Abstract
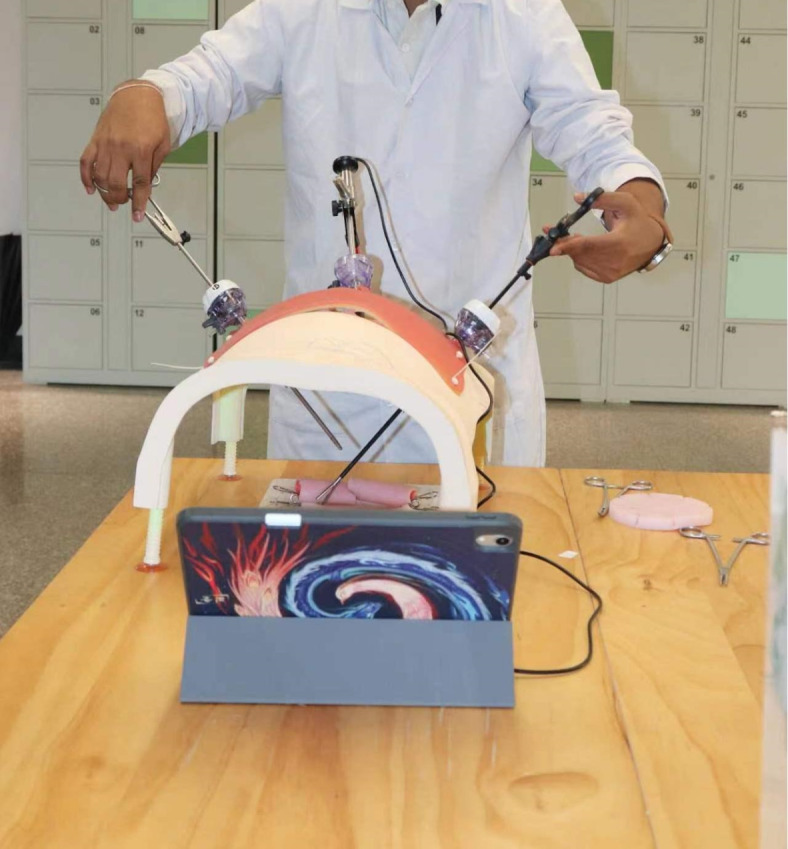
Three-dimensional (3D) printed surgical models provide an excellent surgical training option to closely mimic real operations to teach medical students who currently rely largely on visual learning aided with simple suturing pads. There is an unmet need to create simple to complex surgical training programs suitable for medical students. A prospective cohort study was conducted on a group of 16 6th year students. They were randomly divided into two groups for suture training on a basic training pad or on unique 3D-printed intestinal anastomosis models. After 4 weeks of open and laparoscopic surgical training, exams were performed on the standardized 3D-printed model at the end of each stage to assess surgical performance including surgical time and scores. Both groups had similar skills before the start of each stage. In stage 1, both groups showed comparable learning performance, but the 3D model group performed better in Exam 1. In stage 2, the 3D model group took more time but showed significant improvements and outperformed the pad group in Exam 2 in both performance scores and time. Post-training questionnaires indicated increased interest in surgery and technical training among students using 3D models. Realistic 3D-printed models benefit surgical training, expected to become integral in teaching operative skills and techniques to medical students.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-84887-y.
Keywords: Medical education, Surgical training, 3D-printed model, Intestinal anastomosis, Laparoscopic and open operative skills
Subject terms: Small intestine, Biliary tract, Bile ducts, Preclinical research
Introduction
The start of clinical rotations in 6th year in a medical program is usually a momentous period for most medical students, where they are allowed to take on the title of medical doctor. During this period, it is important to have a holistic view that involves exposing students to the entirety of the surgical care pathway by incorporating theoretical and practical teaching of operative skills1. Over the years, this unaddressed learning need has resulted in a gap between the theoretical knowledge that medical students are taught and the limited opportunities to apply that theoretical learning to patient care2,3. This gap usually results in the often unaddressed lack of the training of operative skills which may result in inevitable feelings among medical students of unpreparedness for a career as a surgeon4.
Simulation plays an important role in medical student education. Indeed, simulation-based training in surgical education has rapidly developed during the 21st century5. While some aspects of training occur outside the OR, and because trainees are working fewer clinician hours, surgery residents and medical school graduates are still expected to reach the same technical proficiency as their predecessors. Simulation-based training can expose medical students to surgical techniques earlier and thereby improve their operative skills and interest6,7. Benchtop models are one of the oldest models used as tools: they are inexpensive, allow familiarity, and provide unlimited practice opportunities when used appropriately, thereby translating into good operative skills on live patients. These models range from computerized simulation, virtual reality, and foam pads, in addition to the use of human cadavers, porcine cadavers, and live animal models (rat, rabbit, dog). A new alternative model using a 3D-printed dry model based on actual CT- modeled reconstruction from a human bilio-enteric anastomosis as a guide for laparoscopic bile-enteric anastomosis as reported by Wang et al.8 has proven to be a suitable alternative with good outcomes for operative skills training.
