al. Health-Care expenditures for tuberculosis in the United States. Arch Intern Med. 1995;155(15):1595–600. [PubMed] [Google Scholar]
- 59.[Chinese expert consensus on multidrug-resistant tuberculosis and Rifampicin-resistant tuberculosis treatment]. Zhonghua Jie He He Hu Xi Za Zhi. 2019;42(10):733–49. [DOI] [PubMed] [Google Scholar]
- 60.Kant S, Tyagi R. The impact of COVID-19 on tuberculosis: challenges and opportunities. Therapeutic Adv Infect Disease. 2021;8:20499361211016973. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from HIS and TBIMS of Wuhan Pulmonary Hospital but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the corresponding author upon reasonable request and with permission of Wuhan Pulmonary Hospital.