Abstract
Introduction
Anterior cruciate ligament (ACL) reconstruction involves prolonged rehabilitation, with Return to Sport (RTS) as a key goal for athletes. Integrating Dual Task (DT) strategies, which combine cognitive and physical tasks, is critical, as multitasking mirrors real-world and sports-specific demands. Assessing how distractions affect performance is essential to optimize RTS outcomes for both the reconstructed and healthy limbs.
Purpose
To analyze the influence of DT on the performance of the Triple Hop Test for distance (THD) in individuals’ status post ACL reconstruction.
Study type
Cross Sectional
Materials and Methods
Seventeen patients post-ACL were recruited and performed THD under two conditions: single task (standard condition) and dual task (with an added neurocognitive task). Assessments were conducted on both the healthy and the previously injured limb over six meters, measured via a standard measuring tape. Paired t-tests and Mann-Whitney-Wilcoxon or Kruskal-Wallis tests were applied to investigate differences. Categorical variables were compared using chi-squared tests.
Results
There was a significant difference in average distance between single task performances in the healthy and previously operated limbs, with a difference of 20.71 cm (p=0.016). A significant difference was also observed in DT performance, with a distance variation of 10.41 cm (p=0.038). Comparing performances, both the healthy and the ACL-reconstructed limbs showed performance deterioration under DT conditions, with a greater percentage decline in the healthy limb.
Conclusions
Dual Task conditions appear to hinder performance in the THD in both the healthy and post-ACL reconstructed limbs.
Level Of Evidence
3b
Keywords: ACL, Assessments, Neurocognitive, RTP, Hop
Introduction
The post-operative rehabilitation after anterior cruciate ligament (ACL) injuries is an important topic in sports medicine and ACL reconstruction is commonly undertaken to restore knee stability and return the individual to function. Neuroplasticity, or the brain’s ability to reorganize itself, allows the central nervous system to adapt to both external (environmental) and internal factors, such as injuries. In some cases, patients may struggle with adopting effective motor-learning strategies, or traditional rehabilitation may not provide sufficient stimulation to promote motor skill recovery. This could help explain why, after an ACL injury, patients do not always regain full motor function, as current rehabilitation programs may not fully engage the neuroplastic potential needed for optimal recovery.1 The efficacy of this recovery process is primarily evaluated through functional tests like the Triple Hop for distance (THD), which is one means to assess the dynamic movement capabilities of individuals. Despite the routine nature of this test, daily life and sports often require multitasking, and the impact of dual-tasking on THD performance remains an underexplored area.2,3
The safe return to sports activities following ACL reconstruction is a critical chapter in the multidisciplinary management of patients undergoing this procedure. Scientific interest in this area has increased over the years, highlighting that despite growing knowledge, the re-injury rate remains high. An area of interest that could have implications for a safer return to sports is the investigation of neurocognitive performance.
The prevalence of individuals experiencing a second injury to the same knee within the first five years after ACL reconstruction exceeds 15%, while it is around 8% for the contralateral knee.4,5 In a recent study, Della Villa et al.6 reported an impressive 42% rate of isolated ACL injuries with non-contact mechanisms experiencing re-injury within five years. According to research by Paterno et al.,7 this risk is up to 15 times higher, with a fourfold increased risk for female individuals of sustaining a homolateral ACL injury and six times for the contralateral knee.
Limited evidence suggests that deficits in neurocognitive functions are associated with an increased risk of re-injury.2,8–10 While the mechanisms through which neurocognitive demands influence injury risk are not fully understood, it is known that performing a motor action under the influence of a dual cognitive task exposes the athlete to a more realistic context that requires cognitive processing and decision-making.11–13 In sports activities, where cognitive demands are high, motor deficits may become more apparent, thereby exposing the patients to a higher risk of injury. The introduction of neurocognitive distraction elements into testing protocols is advocated to provide a more realistic and comprehensive assessment of an athlete’s readiness to return to sport, potentially mitigating the high risk of re-injury associated with ACL rehabilitation.14,15
Emerging studies suggest that current functional tests may not adequately simulate the complex environments encountered during sports, which often leads to injuries. These environments typically involve cognitive distractions that can impact performance, highlighting a gap in standard testing protocols.14,15
Furthermore, neuroplastic changes following ACL injuries can lead to maladaptations such as arthrogenic muscle inhibition, influenced by altered sensory feedback and disrupted homeostasis.16,17 Authors have assessed the effect of cognitive challenge during functional tasks18,19 but this is the first to assess the effect of a dual task during a triple leg hop for distance on ACLR patients. This manuscript explores incorporating dual-task scenarios into the rehabilitation assessment as this could better reflect true functional capacity by mimicking the cognitive and motor tasks athletes face in competitive environments.
