Abstract
Background
A scarcity of data exists concerning atrial fibrillation (AF) during the perioperative stage of non-cardiothoracic surgery, particularly orthopedic surgery. In addition, given the frequency and significant impact of AF in the perioperative period, therefore our aim was to identify prognosis and predictors of elderly hip fracture patients with perioperative AF.
Methods
An examination of hip fracture patients at the Third Hospital of Hebei Medical University, who had been hospitalized from January 2018 to October 2020 in succession, was conducted retrospectively. To determine independent risk factors for paroxysmal AF in elderly hip fracture patients, univariate and multivariate logistic regression analysis were employed. The Kaplan–Meier survival curve demonstrated the correlation between all-cause mortality in the non-AF, paroxysmal AF, and permanent AF groups. An assessment of the correlation between baseline factors, complications, and all-cause mortality was conducted through univariable and multivariable Cox proportional hazards analysis.
Results
Enrolling 1,376 elderly patients with hip fractures, we found 1,189 in the non-AF group, 103 in the paroxysmal AF group, and 84 in the permanent AF group. Kaplan–Meier survival curves revealed a significantly lower overall survival rate in elderly hip fracture patients with AF, especially permanent AF. Based on COX regression analysis, we found that the main risk factors for all-cause death in elderly hip fracture patients with AF were concomitant pulmonary infection(HR 2.006,95%CI 1.019–3.949, P = 0.044), hyponatremia(HR 2.417,95%CI 1.177–4.961, P = 0.016), permanent AF(HR 2.806, 95%CI 1.036–4.198, P = 0.039). Independent risk factors for perioperative paroxysmal AF in elderly hip fracture patients were hypertension(OR 2.248, 95% CI 1.415–3.571, P = 0.001), COPD(OR 4.694, 95% CI 2.207–9.980, P < 0.001) and ACCI(OR 1.436, 95%CI 1.072–1.924, P = 0.015).
Conclusions
The mortality risk is high in elderly patients with hip fractures combined with AF. The independent risk factors for their death include permanent AF, pulmonary infection and hyponatremia. The independent risk factors for perioperative paroxysmal AF in elderly patients with hip fractures are ACCI, hypertension and COPD. we should identify risk factors and optimize the treatment plan at an early stage.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12877-024-05647-1.
Keywords: Non- atrial fibrillation, Paroxysmal atrial fibrillation, Permanent atrial fibrillation, Hip fracture, Risk factors, Prognosis, Elderly
Introduction
As the population continues to age, the number of people aged 60 and over will reach 2 billion by 2050 [1]. Hip fractures are a common type of fracture in the elderly, the number of which is increasing, and surgery is now the treatment of choice for hip fractures [2, 3]. Atrial fibrillation (AF) is a common perioperative arrhythmia with a prevalence ranging from 2 to 60%, and its prognosis is often unsatisfactory [4–7].
Patients with AF were prone to hip fractures: based on an analysis of a large study, a history of AF was significantly associated with an increased risk of hip fracture, even after adjusting for potential confounders such as age, comorbidities, and medication use [8]. A common perioperative complication in elderly hip fracture patients is AF, and they tended to have a poorer prognosis. Among patients who underwent hip fracture surgery, 1-year mortality and 1-year readmission rates were reported to be higher in those with perioperative AF and higher rates of heart failure, thromboembolism, stroke, and dementia [9–11]. Additionally, hypertension and chronic obstructive pulmonary disease have been identified as other risk factors associated with perioperative AF [12]. It has been shown that the main symptoms of paroxysmal AF diagnosed by the first electrocardiogram were palpitations and chest pain, with a 10-year all-cause mortality rate of 30.3 percent [13–15]. In previous study, those with persistent AF had a higher risk of thrombo-embolic events compared with paroxysmal AF [16].
The prognosis of complications and long-term mortality in patients with hip surgery combined with paroxysmal and permanent AF is currently uncertain. Our aim was to explore the prognosis of paroxysmal and permanent AF and the factors that predict perioperative paroxysmal AF. To provide a basis for the management of elderly hip fracture patients with AF.
Methods
Patients and groups
A retrospective study of hip fracture patients aged 65 or above, who were admitted to Hebei Medical University's Third Hospital from January 2018 to October 2020, was sanctioned by the Institutional Review Board. Furthermore, the Third Hospital granted a waiver for informed consent. Individuals aged 65 years or above, hip fracture, willing to participate voluntarily and had normal communication and understanding skills were included in this study. Conversely, those with pathological fractures, multiple fractures or old fractures, incomplete clinical data and those without surgery were excluded. In compliance with European Society of Cardiology (ESC) guidelines [17], three groups were identified for the study: (1) NAF, (2) paroxysmal AF, (3) permanent AF.
Data collection
Demographic data (age, gender), comorbidities (hypertension, coronary heart disease, diabetes, COPD, cancer, stroke), perioperative complications (pulmonary infection, heart failure, stress ulcer, urinary tract infection, stress hyperglycemia, anemia, acute cerebrovascular disease, hyponatremia, hypokalemia, hypoproteinemia), prognostic index (length of stay, and all-cause mortality), Surgical data (type of hip fracture, anesthesia and surgery) were all collected. The patients were followed up until October 1, 2023, during which time we contacted their relatives by phone to record whether they had died.
Definition
Classifying AF types into paroxysmal and permanent, we followed the European Society of Cardiology's guidelines. Paroxysmal AF was determined to be a self-terminating condition that lasted no longer than 7 days, and our diagnosis of it was mainly based on ECG monitoring and electrocardiogram. Permanent AF, on the other hand, was defined as AF in which cardioversion therapy either failed or was not attempted, we diagnosed permanent AF by asking medical history [17].
Statistical analysis
For continuous variables, normality was evaluated using the Shapiro–Wilk test, Mann–Whitney U test or Student's t test was used to compare differences between groups, recorded in mean and standard deviation (SD) or median and interquartile range. For categorical variables, chi-square test or Fisher's exact test was used to compare differences between groups, and recorded in numbers and percentages. Univariate and multivariate logistic regression analyses were used to determine independent risk factors for paroxysmal AF in elderly hip fracture patients. Kaplan–Meier curves were used to represent mortality in patients with AF. Univariate and multivariate analyses of survival outcomes were performed using Cox proportional risk regression models to identify independent prognostic factors. In addition, subgroup analyses were performed to validate the robustness of the results, and outcomes were stratified according to age and presence of comorbidities. The level of significance was set at P < 0.05. SPSS statistical software (version 25.0) and GraphPad Prism software (version 9.0) were used.
