Abstract
CONTEXT:
The mandibular canal (MC) is an essential landmark that should be considered before any surgeries. Therefore, accurately assessing the location and characteristics of the MC in cone beam computed tomography (CBCT) imaging is very important.
AIMS:
To determine the characteristics of the MC in relation to adjacent anatomical structures in CBCT projections.
SETTINGS AND DESIGN:
The convenience sampling method.
METHODS AND MATERIAL:
This was a retrospective study of 112 CBCT images of Vietnamese patients aged 18 to 69 years, taken for clinical indications between 2018 and 2023. The evaluation was carried out by comparing and arranging the anatomical structures of different planes in three-dimensional space to assess and measure relevant dimensions.
STATISTICAL ANALYSIS USED:
Independent samples T-test.
RESULTS:
The average diameter of the MC from the apex of the second premolar to the distal apex of the second molar, if there were no missing teeth in this segment, was 2.58 ± 0.52 mm (right) and 2.55 ± 0.54 mm (left). If there were a missing tooth in this segment, the measurements were 2.51 ± 0.79 mm (right) and 2.47 ± 0.45 mm (left). The difference between the two sides regarding the presence or absence of a missing tooth was not statistically significant.
CONCLUSIONS:
The precise localization of the MC related to the tooth apex and the diameter of the MC can vary in each person. CBCT indications should be considered when establishing treatment planning to avoid damaging the inferior alveolar nerve in the MC.
Keywords: CBCT, cone beam computed tomography, inferior alveolar nerve, mandibular canal, tooth apex
Introduction
The mandibular canal (MC) begins in the mandibular foramen on the medial surface of the ascending mandibular ramus. It runs obliquely downward and forward in the ramus and then horizontally forward in the body until the mental foramen. It carries an inferior alveolar neurovascular bundle, responsible for sensation and blood supply to the mandibular teeth, interdental papillae, and periodontal and alveolar bone tissues. The lowest position of the MC is about 8–10 mm from the lower border of the mandible. It was mentioned that the MC might have different anatomic configurations in the vertical plane. For example, the canal may run lower when it proceeds anteriorly, have a sharp decline, or drape downward in a catenary shape. Variations are largely influenced by individuals, genders, ages, races, the assessing technique used, and degrees of edentulous alveolar bone atrophy.[1]
The MC is an important landmark that should be considered before any surgeries in the posterior mandible as the inferior alveolar nerve (IAN) block, sagittal ramus osteotomy, mandibular third molar surgery, and dental implant replacement. Therefore, accurately assessing the location, characteristics, and related factors of the MC in CBCT imaging is very important to improve treatment planning and control the risk of nerve and blood vessel damage.[2,3,4]
Demanding for implant surgeries, wider availability of three-dimensional exams, and lack of clear definitions in the literature indicate that features of anatomical variations should be reconsidered. The objective of the study was to evaluate features of anatomical variations related to the MC, such as bifid canals, the anterior loop of the mental nerve, and corticalization of the MC.[5] IAN injury is a serious complication in mandibular molar extraction surgery. Determining whether the tooth apex location is truly related to IAN or not is an important step before treatment planning.[6] The avoidance of surgical complications remains a challenging aspect in the field of surgery.[7] Therefore, this issue needs to be reconsidered for a more convincing research study.
The radiographic appearance usually involves a radiolucent zone lined by superior and inferior corticated borders of different variations, which may explain why the MC is hard to visualize in some cases. According to the American Academy of Oral and Maxillofacial Radiology, CBCT should be considered as the imaging modality of choice for dental implant treatment planning as the deficiencies of two-dimensional imaging techniques for the accurate location of the MC are well documented. Furthermore, when evaluating various tomographic techniques for pre-implant treatment planning, the posterior mandible has often been chosen as the test for resize localization of the MC. CBCT can display important anatomical structures as three-dimensional images with high resolution, allowing them to be measured accurately.[4,8] Currently, CBCT imaging has allowed us to overcome the limitations of conventional radiographs by providing high-resolution imaging of craniofacial structures without magnification or distortion.[9] Therefore, it is increasingly used in dental treatment, especially in dental implant replacement.[10]
Although CBCT imaging is a valuable asset in the assessment of sites for implant placement, it is unable to consistently provide visualization and identification of the MC in all instances, and careful evaluation of the implant site is necessary to avoid impingement or violation of vital structures. CBCT cross-sectional imaging is a valuable tool for the identification of vital anatomic structures as part of treatment planning but is not without limitations for the identification of all anatomic structures.[8]
The purpose of this study was to determine the MC in CBCT images and whether the visibility of the MC is affected by gender, location, and/or age.
