Abstract
Objective
Construction a troublemaking risk assessment tool to predict the risk of troublemaking for patients with severe mental disorders in the community of China.
Methods
28,000 cases registered in the Jiangsu Provincial Severe Mental Disorder Management System from January 2017 to December 2019 were collected. The risk factors of troublemaking among patients with severe mental disorders in the community were analyzed through Logistic regression analysis, then the troublemaking risk assessment tool was established and verified.
Results
The incidence of troublemaking among patients with severe mental disorders in the community was 7.15%. The results of multivariate logistic regression analysis showed that males, ≤ 44 years old, duration of disease ≤ 14 years, high school education and below, unemployed, subsistence allowances, schizophrenia, major symptoms > 1, psychiatric visits ≥ 1 time per year, unwilling to participate in community management and community rehabilitation activities, and delayed diagnosis < 2 months were risk factors for troublemaking. The above factors were incorporated into the nomogram model, and the area under the ROC curve of the nomogram model was 0.688 (95%CI: 0.563–0.726). The calibration curve proved that the probability predicted by the model was in good agreement with the actual probability.
Conclusion
The established troublemaking risk assessment tool for patients with severe mental disorders in the community based on Logistic regression analysis had good predictive performance, which could be applied to assess the probability of troublemaking among patients with severe mental disorders in the community.
Keywords: Prediction model, Troublemaking, Severe mental disorder, Community, China
Subject terms: Risk factors, Psychiatric disorders
Introduction
Under the influence of psychiatric symptoms such as command hallucinations and delusions, individuals with mental disorders are prone to disruptive behaviors, including harming others, damaging property, arson, and suicide. This is particularly true for patients with severe mental disorders, such as schizophrenia, intellectual disability with comorbid psychiatric disorders, bipolar disorder, schizoaffective disorder, paranoid psychosis, and epilepsy-related mental disorders, which can severely disturb public order and social stability1,2. In China, there are approximately 16 million individuals with severe mental disorders, with about 10% of them exhibiting disruptive behaviors3. By the end of 2018, the registered number of patients with severe mental disorders was 5,994,054, with a detection rate of 4.3% (5,994,054/1,379,837,956)4. Clearly, the number of diagnosed and managed severe mental disorder patients is significantly lower than the likely true number, posing an unpredictable risk of violent incidents to society. Recent studies on violent incidents involving patients with severe mental disorders in China reveal significant regional differences in the incidence rates, such as 3.9% in Shenzhen5, 11.93% in Shaoxing6, and 24.9% in Chengdu7. According to the authors’ previous research, the local incidence rate of violent incidents is 7.18%16. These variations may be due to differences in sample selection and community registration management policies across studies.
Patients with severe mental disorders, due to the instability of their condition and poor emotional and behavioral control, more frequently engage in suicidal behaviour or major criminal activities such as harming others or damaging property. Their violent behaviors are often characterized by concealment, severity, and recurrence, leading to substantial losses. These actions not only pose a serious threat to public safety but also place a heavy psychological and financial burden on their caregivers8. A recent domestic meta-analysis found that factors such as unemployment, inconsistent medication adherence, male gender, low education level, schizophrenia, being unmarried, and family history are risk factors for high-risk behaviors in patients with severe mental disorders9. International studies have also identified gender and age of onset as related to the risk of violence10.
In many Western countries, structured assessment tools such as the Violence Risk Screening (V-RISK-1)11; Brøset Violence Checklist (BVC)12; Psychopathy Checklist-Revised (PCL-R)13; Historical, Clinical, Risk Management-20 (HCR-20)14; and Level of Service Inventory-Revised (LSI-R)15, are widely used for violence risk assessment in forensic and general psychiatric settings. Although these tools are commonly used in clinical practice, their purposes, benefits, limitations, and abilities to predict future violence vary.
We found that machine learning methods for predicting violent risk behaviors in patients with schizophrenia are considered to have good accuracy and stability. In a systematic review of machine learning systems for risk assessment in schizophrenia patients16, it was observed that most models predicting violent risk used patients’ socio-demographic and clinical characteristics. Some studies found that factors such as age16–18, gender, and educational attainment19,20 are helpful in predicting violence risk. However, other studies reported that these demographic factors do not significantly correlate with the occurrence of violent behavior21.
Other research has linked the accumulation and types of stressors in patients’ histories22, different psychiatric prescriptions23,24, and scores from various tools such as the Brief Psychiatric Rating Scale (BPRS)19, the Positive and Negative Syndrome Scale (PANSS)19, the Insight and Treatment Attitudes Questionnaire (ITAQ)19, the Family APGAR19, the Social Support Rating Scale (SSRS)19, the Family Burden Scale of Disease (FBS)19, and the Social Disability Screening Schedule (SDSS)20 as factors associated with violence risk. Additionally, some studies have incorporated neurological imaging data19,21, biochemical markers25,26, and fMRI or COMT gene data27 to predict violence risk.
Moreover, several studies reported a positive correlation between the daily olanzapine equivalent dosage during previous hospitalizations and violence risk in schizophrenia patients28. Emergency factors such as a history of compulsory psychiatric treatment or separation from primary caregivers during childhood or adolescence were also found to be associated with violence risk29. The reliability of models in current research is typically expressed through the AUROC and Accuracy values, representing the reliability and validity of predictive models. The range of AUROC values reported in most studies is between 0.56 and 0.95, while Accuracy values range from 0.54 to 0.91, indicating considerable variability in model performance15.
Currently, domestic research is also limited to violence risk assessment in patients with schizophrenia. For example, Jiang Yizhou et al.30 used logistic regression analysis to create risk prediction models for violent behavior among community-dwelling schizophrenia patients of different genders. The study found that different risk factors should be considered to prevent violence risk in male and female community-dwelling schizophrenia patients, with strong predictive ability (AUC Male = 0.779; AUC Female = 0.822). Another study31, also using the same method, developed a comprehensive risk prediction model for violent behavior in community-dwelling schizophrenia patients. The AUC for the modeling cohort was 0.78 (CI: 0.74–0.81), which provides a certain reference value. Both studies were focused on schizophrenia patients. Another study32 targeted hospitalized schizophrenia patients and constructed a predictive model for impulsive behavior risk using the same method. The AUC was 0.769, but the sensitivity was relatively low at 0.59. Additionally, some domestically developed models for assessing the risk of mental illness showed predictive validity mostly ranging from poor to moderate levels33.
