Abstract
Statement of the problem
Previous longitudinal studies have found that patients with shortened dental arches (SDA) have a higher risk of long-term tooth loss than complete dental arch (CDA). However, the difference between SDA and CDA concerning oral function has yet to be demonstrated.
Purpose
We aimed to clarify the influence of molar occlusal support on oral function in SDA and CDA participants cross-sectionally and longitudinally.
Materials and methods
We enrolled independent older adults (≥65 years) living in rural areas of Japan. Of these, 257 had CDA, and 21 had SDA without removable prostheses. We assessed the oral function (number of functional teeth, masticatory performance using gummy jelly, occlusal force, oral cleanliness, oral dryness, and maximum tongue pressure) during baseline and two years after baseline (follow-up). Comparison of oral function between SDA and CDA and changes over time were examined using repeated measures analysis of variance and post-hoc test.
Results
Cross-sectional analysis showed that both masticatory performance and occlusal force were significantly lower in SDA than in CDA. The functional teeth tended to decrease over time more in SDA than in CDA (p < 0.001). No longitudinal differences were found between SDA and CDA regarding other factors.
Conclusions
Participants with SDA had fewer teeth over time than CDAs, but no apparent difference was found in the decline of oral function.
Clinical implications
It is notable that prosthetic treatment for patients with SDA, whose main options are either implant or crown prosthesis, removable partial dentures, or no treatment, does not result in a loss of function over time. Prosthetic treatment should be conducted after careful consultation with the SDA patients to determine specific goals for each.
Keywords: Prosthetic restoration, Shortened dental arch, Occlusion, Tooth loss, Oral function
1. Introduction
Human teeth, in general, tend be lost beginning with the posterior molars due to poor cleanability, treatment difficulty, and high occlusal force loading [1]. To prevent increased overloading on the remaining teeth and the loss of masticatory function, dentists restore the patients’ occlusion by replacing the missing using prosthetic treatments such as implants, fixed and/or removable dental prostheses [2,3].
While removable dental prostheses can restore function and aesthetics, it can also progressively damage the remaining teeth and surrounding oral tissues (ex. dental caries, periodontal disease, and resorption of the residual ridge [4,5]) if careful consideration of the treatment plan was not done. To avoid excessive dental treatment, the concept of Shortened Dental Arch (SDA) was introduced. Arnd Käyser defined SDA as a condition when partial edentulism of distal extension edentulous space in the posterior area exists [6].
Previous cross-sectional studies have reported no significant differences between SDA and Complete Dental Arch (CDA) in masticatory ability, symptoms of temporomandibular disorders, remaining teeth migration, and oral comfort [[7], [8], [9], [10]]. On the other hand, SDA patients were found to have a higher risk of tooth loss in the long term, according to a longitudinal study [11,12]. However the difference between SDA and CDA concerning oral function has yet to be demonstrated.
Therefore, this prospective cohort study was conducted to clarify the influence of molar teeth occlusion on oral function and its change over time in older adults with CDA and SDA who had never worn removable dentures.
2. Materials and methods
2.1. Study design and participants
The study protocol received approval from the Ethics Review Committees at Hyogo Medical University (Rinhi 0342) and Niigata University (Approval No.G2021-0027) for research involving human subjects. The investigation adhered to STROBE guidelines, and participants provided written informed consent prior to the survey.
The study population consisted of independent older adults, aged 65 and above, residing in the Tamba-Sasayama region. These individuals took part in the Joint Medical-Dental Health Study (Frail Elderly in Sasayama-Tamba Area; FESTA study) from June 2016 to July 2020. Participants completed surveys at two time points: an initial assessment and a follow-up evaluation conducted two years later.
Table 1 shows inclusion and exclusion criteria for SDA and CDA. The definition of an occlusal unit (OU) followed Kayser's [6].
Table 1.