This study aims to explore the influence of DT on the execution of the THD, comparing the healthy limb to the surgically repaired limb in patients post-ACL reconstruction.14
The hypothesis was that the injured knee will show a greater decline in performance during dual-task conditions compared to the healthy limb.
Material and Methods
Study Design
Between March 2023 and February 2024, patients who had undergone anterior cruciate ligament (ACL) reconstruction surgery were recruited from one physiotherapy clinic for a normal testing procedure after completing the rehabilitation programs. All patients undergoing ACL reconstruction between 2022 and 2023 were screened for inclusion in the study.
Inclusion criteria were: patients who had undergone an ACL reconstruction at least six months but not greater than 12 months prior (with full passive range of motion and absence of swelling) and participated in neurocognitive training during rehabilitation, being 18 years of age or older, of activity level 1 or 2, and having a stable contralateral knee with no history of injury or surgery in the prior two years, The exclusion criteria included the presence of concurrent musculoskeletal conditions (e.g., back, hip, or ankle pain) impairing the ability to perform jumps on both lower limbs, advanced degenerative changes (grade III or higher per the Kellgren-Lawrence classification based on pre-operative or intra-operative radiography), and an inability to speak, read, write, or understand Italian.
Each patient underwent a protocol to evaluate their performance on THD under two different conditions: a single task (standard condition) and a dual task (incorporating a neuro-cognitive task), on both the healthy limb and the post-operative limb. Testing protocols were uniformly applied across all testing sessions and were administered by the same researcher to ensure consistency.
Setting and Procedures
The testing session was conducted in a private musculoskeletal clinic during a single test session following the usual clinical practices. All patients had already completed rehabilitation programs before the testing session, and the testing procedure did not modify any component of the existing rehabilitation pathways. The data were collected as part of routine clinical practice and did not introduce experimental research elements.
Testing Procedure
All procedures were performed following written informed patient consent and in accordance with the ethical standards of the institutional and national research committee and the 1964 Declaration of Helsinki. Since the approval was obtained as part of established clinical practice, no specific code is required. The approval date corresponds to the session held on May 24, 2022. All participants signed an informed consent form before participating in the study.
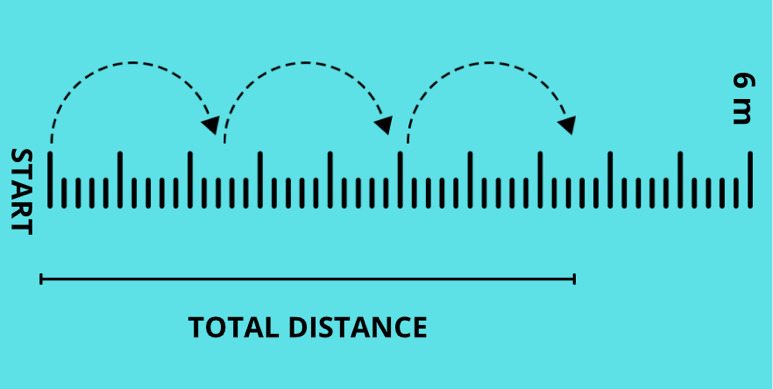
The THD was performed on a concrete floor with a 6-meter-long and 15 cm-wide tape (Figure 1).
Figure 1. Setting for triple leg hop.
Prior to the test, participants underwent a five minute warm-up on a stationary bicycle, followed by 10 bipedal squats, 10 right/left lunges, a one minute break, 10 bipedal vertical jumps, 10 bipedal horizontal jumps, a two minute break, and five vertical and horizontal jumps on each side. Participants then familiarized themselves with the THD by performing it twice per leg without any additional cognitive stimuli.