Although many violence risk assessment tools abroad can be used to help predict the risk of violence, their applicability to the economic and cultural context of China remains a topic for discussion. Currently, reports on the prediction of violent behavior in community-dwelling individuals with severe mental disorders in China are still relatively scarce. Some studies have preliminarily developed a risk assessment tool for violent behavior in this population34. This research ultimately formulated a Severe Mental Disorders Violence Risk Assessment Scale, consisting of five dimensions and 19 items, with good reliability and validity. In addition to basic information, the scale also includes family information, economic status, disease type, history of violent behavior, and treatment status, providing a foundation for our research. However, we must also acknowledge that certain biological factors influencing violent behavior in psychiatric patients, such as genetic factors, remain difficult to measure. Nonetheless, our research findings indicate that environmental factors and patients’ socio-demographic characteristics provide a certain degree of predictability for violent incidents.
Although monitoring, assessing, predicting, preventing, and controlling violent behaviors in patients with severe mental disorders has become an important part of mental health services35, few studies focus on the risk factors for disruptive behaviors, such as diagnostic and treatment information, social support, and symptoms36,37. This study aims to develop a risk assessment tool for disruptive behaviors among patients with severe mental disorders based on the cultural context. This tool is intended to provide community workers with an effective means of early identification of the risk of disruptive behaviors in patients with severe mental disorders in Chinese communities.
Materials and methods
Objects
A total of 28 000 patients with severe mental disorders (schizophrenia, mental retardation with mental disorders, bipolar disorder, schizoaffective disorder, Paranoid psychosis, mental disorder caused by epilepsy)38 registered in the Jiangsu Provincial Severe Mental Disorder Management System from January 2017 to December 2019 were selected as the research objects. Inclusion criteria: (1) ≥ 14 years old; (2) Have a clear diagnosis of mental illness and a reporting unit. Patients with missing basic information and those who moved out of the management system were excluded.
The basic information, diagnosis and treatment information, social support and accident information of the research subjects were collected. Basic information included gender, age, education level, occupation, marital status, and economic status, etc.; medical information includd diagnosis and classification, course of disease, and duration of medication; social support included subsistence allowances, disability certificates, and participation community management of basic public health projects, community rehabilitation services, etc.; troublemaking behaviors were confirmed by the Municipal Public Security Bureau. Poverty is defined as a household per capita monthly income lower than twice the minimum subsistence income standard in Wuxi.
Construction of the nomogram model
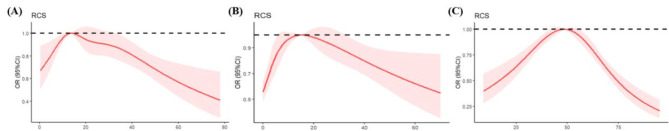
Variables with P < 0.05 in the univariate analysis were included in the multivariate Logistic regression analysis. For continuous variables (age, course of disease, duration of medication, and delayed months), we used restricted cube plots to explore their association with accidents. It was found that the first three exhibited a nonlinear relationship (Fig. 1). Since delayed months appeared to be linear, we recoded the variables, and age, medication, disease duration and delayed months were all reclassified according to their respective P33 and P67. The codes of the variables were shown in Table 1. The risk factors obtained from the Logistic regression analysis were subjected to construct a nomogram of the incidence of troublemaking among patients with severe mental disorders in the community. In the model, β represents the regression coefficients of each risk factor in the logistic regression analysis. The constant term α is the natural logarithm of the ratio between the incidence rate of violent behavior and the non-incidence rate during the study period, calculated using the formula: α=ln[P/(l—P)]. The logistic function for predicting violent behavior among patients with severe mental disorders in the community is expressed as logit(P)αββ1×1β2×2β3×3……βnXn where Xn represents the nth risk factor, and βn represents the regression coefficient for the nth risk factor. Based on the scores assigned to each risk factor, the score range is calculated. The probability of violent behavior is then computed using the formula P = elogit(P)/(1 + elogit(P)), and a corresponding table is created that maps the score to the predicted risk probability.
Fig. 1.
RCS analysis of course of disease (A), duration of medication (B) and age (C).
Table 1.
Variable assignment for multivariate logistic regression analysis.
| Variable | Assignment |
|---|---|
| Troublemaking | 0 = no, 1 = yes |
| Age | 0 = 45–59, 1 = ≤ 44, 2 = ≥ 60 |
| Gender | 0 = female, 1 = male |
| Educational level | 0 = college and above, 1 = high school and below |
| Occupation | 0 = on duty of retired, 1 = unemployed |
| Basic living allowances | 0 = no, 1 = yes |
| Schizophrenia | 0 = no, 1 = yes |
| Disease duration (years) | 0 = 15–27, 1 = ≤ 14, 2 = ≥ 28 |
| Medication duration (years) | 0 = 6–18, 1 = ≤ 6, 2 = ≥ 19 |
| No of previous major symptoms | 0 = 0–1, 1 = > 1 |
| No. of psychiatric visits/year | 0 = 0, 1 = ≥ 1 |
| Agree to community management | 0 = yes, 1 = no |
| Disability certificate | 0 = no, 1 = yes |
| Participate in community rehabilitation activities | 0 = yes, 1 = no |
| Delayed time (months) | 0 = > 12,1 = < 2, 2 = 2–12 |
Statistical analysis
The measurement data were expressed by x ± s, and the t test was used for comparison between two groups; the enumeration data were expressed by rate or composition ratio, and the χ2 test was used for comparison between groups. Multivariate logistic regression was used to analyze the influencing factors of troublemaking. R 4.30 software was used to draw restricted cube plots, nomograms, calibration curves, ROC curves, and related data analysis. The test level ɑ=0.05. We validated the model using data from 2,680 newly identified severe mental illness patients from 2022 to 2023. The reliability and effectiveness of the model were assessed through the area under the ROC curve (AUC) and its 95% confidence interval, accuracy, sensitivity, and specificity.3 Results.