If new medical graduates are required to perform procedures independently, such as skin suturing, basic training in surgical skills ideally needs to be taught and evaluated previously. Even for newly qualified doctors (undergoing postgraduate training), the provision of training in surgical skills could flatten the steep learning curve for the residency program and provide standardized training for all newly graduated doctors. Simulation training is highly valued by medical students when learning practical surgical skills, and medical schools are encouraged to teach basic surgical skills using simulation whenever possible1.
Despite advancements in surgical education, there remains a gap in practical training for medical students. This study aims to bridge this gap by introducing 3D-printed models for surgical training. Using a prospective cohort study according to the STROCSS 20219 and CONSORT 201010, we measured the subjects’ scores during stepwise training with subsequent standardized exams to measure outcomes through a validated assessment scale. We also sought to encourage and deepen medical students’ understanding of surgical training and to provide a new model for the future training of novice doctors.
Materials and methods
Ethical approval and research registration unique identifying number (UIN)
The study was reviewed and approved by the Ethics Committee of Zhejiang Provincial People’s Hospital (KY2024012) on 25/01/2024. The study was in accordance with the Helsinki Declaration of 1964 and later versions. The study has been registered in the Chinese Clinical Trial Registry on 05/02/2024. UIN: ChiCTR2400080695. The first participant was recruited on 07/02/2024, and all participants completed their training on 12/04/2024.
Participants
A total of 16 eligible 6th year medical students participated in this study. Their age was 25.0 ± 1.0 years old, and there were 12 males and four females. All were required to be right-handed to avoid any potential influence of handedness because we used surgical instruments that were classically designed for right-handed individuals. They had no previous experience with a surgical rotation and had no experience or training in suturing or other operative skills. All participants completed an informed consent and a short questionnaire regarding their views on surgical training before and after the training. Participants consented to the anonymous processing of the collected data.
Material
The small intestine and bile duct were the primary components of the jejunojejunostomy anastomosis and biliary-enteric anastomosis that were used for the stepwise training. The 3D data (which provided the content for the transfer of patient data) were based on the CT imaging of a healthy patient and were printed using a dual-head silicone printer. E3D digital medical modeling software v17.06 (Central South E3D Digital Medical and Virtual Reality Research Center, China) was used for boundary segmentation and 3D reconstruction, and the model structure was streamlined through manual editing. Open source Cura 4.4.1 slicing software (Ultimaker, USA) was used to create the 3D-printed slices. The material was made of silicone and specialized for 3D printing.
Training curriculum
Stage 1
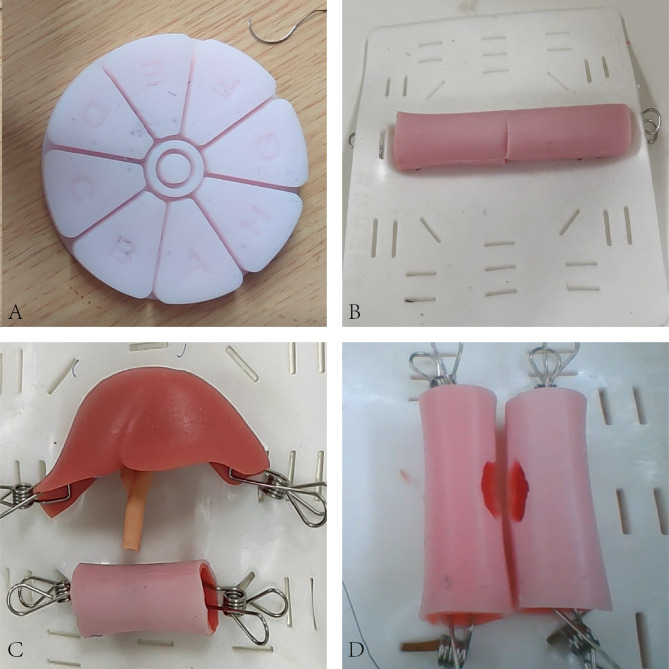
All participants executed four suturing tasks on the given equipment using the basic pad (Fig. 1A) in the following order during the first week:
Knot tying by hand: participants tied a reef knot (also called a square knot) consisting of an underhand and an overhand throw.