Inclusion criteria and exclusion criteria for SDA and CDA.
| Inclusion criteria | SDA | Kennedy I or Kennedy II maxilla or mandible with full occlusal support of anterior teeth with Occlusal units (OU) of 0–6. (In this model 1 M occlusal unit was defined as 1 OU for a pair of occlusal supports in the upper and lower premolars and 2 OU for a pair of occlusal support in the maxillary and mandibular molars as proposed by Kayser [6]) |
| Partially edentulous areas untreated for at least one month and no dental procedures done such as tooth extraction, new dentures, or crown restorations during the study period. | ||
| Intact anterior dental arch restorable with fixed partial dentures or implant-supported fixed partial dentures. | ||
| CDA | Participants who had full occlusal support from all teeth except third molars. The occlusal support was defined as functional teeth (excluding fixed bridges pontics, implants and residual roots) [12,13]. | |
| Exclusion criteria | for both groups | Current use of removable partial dentures, |
| Persons with dental caries, periodontal disease, or temporomandibular joint disorder [12]. |
SDA: shortened dental arch.
CDA: Complete dental arch.
2.2. Assessment of oral function and oral health status
The oral examination was performed by dentists affiliated to the university who participated in the pre-calibration process. All dentists were calibrated twice (2 h/day, 4 h in total) before the evaluation, and the evaluations were reconciled. To eliminate potential measurement bias, the dentists who performed the evaluations were blinded to the purpose of the study. The assessments were conducted before meals and at least 1 h after oral cleaning.
The assessment components encompassed the number of functional teeth, masticatory performance, occlusal force, tongue pressure, oral cleanliness, and oral dryness. The total number of functional teeth (NFT) included the natural teeth, treated teeth with crowns [13]. We evaluated the masticatory performance (MP) score using a test gummy jelly (UHA Mikakuto, Co., Ltd., Osaka, Japan) [14]. We measured the maximum occlusal force (OF) of the left and right first molars using an occlusal force meter (GM10, Nagano Keiki Co., Ltd., Tokyo, Japan), but when the first molar was missing, the adjacent tooth was measured. Then the sum of both measurements was used for the analysis [15]. We evaluated the tongue pressure using the JMS Tongue Pressure Monitor (TPM-02E: JMS, Hiroshima, Japan). We instructed the participants to press the balloon continuously against the palate for approximately 5–7 s using their tongue twice, and the higher value was taken as the participant's maximum tongue pressure value [16]. The bacterial count was measured with a rapid oral bacteria quantification system (Panasonic Healthcare Co. Ltd., Osaka, Japan) using the dielectrophoresis impedance measurement method (level 1–7: few-numerous) [17]. Oral dryness was the maximum of two measurements taken on the tongue using an oral moisture meter (Mucus, LIFE Co., Ltd., Saitama, Japan) [18].
2.3. Sample Size Calculation and statistical analysis
The Shapiro-Wilk test was employed to assess the normality of data distribution. In cases where the data did not follow a normal distribution, transformations using square root or logarithmic methods were applied.
For baseline comparison of the SDA and CDA groups, we employed either the Mann-Whitney U test or the χ2 test. To evaluate differences between SDA and CDA, as well as temporal changes, we utilized repeated measures ANOVA. When statistical significance was observed, post-hoc tests (Bonferroni method) were conducted for the main effect terms (tooth condition (CDA/SDA) and time) and the interaction term. Statistical analyses were performed using SPSS (IBM SPSS Statistics 23, Armonk, NY, USA), with the significance level set at 5 % for all tests.
3. Results
3.1. Characteristics of participants
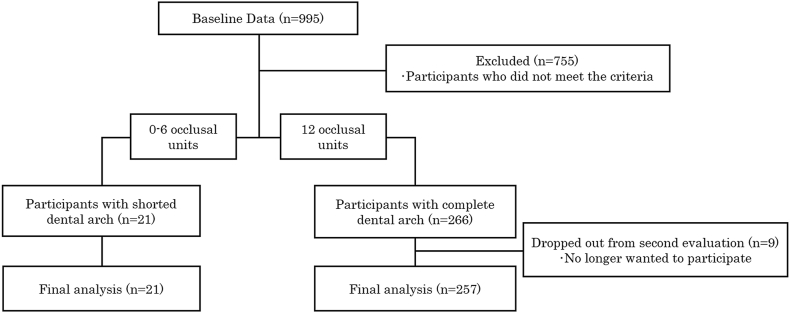
Fig. 1 shows the process of participant selection in both groups. The baseline data consisted of 995 participants, then we excluded those who did not meet the criteria. (n = 755, 75.9 %). Participants were enrolled in two groups according to OU: the SDA group with Kennedy I or Kennedy II maxilla or mandible with full occlusal support of anterior teeth with 1–6 OU and the CDA group with 12 OU. The SDA group (n = 21) represented 3.9 % of the total number of participants (8 males and 13 females with a mean age of 71.3 ± 4.0 years, mean ± S.D.), and no participants dropped out. In the CDA group, nine of the 266 participants (94 males, 172 females) who participated in the baseline did not take part in the re-assessment. Finally, the CDA group included 257 participants (88 males and 169 females, mean age: 71.6 ± 5.4 years, mean ± S.D.).