Univariate analysis of troublemaking among patients
Excluding 47 cases of severe incomplete information and data duplication, a total of 27 953 people were included in this study, including 13 188 males (47.18%) and 14 765 females (52.82%), aged (51.0 ± 15.7) years old, and disease duration (22.85 ± 14.58) years, and the duration of medication was (14.97 ± 13.42) years. The average troublemaking rate of patients with severe mental disorders in the community was 7.15% (1998/27 953). There were significant differences between gender, age, education level, occupation, marital status, economic status, subsistence allowances, diagnosis classification, duration of disease (years), duration of medication (years), whether to participate in community management, disability certificate, the number of major mental symptoms, the number of psychiatric visits per year, and whether to participate in community rehabilitation activities (P < 0.05), see Table 2.
Table 2.
Univariate analysis of troublemaking among patients.
| Factors | No. of non-troublemaking (%) | No. of troublemaking (%) | P |
|---|---|---|---|
| Gender | < 0.001 | ||
| Male | 12,000(46.2) | 1188(59.5) | |
| Female | 13,955 (53.8) | 810 (40.5) | |
| Age | < 0.001 | ||
| ≤44 | 8921 (34.4) | 696 (34.8) | |
| 45–59 | 8154 (31.4) | 762 (38.1) | |
| ≥60 | 8880 (34.2) | 540 (27.0) | |
| Education level | 0.006 | ||
| High school and below | 24,056 (92.7) | 1885 (94.3) | |
| College and above | 1899(7.3) | 113(5.7) | |
| Occupation | < 0.001 | ||
| Unemployed | 8163(31.5) | 850(42.5) | |
| On duty or retired | 17,792 (68.5) | 1148 (57.5) | |
| Marital status | < 0.001 | ||
| Unmarried | 8496 (32.7) | 734 (36.7) | |
| Married | 14,430 (55.6) | 978 (48.9) | |
| Widowed | 990 (3.8) | 64 (3.2) | |
| Divorce | 1706 (6.6) | 209 (10.5) | |
| Unknown | 333 (1.3) | 13 (0.7) | |
| Poverty | < 0.001 | ||
| Yes | 6150(23.7) | 636(31.8) | |
| No | 19,805 (76.3) | 1362 (68.2) | |
| Basic living allowances | < 0.001 | ||
| Yes | 4355 (16.8) | 501 (25.1) | |
| No | 21,600(83.2) | 1497(74.9) | |
| Schizophrenia | < 0.001 | ||
| No | 12,035(46.4) | 691(34.6) | |
| Yes | 13,920 (53.6) | 1307 (65.4) | |
| Disease duration (years) | 0.005 | ||
| ≤14 | 8544 (32.9) | 667 (33.4) | |
| 15–27 | 8779 (33.8) | 732 (36.6) | |
| ≥28 | 8632 (33.3) | 599 (30.0) | |
| Medication duration (years) | < 0.001 | ||
| ≤6 | 9000 (34.7) | 557 (27.9) | |
| 6–18 | 8017 (30.9) | 717 (35.9) | |
| ≥19 | 8938 (34.4) | 724 (36.2) | |
| Agree to community management | < 0.001 | ||
| Yes | 23,816 (91.8) | 1768 (88.5) | |
| No | 2139(8.2) | 230(11.5) | |
| Disability certificate | < 0.001 | ||
| No | 14,354(55.3) | 997(49.9) | |
| Yes | 11,601 (44.7) | 1001 (50.1) | |
| No. of previous major symptoms | < 0.001 | ||
| ≤ 1 | 2342 (9.0) | 435 (21.8) | |
| >1 | 23,613(91.0) | 1563(78.2) | |
| No. of psychiatric visits/year | < 0.001 | ||
| ≥ 1 | 13,258 (51.1) | 1426 (71.4) | |
| 0 | 12,697(48.9) | 572(28.6) | |
| Delayed time (months) | 0.112 | ||
| <2 | 8660 (33.4) | 621 (31.1) | |
| 2–12 | 8381 (32.3) | 669 (33.5) | |
| >12 | 8914 (34.3) | 708 (35.4) | |
| Participate in community rehabilitation activities | < 0.001 | ||
| No | 24,871(95.8) | 1945(98.3) | |
| Yes | 1084 (4.2) | 53 (1.7) |
Multivariate logistic regression analysis of troublemaking among patients
Statistically significant variables and delayed time (month) in the univariate analysis results were included in the multivariate logistic regression analysis model. After screened by the stepwise method, the three variables of medication duration, economy, and marriage were excluded. The results showed that, male, ≥ 60 years old, disease duration ≤ 14 years, high school education and below, unemployed, subsistence allowances, schizophrenia, major symptoms > 1, psychiatric visits ≥ 1 time/year, unwilling to participate in community management and community rehabilitation activities, and delayed diagnosis < 2 months were risk factors for troublemaking, and the differences were statistically significant (P < 0.05). See Table 3.
Table 3.
Multivariate logistic regression analysis of factors related to troublemaking.