Transcutaneous (skin) suturing and knot tying with instruments: participants executed one transcutaneous suture on the incision of their pad and tied the suture using an instrument tie technique.
Vertical mattress suturing—suture and knot tying with instruments: participants executed one vertical mattress suture on the incision of their pad and tied the suture using an instrument tie.
Continuous suturing with knots tied at each end: participants were asked to tie a knot at one end of the board, then apply 4 cm of continuous simple, over-and-over suturing of the edges of the “wound”, and then tie a knot at the end. The knots were tied with an instrument tie.
After one week of training, the participants were randomly divided into two groups according to the randomly generated numbers by observers using computers (eight in each group). The participants in the general group continued the training using the suture pad. The participants in the 3D-printed model group transitioned to training on a 3D-printed intestine model for an end-to-end anastomosis (Fig. 1B). The training involved freehand knot tying, simple interrupted sutures tied with an instrument tie, vertical mattress sutures, and continuous sutures. After 4 weeks of open surgery training, all participants completed Exam 1 by performing a biliary-enteric anastomosis using the model at the end of stage 1 (Fig. 1C).
Fig. 1.
The models used in this study. (A) the basic pad. (B) 3D-printed end-to-end intestinal anastomosis model. (C) 3D-printed biliary-enteric anastomosis model. (D) 3D-printed side-to-side anastomosis model.
Stage 2
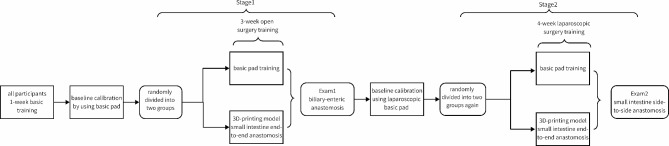
After completing the open training and examination above, all subjects went on to Stage 2 and were randomly divided into two groups again for a 4 week training in laparoscopic surgery (eight in each group). An abdominal simulator was placed on a flat desktop, with a 3D-printed model or pad placed below. 12 mm trocars were placed on the center, left, and right sides of the abdominal simulator for placing laparoscopic instruments. The middle Trocar was used to place a laparoscopic camera, which could be connected to an external screen. The trocars on both sides were used to place laparoscopic instruments, such as forceps, needle holders, and laparoscopic scissors. (Fig. 2) One group of subjects underwent training involving laparoscopic simple sutures, vertical mattress sutures, and continuous suture practice with an instrument tie using the pad under laparoscopy visualization. The other group of subjects underwent surgical training on a 3D-printed end-to-end intestinal anastomosis model, including simple sutures, vertical mattress sutures, and continuous sutures. After 4 weeks of laparoscopic surgery training, all participants completed Exam 2 by performing a laparoscopic side-to-side anastomosis on the model shown in Fig. 1D at the end of stage 2. (Fig. 3)
At the beginning of each stage, an experienced senior surgeon conducted the teaching and suture demonstrations on the use of open and laparoscopic instruments.
Fig. 2.
Laparoscopy visualization set up and surgical training.
Fig. 3.
Flowchart of the study.
Measures
All details from all operations were recorded and downloaded by the simulation trainer and scored by two experienced surgeons. Each participant’s performance was scored at the study site, as the primary endpoints. Each participant’s training time was recorded, as the secondary endpoint. The observer was blinded to the specific order of the observed video. The investigator’s scale for evaluating the trainee’s technical maneuvers was based on the OSATS11 scale and a suture-specific form according to the relevant reported literature12–14. (Table S1-S6)
Data analyses
SPSS software 25.0 was used for the subsequent data analyses and processing. The data with a normal distribution were verified by a two-tailed t-test; the data with a skewed distribution were statistically analyzed by a two-sample rank sum test. Values of P < 0.05 were considered statistically significant. The results from the statistical analyses were entered into GraphPad Prism 10.0, and related charts were drawn. The data were calculated as mean ± standard deviation.
Results
Baseline training and exam scores
At the beginning of the open training (Stage 1), the initial performance of all subjects was evaluated on the basic pad. The performance scores of the basic pad group and the 3D-printed model group were 69.4 ± 11.2 and 74.6 ± 8.5 (full score of 160) (P = 0.313), with times of 9.3 ± 1.9 and 9.1 ± 1.2 min (P = 0.735). The fourth training session was used as the baseline before the group training. The performance scores of the basic pad group and the 3D-printed model group were 94.8 ± 4.6 and 94.2 ± 4.2 (P = 0.829), with times of 7.4 ± 1.4 and 8.2 ± 0.8 min (P = 0.222). There was no statistically significant difference in the scores and times between the two groups. For Exam 1, the performance scores of the basic pad group and the 3D-printed model group were 28.3 ± 1.7 and 31.6 ± 1.7 (full score of 40) (P = 0.001). The time spent on Exam 1 in the basic pad group and the 3D-printed model group was 15.1 ± 2.2 and 14.9 ± 2.45 min (P = 0.818), respectively.