Results
Demographic characteristics
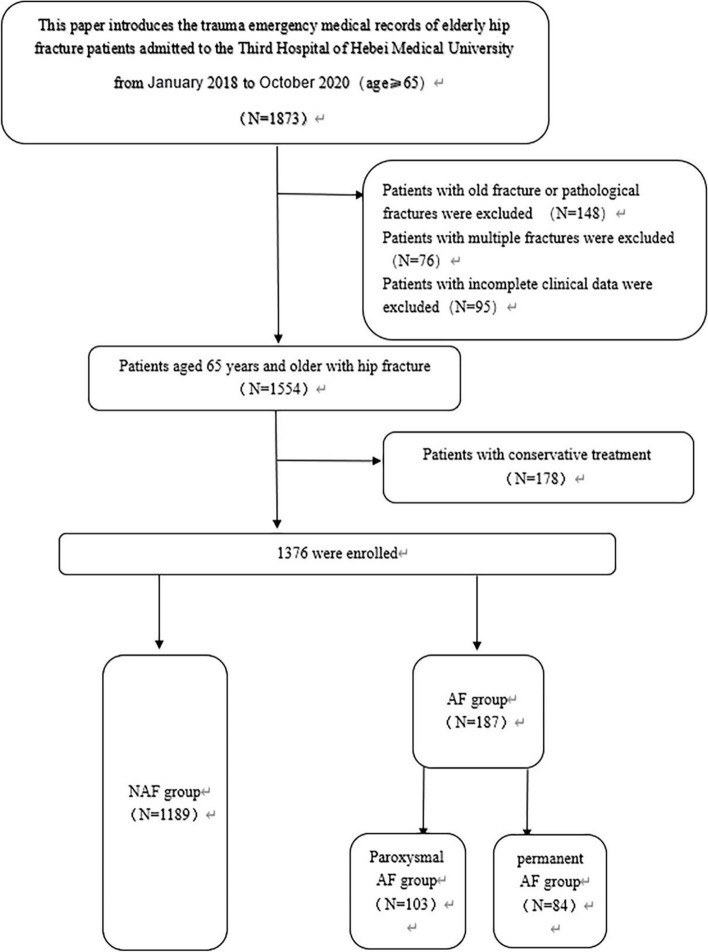
Between January 2018 and October 2020, a total of 1873 patients over the age of 65 years were admitted to our department for hip fracture. Among them, 497 patients were excluded: 148 patients had old fractures or pathological fractures; 76 patients had multiple fractures; and 95 patients had incomplete data; 178 patients received non-surgical treatment. Finally, 1376 cases remained in the analysis, 1189 patients were non-AF, 103 patients were paroxysmal AF and 84 patients were permanent AF. (Fig. 1). Table 1 described the basic characteristics of the patients. Of the patients, 70.3% were female, and the average age was 79.51 years. Hypertension (48.3%) and prior ischemic stroke (39.2%) were the top two comorbidities (Stable1 for more details).
Fig. 1.
The flow diagram of this study
Table 1.
Baseline characteristics of geriatric patients with hip fracture
| Variables | Total (n = 1376) |
NAF (n = 1189) |
AF | (n = 187) |
|---|---|---|---|---|
| Par AF (n = 103) |
Per AF (n = 84) |
|||
| Age, mean ± SD (years) | 79.51 ± 7.346 | 79.29 ± 7.419 | 82.17 ± 6.790 | 79.44 ± 6.335 |
| Age group, n (%) | ||||
| < 75 years | 379 (27.5%) | 344 (28.9%) | 17 (16.5%) | 18 (21.4%) |
| ≥ 75 years | 997 (72.5%) | 845 (71.1%) | 86 (83.5%) | 66 (78.6%) |
| ACCI (IQR) | 5 (4–5) | 5 (4–5) | 6 (4–6) | 5 (4–6) |
| Gender, n (%) | ||||
| Male | 408 (29.7%) | 348 (29.3%) | 36 (35.0%) | 24 (28.6%) |
| Female | 968 (70.3%) | 841 (70.7%) | 67 (65.0%) | 60 (71.4%) |
| Fracture types, n (%) | ||||
| Femoral neck fractures | 648 (47.1%) | 556 (46.8%) | 58 (56.3%) | 34 (40.5%) |
| Intertrochanteric fractures | 728 (52.9%) | 633 (53.2%) | 45 (43.7%) | 50 (59.5%) |
| Comorbidities, n (%) | ||||
| Hypertension | 664 (48.3%) | 538 (45.2%) | 69 (67.0%) | 57 (67.9%) |
| Stroke | 540 (39.2%) | 446 (37.5%) | 49 (47.6%) | 45 (53.6%) |
| Coronary heart disease | 368 (26.7%) | 294 (24.7%) | 47 (45.6%) | 27 (32.1%) |
| Diabetes | 300 (21.8%) | 254 (21.4%) | 18 (17.5%) | 28 (33.3%) |
| COPD | 47 (3.4%) | 28 (2.4%) | 15 (14.6%) | 10 (11.9%) |
| Cancer | 62 (4.5%) | 53 (4.5%) | 5 (4.9%) | 4 (4.8%) |
| Surgical type, n (%) | ||||
| Replacement | 586 (42.6%) | 503 (42.3%) | 52 (50.5%) | 31 (36.9%) |
| Fixation | 790 (57.4%) | 686 (57.7%) | 51 (49.5%) | 53 (63.1%) |
| Anesthesia type, n (%) | ||||
| General | 792 (57.6%) | 686 (57.7%) | 57 (55.3%) | 49 (58.3%) |
| Lumbar | 584 (42.4%) | 503 (42.3%) | 46 (44.7%) | 35 (41.7%) |
Values are presented as mean ± standard deviation, median (interquartile range), or number (percentage) as appropriate
SD Standard deviation, AF Atrial fibrillation, NAF Non atrial fibrillation, Par AF Paroxysmal atrial fibrillation, Per AF Permanent atrial fibrillation, COPD Chronic obstructive pulmonary disease, ACCI Age-Adjusted Charlson Comorbidity Index
Comparison of the prognosis of combined NAF and AF in elderly hip fracture patients
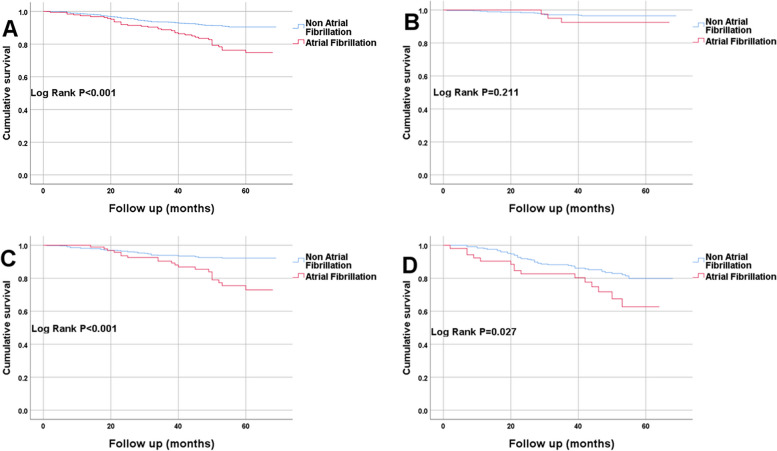