Subjects and Methods
In this retrospective study, we reviewed 112 random CBCT images of Vietnamese patients taken for various clinical indications between 2018 and 2023 at the Can Tho University of Medicine and Pharmacy Hospital, conducted from June 2023 to June 2024. The prevailing data, including gender and edentulous assessment due to any tooth absence/presence, were also chosen to assess the correlation. The research was approved by the Research Ethics Committee of Can Tho University of Medicine and Pharmacy following the inclusion criteria: patients aged 18–69 years, with a symmetrical mandible; one missing tooth was allowed (in the following positions: the second premolar, the first molar, or the second molar on each third and fourth dental arches); and all CBCT images needed to be at a high enough resolution to identify the mandibular structure in detail, with a CBCT voxel size approximate or equal to 0.3 mm.[2,11,12,13,14] Exclusion criteria were patients with insufficient information, having teeth with a part apical closure or apical resorption, presence of unerupted or partially erupted teeth, mixed teeth, pathological mandibular lesions, a history of mandibular fractures, and surgeries.[2,11,13,14,15]
The fundamental indicators in this study included the correlation between the MC and the apex of the teeth at the following positions: the second premolar, the mesial apex of the first molar, the distal apex of the first molar, the mesial apex of the second molar, the distal apex of the second molar, and the diameter of the mandibular canal corresponding to the teeth positions mentioned above. Positions used the vertical plane and were rotated to address the appropriate axis so that the plane cut through the apex and was perpendicular to the MC at the comparable positions [Figure 1]. There were six positions: lingual contact (LiC), buccal contact (BC), lower contact (LoC), lingual noncontact (LiN), buccal noncontact (BN), and lower noncontact (LoN) according to the system coordinate based on Wang’s classification (2015) [Figure 2]. The diameter was stored as a measuring tool at a perpendicular location to the tooth [Figure 3].
Figure 1.
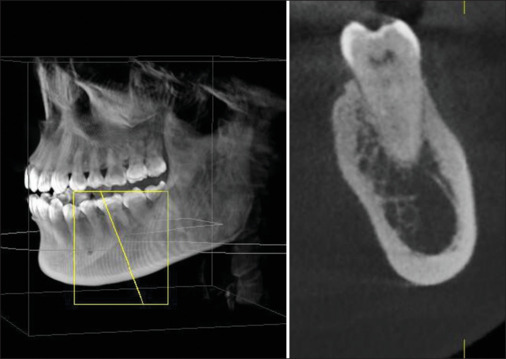
The sagittal plane has been appropriately rotated to pass through the apex and intersect perpendicular to the axis of the MC at the location of the mesial apex of the first molar
Figure 2.
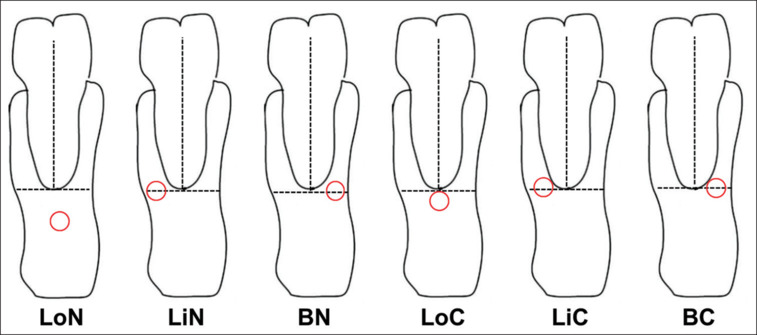
Guidelines for assessing the correlation of the MC. LiC - Lingual contact, BC - Buccal contact, LoC - Lower contact, LiN - lingual noncontact, BN - buccal noncontact and LoN - Lower noncontact
Figure 3.