During the Stage 2 laparoscopic simulation training, the initial performance of all subjects was evaluated on the basic pad. The performance scores of the basic pad group and the 3D-printed model group were 50.2 ± 1.8 and 50.1 ± 1.7 (full score of 120) (P = 0.902), respectively. The time spent was 29.6 ± 1.7 and 29.7 ± 1.6 min (P = 0.905). There were no statistically significant differences in the scores and times between the two groups. For Exam 2, the performance scores of the basic pad group and the 3D-printed model group were 25.6 ± 1.6 and 30.0 ± 1.9; P < 0.001). The time they spent was 35.2 ± 8.5 and 26.7 ± 3.0 min (P = 0.018), respectively. There were statistically significant differences between the two groups in both the scores and time spent (Table 1).
Table 1.
Baseline training and exam scores.
| Basic pad group | 3D-printed model group | P value | ||
|---|---|---|---|---|
| First training (all using basic pad) | Score | 69.4 ± 11.2 | 74.6 ± 8.5 | 0.313 |
| Time (min) | 9.3 ± 1.9 | 9.1 ± 1.2 | 0.735 | |
| Fourth training (all using basic pad) | Score | 94.8 ± 4.6 | 94.2 ± 4.2 | 0.829 |
| Time (min) | 7.4 ± 1.4 | 8.2 ± 0.8 | 0.222 | |
| Exam 1 (biliary-enteric anastomosis) | Score | 28.3 ± 1.7 | 31.6 ± 1.7 | 0.001 |
| Time (min) | 15.1 ± 2.2 | 14.9 ± 2.5 | 0.818 | |