| Coefficients | Estimate | SE | OR(95%CI) | Z | P |
|---|---|---|---|---|---|
| intercept | -2.296 | 0.159 | -14.402 | < 0.001 | |
| Age ≤ 44 | -0.172 | 0.060 | 0.842(0.751 ~ 0.944) | -2.876 | 0.004 |
| Age ≥ 60 | -0.381 | 0.060 | 0.683(0.604 ~ 0.772) | -6.091 | < 0.001 |
| Male | -0.491 | 0.049 | 0.612(0.556 ~ 0.673) | -10.122 | < 0.001 |
| Disease duration ≤ 14 years | 0.151 | 0.059 | 1.163(1.036 ~ 1.306) | 2.083 | 0.037 |
| Disease duration ≥ 28 years | -0.038 | 0.062 | 0.963(0.853 ~ 1.088) | -1.027 | 0.305 |
| High school and below | 0.430 | 0.104 | 1.204(1.038 ~ 1.356) | 4.059 | < 0.001 |
| Unemployed | 0.329 | 0.050 | 1.389(1.261 ~ 1.531) | -6.750 | < 0.001 |
| Have basic living allowances | 0.334 | 0.058 | 1.397(1.246 ~ 1.563) | 5.750 | < 0.001 |
| Schizophrenia | 0.187 | 0.054 | 1.206(1.084 ~ 1.342) | 3.363 | < 0.001 |
| No. of previous major symptoms > 1 | 0.764 | 0.061 | 1.654(1.348 ~ 1.953) | 12.587 | < 0.001 |
| No. of psychiatric visits/year ≥ 1 | 0.755 | 0.057 | 2.127(1.905 ~ 2.378) | 13.321 | < 0.001 |
| Agree to community management | 0.577 | 0.113 | 1.781(1.437 ~ 2.236) | 5.101 | < 0.001 |
| Have disability certificate | 0.090 | 0.050 | 1.094(0.992 ~ 1.207) | 1.767 | 0.077 |
| Participate in community rehabilitation activities | 0.632 | 0.093 | 1.880(1.563 ~ 2.248) | 6.856 | < 0.001 |
| Delayed diagnosis < 2 months | -0.250 | 0.059 | 0.779(0.697 ~ 0.870) | -4.216 | < 0.001 |
| Delayed diagnosis 2–12 months | -0.097 | 0.061 | 0.907(0.804 ~ 1.022) | -1.596 | 0.111 |
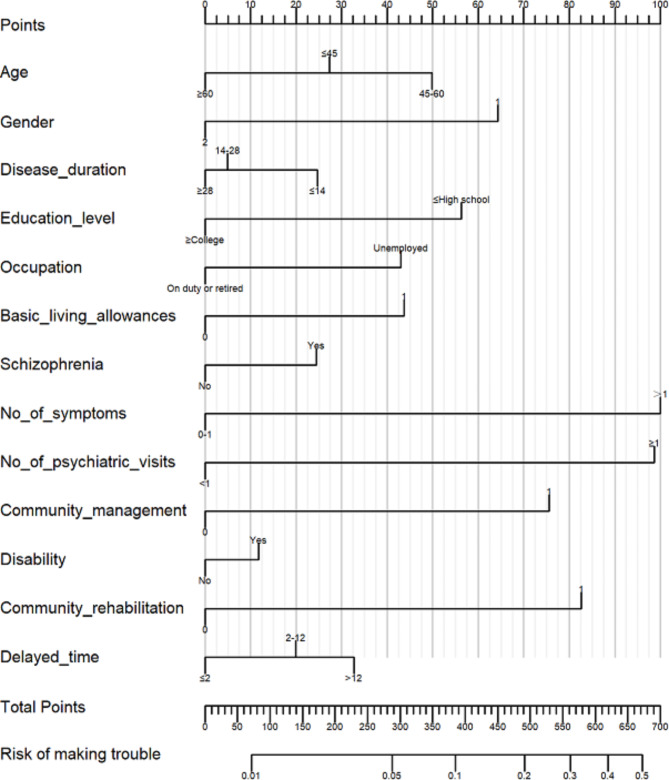
Construction and performance of nomogram prediction model
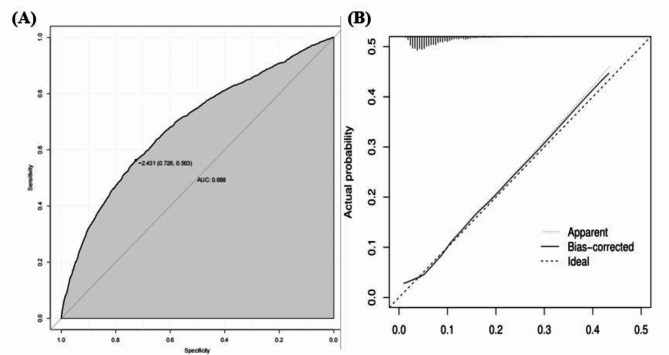
On the basis of Logistic regression analysis, age, gender, course of disease, education level, occupation, subsistence allowances, diagnostic classification, duration of medication, number of previous main symptoms, number of psychiatric visits per year, whether to participate in community management, whether to have disability certificate, whether to participate in community rehabilitation services were included in the nomogram analysis. The value of each of variable was given a score on the point scale axis. A total score could be easily calculated by adding each single score and, by projecting the total score to the lower total point scale, we were able to estimate the probability of the risk of accidents and disasters. See Fig. 2. Then, the ROC curve was applied to evaluate the discriminative ability of the nomogram model. The area under the ROC curve of the nomogram model was 0.688 (95% CI: 0.563 ~ 0.726), and the predictive performance was at a medium to high level (Fig. 3A). The calibration curve of the nomogram showed that the troublemaking probability predicted by the nomogram was in good agreement with the actual probability (Fig. 3B).
Fig. 2.
A nomograph for predicting the risk of troublemaking among patients with severe mental disorders in the community.
Fig. 3.
Verification of the nomogram prediction model, (A) ROC curve, (B) calibration curve.
Establishment of the troublemaking risk assessment tool
Transform according to the regression coefficient β of each factor in the model, so as to assign scores to each risk factor, gender (male = 64 points, female = 0 points), age (≤ 44 = 27 points, 45–59 = 50 points, > 60 = 0 points), duration of disease (≤ 14 years = 25 points, 15–27 years = 5, ≥ 28 years = 0 points), education level (high school and below = 56 points, college and above = 0 points), occupation status (on duty or retired = 0 points, unemployed = 43 points), subsistence allowances (yes = 44 points, no = 0 points), diagnostic classification (schizophrenia = 24 points, non-schizophrenia = 0 points), number of main symptoms (0–1 = 0 points, > 1 = 100 points), the number of psychiatric visits per year (0 = 0 points, ≥ 1 = 99 points), community management services (participation = 0 points, non-participation = 73 points ), disability certificate (no = 0 points, yes = 12 points), delayed diagnosis (< 2 months = 0 points, 2–12 months = 20 points, > 12 months = 33 points), community rehabilitation activities (participation = 0 points, not participating = 83 points). See Table 4. The correspondence table between assessment score and risk prediction probability was shown in Table 5.
Table 4.
The assigned scores of each risk factor.
| Risk factor | Categories | Points |
|---|---|---|
| Gender | ||
| Female | 0 | |
| Male | 64 | |
| Age | ||
| ≤ 44 | 27 | |
| 45–59 | 50 | |
| > 60 | 0 | |
| Disease duration | ||
| ≤ 14 | 25 | |
| 15–27 | 5 | |
| ≥ 28 | 0 | |
| Education level | ||
| College and above | 0 | |
| High school and below | 56 | |
| Occupation | ||
| On duty of retired | 0 | |
| Unemployed | 43 | |
| Basic living allowances | ||
| No | 0 | |
| Yes | 44 | |
| Schizophrenia | ||
| No | 0 | |
| Yes | 24 | |
| No. of previous major symptoms | ||
| 0–1 | 0 | |
| > 1 | 100 | |
| No. of psychiatric visits/year | ||
| 0 | 0 | |
| ≥ 1 | 99 | |
| Agree to community management | ||
| Yes | 0 | |
| No | 76 | |
| Disability certificate | ||
| No | 0 | |
| Yes | 12 | |
| Delayed time (months) | ||
| < 2 | 0 | |
| 2–12 | 20 | |
| > 12 | 33 | |
| Participate in community rehabilitation activities | ||
| Yes | 0 | |
| No | 83 |
Table 5.