Table 2 described the outcomes for the elderly hip fracture patients (NAF, paroxysmal AF, permanent AF), including complications, length of stay and overall mortality (Stable2 for more details). Table 3 described the outcomes for the elderly hip fracture patients (NAF, AF), including complications, length of stay and overall mortality. In Table 3, the incidence of pulmonary infection, heart failure, stress ulcers, urinary tract infection, acute cerebrovascular disease, hypokalemia, length of stay, and all-cause mortality were significantly higher in AF patients compared to those without AF (P < 0.05). However, there was no significant difference in the anemia, stress hyperglycemia, hypoproteinemia and hyponatremia between the two groups. We also found that anemia and hypoproteinemia were the most common complications in both groups. At the end of the research, the AF cohort had 38 fatalities (20.3%) as demonstrated by the Kaplan–Meier survival curve (Fig. 2A), which was greater (log rank p < 0.001) than the non-AF group (8.7%).
Table 2.
Comparison of the outcomes of patients with non- atrial fibrillation paroxysmal atrial fibrillation and permanent atrial fibrillation in elderly patients with hip fracture
| Variables | Total (n = 1376) |
NAF (n = 1189) |
AF | (n = 187) |
|---|---|---|---|---|
| Par AF (n = 103) |
Per AF (n = 84) |
|||
| Pulmonary infection | 204 (14.8%) | 162 (13.6%) | 21 (20.4%) | 21 (25.0%) |
| Heart failure | 421 (30.6%) | 329 (27.7%) | 44 (42.7%) | 48 (57.1%) |
| Stress ulcer | 25 (1.8%) | 9 (0.8%) | 7 (6.8%) | 9 (10.7%) |
| Urinary tract infection | 49 (3.6%) | 33 (2.8%) | 8 (7.8%) | 8 (9.5%) |
| Anemia | 648 (47.1%) | 553 (46.5%) | 51 (49.5%) | 44 (52.4%) |
| Stress hyperglycemia | 52 (3.8%) | 45 (3.8%) | 3 (2.9%) | 4 (4.8%) |
| Acute cerebrovascular disease | 51 (3.7%) | 16 (1.3%) | 17 (16.5%) | 18 (21.4%) |
| Hyponatremia | 421 (30.6%) | 359 (30.2%) | 38 (36.9%) | 24 (28.6%) |
| Hypokalemia | 325 (23.6%) | 261 (22.0%) | 45 (43.7%) | 19 (22.6%) |
| Hypoalbuminemia | 700 (50.9%) | 606 (51.0%) | 55 (53.4%) | 39 (46.4%) |
| Hospital stay (IQR), days | 12 (10,16) | 12 (10,16) | 13 (10,17) | 13 (11,17) |
| All-cause mortality | 141 (10.3%) | 103 (8.7%) | 13 (13.5%) | 25 (29.8%) |
Values are presented as mean ± standard deviation, median (interquartile range), or number (percentage) as appropriate
AF Atrial fibrillation, NAF Non atrial fibrillation, Par AF Paroxysmal atrial fibrillation, Per AF Permanent atrial fibrillation
Table 3.
Comparison of the outcome of patients with non- atrial fibrillation and atrial fibrillation in old patients with hip fracture
| Variables | Total (n = 1376) |
NAF (n = 1189) |
AF (n = 187) |
P值 |
|---|---|---|---|---|
| Pulmonary infection | 204 (14.8%) | 162 (13.6%) | 42 (22.5%) | 0.002 |
| Heart failure | 421 (30.6%) | 329 (27.7%) | 92 (49.2%) | < 0.001 |
| Stress ulcer | 25 (1.8%) | 9 (0.8%) | 16 (8.6%) | < 0.001 |
| Urinary tract infection | 49 (3.6%) | 33 (2.8%) | 16 (8.6%) | < 0.001 |
| Anemia | 648 (47.1%) | 553 (46.5%) | 95 (50.8%) | 0.274 |
| Stress hyperglycemia | 52 (3.8%) | 45 (3.8%) | 7 (3.7%) | 0.978 |
| Acute cerebrovascular disease | 51 (3.7%) | 16 (1.3%) | 35 (18.7%) | < 0.001 |
| Hyponatremia | 421 (30.6%) | 359 (30.2%) | 62 (33.2%) | 0.414 |
| Hypokalemia | 325 (23.6%) | 261 (22.0%) | 64 (34.2%) | < 0.001 |
| Hypoalbuminemia | 700 (50.9%) | 606 (51.0%) | 94 (50.3%) | 0.859 |
| Hospital stay (IQR), days | 12 (10,16) | 12 (10,16) | 13 (10,17) | 0.010 |
| All-cause mortality | 141 (10.2%) | 103 (8.7%) | 38 (20.3%) | < 0.001 |
Values are presented as mean ± standard deviation, median (interquartile range), or number (percentage) as appropriate
AF Atrial fibrillation, NAF Non atrial fibrillation, Par AF Paroxysmal atrial fibrillation, Per AF Permanent atrial fibrillation
Fig. 2.