| First laparoscopic training (all using basic pad) | Score | 50.2 ± 1.8 | 50.1 ± 1.7 | 0.902 |
| Time (min) | 29.6 ± 1.7 | 29.7 ± 1.6 | 0.905 | |
| Exam 2 (laparoscopic side-to-side anastomosis) | Score | 25.6 ± 1.6 | 30.0 ± 1.9 | <0.001 |
| Time (min) | 35.2 ± 8.5 | 26.7 ± 3.0 | 0.018 |
Scores at the different training stages
In stage 1 of open surgery training, the performance scores of the basic pad group (full score of 160) increased from 91.8 ± 7.3 to 132.1 ± 10.7 and the time spent decreased from 7.3 ± 1.01 to 5.6 ± 0.80 min. The performance scores (full score of 35) of the 3D-printed model group increased from 15.6 ± 2.6 to 29.9 ± 1.3, and the time spent decreased from 21.7 ± 5.9 to 13.5 ± 2.3 min (Fig. 4).
Fig. 4.
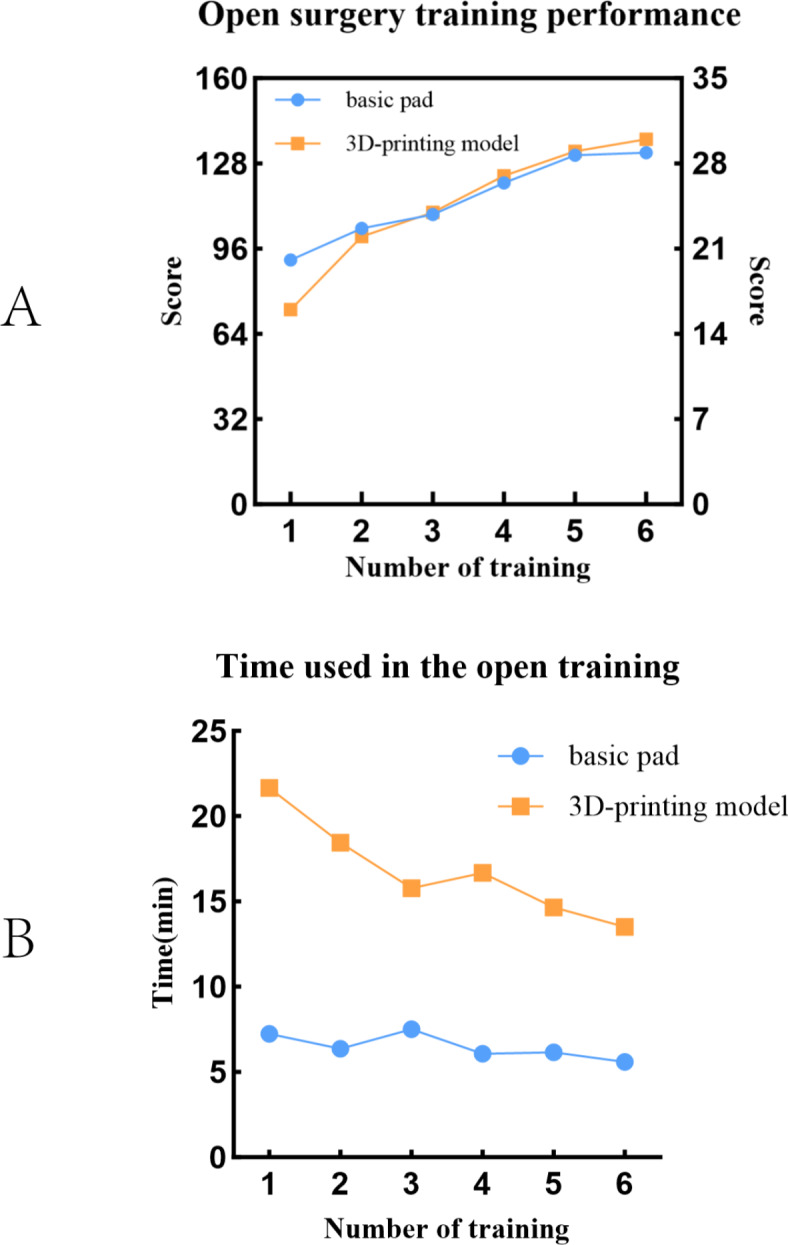
The score and time used in stage 1.
In Stage 2, the laparoscopic surgery training, the performance scores of the basic pad group (full score of 120) increased from 55.0 ± 3.9 to 77.7 ± 5.64, and the time spent decreased from 26.3 ± 4.2 to 21.4 ± 5.5 min. The performance scores (full score of 40) of the 3D-printed model group increased from 20.1 ± 1.5 to 30.2 ± 1.45 and the time spent decreased from 38.6 ± 8.1 to 23.5 ± 2.8 min (Fig. 5).
Fig. 5.
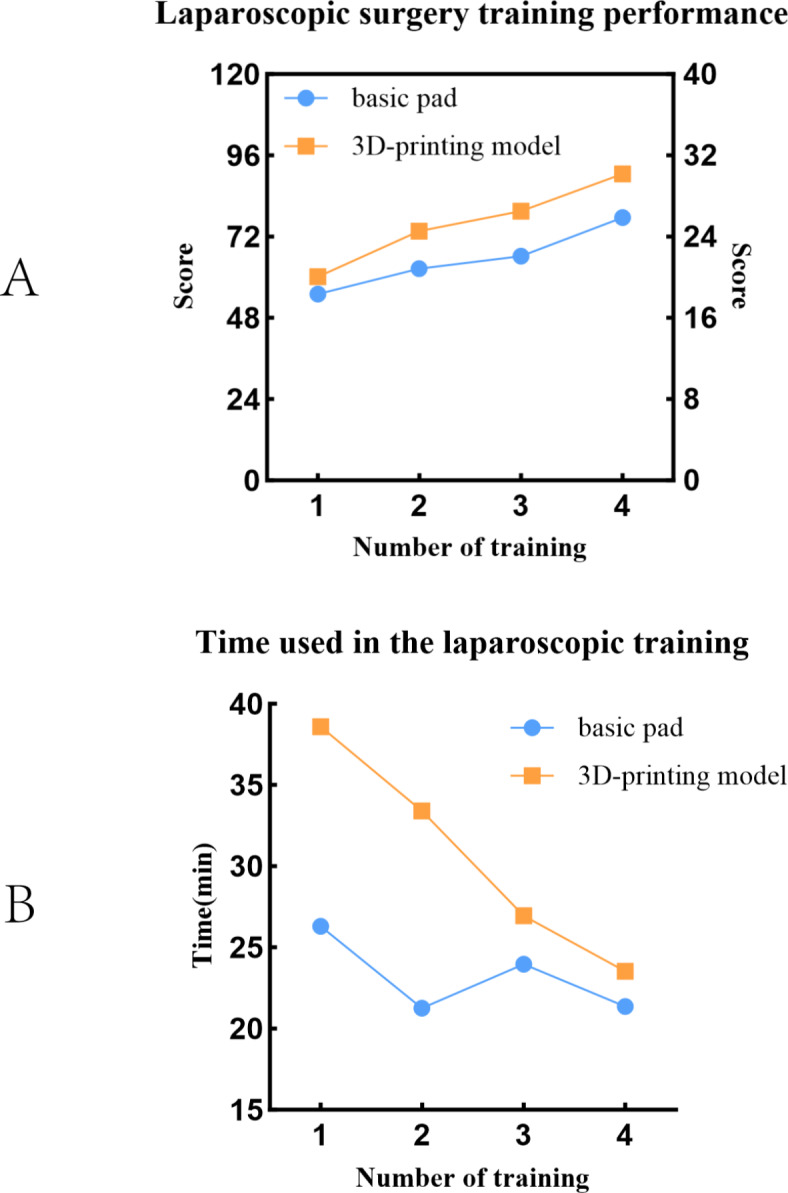
The score and time used in stage 2.