Correspondence between score and risk prediction probability.
| Point total | Estimate of risk |
|---|---|
| 72 | 0.01 |
| 287 | 0.05 |
| 385 | 0.10 |
| 491 | 0.20 |
| 562 | 0.30 |
| 620 | 0.40 |
| 673 | 0.50 |
Model validation
The results showed that the area under the ROC curve (AUC) was 0.708 (95% CI: 0.583–0.749), with an accuracy of 79.43%, sensitivity of 76.74%, and specificity of 83.57%. The constructed model demonstrated good reliability and effectiveness in predicting violence risk.
Discussion
Troublemaking behaviors of patients with severe mental disorders are often destructive and sudden39, seriously threatening public safety. However, neither psychiatry, mental hygiene, nor sociology can make accurate predictions and interventions alone. The prediction and intervention of troublemaking behaviors of patients with severe mental disorders is not a problem that can be solved by a single discipline, but requires the joint participation of multiple disciplines40,41. Therefore, it is urgent to construct a troublemaking risk prediction model suitable for patients with severe mental disorders in the community, so as to provide risk assessment tool for community workers to solve the difficulties in risk assessment.
Currently, structured assessment tools are commonly used for violence risk assessment in forensic and inpatient psychiatric patients42,43. Although these tools are widely utilized in clinical practice, their purposes, benefits, limitations, and abilities to predict future violence vary. Applying these scales to the routine follow-up management of community-dwelling patients with severe mental illnesses is less appropriate. Furthermore, these Western-developed scales yield different results across racial and ethnic groups. For example, certain items on the HCR-20 scale are interpreted differently by different populations, leading to significant variation in scores42. In some cultures, verbal conflicts may be seen as a normal form of emotional expression, while in others, they may be perceived as indicators of violent tendencies. Such cultural differences may not be adequately accounted for, resulting in biased assessment outcomes. Additionally, these single scales are relatively limited, as they fail to include biological indicators. Research using machine learning methods to predict violent behaviors in schizophrenia patients has incorporated factors such as neurobiology and genomics27,44,45, representing further exploration in violence risk prediction. However, the factors influencing violence risk in psychiatric patients are multifaceted, varying according to different societal models and economic influences. The expression of symptoms, including violent behaviors, differs across countries due to variations in mental health services, social assistance policies, and the level of community acceptance and understanding, which also influence policy changes46.
Domestic scholars are working to develop prediction models tailored to local conditions. In addition, the large number of community-dwelling patients with severe mental disorders in China, combined with relatively scarce community mental health resources47, highlights the need for practical tools that are simple and easy to use. Incorporating imaging and biological factors is not only financially prohibitive but also poses challenges in terms of time, labor, and patient cooperation. Currently, most risk prediction efforts focus on schizophrenia patients at high risk of violence, which does not apply to the six categories of mental illnesses covered under the National Basic Public Health Service Standards. The goal is to develop a predictive model for severe mental disorders suitable for community management and services. Clearly, existing domestic models are not fully applicable to community settings. Our research focuses on demographic and social environment factors, diagnostic and treatment information, social support, and symptom data48. These data are either pre-existing in patient records or can be obtained through simple surveys. Community mental health workers can access this information during their routine work for risk assessment, making the approach relatively feasible.
This study found that the average incidence of troublemaking among patients with severe mental disorders in Wuxi from 2017 to 2019 was 7.15%. In this study, males were more likely to troublemaking than women, which was consistent with the results of Wan et al.49 and Miao et al.50. The reason was that men tend to bear more financial burdens of the family, which lead to the relapse of mental illnesses. In terms of age, compared with the 45–60 age group, patients with severe mental disorders ≤ 45 years old were more likely to troublemaking, which was consistent with the results of Jiang et al.7. Young and middle-aged people are more energetic and energetic, and they bear greater pressure in society and family. However, young and middle-aged people are also an important age group for the first onset of severe mental disorders, such as schizophrenia, which easily to be ignored, leading to the delayed diagnosis and troublemaking.
Compared with non-schizophrenic patients, schizophrenic patients were more likely to troublemaking, which was proved by Song et al.51. Patients with schizophrenia often have aggressive behaviors due to symptoms such as delusions of persecution and command auditory hallucinations, which lead more prone to impulsive injury and destructive behavior. In terms of occupation, unemployed patients were more likely to troublemaking52, because the persistence of mental symptoms leads to loss of social function, unemployment and loss of economic resources. We also found that patients with more main symptoms in the past and more visits to psychiatrists each year were also risk factors for troublemaking. In terms of social support, patients who did not participate in community management and community rehabilitation activities were more likely to troublemaking. Patients who participate in community management and community rehabilitation activities could receive social attention, including regular follow-up visits by psychiatrists, care from neighborhood or neighborhood committees, and planned rehabilitation activities by mental rehabilitation therapists, which can promote the recovery of patients, improve the living ability53, reduce the stigma54, and reduce the burden on families. These patients receive free management services in the national basic public health service, which could effectively reduce the occurrence of troublemaking55. A meta-analysis of the effect of community comprehensive management interventions for patients with severe mental disorders also proved that community comprehensive management interventions can reduce the occurrence of troublemaking56.
Patients with mental disability certificates were more likely to be at risk of troublemaking, since these patients have more serious illnesses, cognitive dysfunction, lack self-awareness and unable to take medication regularly (which could reduce the risk of violence)57. Patients with subsistence allowances were also high-risk groups of troublemaking, since they have financial difficulties, un-guaranteed family life, and unregular treatment58. Compared with patients with higher education, patients with high school education and below were more likely to cause accidents, because of their early onset, decline in learning ability, impairment of social work and adaptability, and more severe disease severity. Studies59,60 also found that the rate of troublemaking decreased with the increase of education level. Shorter course of disease and delayed diagnosis were risk factors for troublemaking, which have been confirmed that patients with severe mental disorders who have just been discovered and treated for a short period of time are more likely to be involved in troublemaking because of the lack of awareness of mental illness61.