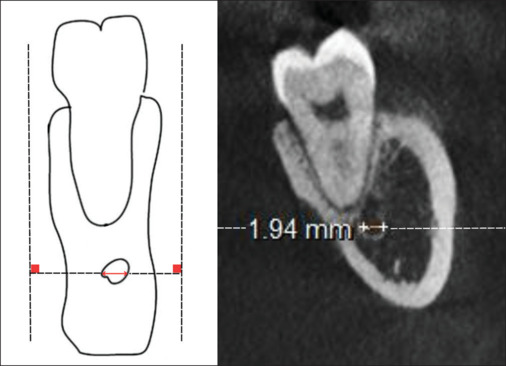
Corresponding diameter of the MC at the mesial apex of the first molar
We selected the sample using the convenience sampling method while complying with the sampling method. All the images were taken with a CBCT scanner: Sirona Orthophos SL 3D (Sirona, Germany), with a basic voxel size of 0.08 mm; a tube current and voltage of 3.0–16.0 mA and 60–90 kV, respectively; and a scan time of 14.9 s, and the cylindrical volume (field of view) measured 40–40 mm, 60–60 mm, or 80–80 mm. Scanning images were processed using GALILEOS software version 1.8 (Sirona, Germany) on a Samsung computer screen (LF27T350FHEXXV, Korea), following the manufacturer’s standard techniques and posture. Assembling data were imported into Microsoft Excel 2020 and Google Drive software, followed by SPSS Statistics 22.0 for analysis and accomplishment. CBCT projections were taken by a dental radiological technologist. The evaluation process was carried out by comparing and arranging the anatomical structures to different planes in three-dimensional (frontal, transverse, and sagittal) space to assess and measure relevant dimensions.
To avoid mistakes during the measurement of CBCT, all stages were verified by one examiner. The researcher’s consistency was determined as follows: After sampling was completed, 20 films were randomly selected from the total number of samples to be plotted and remeasured using the same method and checker over a period of at least 45 days (test–retest method). The statistics from the second measurement were compared to the first measurement using the Pearson correlation coefficient.
Results
From 112 CBCT images, 55 and 57 images belonged to men and women, respectively. The mean age of the patients was 33.19 years (SD ± 10.76). All results were expressed as mean ± standard deviation.
On the right, the average diameter of the MC at the apex of the examined teeth gradually decreased from the apex of the second premolar to the distal apex of the first molar. Then, it increased again at the distal apex of the second molar. The measurements for each position were as follows: 2.53 ± 0.66 mm, 2.44 ± 0.48 mm, 2.39 ± 0.41 mm, 2.44 ± 0.44 mm, and 2.50 ± 0.53 mm. When considering gender differences, the increase and decrease follow the same order as mentioned above. For men, the measurements were 2.75 ± 0.70 mm, 2.55 ± 0.43 mm, 2.51 ± 0.39 mm, 2.55 ± 0.42 mm, and 2.55 ± 0.45 mm. For women, the measurements were 2.32 ± 0.56 mm, 2.34 ± 0.50 mm, 2.29 ± 0.40 mm, 2.35 ± 0.44 mm, and 2.39 ± 0.59 mm. At each position corresponding to the apex, the average diameters of men were larger than that of women [Table 1].
Table 1.
Average diameter of the mandibular canal at the apex of the examined teeth (right)
| Gender | Apex of the second premolar (mm) | Mesial apex of the first molar (mm) | Distal apex of the first molar (mm) | Mesial apex of the second molar (mm) | Distal apex of the second molar (mm) | Number |
|---|---|---|---|---|---|---|
| Male | 2.75±0.70 | 2.55±0.43 | 2.51±0.39 | 2.55±0.42 | 2.55±0.45 | 55 |
| Female | 2.32±0.56 | 2.34±0.50 | 2.29±0.40 | 2.35±0.44 | 2.39±0.59 | 57 |
The left side has the same regulations; the average diameters of the MC were measured at positions from the apex of the second premolar to the distal apex of the second molar, yielding the following results: 2.49 ± 0.61 mm, 2.41 ± 0.63 mm, 2.40 ± 0.70 mm, 2.53 ± 0.59 mm, and 2.54 ± 0.55 mm. When considering gender differences, at each position corresponding to the apex, the average diameters of men were larger than that of women [Table 2].
Table 2.