Fig. 1.
Flowchart showing the process of determining the final analysis participants.
The baseline data consisted of 995 participants, then we excluded those who did not meet the criteria. (n=755, 75.9%). Participants were enrolled in two groups according to OU: the SDA group with 0-6 OU and the CDA group with 12 OU. The SDA group (n=21) represented 3.9% of the total number of participants (8 males and 13 females with a mean age of 71.3 ± 4.0 years, mean ± S.D.), and no participants dropped out. In the CDA group, nine of the 266 participants (94 males, 172 females) who participated in the baseline did not take part in the re-assessment. Finally, the CDA group included 257 participants (88 males and 169 females, mean age: 71.6 ± 5.4 years, mean ± S.D.).
Table 2 shows the participant characteristics. The mean NFT in the SDA group was 23.5 ± 0.7. The mean MP was 3.8 ± 0.4 in the SDA group and 5.4 ± 0.1 in the CDA group. There were significant differences in the NFT (p < 0.001) and MP (p < 0.001) between the groups. On the other hand, there were no significant differences between groups in other oral functions as well as demographic data.
Table 2.
Baseline characteristics of participants.
| Evaluated items |
CDA (n = 257) |
SDA (n = 21) |
p |
|---|---|---|---|
| Age (years) | 71.6 ± 5.4 | 71.3 ± 4.0 | 0.21 |
| Gender (Male) | 81 (31.5%) | 8 (38.1%) | 0.79 |
| Num. of Functional teetha | 28.0 ± 0.0 | 23.5 ± 0.7 | <0.001 |
| Masticatory performance (score) | 5.4 ± 0.1 | 3.8 ± 0.4 | <0.001 |
| Occlusal force (kgf)a | 83.5 ± 2.2 | 60.1 ± 5.1 | 0.003 |
| Oral cleanliness (Lv) | 4.9 ± 0.1 | 4.5 ± 0.3 | 0.07 |
| Oral dryness | 26.7 ± 0.3 | 26.3 ± 1.1 | 0.71 |
| Tongue pressure (kPa) | 32.4 ± 0.5 | 30.5 ± 1.3 | 0.28 |
Data are presented as the mean ± standard deviation, or number of participants (%).
CDA: Complete dental arch.
SDA: shortened dental arch.
Number of functional teeth: Natural teeth and treated teeth that have a crown, excluding bridge pontics and implants.
Masticatory performance (Score): Gummy jelly score evaluation by visual inspection.
Occlusal force (kgf): Measured by the occlusal force meter.
Oral cleanliness (Lv): Bacterial count (Level 1–7) on the tongue surface using a dielectrophoretic impedance measurement method.
Oral dryness: Maximum value of two measurements on the tongue using an oral moisture meter.
Tongue pressure (kPa): Maximum value obtained from two measurements using the JMS tongue pressure meter.
p: Comparison of CDA and SDA by Mann-Whitney U test.
Significant difference between CDA and SDA, by the Mann-Whitney U test or χ-square test.
3.2. Changes in oral functions over time
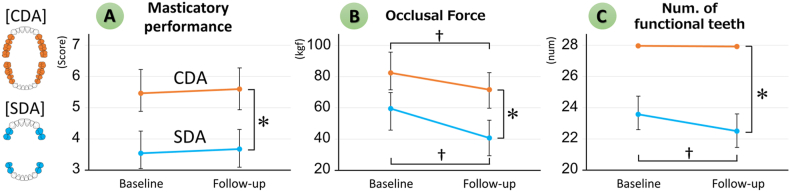
The MP and OF were significantly lower in SDA than in CDA at both baseline and follow-up, but there were no significant differences between SDA and CDA in other oral functions (Fig. 2A, B and Table 3).
