INTRODUCTION
Central venous thrombosis (CVT), a blood clot in the dural venous sinuses of the brain, is a rare condition, accounting for less than 1% of all strokes. Despite its rarity, CVT carries a mortality rate of 5.5 – 18% even with treatment.1 This case report highlights a patient with this potentially fatal condition who presented with only a headache and no neurological deficits. Clinicians should maintain a high index of suspicion for CVT, even in patients without traditional hypercoagulable risk factors.
CASE REPORT
A 43-year-old woman with a history of ocular migraines presented with a three-day history of waxing and waning headache, nausea, and vomiting. Her primary concern was that the headache differed in character and intensity from her usual ocular migraines. The headache was so debilitating that she was unable to complete her normal activities. It was severe, frontal, and associated with photophobia, phonophobia, nausea, and vomiting. Despite taking acetaminophen and ibuprofen at home, she experienced only mild relief. A few weeks prior, she and her daughter had a viral illness with conjunctivitis and vomiting. Differential diagnoses included migraine, intracranial mass, dural venous thrombosis, viral illness, hypertensive emergency, electrolyte abnormality, thyroid dysfunction, and pregnancy.
Upon presentation to the emergency department (ED), her vitals were notable for elevated blood pressure at 177/111 mmHg, a heart rate of 100 beats per minute, a respiratory rate of 16 breaths per minute, room air oxygen saturation of 97%, and a temperature of 36.6°C. Initial and repeat neurological examinations were reassuring, with no focal deficits. Cranial nerves II through XII were intact, sensation and motor function were equal, and gait was normal. She was treated with intravenous fluids, prochlorperazine, diphenhydramine, ketorolac, and magnesium for symptom management. A complete blood count (CBC), comprehensive metabolic panel (CMP), thyroid-stimulating hormone (TSH), magnesium, and phosphorus levels were ordered, all of which were unremarkable. There was no leukocytosis, electrolyte imbalance, or thyroid dysfunction contributing to her headache. A point-of-care urine pregnancy test (UHCG) was negative, and an infectious workup, including a respiratory viral panel, also was negative.
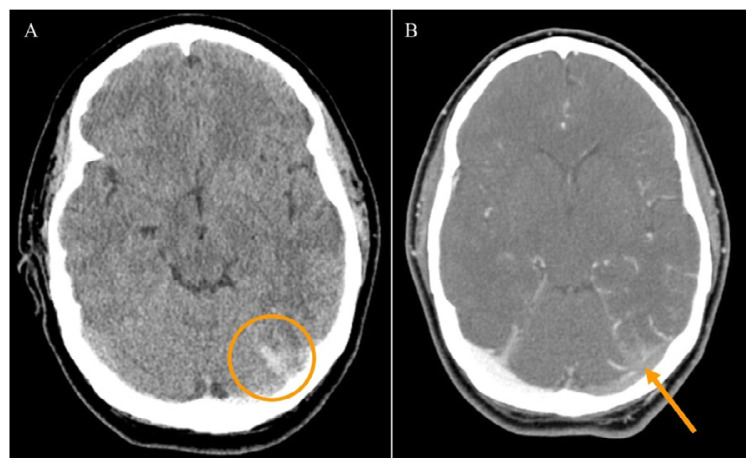
Given that the headache differed in character and intensity from her typical migraines and was unrelieved by home medications, a non-contrast head computed tomography (CT) was ordered immediately upon presentation. The CT was notable for an asymmetric hyperdensity of the left transverse and sigmoid sinus, raising concern for CVT (Figure 1). Additionally, there was a left peritentorial hyperdensity suggesting an adjacent thrombosed vein. A subsequent CT venogram with contrast confirmed an acute central venous sinus thrombosis involving the left transverse, sigmoid, and jugular sinuses (Figure 2). The patient was started on a heparin drip, and neurology was consulted. After evaluation, she was admitted to the neurology service for further assessment of the underlying cause of the CVT.
Figure 1.
(A) CT head without contrast showing abnormal asymmetric hyper-density involving the left transverse (orange circle) and sigmoid sinus. (B) CT venogram head with contrast showing acute CVT propagating from the sinus confluence through the left transverse (orange arrow) and sigmoid sinus.
Figure 2.