The Kaplan–Meier curve for non-atrial fibrillation and atrial fibrillation. A all patients; B Patients aged 65-75 years; C Patients aged 76-85 years; D Patients aged 86-95 years
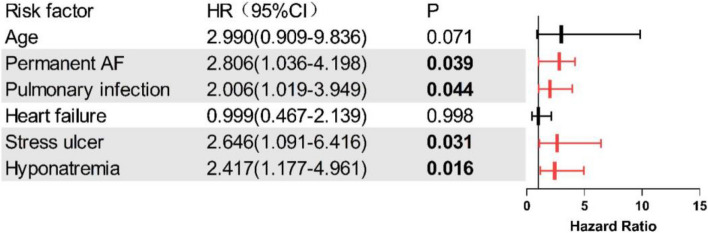
Clinical variables predicting all-cause mortality in patients with AF
Table 4 described the relationship between all-cause mortality and relevant clinical variables in elderly hip fracture patients with AF. Univariate COX analysis showed that age over 75 years, permanent AF, pulmonary infection, stress ulcer, heart failure, and hyponatremia were also associated with all-cause mortality (p < 0.05). The multivariate COX proportional risk model incorporated the factors chosen from the univariate COX regression analysis. Because stress ulcers were rare and occur sporadically, they were not included. Independent risk factors for all-cause mortality in patients identified by multivariate COX proportional risk model, which included permanent AF (HR 2.806, 95%CI 1.036–4.198, P = 0.039), pulmonary infection (HR 2.006,95%CI 1.019–3.949, P = 0.044), hyponatremia (HR 2.417,95%CI 1.177–4.961, P = 0.016). A forest plot was employed to illustrate the risk factors that foretold all-cause mortality in AF patients, as depicted in Fig. 3.
Table 4.
Cox proportional risk regression model for overall survival in patients with atrial fibrillation
| Variables | Univariate HR (95% CI) |
P value | Multivariate HR (95% CI) |
P value |
|---|---|---|---|---|
| Age ≥ 75 | 3.180 (0.997–10.348) | 0.055 | 2.990 (0.909–9.836) | 0.071 |
| Gender | 1.615 (0.764–3.414) | 0.210 | ||
| Fracture types | 1.801 (0.921–3.522) | 0.085 | ||
| Permanent AF | 2.140 (1.093–4.193) | 0.027 | 2.806 (1.036–4.198) | 0.039 |
| Pulmonary infection | 2.495 (1.287–4.835) | 0.007 | 2.006 (1.019–3.949) | 0.044 |
| Heart failure | 2.033 (1.051–3.934) | 0.035 | 0.999 (0.467–2.139) | 0.998 |
| Stress ulcer | 3.238 (1.421–7.380) | 0.005 | 2.646 (1.091–6.416) | 0.031 |
| Urinary tract infection | 0.292 (0.040–2.130) | 0.225 | ||
| Anemia | 1.433 (0.752–2.730) | 0.274 | ||
| Stress hyperglycemia | 1.980 (0.472–8.311) | 0.351 | ||
| Acute cerebrovascular disease | 0.891 (0.372–2.133) | 0.796 | ||
| Surgical type | 1.685 (0.850–3.341) | 0.135 | ||
| Anesthesia type | 0.567 (0.289–1.111) | 0.098 | ||
| Hyponatremia | 2.275 (1.199–4.317) | 0.012 | 2.417 (1.177–4.961) | 0.016 |
| Hypokalemia | 1.483 (0.772–2.848) | 0.236 | ||
| Hypoalbuminemia | 1.473 (0.773–2.807) | 0.239 | ||
| Hospital stay (IQR), days | 0.987 (0.929–1.049) | 0.675 |
Hypokalemia = potassium level < 3.5 mmol/L. Hyponatremia = sodium level < 135 mmol/L, Hypoalbuminemia = albumin level < 35 g/L
Abbreviations: HR Hazard ratio, CI Confidence interval
Fig. 3.
The forest map of risk factors for all-cause mortality in patients with AF
Subgroup analysis
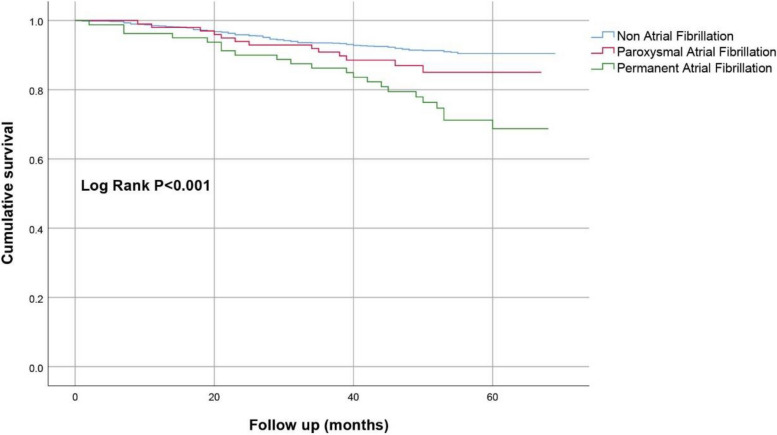
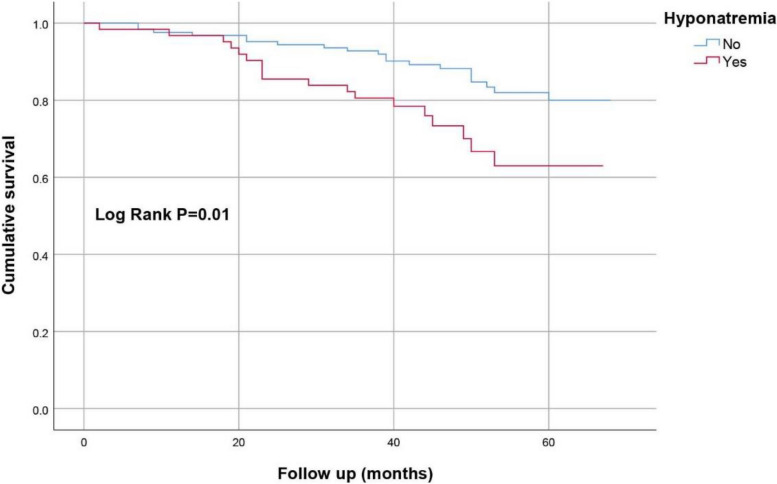
We divided the subjects into three age groups: 65–75 years, 76–85 years, and 86–95 years, we observed that patients with AF consistently exhibited higher mortality rates compared to those non-AF(Fig. 2BCD). Furthermore, fatalities (29.8%) in the permanent AF cohort were higher than those in the paroxysmal AF group and the non-AF group, as demonstrated by the Kaplan–Meier survival curve (Fig. 4) (Log Rank p < 0.001). Elderly hip fracture patients with AF were divided into two groups according to whether they were combined with hyponatremia or not, and the Kaplan–Meier survival curve (Fig. 5) showed that the mortality rate was higher in the combined hyponatremia group than in the non-hyponatremia group (Log Rank p = 0.01). Similarly, according to whether they were combined with pulmonary infection or not, the Kaplan–Meier survival curve (Fig. 6) showed that the mortality rate was higher in the combined pulmonary infection group (Log Rank p = 0.005).