Fig. 2.
Changes in oral functions over time
Comparisons between SDA and CDA and changes over time were examined using repeated measures ANOVA.
Values are presented as the mean ± standard deviation.
∗: Significant difference in Dentition status by repeated measures ANOVA.
†: Significant difference between Pre and Post for each dentition by repeated measures ANOVA. Variables are the same as in Table 2
Table 3.
Results of the repeated measures ANOVA of oral function factors.
| Evaluated items | Dentition status(SDA/CDA) |
Time(pre/post) |
Interaction(Dentition status×Time) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| F | p | η2 | F | p | η2 | F | p | η2 | |
| Num. of functional teeth | 276.4a | <0.001 | 0.51 | 46.0a | <0.001 | 0.15 | 18.4a | <0.001 | 0.07 |
| Masticatory performance (score) | 26.5a | <0.001 | 0.10 | 0.14 | 0.71 | 0.001 | 0.003 | 0.95 | <0.001 |
| Occlusal force (kgf) | 15.4a | <0.001 | 0.06 | 20.6a | <0.001 | 0.07 | 2.16 | 0.14 | 0.008 |
| Oral cleanliness (Lv) | 7.3 | 0.14 | 0.03 | 1.8 | 0.18 | 0.007 | 0.34 | 0.56 | 0.001 |
| Oral dryness | 0.01 | 0.92 | <0.001 | 2.6 | 0.11 | 0.01 | 0.22 | 0.64 | 0.001 |
| Tongue pressure (kPa) | 0.92 | 0.34 | 0.004 | 0.25 | 0.62 | 0.001 | 0.26 | 0.61 | 0.001 |
Comparisons between SDA and CDA and changes over time were examined using repeated measures ANOVA.
Main effect: Dentition status (CDA/SDA), Time(pre/post), Interaction: Condition × Time.
F is significant at the 0.05 level, and p value is the significance probability of each main effect and interaction. Variables are the same as in Table 2.
Both SDA and CDA showed no significant difference in MP but showed a significant decrease in OF over time (Fig. 2B). On the other hand, SDA with less occlusal support showed a decrease in NFT faster than CDA, indicating an interaction between time and SDA/CDA (Fig. 2C).
4. Discussion
In this study, the SDA group had significantly lower occlusal force than the CDA group. The difference between the occlusal force of the SDA and CDA groups was probably due to the decrease in occlusal support resulting from the decrease in the number of teeth in the SDA group [19]. In addition, a decrease in occlusal force over time was observed in both the SDA and CDA groups. This result agreed with the report of Shiga et al., which mentioned that although the occlusal force of adults with natural dentition does not differ from 20 to 60 years of age, it was found to decrease significantly after 60 years of age [20]. Furthermore, it has been reported that the occlusal force is less affected by aging when many teeth are present [21]. Since the occlusal force of the CDA group was thought to be less affected by aging in our present study, it resulted in a relatively greater decrease in the occlusal force of the SDA group than the CDA group.
The masticatory performance, on the other hand, did not significantly change over time in both groups. Because masticatory performance is influenced by the occlusal force, which is also dependent on the presence or absence of occlusal support of the molars [22], it was likely that in the SDA group with remaining occlusal support, the decrease in occlusal force had less influence on the masticatory performance over time.
There were no significant differences between the SDA and CDA groups in oral environmental factors such as oral cleanliness and oral dryness. This suggests that regardless of oral environmental status, being an SDA is likely to be a factor in long-term tooth loss by itself.
5. Conclusions
We conclude from our study findings that participants with SDA had fewer teeth over time than those with CDA, but no apparent difference was found in the decline of oral function. Prosthetic treatment for patients with SDA, whose main options are either implant crown prosthesis, removable partial dentures, or no treatment at all, should be performed with careful consideration for each SDA patient because each has different priorities in terms of outcomes from prosthetic treatment.
CRediT authorship contribution statement
Tasuku Yoshimoto: Writing – review & editing, Writing – original draft, Visualization, Methodology, Formal analysis, Data curation, Conceptualization. Yoko Hasegawa: Writing – review & editing, Visualization, Methodology, Formal analysis, Conceptualization. Aye Mya Mya Khaing: Visualization, Data curation. Ma Therese Sta Maria: Writing – review & editing, Visualization. Hirokazu Hattori: Resources, Investigation, Data curation. Hiromitsu Kishimoto: Resources, Methodology, Investigation, Data curation. Ken Shinmura: Resources, Methodology, Investigation, Data curation. Takahiro Ono: Writing – review & editing, Supervision, Resources, Project administration, Methodology, Funding acquisition, Conceptualization.