Questionnaire before and after training
All subjects completed a questionnaire survey consisting of five questions (1–10 points, 10 points for maximum), including questions about their views on the use of models for surgical training and evaluation of the comfort and potential of using 3D-printed models (Table 2). The scores of the subjects answering the question on the importance of training increased from 8.1 ± 1.1 to 8.9 ± 1.1 after training (P = 0.029).
Table 2.
Questionare scores.
| Question | Score |
|---|---|
| Before the training | |
| 1. How much improvement do you think you can get through the 3D printing model ? (1–10, 10 means great improvement) | 8.8 ± 1.2 |
| 2. How important do you think it is for medical students to use surgical models for surgical training ? (1–10, 10 means very important) | 8.1 ± 1.1 |
| After the training | |
| 3. Do you think the 3D printing model is comfortable in this training ? (1–10, 10 means very comfortable) | 8.4 ± 1.1 |
| 4. How important do you think it is for medical students to use surgical models for surgical training ? (1–10, 10 means very important) | 8.9 ± 1.1 |
| 5. What do you think about the potential of 3D printing models in improving surgical skills? (1–10, 10 means very important) | 8.4 ± 1.4 |
| 6. Comparison of Question 2 and Question 4 (P value) | 0.029 |
The discomfort of the subjects
All the trainees completed the clinical theoretical study and were able to understand and participate in the experiment. All the subjects were taught by professional and experienced surgeons before the formal training. During the training process, an observer was responsible for evaluating the physical and mental state of the subjects. Neither the basic pad nor the 3D-printed models involve potential biological hazards. All surgical instruments were thoroughly disinfected and properly prepared before use. No puncture injuries occurred in this experiment, and no subjects reported any discomfort in the group survey 1 month after the training.
Discussion
In this study, it appeared that through early exposure to 3D-printed models, trainees could obtain a better training experience for the necessary operative skills that will be required of fully trained doctors once they graduate, which is not only reflected in improvements to their skill scores and reduced operation time, but also in the improvement of medical students” awareness of the importance of surgical training, the strengthening of interest in the field of surgery, and the recognition of the potential of 3D-printed models for future surgical training. Use of the 3D-printed model takes more time than the basic pad, because 3D printing simulates a realistic surgical fit, which includes controlling the position of the overall model, mastering the next surgical steps, and selecting the stitching angle that trainees need to independently control, but the spending of more time in training statistically significantly improved the acquisition surgical skills. The results showed that in stage 2, the 3D printing model group experienced a significant improvement in performance. After only 1–2 rounds of training, their results were on par with those of the control group, who trained for four rounds. They can break through the platform period faster and thus acquire surgical skills more quickly and effectively.
Simulation training replicates the outward qualities of specific objects or processes to realistically depict various clinical scenarios. Traditional simulation for operative suturing focuses on repetitive technical skills using standard suture pads, which some view as insufficient for comprehensive beginner training. This repetitive nature can become monotonous and disconnected from real clinical situations, leading to decreased student interest and engagement, ultimately affecting training effectiveness and surgical practice. However, junior trainees often have limited opportunities to enhance their abilities in traditional operating room settings15. Incorporating laparoscopic surgery training into medical education is essential for providing students with a foundational understanding of minimally invasive techniques, which have become indispensable in modern surgical practice. For medical students who have yet to decide on their future specialty, the objective of basic laparoscopic skill training is not to rapidly transform them into proficient laparoscopic surgeons, but rather to enhance fundamental skills such as hand-eye coordination, spatial awareness, and surgical dexterity—skills that are valuable across all medical disciplines. Additionally, this training fosters a broader understanding of surgical principles, ultimately contributing to the development of well-rounded clinical capabilities. Regulatory bodies like the Accreditation Council for Medical Education (ACGME) in the United States increasingly require surgeons to demonstrate proficiency through surgical simulation programs, including laboratory-based operative training. In regions such as China, high-quality simulation training for medical students and junior doctors remains limited16. Simulation training is widely utilized in various surgical specialties, including digestive17, thoracic, cardiovascular surgery18, orthopedics, and ophthalmology19. Surgeons can enhance their skills and achieve proficiency more rapidly, especially in laparoscopic and robotic surgery, by using continuously improving simulators20.