For each leg, three trials were performed for each test condition (single and dual task). Trials were always conducted starting with the healthy leg followed by the injured leg. To qualify as successful, the landing of the THD had to be maintained for two seconds. If the attempt was unsuccessful, verbal feedback was provided, and the test was repeated without additional instructions, typically requiring one or two extra trials. The mean distance from the three trials was used for analysis.
In the dual task condition, cognitive interference was introduced through the use of two smartphones (iPhone X) placed on tripods at eye level to the right and left of the participant and an iPad in front showing a sequence of 8 numbers every 0.3 seconds through the switch-ON app. The phones displayed a color signal changing between blue, yellow, and green every 0.3 seconds. Participants began the test when the signal turned green, regardless of phone position. During the THD, participants were instructed to prioritize the cognitive task of observing the number sequence and recalling it in reverse order after completion of the physical test. The accuracy of the neuro-cognitive task was not assessed (Figure 2).
Figure 2. Setup for THD with cognitive interference.

Two iPhone X were placed at the same distance left/right from the patient’s side and at the end of the tape an iPad was placed in front of the patent that played a random sequence of numbers.
In research contexts, the effect of the dual task can be quantified as the percentage change in performance parameters between the dual task and single task, known as the Dual Task Cost (DTC).3 The dual task cost, as proposed by Grooms and colleagues,3refers to the decline in performance observed when an individual is required to simultaneously execute both a cognitive task and a physical task, such as during neurocognitive testing for ACL rehabilitation. In the context of ACL patients, this cost is typically evaluated by comparing performance on functional motor tasks (e.g., jumping, cutting, or balancing) with and without the addition of a concurrent cognitive task, such as responding to visual or auditory stimuli, or engaging in working memory challenges. The dual task cost is calculated by comparing performance on a task when it is performed in isolation (single task) to performance when it is paired with a concurrent cognitive task (dual task). The formula is typically . According to the formula, a greater distance covered in the jump indicates better performance; thus, a DTC value below 100% indicates a performance deterioration in the dual-task condition, while a value above 100% reflects improved performance under dual-task conditions.
Statistical Analysis
The sample size for this observational descriptive study was determined based on a hypothesized 15% reduction in jump height post-intervention from a literature-based mean (μ) of 547 cm to 464 cm, with a population standard deviation (σ) of 97 cm. The calculated effect size (d) was 0.8556701, indicating an expected 15% decrease. Thus, a sample size of 17 subjects was determined a priori to ensure 95% power (1−β), reflecting the likelihood of detecting a true effect.
All statistical analyses were performed using Stata version 18. Paired Student’s t-tests were used to compare the means of continuous variables with normal distributions. For continuous variables not meeting normality assumptions, nonparametric tests (Mann-Whitney-Wilcoxon or Kruskal-Wallis) were applied. Frequency distributions of categorical variables were compared using 2x2 contingency tables and chi-square tests.
Results
Seventeen patients were included (mean age of 23.2 ± 5.1 years), 12 males and 5 females Detailed demographic and clinical characteristics of the patients are shown in Table 1.
Table 1. Demographic and clinical characteristics of the included patients.
| Male | Female | Total | p-value | |
|---|---|---|---|---|
| N | 12 (70.6%) | 5 (29.4%) | 17 (100.0%) | |
| Age (years) | 23.7 (5.4) | 22.2 (4.9) | 23.2 (5.1) | 0.607 |
| Weight (kg) | 73.1 (10.2) | 66.2 (6.5) | 71.1 (9.7) | 0.189 |
| Height (cm) | 178.9 (7.9) | 175.0 (8.5) | 177.8 (8.0) | 0.377 |
| BMI (Kg/m2) | 22.8 (2.5) | 21.6 (1.4) | 22.4 (2.3) | 0.343 |
| Injured Leg | ||||
| Right | 7 (58.3%) | 1 (20.0%) | 8 (47.1%) | 0.149 |
| Left | 5 (41.7%) | 4 (80.0%) | 9 (52.9%) | |
| Activity level (moderate) | 1 (8.3%) | 1 (20%) | 2 (11.8%) | 0.496 |
| Activity level (intense) | 11 (91.7%) | 4 (80%) | 15 (88.2%) |
During the THD under ST conditions, a statistically significant difference in the average distance was observed between the healthy and operated limbs, with a mean difference of 20.7 +/- 3.64 cm (p= 0.016). A statistically significant difference was also noted under DT conditions, with a difference of 10.41 cm ± 22.6, (p= 0.038) between the healthy and operated limbs.