Fig. 4.
The Kaplan–Meier curve for non-atrial fibrillation, paroxysmal atrial fibrillation and permanent atrial fibrillation
Fig. 5.
Kaplan–Meier curve of perioperative hyponatremia in elderly patients with hip fracture and atrial fibrillation
Fig. 6.
Kaplan–Meier curve of perioperative pulmonary infection in elderly patients with hip fracture and atrial fibrillation
Non AF and paroxysmal AF Patient characteristics at baseline
Table 5 summarized the characteristics of patients with NAF and paroxysmal AF hip fractures. Most patients were women (70.3%), and the top four comorbidities were hypertension (47.0%), stroke (38.3%), coronary heart disease (26.4%), and diabetes (21.1%). No distinctions between genders were observed between the groups, yet age was distinct; paroxysmal AF patients were older than NAF patients (82.17 ± 6.790 years for paroxysmal AF, 79.29 ± 7.419 years for NAF, p < 0.001). The burden of chronic diseases, as assessed by the age-adjusted Charlson Comorbidity Index (ACCI), was higher in patients with paroxysmal AF than in those with NAF (6(4–6) versus 5(4–5), p < 0.001). Statistically, a significant distinction was observed between those with a history of hypertension, stroke, COPD, and coronary heart disease (p < 0.05). Despite the fact that those with paroxysmal AF appeared to have a greater prevalence of diabetes and cancer, no noteworthy disparity was discovered. Additionally, age ≥ 75 was found to be significantly higher among patients with paroxysmal AF.
Table 5.
Baseline characteristics of geriatric hip fracture patients with non-atrial fibrillation and paroxysmal atrial fibrillation
| Variables | Total (n = 1292) |
NAF (n = 1189) |
Par AF (n = 103) |
F/t/z | P 值 |
|---|---|---|---|---|---|
| Age, mean ± SD (years) | 79.51 ± 7.409 | 79.29 ± 7.419 | 82.17 ± 6.790 | 3.804 | < 0.001 |
| Age group, n (%) | |||||
| < 75 years | 361 (27.9%) | 344 (28.9%) | 17 (16.5%) | 7.270 | 0.007 |
| ≥ 75 years | 931 (72.1%) | 845 (71.1%) | 86 (83.5%) | ||
| Gender, n (%) | |||||
| Male | 384 (29.7%) | 348 (29.3%) | 36 (35.0%) | 1.466 | 0.226 |
| Female | 908 (70.3%) | 841 (70.7%) | 67 (65.0%) | ||
| ACCI | 5 (4–5) | 5 (4–5) | 6 (4–6) | 7.259 | < 0.001 |
| Fracture types, n (%) | |||||
| Femoral neck fractures | 614 (47.5%) | 556 (46.8%) | 58 (56.3%) | 3.466 | 0.063 |
| Intertrochanteric fractures | 678 (52.5%) | 633 (53.2%) | 45 (43.7%) | ||
| Comorbidities, n (%) | |||||
| Hypertension | 607 (47.0%) | 538 (45.2%) | 69 (67.0%) | 17.989 | < 0.001 |
| Stroke | 495 (38.3%) | 446 (37.5%) | 49 (47.6%) | 4.061 | 0.044 |
| Coronary heart disease | 341 (26.4%) | 294 (24.7%) | 47 (45.6%) | 21.322 | < 0.001 |
| Diabetes | 272 (21.1%) | 254 (21.4%) | 18 (17.5%) | 0.862 | 0.353 |
| COPD | 43 (3.3%) | 28 (2.4%) | 15 (14.6%) | 43.909 | < 0.001 |
| Cancer | 58 (4.5%) | 53 (4.5%) | 5 (4.9%) | 0.035 | 0.852 |
| Surgical type, n (%) | |||||
| Replacement | 555 (43.0%) | 503 (42.3%) | 52 (50.5%) | 2.589 | 0.108 |
| Fixation | 737 (57.0%) | 686 (57.7%) | 51 (49.5%) | ||
| Anesthesia type, n (%) | |||||
| General | 743 (57.5%) | 686 (57.7%) | 57 (55.3%) | 0.215 | 0.643 |
| Lumbar | 549 (42.5%) | 503 (42.3%) | 46 (44.7%) | ||
Values are presented as mean ± standard deviation, median (interquartile range), or number (percentage) as appropriate
SD Standard deviation, AF Atrial fibrillation, NAF Non atrial fibrillation, Par AF Paroxysmal atrial fibrillation, Per AF Permanent atrial fibrillation, COPD Chronic obstructive pulmonary disease, ACCI Age-Adjusted Charlson Comorbidity Index
Clinical variables predicting the appearance of paroxysmal AF
In Table 6, univariate logistic analysis (p < 0.05) revealed a correlation between age, ACCI, combined hypertension, stroke, coronary heart disease, and COPD and paroxysmal AF in elderly patients with hip fracture. To further investigate this association, a multivariate logistic proportional hazards model was then implemented. Elderly patients with hip fracture who have combined hypertension (OR 2.248, 95% CI 1.415–3.571, P = 0.001), COPD (OR 4.694, 95% CI 2.207–9.980, P < 0.001), ACCI (OR 1.436, 95%CI 1.072–1.924, P = 0.015) were at an increased risk for perioperative.