Average diameters of the mandibular canal at the apex of the examined teeth (left)
| Gender | Apex of the second premolar (mm) | Mesial apex of the first molar (mm) | Distal apex of the first molar (mm) | Mesial apex of the second molar (mm) | Distal apex of the second molar (mm) | Number |
|---|---|---|---|---|---|---|
| Male | 2.59±0.67 | 2.53±0.71 | 2.45±0.71 | 2.59±0.55 | 2.63±0.57 | 55 |
| Female | 2.40±0.53 | 2.28±0.53 | 2.35±0.68 | 2.47±0.62 | 2.46±0.53 | 57 |
On the other hand, when considering the average diameter of the MC from the apex of the second premolar to the distal apex of the second molar, the results for males and females were as follows: on the right side, 2.72 ± 0.95 mm for males and 2.35 ± 0.35 mm for females (P = 0.007, independent samples T-test), and on the left side, 2.56 ± 0.51 mm for males and 2.41 ± 0.41 mm for females (P = 0.089, independent samples T-test). However, when evaluating the correlation between these average diameters and gender, statistically significant differences were only found on the right.
The average diameter of the MC from the apex of the second premolar to the distal apex of the second molar (if there was no missing tooth in this segment) was 2.46 ± 0.30 mm on the right and 2.49 ± 0.36 mm on the left. If there was a missing tooth in this segment, the measurement was 2.46 ± 0.51 mm on the right and 2.49 ± 0.57 mm on the left. The difference between the two sides regarding the presence or absence of a missing tooth was not statistically significant [Table 3].
Table 3.
Average diameter of the mandibular canal from the apex of the second premolar to the distal apex of the second molar
| Remaining tooth (mm) | Missing tooth (mm) | P | |
|---|---|---|---|
| Right | 2.58±0.52 | 2.51±0.79 | 0.694 |
| Left | 2.55±0.54 | 2.47±0.45 | 0.513 |
Independent samples t-test
When evaluating the relative position between the tooth apex and the longitudinal section of the MC at the corresponding position, six values were obtained: LiC, BC, LoC, LiN, BN, and LoN. On the right side, the highest corresponding results from the apex of the second premolar to the distal apex of the second molar all showed lower noncontact rates: 72.48%, 73.40%, 73.40%, 69.16%, and 58.88%. Similar results were obtained on the left side with the following ratios: 79.09%, 74.51%, 66.67%, 60.75%, and 60.75%. When evaluating the correlation according to Koivisto, the corresponding results of the MC compared to the second molar were as follows: 18.75% buccal, 81.25% lower, and 0% lingual; for the first molar: 11.36% buccal, 68.18% lower, and 20.45% lingual; and for the second premolar: 12.63% buccal, 63.16% lower, and 24.21% lingual [Table 4].
Table 4.
Evaluating the relative position between the tooth apex and the longitudinal section of the MC at the corresponding position
| Respective location | Apex of the second premolar | Mesial apex of the first molar | Distal apex of the first | Mesial apex of the second molar | Distal apex of the second molar | |
|---|---|---|---|---|---|---|
| Right | LiC | 0.92% | 0.00% | 0.00% | 0.93% | 5.61% |
| LoC | 6.42% | 2.13% | 2.13% | 2.81% | 11.21% | |
| BC | 0.92% | 1.06% | 1.06% | 0.93% | 0.00% | |
| LiN | 6.42% | 15.96% | 15.96% | 15.89% | 10.28% | |
| LoN | 72.48% | 73.40% | 73.40% | 69.16% | 58.88% | |
| BN | 12.84% | 7.45% | 7.45% | 10.28% | 14.02% | |
| Left | LiC | 0.91% | 1.96% | 3.92% | 2.81% | 3.74% |
| LoC | 4.55% | 0.98% | 1.96% | 8.41% | 13.08% | |
| BC | 0.00% | 0.98% | 0.00% | 2.80% | 1.87% | |
| LiN | 5.45% | 16.67% | 21.57% | 13.08% | 5.61% | |
| LoN | 79.09% | 74.51% | 66.67% | 60.75% | 60.75% | |
| BN | 10% | 4.90% | 5.88% | 12.15% | 14.95% |
LiC=Lingual contact, BC=Buccal contact, LoC=Lower contact, LiN=lingual noncontact, BN=buccal noncontact and LoN=Lower noncontact
Discussion
Conventional two-dimensional presurgical radiology (panoramic radiographs, periapical radiographs, etc.) often fails to show anatomical structures such as the MC and the apex of the examined teeth. Contemporary imaging techniques such as CT may be particularly suitable in preoperative treatment planning as three-dimensional visualization and high-resolution analysis of the entire body of the mandible provide adequate information for the location of these structures.[16]
In 2016, Koivisto and colleagues conducted the study “Evaluation of the visibility and the course of the mandibular incisive canal and the lingual foramen using cone-beam computed tomography”. Respective locations of the MC to the teeth (buccal, lower, or lingual) were as follows: second molar (57% buccal, 40% lower, and 3% lingual), first molar (18% buccal, 55% lower, and 27% lingual), and second premolar (33% buccal, 55% lower, and 11% lingual). The average diameter of the MC along the length of the canal from the second molar to the second premolar was 3.03 mm on the left and 2.91 mm on the right.[12] The result did not show much disparity; however, this could be explained by the variety of demographics, scanning equipment quality, and types of analysis software.