When comparing the differences in performance between the healthy and operated limbs DTC results were utilized and the results are presented in Table 2.
Table 2. Percentage of Dual Task Cost in the healthy and post-operative limb during the Triple Hop Test.
| Males (%) n=12 (70,6) | Females (%) n=5 (29,4) | Full sample (%) n=17 (100) | |
|---|---|---|---|
| DTC Healthy limb1 | 6.09% | 4.54% | 6.49% |
| DTC Healthy limb2 | 6.23% | 7.78% | 6.66% |
| DTC Post=operative limb1 | 4.30% | 4.37% | 4.32% |
| DTC Post-operative limb2 | 5.11% | 4.04% | 4.80% |
1=Average performance, 2=Best performance
A higher percentage drop in performance for the healthy limb is demonstrated compared to the operated limb.
Discussion
Main Findings
The most important finding of the present study is that patients who have undergone anterior cruciate ligament (ACL) reconstruction showed disparities between the healthy limb and the operated limb in the THD. Performance measurements were significantly better in the healthy limb versus the post operative limb.
An unexpected outcome was that the sample demonstrated a better dual task cost value on the post-operative limb compared to the healthy one. All subjects included in the study integrated traditional rehabilitation with motor learning that incorporated elements of distraction from the earliest stages. This allows us to hypothesize that the administered interventions might have addressed deficits that would have been expected. One possible explanation for the better result in DTC condition, is that the majority of the ‘neurocognitive’ training was performed on the post-operative leg. Patients generally engaged in strength and conditioning exercises for both limbs; however, the injured leg was more frequently targeted during dual-task conditions and cognitive challenges. These included tasks such as maintaining balance while tracking the movement of a laser pointer with their gaze or performing exercises like jumps and running drills while memorizing sequences of numbers displayed on a screen. Notably, there was a more pronounced performance decline in the healthy limb compared to the operated limb, further underscoring the complexity of the relationship between ACL reconstruction and motor skills. A second reason could be that neuroplastic alterations occur bilaterally, potentially affecting the healthy limb as well or strength deficit that could persist after completing rehabilitation program.20 Finally, due to deconditioning, the healthy limb may not always represent a realistic target for recovery. It is important to note that In this research design, only the distance of the hop was measured, which do not incorporate metrics pertaining to quality, such as knee valgus motion or trunk displacement. Cognitive proficiency/scores, such as the accurate recall of numerical sequences were also not measured.
Clinical Implication
Despite the modest magnitude of these disparities, the findings are crucial from both clinical and scientific perspectives. Clinically, they underscore the need to develop specific rehabilitative approaches that can precisely measure the effects of neurocognitive interventions based on the pathophysiology of ACL reconstruction that involves neuroplastic changes in the brain. In research, the examination of performance assessments assists in deepening the understanding of the effects of specific rehabilitation protocols, enhancing knowledge in a critical area of medical research. . A previous study had investigated the effects of dual tasking in the context of the triple hop test, focusing on healthy subjects and finding no significant performance variations. In the current study, substantial differences were observed not only in healthy participants but also in those with ACLR, suggesting that both lower limbs could be negatively affected in terms of overall performance.
A strength of the study is its novelty in evaluating the effects of dual tasking on the outcomes of the triple hop test between six and 12 months after ACL reconstruction. This indicates that after ACL surgery, limited cognitive resources may not only impact the affected limb but also the uninjured limb. This consideration is crucial, especially given that a significant percentage of re-injuries occur in the contralateral limb.
Limitations
Due to limited resources and the small number of patients recruited, it was not feasible to test subjects who had not undergone neuro-cognitive training as part of their rehabilitation. A limitation relates to the neuro-cognitive skills prescribed during the rehabilitation period prior to the tests. Rehabilitation tasks and progressions for these subjects were not reported.