The use of 3D-printed models is anticipated to replace cadavers as the primary medium for surgical training21. These models, based on CT scan data from healthy individuals and adjusted for material composition, closely mimic actual tissues and provide realistic tactile feedback22. From a financial perspective, recent advancements in printing technology and the availability of more affordable materials have significantly reduced the cost of 3D-printed models. In this study, we employed cost-effective materials and optimized printing protocols, enhancing the scalability and feasibility of the approach. Moreover, the educational benefits, coupled with a reduced reliance on animal or cadaver models, provide a compelling justification for the initial investment. From an environmental standpoint, the adoption of more sustainable practices in 3D printing is essential. The models used in this study are designed for reuse over 8–15 cycles, which helps minimize material waste. While disposable models may be useful in specific training contexts, their environmental impact raises concerns regarding sustainability. Moving forward, it is crucial to explore cost-effective and sustainable materials, as well as recycling mechanisms, such as incorporating replaceable components into the model design23 and investigating the potential for re-melting materials for future prints. These strategies aim to balance educational objectives with environmental responsibility.
Surgical training that incorporates 3D-printed models may require more stringent and standard specific steps, such as a focus on the exact needle insertion site, especially in laparoscopic training where the tissue is visualized by a camera and cannot be “felt”. The appropriate points can be marked on the model to help set the standard site for needle placement, which may help medical students to better master standardized operative skills. What needs to be recognized and emphasized to the learner is that there is no “set final surgical achievement ” in the real surgical world, and surgeons are constantly practicing using qualified technology to perfect their surgical skills. For this reason, the use of set markers for simulation training may affect how medical students improve their surgical skills through continuous trial and error and it may even be conducive to an earlier, more rapid appropriate flattening of the learning curve.
Hand dominance is a concern that is rarely mentioned by surgeons. Manual dexterity appears to have an impact on the final result, whether the suturing is done in the open or laparoscopic setting. The ultimate ambidexterity of left-handed trainees is superior to that of right-handed trainees after dexterity training17,24. In this experiment, the subjects were required to be right-handed and to use the right hand for tying knots to avoid any potential influence of handedness on the use of surgical instruments designed originally for right-handed individuals. Laparoscopic left-handed knot tying can be advantageous when suturing in tight spaces to minimize possible peripheral tissue damage from a right-handed knot technique such as closure of the esophageal hiatus. We believe that this is an area of operative training that warrants further research and exploration in the future.
The 3D visualization system is an advanced innovation that enhances surgeons’ precision when handling complex surgical scenarios, thereby reducing unnecessary injuries caused by differences in visual and tactile perception25. Several studies have compared the roles of 3D visualization systems and 2D views in surgical training26. While 3D visualization systems have shown a positive impact on accelerating skill acquisition to some extent27, some research has revealed that novices trained exclusively with 3D visualization systems tend to perform worse in 2D-view scenarios28. Moreover, these systems have not demonstrated improved outcomes when translated into clinical tasks29, posing a challenge for beginners acquiring foundational surgical skills. As a result, our study did not incorporate the use of 3D visualization systems. On one hand, performing laparoscopic surgeries with a 2D view remains the most commonly adopted approach in operating rooms (OR) today. For beginners, learning and adapting to the 2D laparoscopic view is a critical first step. Therefore, using 3D-printed models designed for 2D views better aligns with the training needs of novice surgeons. On the other hand, the cost of 3D visualization systems can limit their use in non-tertiary hospitals, further constraining their widespread application in training programs. Nevertheless, the 3D visualization system possesses significant potential. We believe its integration with 3D-printed models could enhance surgical training outcomes and facilitate skill acquisition, particularly for more advanced procedures. We look forward to seeing this system applied in training programs for more experienced surgeons, such as residents and fellows, to prepare them for more complex surgical scenarios.
This study has some limitations. First, although one group was exposed to the 3D printed model while the other was not, the focus of this study was on mastering the suture technique and the ability to transfer fundamental skills to a new scenario. We assessed suture skills by using scenarios of varying difficulty levels, which could avoid certain biases. Furthermore, the study did not ascertain the level of interest among medical students in pursuing a career in surgery. This aspect is noteworthy as those intending to pursue surgery may have been more inclined to participate compared to those with different career aspirations. Additionally, it is recommended that future research includes a follow-up to assess the subsequent performance of participating medical students in the surgical field or in their chosen medical/surgical specialty. Although the investigators in this study were from a single center, this approach allowed us to more closely manage the technical evaluations and the research environment. More research in surgical and operative training is worth exploring in the future to explore and promote more high-quality surgical training courses; future work could include the use of a more advanced and improved OSATS scale, including A-OSATS30, and the contemporary scientific evaluation system based on the Messick Validity Framework training system31.