Ethics statement
This study was conducted with the approval of the Hyogo Medical University Ethics Review Committee (Rinhi 0342) and the Niigata University Ethics Review Committee for Research Involving Human Subjects (Approval No.G2021-0027)
Data availability statement
Data will be made available on request.
Role of funding source
This study was supported by Osaka Gas Group Welfare Foundation, the Hyogo Dental Association, 8020 Foundation, Mitsui Sumitomo Insurance Welfare Foundation (to Hasegawa Y) and and by the Japan Society for the Promotion of Science (JSPS) Grant-in-Aid for Scientific Research (KAKENHI) (grant no. 16KT0012) (to Shinmura K). The funders had no role in the study design, data collection and analysis, preparation of the manuscript, or decision about its publication.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Shinmura K reports financial support was provided by Osaka Gas Group Welfare Foundation. Shinmura K reports financial support was provided by the Hyogo Dental Association. Shinmura K reports financial support was provided by 8020 Promotion Foundation. Shinmura K and Hasegawa Y reports financial support was provided by Mitsui Sumitomo Insurance Welfare Foundation. Shinmura K reports financial support was provided by Japan Society for the Promotion of Science. If there are other authors, they declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We would like to express our sincere appreciation to our colleagues at the Hyogo Medical University Department of Dental and Oral Surgery, and all members of the FESTA (Frail Elderly in Sasayama-Tamba Area) research team (titles omitted) for their assistance in the implementation of this study (Hiroshi Kusunoki, Yosuke Wada, Takara Mori, Shotaro Tsuji, Kayoko Tamaki, Ryota Matsuzawa, and Koutatsu Nagai; and to everyone at the Hyogo Medical University Sasayama Medical Center).
Contributor Information
Yoko Hasegawa, Email: cem17150@dent.niigata-u.ac.jp.
Takahiro Ono, Email: ono-t@cc.osaka-dent.ac.jp.
References
- 1.Ministry of Health L.a.W. Survey of dental diseases (2016): summary of results. https://www.mhlw.go.jp/toukei/list/62-17b.html
- 2.Gilbert G.H., Miller M.K., Duncan R.P., Ringelberg M.L., Dolan T.A., Foerster U. Tooth-specific and person-level predictors of 24-month tooth loss among older adults. Community Dent. Oral Epidemiol. 1999;27:372–385. doi: 10.1111/j.1600-0528.1999.tb02034.x. [DOI] [PubMed] [Google Scholar]
- 3.Ikebe K., Matsuda K., Kagawa R. Association of masticatory performance with age, gender, number of teeth, occlusal force and salivary flow in Japanese older adults: is ageing a risk factor for masticatory dysfunction? Arch. Oral Biol. 2011;56:991–996. doi: 10.1016/j.archoralbio.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 4.Wilding R.J., Reddy J. Periodontal disease in partial denture wearers–a biological index. J. Oral Rehabil. 1987;14:111–124. doi: 10.1111/j.1365-2842.1987.tb00700.x. [DOI] [PubMed] [Google Scholar]
- 5.MacEntee M.I. Biologic sequelae of tooth replacement with removable partial dentures: a case for caution. J. Prosthet. Dent. 1993;70:132–134. doi: 10.1016/0022-3913(93)90007-b. [DOI] [PubMed] [Google Scholar]
- 6.Käyser A.F. Shortened dental arches and oral function. J. Oral Rehabil. 1981;8:457–462. doi: 10.1111/j.1365-2842.1981.tb00519.x. [DOI] [PubMed] [Google Scholar]
- 7.Käyser A.F. Shortened dental arch: a therapeutic concept in reduced dentitions and certain high-risk groups. Int. J. Periodontics Restor. Dent. 1989;9:426–449. [PubMed] [Google Scholar]