Different variables could provide deeper insights into the observed differences between the performance of the healthy and operated limbs, which, while statistically significant, remained below a 15% threshold. As mentioned, this study considered performance only qualitatively (distance), while the influences of dual tasking on biomechanical quality (kinematics) were not accounted for due to resource limitations. Cognitive distraction could impact the quality of performance during activities and the subsequent risk of injury, highlighting the need for further exploration of the relationship between these variables. For instance, while performing a jump, the patient might recall numbers displayed on a screen. If the uninjured leg achieves 4/4 correct responses but the injured leg achieves only 2/4, this may indicate a decline in cognitive performance during functional tasks.
Finally, strength data were not included in the testing session so it cannot be assumed that deficits in performance are a consequence of a decline in strength. Including a cognitive task evaluation within the functional assessment could provide valuable insights. The relatively small sample size and low proportion of female participants limit the generalizability of these findings to the broader population undergoing ACL reconstruction.
Although RTS testing impacts the risk of reinjury, it cannot fully predict who may sustain a second ACL injury.21,22 Future research should evaluate dual-task effects in this population, focusing on both performance quantity (e.g., distance) and quality (e.g., kinematics and cognitive function). Investigating the impact of neurocognitive training or graft type on dual-task cost could provide further insights.
Conclusions
The results of this study demonstrate significant disparities in performance on the THD between the healthy and operated limbs of patients following anterior cruciate ligament (ACL) reconstruction, under both single and dual task conditions. Notably, the healthy limb exhibited a greater decline in performance, suggesting that both limbs are vulnerable to the effects of cognitive load post-surgery. These insights suggest the potential value of incorporating neuro-cognitive elements in future research to better address the complex demands of real-world activities and explore strategies to reduce the risk of re-injury.
The results underscore the importance of considering both limbs in the rehabilitation process, reflecting the interconnectedness of bodily systems and the widespread impact of cognitive factors on motor performance. Further research is encouraged to explore the broader implications of dual task training in ACL rehabilitation and its potential to improve long-term outcomes for patients returning to sport.
References
- Neuroplasticity and anterior cruciate ligament injury. Kakavas G., Malliaropoulos N., Pruna R., Traster D., Bikos G., Maffulli N. 2020Indian J Orthop. 54:275–280. doi: 10.1007/s43465-020-00045-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Incorporating a dual-task assessment protocol with functional hop testing. Ness B. M., Zimney K., Kernozek T., Schweinle W. E., Schweinle A. 2020Int J Sports Phys Ther. 15(3):407–420. doi: 10.26603/ijspt20200407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Combining neurocognitive and functional tests to improve return-to-sport decisions following ACL reconstruction. Grooms D. R., Chaput M., Simon J. E., Criss C. R., Myer G. D., Diekfuss J. A. 2023J Orthop Sports Phys Ther. 53(8):415–419. doi: 10.2519/jospt.2023.11489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. Wright R. W., Magnussen R. A., Dunn W. R., Spindler K. P. 2011J Bone Joint Surg Am. 93(12):1159–1165. doi: 10.2106/JBJS.J.00898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anterior cruciate ligament ruptures: return to play and long-term outcome in elite handball players. Schiffner E., Latz D., Grassmann J. P.., et al. 2018Knee Surg Sports Traumatol Arthrosc. 26(1):192–198. [Google Scholar]