For the mandibular first molars with two roots, the distance from the mesial and distal apex to the MC was 6.41 ± 2.67 mm and 5.82 ± 2.79 mm, respectively. For the mandibular first molars with three roots, the distances from the mesial, buccal, and lingual apexes to the MC were 7.02 ± 2.16 mm, 6.89 ± 2.26 mm, and 8.02 ± 2.33 mm, respectively. Therefore, it can be concluded that the MC is located further from the apex in older people. There are differences in the distance between the MC and some anatomical landmarks, with dimensions being larger in males than in females.[17] Differences due to anthropological factors and the use of different CBCT analysis software also affect the results.
The research by Christiano de Oliveira-Santos and colleagues showed that most MCs are 2–4 mm in diameter.[5] This result seems to correspond with our results. Although the diameter of the MC varies in each individual according to their gender and race, the results of the average diameter in this study could represent for any racial groups.
Conclusion
The precise localization of the MC relative to the tooth apex and the diameter of the MC can vary in each person. CBCT provides cross-sectional images that can help surgeons with oral disease diagnosis and treatment processes. CBCT indications should be considered when establishing treatment planning to avoid damaging the IAN block in the MC. Otherwise, when CBCT conditions are not ideal, having enough knowledge about anatomical structures is necessary to realize the risk of bias during treatment.
Key messages
The MC is an essential landmark that should be considered before any surgeries. CBCT indications should be considered when establishing treatment planning to avoid damaging the inferior alveolar nerve in the MC.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
I would like to extend my deep appreciation to Can Tho University of Medicine and Pharmacy that provided financial support and facilitated the smooth operation of our research activities. Their investment in our work enabled us to conduct this study and make meaningful contributions to the field.
I would like to express my gratitude to the Can Tho University of Medicine and Pharmacy Hospital that provided location and equipment support for this research. The support provided enabled us to conduct data collection, analysis. These resources have been instrumental in conducting experiments, gathering data, and analyzing findings.
I also would like to acknowledge the Faculty of Odonto-Stomatology, Can Tho University of Medicine and Pharmacy for their support and provision of resources throughout the course of this research. It played a crucial role in the successful execution of this study and the attainment of our research goals.
I want to express my heartfelt appreciation to all the participants who voluntarily shared their personal information and their time for this research. Without their willingness to contribute, this study would not have been possible.
Lastly, I am deeply thankful to the members of the research team, Lam Nguyen Le, Loc Truong Tan, Anh The Thien Dang, My Hoan Truong, Duyen Kim Ngoc Huynh, Luan Minh Nguyen and collaborators for their contributions, expertise and collaborative spirit to the successful completion of this study. Their dedication and hard work have significantly enhanced the quality and depth of this study.
In conclusion, I am immensely grateful to all the individuals and organizations who contributed to this research. Their expertise, valuable insights and unwavering support throughout the project have been instrumental in the accomplishment of our research goals.
Funding Statement
Nil.