Table 6.
Univariate and multivariate logistic regression analysis for factors associated with perioperative paroxysmal aF in old patients with hip fracture
| Variables | Univariate OR (95% CI) |
P value | Multivariate OR (95% CI) |
P value |
|---|---|---|---|---|
| Age | 1.056 (1.026–1.086) | < 0.001 | 1.031 (0.992–1.071) | 0.125 |
| Gender | 0.770 (0.504–1.177) | 0.227 | ||
| Fracture types | 0.681 (0.454–1.022) | 0.064 | ||
| ACCI | 1.800 (1.522–2.128) | < 0.001 | 1.436 (1.072–1.924) | 0.015 |
| Hypertension | 2.456 (1.603–3.761) | < 0.001 | 2.248 (1.415–3.571) | 0.001 |
| Stroke | 1.512 (1.009–2.264) | 0.045 | 0.844 (0.494–1.442) | 0.535 |
| Coronary heart disease | 2.555 (1.696–3.848) | < 0.001 | 1.305 (0.761–2.236) | 0.333 |
| Diabetes | 0.780 (0.460–1.321) | 0.354 | ||
| COPD | 7.068 (3.640–13.723) | < 0.001 | 4.694 (2.207–9.980) | < 0.001 |
| Cancer | 1.094 (0.427–2.799) | 0.852 | ||
| Surgical type | 0.719 (0.481–1.076) | 0.109 | ||
| Anesthesia type | 1.101 (0.734–1.650) | 0.643 |
N 1292 (cases: 103, controls: 1189)
Abbreviations: OR Odds ratio, CI Confidence interval, COPD Chronic obstructive pulmonary disease, ACCI Age-Adjusted Charlson Comorbidity Index
Discussion
Clinical outcomes
We explored the prognosis of elderly hip fracture patients with AF and the predictors of paroxysmal AF. We found that elderly hip fracture patients with AF had a poor prognosis, which was worse in patients with permanent AF than in patients with paroxysmal AF. Permanent AF, pulmonary infection, and hyponatremia were independent risk factors for death in AF patients. The incidence of hip fracture in elderly patients with paroxysmal AF was linked with ACCI, hypertension, and COPD. These results suggested that people in poorer health were more likely to develop AF and that AF further worsens their health and reduces their survival.
Comparison with other studies
We found a higher mortality rate after hip fracture in patients with AF, and in Sairenchi's study, he found that AF, even in those without other TCVRFs (standard cerebrocardiovascular risk factors), was an independent hazard for prior ischemic stroke and all-cause cardiovascular mortality, the results were similar to our study [6]. The risk of mortality after hip fracture surgery in patients with AF is influenced by multiple factors. We found permanent AF was an independent indicator of mortality in elderly hip fracture patients with AF. The prevailing view is that permanent and persistent AF patients are associated with poorer survival [18, 19]. Amalia Baroutid's study revealed that, at a median follow-up of 31 months (interquartile range 10 to 52 months), 37.3% of patients perished. In comparison to those with paroxysmal AF, permanent AF patients had a higher mortality rate (aHR,1.37; 95% CI,1.08–1.74, P = 0.009), but similar rates of cardiovascular (CV) mortality or hospitalization (aHR,1.09; 95%CI, 0.91–1.31, P = 0.35), This result is in line with our findings. The mechanism, on the one hand, may be the long duration of permanent AF and therefore the high risk of thromboembolic events, on the other hand, patients with permanent AF are usually accompanied by structural and functional changes in the heart, are less able to repair themselves and cope with the risks [20–22]. And it may be associated with a greater likelihood of heart failure. In our study, we found a higher incidence of perioperative heart failure in patients with AF. They are often associated with each other, as AF facilitates HF to occur and vice-versa [23]. AF leading to heart failure may be caused by reduction in cardiac ejection fraction, leading to a reduction in coronary perfusion to the heart, which in turn leads to a reduction in atrial blood supply, resulting in atrial arrhythmias [24–26]. Therefore, heart rate should be controlled and thrombosis should be prevented and it is additionally crucial to enhance perioperative infusion management in these patients to ensure adequate but not overloaded coronary blood supply. And may be associated with stress ulcers. Although stress ulcers were less common than other postoperative complications, according to relevant study, they are 0.2% to 2% [27]. We found that the incidence of stress ulcer in patients with AF was significantly higher than that in the control group and its prognosis is poor. The patient may eat less due to pain, stress, nausea, vomiting, gastrointestinal distress and thus lack the necessary nutrients. And stress ulcers may cause significant bleeding and increase the risk of death [28]. Therefor ulcers should be actively prevented after elderly hip fracture has occurred.
We found that pulmonary infection is an independent indicator of AF mortality in elderly hip fracture patients. Kjørholt’s research revealed that pneumonia is a common complication of hip fracture and can increase mortality by up to four times [29]. The mechanism may be that pneumonia significantly increases the risk of heart failure and AKI, which has been reported in previous studies [30]. We also found that hyponatremia is an independent predictive risk factor for death in hip fracture patients with AF, A serum sodium concentration of less than 135 mmol/L is what defines hyponatremia, an electrolyte abnormality that is often seen in heart failure patients and has been linked to adverse results, as confirmed by the study of Dimitrios Farmakis al, we thought that it also applies to elderly hip fracture patients with AF [31–33]. The mechanism may be that a number of physiological and metabolic disturbances that can be triggered by hyponatremia, especially cerebral oedema, cardiovascular problems, and exacerbation of the underlying disease, greatly increase the risk of death in patients [34]. Therefore, we should take care of regular medical check-ups and monitoring of serum sodium levels.
In order to improve the survival rate of elderly hip fracture patients with AF, mortality risk factors we should early identification, careful management and targeted treatment, in addition we should also prevent perioperative AF (paroxysmal AF).