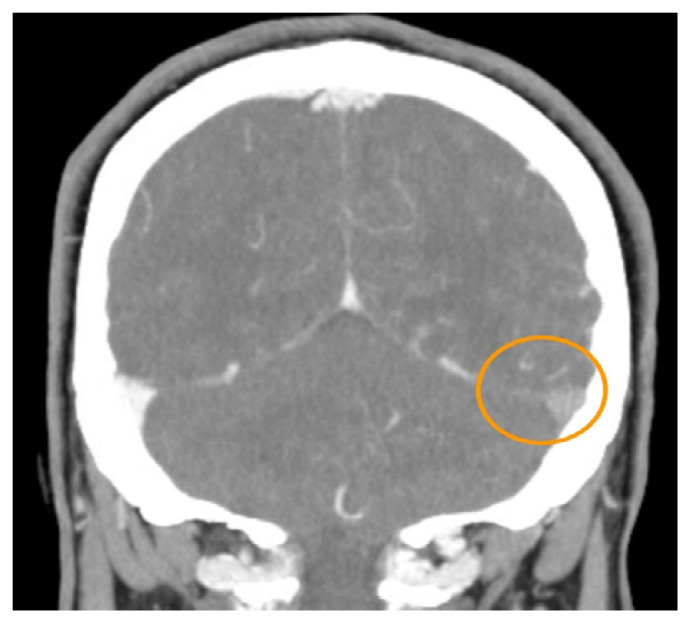
CT venogram with contrast head showing asymmetric filling defect in left transverse sinus (orange circle).
The following day, a repeat non-contrast head CT showed stable findings, and she was transitioned from heparin to apixaban. During her admission, hypercoagulable labs and additional imaging were conducted to investigate the cause of the thrombus. Tests for beta-2-glycoprotein and cardiolipin antibodies, factor 2 mutation, factor V Leiden mutation, protein C and S deficiencies, antithrombin III deficiency, lupus anticoagulant, and homocysteine levels were all negative. A CT of the chest, abdomen, and pelvis with contrast also was negative for malignancy. Upon discharge, the patient was instructed to continue anticoagulation with apixaban and to follow up with magnetic resonance imaging (MRI) with and without contrast.
Three months later, MRI showed significant recanalization of the sinuses. At her follow-up appointment with neurology, she was advised to discontinue apixaban, begin aspirin, and stay up-to-date with her annual SARS-CoV-2 vaccinations.
DISCUSSION
The cerebral sinuses are made up of the superficial and deep venous system that eventually drain into the internal jugular vein.2 The superior sagittal and cavernous sinus are the major portions of the superficial venous system; and the deep system consists of the straight, transverse, and sigmoid sinuses. Multiple venous sinuses are involved in most patients diagnosed with a CVT.2,3 Involvement of the straight sinus and deep venous system is more likely to present with altered consciousness or confusion.3 Our patient was involved of her transverse and sigmoid sinuses. This is one potential reason why she remained alert and oriented with no change in mentation upon arrival to the ED.
The described patient presented with a headache worse and different in character from her typical migraines without papilledema or stroke-like symptoms. The clinical presentation of CVT is variable and somewhat dependent on the size of thrombus, sinuses affected, presence of collateral flow, and acuity of onset. About 40% of CVT patients present with stroke-like symptoms within 48 hours of symptom onset.1 Persistent and/or progressively worsening headache is the most common presenting symptom, seen in 80 – 90% of cases, and can uncommonly be the only presenting symptom.1–3 A case series of CVT presenting with isolated headache found that while the character of headache was not uniform, it tended to be severe, progressive, continuous, and different from the patients’ usual migraines.4 Papilledema has been reported in up to 85% of patients with acute or subacute onset and 100% of patients with chronic onset CVT.2,3
CVT is most common in women, comprising approximately 70% of cases, and is strongly associated with oral contraceptive use and pregnancy. However, numerous other prothrombotic risk factors have been implicated.1,3 Median age of those affected is 30 to 41 years.3 Rarely, there have been cases of CVT reported in patients without preexisting co-morbidities and a negative coagulation workup as in our patient. In several cases, an acute viral illness preceded the CVT by about seven days.5 The SARS-CoV-2 virus has been identified in several previously healthy patients as a suggested agent for the creation of a hypercoagulable state. The virus’ tropism for the ACE2 receptor on endothelial cells leads to endothelial damage and excessive clot formation.6,7
Another suggested mechanism of acute viral infection leading to CVT is the generation of a cytokine storm with subsequent endothelial damage and a prothrombotic state.8 Adenovirus, one of the leading causes of conjunctivitis, is one virus capable of creating a cytokine storm.9 Bacterial and fungal infections of the head and neck, including orbital cellulitis, paranasal sinusitis, and otitis media/mastoiditis, can also precede CVT.1,10 Our patient lacked prothrombotic risk factors, but was endorsing viral symptoms, including conjunctivitis a few weeks prior to her ED presentation. Overall mortality is 5.5 – 18%, with severe or permanent disability in 6 – 10% of surviving patients.1 Most patients have a favorable prognosis after treatment.1,3
Neuroimaging is considered the gold standard diagnostic tool and is required for formal diagnosis and CVT localization.2 CT is the initial imaging modality of choice for most patients with non-specific neurological symptoms, primarily due to how rapidly it can be acquired.11 Findings on CT include hyperattenuation of the affected venous sinus, dense clot sign, and indirect signs such as cerebral edema, mass effect, and hemorrhage.2,11 However, Cumurciuc et al.4 and Timóteo et al.12 noted that non-contrast CT examination was normal in 40% of patients, who presented with isolated headache, but ultimately had a CVT. This finding suggests that CT and MRI venogram should be considered to evaluate for filling defects in patients presenting with severe headache and an initial negative workup. These imaging modalities may show evidence of collateralization to bypass the occluded segment(s).13
Although 57 – 86% of treated patients make a full recovery, mortality is still as high as 18%.1 Potential risk factors for increased mortality include age (infancy or elderly), altered mental status, GCS <9, coma, ICH, malignancy, deep vein thrombosis, and hyperglycemia.1 The ultimate cause of death for patients diagnosed and treated for a CVT are herniation, status epilepticus, and pulmonary embolism.1
CONCLUSIONS
CVT often occurs in the presence of hypercoagulability, malignancy, or viral illness. Due to an unremarkable hypercoagulable and malignant work up, etiology of our patient’s CVT is unknown and suspected to be related to viral illness. It is important for ED providers to consider CVT for patients presenting with a headache and normal neurologic exam.