References
- 1.Juodzbalys G, Wang H-L, Sabalys G. Anatomy of mandibular vital structures. Part I: mandibular canal and inferior alveolar neurovascular bundle in relation with dental implantology. J Oral Maxillofac Res. 2010;1:e2. doi: 10.5037/jomr.2010.1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahn B-S, Oh SH, Heo C-K, Kim G-T, Choi Y-S, Hwang E-H. Cone-beam computed tomography of mandibular foramen and lingula for mandibular anesthesia. Imaging Sci Dent. 2020;50:125–32. doi: 10.5624/isd.2020.50.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jung Y-H, Cho B-H. Radiographic evaluation of the course and visibility of the mandibular canal. Imaging Sci Dent. 2014;44:273–8. doi: 10.5624/isd.2014.44.4.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Takeshita Y, Shimizu M, Jasa GR, Weerawanich W, Okamura K, Yoshida S, et al. Prediction of detectability of the mandibular canal by quantitative image quality evaluation using cone beam CT. Dentomaxillofac Radiol. 2018;47:20170369. doi: 10.1259/dmfr.20170369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Oliveira-Santos C, Souza PHC, de Azambuja Berti-Couto S, Stinkens L, Moyaert K, Rubira-Bullen IRF, et al. Assessment of variations of the mandibular canal through cone beam computed tomography. Clin Oral Investig. 2012;16:387–93. doi: 10.1007/s00784-011-0544-9. [DOI] [PubMed] [Google Scholar]
- 6.Vinh KNK, Dan TTP, Tan LN. Clinical features and paraclinical of third molar tooth in the closed relationship with inferior alveolar nerve in coronectomy. Can Tho J Med Pharm. 2023;64:118–23. [Google Scholar]
- 7.Alshamrani AS, Tokhtah RA, Al-Omar A. Cone-beam computed tomography evaluation of prevalence and location of mandibular incisive canal in patients attending King Saud University Dental Hospital. J Orthod Sci. 2021;10:21. doi: 10.4103/jos.jos_108_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miles MS, Parks ET, Eckert GJ, Blanchard SB. Comparative evaluation of mandibular canal visibility on cross-sectional cone-beam CT images: A retrospective study. Dentomaxillofac Radiol. 2016;45:20150296. doi: 10.1259/dmfr.20150296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alhazmi N. Assessment of mandibular asymmetry in different skeletal malocclusions and vertical patterns in adult individuals: A cone-beam computed tomography study. J Orthod Sci. 2023;12:33. doi: 10.4103/jos.jos_112_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quang NVD, Lam LN, Khanh HQ. Evaluation of the accuracy of stereolithography surgical guide used in posterior mandibular dental implants. Can Tho J Med Pharm. 2022;53:112–20. [Google Scholar]
- 11.Mahnaz S, Mitra KK. CBCT assessment of mental foramen position relative to anatomical landmarks. Int J Dent. 2016;2016:5821048. doi: 10.1155/2016/5821048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koivisto T, Chiona D, Milroy LL, McClanahan SB, Ahmad M, Bowles WR. Mandibular canal location: Cone-beam computed tomography examination. J Endod. 2016;42:1018–21. doi: 10.1016/j.joen.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 13.Alam MK, Alhabib S, Alzarea BK, Irshad M, Faruqi S, Sghaireen MG, et al. 3D CBCT morphometric assessment of mental foramen in Arabic population and global comparison: Imperative for invasive and non-invasive procedures in mandible. Acta Odontol Scand. 2018;76:98–104. doi: 10.1080/00016357.2017.1387813. [DOI] [PubMed] [Google Scholar]
- 14.Feuerstein D, Costa-Mendes L, Esclassan R, Marty M, Vaysse F, Noirrit E. The mandibular plane: A stable reference to localize the mandibular foramen, even during growth. Oral Radiol. 2020;36:69–79. doi: 10.1007/s11282-019-00381-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dos Santos Oliveira R, Coutinho MR, Panzarella FK. Morphometric analysis of the mental foramen using cone-beam computed tomography. Int J Dent. 2018;2018:4571895. doi: 10.1155/2018/4571895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Makris N, Stamatakis H, Syriopoulos K, Tsiklakis K, van der Stelt PF. Evaluation of the visibility and the course of the mandibular incisive canal and the lingual foramen using cone-beam computed tomography. Clin Oral Implants Res. 2010;21:766–71. doi: 10.1111/j.1600-0501.2009.01903.x. [DOI] [PubMed] [Google Scholar]
- 17.Hoang DBT, Huynh KK, Tran NMD. Sectional Anatomical Distances in the Region of the First lower Molars on Cone Beam CT; Vietnam. Med. J. 2022:515.2. [Google Scholar]