In our study, hypertension was an independent risk factor for perioperative paroxysmal AF. The results of Monika Gawałko et al. were consistent with ours. Hypertension is prevalent in > 70% of patients with AF. In turn, hypertensive patients have up to 73% greater likelihood of AF. Current guidelines recommend that systematic AF screening may be warranted in all patients aged ≥ 65 years with at least one cardiovascular disease, including hypertension [35]. The mechanism may be that hypertension significantly increases the risk of AF by causing changes in cardiac structure and function, as well as comorbidities with other cardiovascular diseases.
ACCI was also an independent risk factor for perioperative paroxysmal AF. Charlson et al. created the Charlson Comorbidity Index, a tool for assessing the mortality risk due to comorbidities [36]. Patients with higher ACCI scores are prone to AF due to multiple chronic diseases, changes in cardiac structure and function, and an underlying systemic inflammatory response. COPD was also an independent risk factor for perioperative paroxysmal AF. This is consistent with other findings. A study utilizing the Spanish National Hospital Discharge Database discovered that COPD is a common comorbidity in patients hospitalized for AF [37]. In the Atherosclerosis Risk in Community (ARIC) cohort study, COPD and reduced lung function have been independently linked to the emergence of AF, despite the presence of risk factors for cardiovascular disease (e.g. smoking) in many COPD patients that may be confounding factors [38]. The mechanism may be that COPD triggered pathological process that includes hypoxia, electrolyte imbalance, altered pulmonary hemodynamics, pulmonary hypertension, elevated pCO2 levels and elevated systolic blood pressure, all of which are risk factors for AF [39, 40]. COPD patients may have low serum potassium levels due to electrolyte disturbances caused by overuse of corticosteroids or beta-blockers, the p-wave's length is augmented, a hazard factor for AF, as a result of this [41].
Limitations
This study has several limitations. First, this study is a single-center, retrospective cohort study, which limits the generalizability of the study. Second, due to the relatively low incidence of AF, the study population is limited in size. In the future, larger sample size studies are needed to carry out. Third, the lack of data on the initial onset of permanent AF prevents the analysis of risk factors for permanent AF in elderly hip fracture patients with AF, thus, only paroxysmal AF risk factors are assessed. Fourth, patient medication adherence is influenced by a variety of factors and there may be instances where patients discontinue medication on their own, which will require more refined management in the future.
Conclusions
The mortality risk is high in elderly patients with hip fractures combined with AF. The independent risk factors for their death include permanent AF, pulmonary infection and hyponatremia. The independent risk factors for perioperative paroxysmal AF in elderly patients with hip fractures are ACCI, hypertension and COPD. To enhance the survival rate of elderly patients with hip fractures, for patients with AF (especially those with permanent AF), we should strengthen the care, prevent pulmonary infection and hyponatremia. Additionally, we should prevent the occurrence of AF. For patients with multiple underlying diseases and hypertension and COPD, we should identify and optimize the treatment plan at an early stage.
Supplementary Information
Acknowledgements
None
Abbreviations
- AF
Atrial fibrillation
- NAF
Non atrial fibrillation
- Par AF
Paroxysmal atrial fibrillation
- Per AF
Permanent atrial fibrillation
- COPD
Chronic obstructive pulmonary disease
- ACCI
Age-adjusted Charlson Comorbidity Index
Authors’ contributions
ZQ. W and ZY. H conceived the study. W. L, AY.M and W. Z supported study preparation and data collection. WN. L, SH.L, SD.R, QI.Y, MM,F and JK.K collected the data and drafted the manuscript. ZQ. W and ZY. H critically reviewed the manuscript for important intellectual content. All authors approved the final version of the manuscript.
Data availability
The data supporting the findings of this study are available upon request from Zhi qian Wang.
Declarations
Ethics approval and consent to participate
The ethics committee of the Third Hospital of Hebei Medical University gave their approval to this study protocol, in accordance with the Helsinki Declaration (approval number 2021–087-1) and an exemption from obtaining informed consent was granted due to the retrospective nature of the data collection. To ensure patient privacy, all data was anonymized before analysis.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Wei Li, Aoying Min and Wei Zhao contributed equally as the first and co-first authors.
Contributor Information
Zhiqian Wang, Email: 37800709@hebmu.edu.cn.
Zhiyong Hou, Email: drzyhou@hebmu.edu.cn.
References
- 1.Boe DM, Boule LA, Kovacs EJ. Innate immune responses in the ageing lung. Clin Exp Immunol. 2017;187(1):16–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17(12):1726–33. [DOI] [PubMed] [Google Scholar]
- 3.Prince MJ, et al. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385(9967):549–62. [DOI] [PubMed] [Google Scholar]
- 4.Bhave PD, et al. Incidence, predictors, and outcomes associated with postoperative atrial fibrillation after major noncardiac surgery. Am Heart J. 2012;164(6):918–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alonso-Coello P, et al. Predictors, Prognosis, and Management of New Clinically Important Atrial Fibrillation After Noncardiac Surgery: A Prospective Cohort Study. Anesth Analg. 2017;125(1):162–9. [DOI] [PubMed] [Google Scholar]
- 6.Sairenchi T, et al. Atrial Fibrillation With and Without Cardiovascular Risk Factors and Stroke Mortality. J Atheroscler Thromb. 2021;28(3):241–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Go AS, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285(18):2370–5. [DOI] [PubMed] [Google Scholar]
- 8.Wong CX, et al. Atrial fibrillation and risk of hip fracture: A population-based analysis of 113,600 individuals. Int J Cardiol. 2017;243:229–32. [DOI] [PubMed] [Google Scholar]