REFERENCES
- 1.Ranjan R, Ken-Dror G, Sharma P. Pathophysiology, diagnosis and management of cerebral venous thrombosis: A comprehensive review. Medicine (Baltimore) 2023;102(48):e36366. doi: 10.1097/MD.0000000000036366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Idiculla PS, Gurala D, Palanisamy M, Vijayakumar R, Dhandapani S, Nagarajan E. Cerebral venous thrombosis: A comprehensive review. Eur Neurol. 2020;83(4):369–379. doi: 10.1159/000509802. [DOI] [PubMed] [Google Scholar]
- 3.Luo Y, Tian X, Wang X. Diagnosis and treatment of cerebral venous thrombosis: A review. Front Aging Neurosci. 2018;10(2) doi: 10.3389/fnagi.2018.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cumurciuc R, Crassard I, Sarov M, Valade D, Bousser MG. Headache as the only neurological sign of cerebral venous thrombosis: A series of 17 cases. J Neurol Neurosurg Psychiatry. 2005;76(8):1084–1087. doi: 10.1136/jnnp.2004.056275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kallel N, Saidani A, Kotti A, et al. Coronavirus disease 19 (COVID-19) and Cerebral venous sinus thrombosis (CVST): A case series and review of the literature. Clin Case Rep. 2022;10(8):e6143. doi: 10.1002/ccr3.6143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bolaji P, Kukoyi B, Ahmad N, Wharton C. Extensive cerebral venous sinus thrombosis: A potential complication in a patient with COVID-19 disease. BMJ Case Reports. 2020;13:e236820. doi: 10.1136/bcr-2020-236820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abdulgayoom M, Abdelmahmuod E, Elfaki A, Halabiya MA. Cerebral venous sinus thrombosis as an unexpected complication of COVID-19 pneumonia. Cureus. 2021;13(7):e16498. doi: 10.7759/cureus.16498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asif R, O’ Mahony MS. Rare complication of COVID-19 presenting as isolated headache. BMJ Case Rep. 2020;13(10):e239275. doi: 10.1136/bcr-2020-239275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Solano D, Fu L, Czyz CN. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2024. Jan 28, 2023. Aug 28, Viral conjunctivitis. [PubMed] [Google Scholar]
- 10.Korathanakhun P, Petpichetchian W, Sathirapanya P, Geater SL. Cerebral venous thrombosis: Comparing characteristics of infective and non-infective aetiologies: A 12-year retrospective study. Postgrad Med J. 2015;91(1082):670–674. doi: 10.1136/postgradmedj-2015-133592. [DOI] [PubMed] [Google Scholar]
- 11.Dmytriw AA, Song JSA, Yu E, Poon CS. Cerebral venous thrombosis: State of the art diagnosis and management. Neuroradiology. 2018;60(7):669–685. doi: 10.1007/s00234-018-2032-2. [DOI] [PubMed] [Google Scholar]
- 12.Timóteo Â, Inácio N, Machado S, Pinto AA, Parreira E. Headache as the sole presentation of cerebral venous thrombosis: A prospective study. J Headache Pain. 2012;13(6):487–490. doi: 10.1007/s10194-012-0456-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barboza MA, Mejías C, Colin-Luna J, Quiroz-Compean A, Arauz A. Intracranial venous collaterals in cerebral venous thrombosis: Clinical and imaging impact. J Neurol Neurosurg Psychiatry. 2015;86(12):1314–1318. doi: 10.1136/jnnp-2014-309717. [DOI] [PubMed] [Google Scholar]