This study also has certain deficiencies. First, the incidence of troublemaking varies greatly in different regions. Additionally, due to factors such as stigmatization, the prevalence of severe mental disorders is significantly underestimated, which also affects the reported incidence of violent behavior. Therefore, the ability of our model to predict troublemaking risks requires more research in different regions to verify its authenticity and stability. Secondly, although more than 10 influencing factors were included in our study, the grouping of each factor is still not clear or detailed. Whether the risk of troublemaking caused by different diseases can be analyzed together requires further analysis. At the same time, more attention could be paid to other risk factors not included in this study, such as the content of clinical treatment, the type and amount of medication, drug side effects, family stress events, etc.
In conclusion, a large-sample Logistic regression analysis was applied to screen out influential factors with evaluation value against troublemaking to build a risk prediction model. The evaluation content was practical and the model was stable. The area under the ROC curve of the model was 0.688(95%CI:0.563 ~ 0.726). In order to facilitate the implementation of classified management services for the prevention and treatment of mental illness in the community and the implementation of risk assessment interventions for clinical medical workers, a nomogram model of the risk of troublemaking was established, and assigned the risk factors according to the regression coefficient β of each factor in the Logistic regression model, and a score and risk prediction probability correspondence table was provided to help community workers to carry out early risk assessment, so as to implement classified intervention measures and prevent troublemaking among patients with severe mental disorders in the community.
Acknowledgements
Not applicable.
Author contributions
Shiming Li and Qitao Yin conceived the study; Shiming Li, Queping Yang, Yingying Ji collected the data; Jieyun Yin and Shiming Li performed the data analysis; Shiming Li and Haohao Zhu wrote the manuscript and edited the manuscript. All authors reviewed the manuscript.
Funding
The work is supported by Wuxi Municipal Health Commission (No. M202211), Wuxi Taihu Talent Project (No. WXTTP2021), Wuxi Medical Development Discipline Project (No. FZXK2021012) and Wuxi City Soft Science Project (KX-21-C230).
Data availability
The dataset generated during and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Wuxi Mental Health Centre. The informed consent have been waived by the Ethics Committee of Wuxi Mental Health Center. All methods were performed in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shiming Li and Jieyun Yin contributed equally to this work.
Contributor Information
Haohao Zhu, Email: zhuhh@jiangnan.edu.cn.
Qitao Yin, Email: yqt1209@163.com.
References
- 1.Merchant, R. et al. Digital technology for management of severe mental disorders in low- and middle-income countries. Curr. Opin. Psychiatry. 33 (5), 501 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Montejo, A. L., Montejo, L. & Baldwin, D. S. The impact of severe mental disorders and psychotropic medications on sexual health and its implications for clinical management. World Psychiatry. 17 (1), 3–11 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang, Y. et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 6 (3), 211–224 (2019). [DOI] [PubMed] [Google Scholar]
- 4.Wang, X. et al. Analysis of the management and treatment status of patients with severe mental disorders in China in 2018. Chin. J. Psychiatry. 53 (05), 438–445 (2020). [Google Scholar]
- 5.Liu, C. F. et al. Analysis of factors influencing high-risk behaviors in patients with severe mental disorders. Prev. Med.31 (01), 51–54. 10.19485/j.cnki.issn2096-5087.2019.01.012 (2019). [Google Scholar]
- 6.Yu, T. et al. Analysis of factors influencing violent incidents among patients with severe mental disorders in Shaoxing. Prev. Med.30 (06), 621–623. 10.19485/j.cnki.issn2096-5087.2018.06.023 (2018). [Google Scholar]
- 7.Jiang, F. G. & Yan, G. J. Analysis of influencing factors of accidents and disasters among patients with severe mental disorders under management in Chengdu community. Mod. Prev. Med.46 (14), 2584–2587 (2019). [Google Scholar]
- 8.Go, D. S. et al. A comparison of disease burden and the government budget for mental health in Korea. J. Ment Health. 31 (4), 471–478. 10.1080/09638237.2020.1765999 (2022). [DOI] [PubMed] [Google Scholar]
- 9.Zhou, X. L. & Li, J. Meta-analysis of risk factors for high-risk behaviors among community patients with severe mental disorders in China. Chin. Prev. Chronic Dis.28 (07), 545–548. 10.16386/j.cjpccd.issn.1004-6194.2020.07.016 (2020). [Google Scholar]
- 10.Talevi, D. et al. Violence in severe mental disorders: the association with age at onset and gender. Riv Psichiatr. 58 (1), 27–29. 10.1708/3964.39428 (2023). [DOI] [PubMed] [Google Scholar]
- 11.Roaldset, J. O., Lockertsen, Ø., Gustavsen, C. C., Landheim, T. & Bjørkly, S. Comparison of V-RISK-Y and V-RISK-10 for risk of violence: A one-year study from a psychiatric emergency department for adolescents. Asian J Psychiatr. ;96:104044. (2024). 10.1016/j.ajp.2024.104044. Epub 024 Apr 4. PMID: 38598935. [DOI] [PubMed]
- 12.Anderson, K. K. & Jenson, C. E. Violence risk-assessment screening tools for acute care mental health settings: literature review. Arch. Psychiatr Nurs.33 (1), 112–119. 10.1016/j.apnu.2018.08.012 (2019). Epub 2018 Sep 6. PMID: 30663614. [DOI] [PubMed] [Google Scholar]
- 13.Jaber, F. S. & Mahmoud, K. F. Risk tools for the prediction of violence: ‘VRAG, HCR-20, PCL-R’. J Psychiatr Ment Health Nurs. ;22(2):133 – 41. (2015). 10.1111/jpm.12102. Epub 2013 Jul 3. PMID: 23834372. [DOI] [PubMed]
- 14.Lowder, E. M., Desmarais, S. L., Rade, C. B., Johnson, K. L. & Van Dorn, R. A. Reliability and validity of START and LSI-R assessments in Mental Health Jail Diversion clients. Assessment26 (7), 1347–1361 (2019). Epub 2017 Apr 15. PMID: 28412837. [DOI] [PubMed] [Google Scholar]