- 9.Leibowitz D, et al. Perioperative atrial fibrillation is associated with increased one-year mortality in elderly patients after repair of hip fracture. Int J Cardiol. 2017;227:58–60. [DOI] [PubMed] [Google Scholar]
- 10.Prince-Wright LH, et al. Postoperative atrial fibrillation following non-cardiac surgery: Predictors and risk of mortality. Am J Surg. 2022;224(4):1062–7. [DOI] [PubMed] [Google Scholar]
- 11.Staerk L, et al. Atrial Fibrillation: Epidemiology, Pathophysiology, and Clinical Outcomes. Circ Res. 2017;120(9):1501–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Philip I, Berroëta C, Leblanc I. Perioperative challenges of atrial fibrillation. Curr Opin Anaesthesiol. 2014;27(3):344–52. [DOI] [PubMed] [Google Scholar]
- 13.Padfield GJ, et al. Progression of paroxysmal to persistent atrial fibrillation: 10-year follow-up in the Canadian Registry of Atrial Fibrillation. Heart Rhythm. 2017;14(6):801–7. [DOI] [PubMed] [Google Scholar]
- 14.Chiang CE, et al. Distribution and risk profile of paroxysmal, persistent, and permanent atrial fibrillation in routine clinical practice: insight from the real-life global survey evaluating patients with atrial fibrillation international registry. Circ Arrhythm Electrophysiol. 2012;5(4):632–9. [DOI] [PubMed] [Google Scholar]
- 15.Steinberg BA, et al. Rate versus rhythm control for management of atrial fibrillation in clinical practice: results from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF) registry. Am Heart J. 2013;165(4):622–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Steinberg BA, et al. Higher risk of death and stroke in patients with persistent vs. paroxysmal atrial fibrillation: results from the ROCKET-AF Trial. Eur Heart J. 2015;36(5):288–96. [DOI] [PMC free article] [PubMed]
- 17.Camm AJ, et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J. 2010;31(19):2369–429. [DOI] [PubMed] [Google Scholar]
- 18.Friberg L, et al. Increased mortality in paroxysmal atrial fibrillation: report from the Stockholm Cohort-Study of Atrial Fibrillation (SCAF). Eur Heart J. 2007;28(19):2346–53. [DOI] [PubMed] [Google Scholar]
- 19.Keating RJ, et al. Effect of atrial fibrillation pattern on survival in a community-based cohort. Am J Cardiol. 2005;96(10):1420–4. [DOI] [PubMed] [Google Scholar]
- 20.Baroutidou A, et al. Associations of Atrial Fibrillation Patterns With Mortality and Cardiovascular Events: Implications of the MISOAC-AF Trial. J Cardiovasc PharmacolTher. 2022;27:1–9. 10.1177/10742484211069422. [DOI] [PubMed] [Google Scholar]
- 21.Tzikas A, et al. Motivational Interviewing to Support Oral AntiCoagulation adherence in patients with non-valvular Atrial Fibrillation (MISOAC-AF): a randomized clinical trial. Eur Heart J Cardiovasc Pharmacother. 2021;7(Fi1):f63–71. [DOI] [PubMed] [Google Scholar]
- 22.Samaras A, et al. Rationale and design of a randomized study comparing Motivational Interviewing to Support Oral Anticoagulation adherence versus usual care in patients with nonvalvular atrial fibrillation: The MISOAC-AF trial. Hellenic J Cardiol. 2020;61(6):453–4. [DOI] [PubMed] [Google Scholar]
- 23.Bergau L, et al. Atrial Fibrillation and Heart Failure. J Clin Med. 2022;11:2510. 10.3390/jcm11092510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jalife J, Kaur K. Atrial remodeling, fibrosis, and atrial fibrillation. Trends Cardiovasc Med. 2015;25(6):475–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sohns C, Marrouche NF. Atrial fibrillation and cardiac fibrosis. Eur Heart J. 2020;41(10):1123–31. [DOI] [PubMed] [Google Scholar]
- 26.Bisbal F, et al. Atrial Failure as a Clinical Entity: JACC Review Topic of the Week. J Am Coll Cardiol. 2020;75(2):222–32. [DOI] [PubMed] [Google Scholar]
- 27.Krawiec F, et al. Duodenal ulcers are a major cause of gastrointestinal bleeding after cardiac surgery. J Thorac Cardiovasc Surg. 2017;154(1):181–8. [DOI] [PubMed] [Google Scholar]
- 28.Finkenstedt A, Berger MM, Joannidis M. Stress ulcer prophylaxis: Is mortality a useful endpoint? Intensive Care Med. 2020;46(11):2058–60. [DOI] [PubMed] [Google Scholar]
- 29.Kjørholt KE, et al. Increased risk of mortality after postoperative infection in hip fracture patients. Bone. 2019;127:563–70. [DOI] [PubMed] [Google Scholar]
- 30.Marrie TJ. Community-acquired pneumonia. Clin Infect Dis. 1994;18(4): 501–13; quiz 514–5. [DOI] [PubMed]
- 31.Farmakis D, et al. Hyponatremia in heart failure. Heart Fail Rev. 2009;14(2):59–63. [DOI] [PubMed] [Google Scholar]
- 32.Sica DA. Hyponatremia and heart failure–pathophysiology and implications. Congest Heart Fail. 2005;11(5):274–7. [DOI] [PubMed] [Google Scholar]
- 33.Bavishi C, et al. Prognostic significance of hyponatremia among ambulatory patients with heart failure and preserved and reduced ejection fractions. Am J Cardiol. 2014;113(11):1834–8. [DOI] [PubMed] [Google Scholar]
- 34.Vígh J, et al. The clinical importance of hyponatremia. Orv Hetil. 2019;160(8):314–9. [DOI] [PubMed] [Google Scholar]
- 35.Gawałko M, Linz D. Atrial Fibrillation Detection and Management in Hypertension. Hypertension. 2023;80(3):523–33. [DOI] [PubMed] [Google Scholar]
- 36.Charlson ME, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. [DOI] [PubMed] [Google Scholar]
- 37.Méndez-Bailón M, et al. Chronic obstructive pulmonary disease predicts higher incidence and in hospital mortality for atrial fibrillation. An observational study using hospital discharge data in Spain (2004–2013). Int J Cardiol. 2017;236:209–215. [DOI] [PubMed]
- 38.Li J, et al. Airflow obstruction, lung function, and incidence of atrial fibrillation: the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2014;129(9):971–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang L, et al. Structural changes in the progression of atrial fibrillation: potential role of glycogen and fibrosis as perpetuating factors. Int J Clin Exp Pathol. 2015;8(2):1712–8. [PMC free article] [PubMed] [Google Scholar]
- 40.Terzano C, et al. Atrial fibrillation in the acute, hypercapnic exacerbations of COPD. Eur Rev Med Pharmacol Sci. 2014;18(19):2908–17. [PubMed] [Google Scholar]
- 41.Krijthe BP, et al. Serum potassium levels and the risk of atrial fibrillation: the Rotterdam Study. Int J Cardiol. 2013;168(6):5411–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data supporting the findings of this study are available upon request from Zhi qian Wang.