- High rate of second ACL injury following ACL reconstruction in male professional footballers: An updated longitudinal analysis from 118 players in the UEFA Elite Club Injury Study. Della Villa F., Hägglund M., Della Villa S., Ekstrand J., Waldén M. 2021Br J Sports Med. 55(23):1350–1356. doi: 10.1136/bjsports-2020-103555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Paterno M. V., Rauh M. J., Schmitt L. C., Ford K. R., Hewett T. E. 2012Clin J Sport Med. 22(2):116–121. doi: 10.1097/JSM.0b013e318246ef9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drop-jump landing varies with baseline neurocognition: Implications for anterior cruciate ligament injury risk and prevention. Herman D. C., Barth J. T. 2016Am J Sports Med. 44(9):2347–53. doi: 10.1177/0363546516657338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Arden C. L., Webster K. E., Taylor N. F., Feller J. A. 2011Br J Sports Med. 45(7):596–606. doi: 10.1136/bjsm.2010.076364. [DOI] [PubMed] [Google Scholar]
- Associations between cognitive function and ACL injury-related biomechanics: a systematic review. Bertozzi F., Fischer P. D., Hutchison K. A., Zago M., Sforza C., Monfort S. M. 2023Sports Health. 15(6):855–866. doi: 10.1177/19417381221146557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Effects of decision making on landing mechanics as a function of task and sex. Mache M. A., Hoffman M. A., Hannigan K., Golden G. M., Pavol M. J. 2013Clin Biomech. 28(1):104–9. doi: 10.1016/j.clinbiomech.2012.10.001. [DOI] [PubMed] [Google Scholar]
- Decision making and experience level influence frontal plane knee joint biomechanics during a cutting maneuver. Kipp K., Brown T. N., McLean S. G., Palmieri-Smith R. M. 2013J Appl Biomech. 29(6):756–762. doi: 10.1123/jab.29.6.756. [DOI] [PubMed] [Google Scholar]
- Dual-task and anticipation impact lower limb biomechanics during a single-leg cut with body borne load. Seymore K. D., Cameron S. E., Kaplan J. T., Ramsay J. W., Brown T. N. 2017J Biomech. 65:131–137. doi: 10.1016/j.jbiomech.2017.10.021. [DOI] [PubMed] [Google Scholar]
- Think outside the box: incorporating secondary cognitive tasks into return to sport testing after ACL reconstruction. Chaaban C. R., Turner J. A., Padua D. A. 2023Front Sports Act Living. 4:1089882. doi: 10.3389/fspor.2022.1089882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Is it time we better understood the tests we are using for return to sport decision making following ACL reconstruction? A critical review of the hop tests. Davies W. T., Myer G. D., Read P. J. 2017Sports Med. 47(5):763–775. doi: 10.1007/s40279-019-01221-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Functional performance testing after anterior cruciate ligament reconstruction: a systematic review. Abrams G. D., Harris J. D., Gupta A. K.., et al. 2014Orthop J Sports Med. 2(1):2325967113518305. doi: 10.1177/2325967113518305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longitudinal evaluation of quadriceps strength and corticospinal excitability following anterior cruciate ligament reconstruction. Lepley L. K., Gribble P. L., Thomas A. C., Tevald M. A., Sohn D. H., Pietrosimone B. G. 2019Phys Ther. 99(1):35–46. [Google Scholar]
- Effects of narrow-base walking and dual tasking on gait spatiotemporal characteristics in anterior cruciate ligament-injured adults compared to healthy adults. Mazaheri M., Negahban H., Soltani M.., et al. 2017Knee Surg Sports Traumatol Arthrosc. 25(8):2528–2535. doi: 10.1007/s00167-016-4014-4. [DOI] [PubMed] [Google Scholar]
- Reliability of dynamic balance simultaneously with cognitive performance in patientss with ACL deficiency and after ACL reconstructions and in healthy controls. Akhbari B., Salavati M., Ahadi J.., et al. 2015Knee Surg Sports Traumatol Arthrosc. 23(11):3178–3185. doi: 10.1007/s00167-014-3116-0. [DOI] [PubMed] [Google Scholar]
- Knee joint pathology and efferent pathway dysfunction: Mapping muscle inhibition from motor cortex to muscle force. Sherman D. A., Rush J., Glaviano N. R., Norte G. E. 2024Musculoskel Sci Pract. 103204 doi: 10.1016/j.msksp.2024.103204. [DOI] [PubMed] [Google Scholar]
- The development and reliability of 4 clinical neurocognitive single-leg hop tests: Implications for return to activity decision-making. Millikan N., Grooms D. R., Hoffman B., Simon J. E. 2019J Sport Rehabil. 28(5):536–544. doi: 10.1123/jsr.2018-0037. [DOI] [PubMed] [Google Scholar]
- The association between passing return-to-sport criteria and second anterior cruciate ligament injury risk: A systematic review with meta-analysis. Losciale J. M., Zdeb R. M., Ledbetter L., Reiman M. P., Sell T. C. 2019J Orthop Sports Phys Ther. 49(2):43–54. doi: 10.2519/jospt.2019.8190. [DOI] [PubMed] [Google Scholar]