- 15.Parsaei, M. et al. Machine learning for prediction of violent behaviors in schizophrenia spectrum disorders: a systematic review. Front. Psychiatry. 15, 1384828. 10.3389/fpsyt.2024.1384828 (2024). PMID: 38577400; PMCID: PMC10991827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang, K. Z. et al. Prediction of physical violence in schizophrenia with machine learning algorithms. Psychiatry Res.289, 112960. 10.1016/j.psychres.2020.112960 (2020). Epub 2020 Apr 13. PMID: 32361562. [DOI] [PubMed] [Google Scholar]
- 17.Sonnweber, M., Lau, S. & Kirchebner, J. Exploring characteristics of Homicide offenders with Schizophrenia Spectrum disorders Via Machine Learning. Int. J. Offender Ther. Comp. Criminol.68 (6–7), 713–732. 10.1177/0306624X221102799 (2024). Epub 2022 Jun 22. PMID: 35730542; PMCID: PMC11041084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheng, N. et al. Application of machine learning in predicting aggressive behaviors from hospitalized patients with schizophrenia. Front. Psychiatry. 14, 1016586. 10.3389/fpsyt.2023.1016586 (2023). PMID: 37020730; PMCID: PMC10067917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gou, N. et al. Identification of violent patients with schizophrenia using a hybrid machine learning approach at the individual level. Psychiatry Res.306, 114294 (2021). Epub 2021 Nov 17. PMID: 34823086. [DOI] [PubMed] [Google Scholar]
- 20.Yu, T., Zhang, X., Liu, X., Xu, C. & Deng, C. The prediction and influential factors of violence in male Schizophrenia patients with machine learning algorithms. Front. Psychiatry. 13, 799899. 10.3389/fpsyt.2022.799899 (2022). PMID: 35360130; PMCID: PMC8962616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yu, T., Pei, W., Xu, C., Zhang, X. & Deng, C. Prediction of violence in male schizophrenia using sMRI, based on machine learning algorithms. BMC Psychiatry. 22 (1), 676. 10.1186/s12888-022-04331-1 (2022). PMID: 36320010; PMCID: PMC9628088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sun, L. et al. Candidate symptomatic markers for predicting violence in schizophrenia: a cross-sectional study of 7711 patients in a Chinese population. Asian J. Psychiatr. 59, 102645. 10.1016/j.ajp.2021.102645 (2021). [DOI] [PubMed] [Google Scholar]
- 23.Machetanz, L., Günther, M. P., Lau, S. & Kirchebner, J. High risk, high dose?-Pharmacotherapeutic prescription patterns of offender and Non-offender patients with Schizophrenia Spectrum Disorder. Biomedicines10 (12), 3243. 10.3390/biomedicines10123243 (2022). PMID: 36551999; PMCID: PMC9775158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Machetanz, L., Hofmann, A. B., Möhrke, J. & Kirchebner, J. Offenders and non-offenders with schizophrenia spectrum disorders: the crime-preventive potential of sufficient embedment in the mental healthcare and support system. Front. Psychiatry. 14, 1231851. 10.3389/fpsyt.2023.1231851 (2023). PMID: 37711423; PMCID: PMC10498463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen, S. C., Chu, N. H., Hwu, H. G. & Chen, W. J. Trajectory classes of violent behavior and their relationship to lipid levels in schizophrenia inpatients. J Psychiatr Res. (2015). Jul-Aug;66–67:105 – 11 10.1016/j.jpsychires.2015.04.022. Epub 2015 May 9. PMID: 26004299. [DOI] [PubMed]
- 26.Chen, X. et al. Dysregulation of amino acids and lipids metabolism in schizophrenia with violence. BMC Psychiatry. 20 (1), 97. 10.1186/s12888-020-02499-y (2020). PMID: 32131778; PMCID: PMC7055102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tang, X., Jin, J., Tang, Y., Cao, J. & Huang, J. Risk assessment of aggressive behavior in Chinese patients with schizophrenia by fMRI and COMT gene. Neuropsychiatr Dis. Treat.13, 387–395 (2017). PMID: 28223811; PMCID: PMC5308585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kirchebner, J., Lau, S. & Machetanz, L. Offenders and non-offenders with schizophrenia spectrum disorders: do they really differ in known risk factors for aggression? Front. Psychiatry. 14, 1145644. 10.3389/fpsyt.2023.1145644 (2023). PMID: 37139319; PMCID: PMC10150953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kirchebner, J., Sonnweber, M., Nater, U. M., Günther, M. & Lau, S. Stress, Schizophrenia, and violence: a Machine Learning Approach. J. Interpers. Violence. 37 (1–2), 602–622 (2022). Epub 2020 Apr 20. PMID: 32306866. [DOI] [PubMed] [Google Scholar]
- 30.江弋舟, 陈春梅,朱有为,等.社区不同性别精神分裂症患者危险行为发生风险预测模型的建立与验证[J].上海预防医学,2022,34(10):948–954 .10.19428/j.cnki.sjpm.2022.21677
- 31.Jiang, Y. Z. et al. Development and validation of a risk prediction model for dangerous behaviors among schizophrenia patients of different genders in the community. Shanghai J. Prev. Med.34 (10), 948–954. 10.19428/j.cnki.sjpm.2022.21677 (2022). [Google Scholar]
- 32.Zhang, W. B. et al. Development of a comprehensive risk prediction model for violent behavior in community schizophrenia patients. Chin. Mental Health J.36 (10), 844–850 (2022). [Google Scholar]
- 33.Zhou, J. et al. Violence risk assessment in psychiatric patients in China: a systematic review. Aust N Z. J. Psychiatry. 50 (1), 33–45 (2016). doi: 10.1177/0004867415585580. Epub 2015 May 19. PMID: 25991764; PMCID: PMC4702215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wan, L. et al. Preliminary development of a risk assessment scale for violent behavior among patients with severe mental disorders in Changzhou. Occup. Health. 35 (21), 2966–2970. 10.13329/j.cnki.zyyjk.2019.0754 (2019). [Google Scholar]
- 35.Mills, J. F. Violence risk assessment: a brief review, current issues, and future directions. Can. Psychol.58 (1), 40–49 (2017). [Google Scholar]
- 36.Rund, B. R. The association between schizophrenia and violence. Schizophr Res.199, 39–40 (2018). [DOI] [PubMed] [Google Scholar]
- 37.Bulgari, V. et al. Clinical and neuropsychological features of violence in schizophrenia: a prospective cohort study. Schizophr Res.181, 124–130 (2017). [DOI] [PubMed] [Google Scholar]