- 8.Käyser A.F., Witter D.J., Spanauf A.J. vol. 32. 1987. pp. 178–182. (Overtreatment with Removable Partial Dentures in Shortened Dental Arches, Australian Dental Journal). [DOI] [PubMed] [Google Scholar]
- 9.Kanno T., Carlsson G.E. A review of the shortened dental arch concept focusing on the work by the Käyser/Nijmegen group. J. Oral Rehabil. 2006;33:850–862. doi: 10.1111/j.1365-2842.2006.01625.x. [DOI] [PubMed] [Google Scholar]
- 10.Witter D.J., Elteren P., Käyser A.F., Rossum M.J. The effect of removable partial dentures on the oral function in shortened dental arches. J. Oral Rehabil. 1989;16:27–33. doi: 10.1111/j.1365-2842.1989.tb01314.x. [DOI] [PubMed] [Google Scholar]
- 11.Gerritsen A.E., Witter D.J., Bronkhorst E.M., Creugers N.H. Increased risk for premolar tooth loss in shortened dental arches. J. Dent. 2013;41:726–731. doi: 10.1016/j.jdent.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 12.Fueki K., Igarashi Y., Maeda Y., Baba K., Koyano K., Sasaki K., Akagawa Y., Kuboki T., Kasugai S., Garrett N.R. Effect of prosthetic restoration on oral health-related quality of life in participants with shortened dental arches: a multicentre study. J. Oral Rehabil. 2015;42:701–708. doi: 10.1111/joor.12297. [DOI] [PubMed] [Google Scholar]
- 13.Yoshimoto T., Hasegawa Y., Salazar S., Kikuchi S., Hori K., Ono T. Factors affecting masticatory satisfaction in participants with removable partial dentures. IJERPH. 2021;18:6620. doi: 10.3390/ijerph18126620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nokubi T., Yoshimuta Y., Nokubi F., Yasui S., Kusunoki C., Ono T., Maeda Y., Yokota K. Validity and reliability of a visual scoring method for masticatory ability using test gummy jelly. Gerodontology. 2013;30:76–82. doi: 10.1111/j.1741-2358.2012.00647.x. [DOI] [PubMed] [Google Scholar]
- 15.Varga S., Spalj S. Maximum voluntary molar bite force in subjects with normal occlusion. Eur J Orthodont. 2011;33:427–433. doi: 10.1093/ejo/cjq097. [DOI] [PubMed] [Google Scholar]
- 16.Hayashi R., Tsuga K., Hosokawa R. A novel handy probe for tongue pressure measurement. Int. J. Prosthodont. (IJP) 2002;15:385–388. [PubMed] [Google Scholar]
- 17.Hamada R., Suehiro J., Nakano M. Development of rapid oral bacteria detection apparatus based on dielectrophoretic impedance measurement method. IET Nanobiotechnol. 2011;5:25–31. doi: 10.1049/iet-nbt.2010.0011. [DOI] [PubMed] [Google Scholar]
- 18.Takahashi F., Koji T., Morita O. The usefulness of an oral moisture checking device (Moisture Checker for Mucus) Nihon Hotetsu Shika Gakkai zasshi. 2005;49:283–289. doi: 10.2186/jjps.49.283. [DOI] [PubMed] [Google Scholar]
- 19.Iwasaki M., Hirano H., Motokawa K. Interrelationships among whole-body skeletal muscle mass, masseter muscle mass, oral function, and dentition status in older Japanese adults. BMC Geriatr. 2021;21:582. doi: 10.1186/s12877-021-02552-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shiga H., Komino M., Yokoyama M. Relationship between age and occlusal force in adults with natural dentition. Odontology. 2023;111:487–492. doi: 10.1007/s10266-022-00750-4. [DOI] [PubMed] [Google Scholar]
- 21.Motegi E., Nomura M., Tachiki C. Occlusal force in people in their sixties attending college for elderly. Bull. Tokyo Dent. Coll. 2009;50:135–140. doi: 10.2209/tdcpublication.50.135. [DOI] [PubMed] [Google Scholar]
- 22.Kosaka T., Ono T., Kida M., Kikui M., Yamamoto M., Yasui S., Nokubi T., Maeda Y., Kokubo Y., Watanabe M., Miyamoto Y. A multi-factorial model of masticatory performance: the Suita study. J. Oral Rehabil. 2016;43:340–347. doi: 10.1111/joor.12371. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.