- 38.National Health Commission of the People’s Republic of China. Standards for the management and treatment of severe mental disorders (2018 edition). Chin. J. Pract. Rural Doctors. 25 (7), 11–22 (2018). [Google Scholar]
- 39.Li, S. M. et al. Analysis of troublemaking behaviors of patients with severe mental disorders in the community and their influencing factors. Chin. Prev. Chronic Dis.28 (11), 811–815 (2020). [Google Scholar]
- 40.Li, Z. et al. Effect of community-based standardized mental disorders management on patients with severe mental disorders. Chin. Gen. Pract.21 (35), 4322 (2018). [Google Scholar]
- 41.Fusar-Poli, P. Integrated mental health services for the developmental period (0 to 25 years): a critical review of the evidence. Front. Psychiatry. 10, 355 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dudeck, M. et al. Evaluation of whether commonly used risk assessment tools are applicable to women in forensic psychiatric institutions. Compr. Psychiatry. 135, 152528. 10.1016/j.comppsych.2024.152528 (2024). Epub 2024 Sep 2. PMID: 39241375. [DOI] [PubMed] [Google Scholar]
- 43.Ramesh, T., Igoumenou, A., Vazquez Montes, M. & Fazel, S. Use of risk assessment instruments to predict violence in forensic psychiatric hospitals: a systematic review and meta-analysis. Eur. Psychiatry. 52, 47–53. 10.1016/j.eurpsy.2018.02.007 (2018). Epub 2018 Apr 4. PMID: 29626758; PMCID: PMC6020743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yu, T., Pei, W., Xu, C., Zhang, X. & Deng, C. Investigation of peripheral inflammatory biomarkers in association with violence in schizophrenia. BMC Psychiatry. 24 (1), 542. 10.1186/s12888-024-05966-y (2024). PMID: 39085826; PMCID: PMC11293062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lu, J. et al. Brain structural alterations associated with impulsiveness in male violent patients with schizophrenia. BMC Psychiatry. 24 (1), 281. 10.1186/s12888-024-05721-3 (2024). PMID: 38622613; PMCID: PMC11017613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mezey, G. et al. Modelling social exclusion in a diagnostically-mixed sample of people with severe mental illness. Int. J. Soc. Psychiatry. 68 (2), 420–428 (2022). Epub 2021 Mar 17. PMID: 33730906; PMCID: PMC8841629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liang, D., Mays, V. M. & Hwang, W. C. Integrated mental health services in China: challenges and planning for the future. Health Policy Plan.33 (1), 107–122. 10.1093/heapol/czx137 (2018). PMID: 29040516; PMCID: PMC5886187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhang, L. et al. Identifying risk factors to predict violent behaviour in community patients with severe mental disorders: a retrospective study of 5277 patients in China. Asian J. Psychiatr. 83, 103507 (2023). Epub 2023 Feb 9. PMID: 36796125. [DOI] [PubMed] [Google Scholar]
- 49.Wan, L. et al. Analysis of demographic and clinical characteristics of patients with severe mental disorders who are prone to accidents in Changzhou. China Med. Herald. 15 (23), 47–50 (2018). [Google Scholar]
- 50.Miao, H. Y., Xu, J. & Huang, J. P. Comparison of accident risk between urban and suburban patients with severe mental illness in Nantong. J. Clin. Psychiatry. 24 (6), 42–43 (2014). [Google Scholar]
- 51.Song, Z. W. et al. Investigation on accidents and disasters among patients with severe mental illness in Shunde District, Foshan City. Nerv. Dis. Ment Health. 13 (1), 30–32 (2013). [Google Scholar]
- 52.Li, Y. et al. The association between medication adherence and disease stability in patients with severe mental disorders and area variation: community-based prospective study in Southwest China. Community Ment Health J.56 (2), 322–327 (2020). [DOI] [PubMed] [Google Scholar]
- 53.Fan, Y. et al. A community-based peer support service for persons with severe mental illness in China. BMC Psychiatry. 18 (1), 1–10 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cruwys, T. et al. The recovery model in chronic mental health: a community-based investigation of social identity processes. Psychiatry Res.291, 113241 (2020). [DOI] [PubMed] [Google Scholar]
- 55.Liu, Y. et al. Characterizing racial differences of mental health burdens, psychosocial determinants, and impacts on HIV prevention outcomes among young men who have sex with men: a community-based study in two US cities. J. Racial Ethn. Health Disparities. 9 (4), 1114–1124 (2022). [DOI] [PubMed] [Google Scholar]
- 56.Xu, Y. Q., Li, Y. & Jiang, B. F. Meta-analysis of the community comprehensive management intervention effect on patients with severe mental illness causing accidents. Chin. Public. Health. 31 (8), 1091–1094 (2015). [Google Scholar]
- 57.Sariaslan, A. et al. Associations between individual antipsychotics and the risk of arrests and convictions of violent and other crime: a nationwide within-individual study of 74,925 persons. Psychol. Med.52(16), 1–9 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Whiting, D., Lichtenstein, P. & Fazel, S. Violence and mental disorders: a structured review of associations by individual diagnoses, risk factors, and risk assessment. Lancet Psychiatry. 8 (2), 150–161 (2021). [DOI] [PubMed] [Google Scholar]
- 59.Yu, R. et al. Mental disorders and intimate partner violence perpetrated by men towards women: a Swedish population-based longitudinal study. PLoS Med.16(12), e1002995 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Halim, N. et al. Intimate partner violence during pregnancy and perinatal mental disorders in low and lower-middle income countries: a systematic review of literature, 1990–2017. Clin. Psychol. Rev.66, 117–135 (2018). [DOI] [PubMed] [Google Scholar]
- 61.Ying, Y. et al. Electroconvulsive therapy is associated with lower readmission rates in patients with schizophrenia. Brain Stimul. 14 (4), 913–921 (2021). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset generated during and analyzed during the current study are available from the corresponding author on reasonable request.