Conclusion
The use of a highly realistic, 3D-printed model appeared to have unique advantages compared to the traditional training model for the operative training of medical students. The use of such more realistic models provides a good bridge for novice doctors to have hands-on contact with and understand real-world operative techniques, operations, and the operating room environment, both in open and laparoscopic settings. Through regular staged surgical training for specific tasks, medical students can master basic suturing skills in both the open and laparoscopic approach in a more comprehensive and rapid fashion.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the cooperation of the medical students who participated in this trial, colleagues from Zhejiang Provincial People’s Hospital and International Education College of Zhejiang Chinese Medical University who contributed to this research. We thank LetPub (www.letpub.com) for linguistic assistance and pre-submission expert review.
Author contributions
Zhihao Zhu and Sidney Moses Amadi contributed equally to this work. Zhihao Zhu writing—original draft, validation, formal analysis and methodology. Sidney Moses Amadi writing—original draft and visualization. Jinlei Mao, Minjun Xia and Menghui Zhou data curation. Nikhilkumar Jagadishbhai Parikh investigation. Junfeng Hu and Zhifei Wang contributed equally to this work. Junfeng Hu conceptualization, supervision and project administration. Zhifei Wang: conceptualization, resources, supervision, funding acquisition and writing—review & editing.
Funding
This work was supported by the fund of The Science and Technology Cooperation Project of Zhejiang Provincial Department of Science and Technology (2024C04027) and The Special Project for Key R&D Tasks of the Xinjiang Uygur Autonomous Region (Project No.2023B03010-1).
Data availability
All original data are available upon reasonable request to the corresponding authors.
Declarations
Competing interests
The authors declare no competing interests.
Research registration unique identifying number (UIN)
The study has been registered in the Chinese Clinical Trial Registry in 05/02/2024.
UIN: ChiCTR2400080695.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Zhihao Zhu and Sidney Moses Amadi.
Contributor Information
Junfeng Hu, Email: hjfeng234@126.com.
Zhifei Wang, Email: zhifei1973@126.com.
References
- 1.Ravi, K. et al. Undergraduate Surgical Education: A Global Perspective. Indian J. Surg.84, 153–161 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bevilacqua, L. A. et al. Surgical Boot Camp for Fourth-Year Medical students: impact on objective skills and subjective confidence. Surgery167, 298–301 (2020). [DOI] [PubMed] [Google Scholar]
- 3.Davis, C. R., Toll, E. C., Bates, A. S., Cole, M. D. & Smith, F. C. T. Surgical and Procedural skills Training at Medical School – a National Review. Int. J. Surg.12, 877–882 (2014). [DOI] [PubMed] [Google Scholar]
- 4.Theodoulou, I., Nicolaides, M., Athanasiou, T., Papalois, A. & Sideris, M. Simulation-based learning strategies to teach undergraduate students Basic Surgical skills: a systematic review. J. Surg. Educ.75, 1374–1388 (2018). [DOI] [PubMed] [Google Scholar]
- 5.Zhang, J. et al. The Transition of Surgical Simulation Training and its learning curve: a bibliometric analysis from 2000 to 2023. Int. J. Surg.110, 3326–3337 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seo, H. S. et al. A one-Day Surgical-Skill Training Course for Medical Students’ Improved Surgical skills and increased interest in surgery as a Career. BMC Med. Educ.17, (2017). [DOI] [PMC free article] [PubMed]
- 7.Bjerrum, F., Thomsen, A. S. S., Nayahangan, L. J. & Konge, L. Surgical Simulation: current practices and Future perspectives for technical skills training. Med. Teach.40, 668–675 (2018). [DOI] [PubMed] [Google Scholar]
- 8.Xia, J. et al. Development and evaluation of a portable and soft 3D-Printed cast for laparoscopic Choledochojejunostomy Model in Surgical Training. Bmc Med. Educ.23, 77 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mathew, G. et al. Strocss 2021: strengthening the reporting of Cohort, cross-sectional and case-control studies in surgery. Int. J. Surg.96, 106165 (2021). [DOI] [PubMed] [Google Scholar]
- 10.Schulz, K. F., Altman, D. G. & Moher, D. Consort 2010 Statement: updated guidelines for reporting parallel Group Randomised trials. BMJ-British Med. J.340, c332 (2010). [Google Scholar]
- 11.Martin, J. A. et al. Objective Structured Assessment of Technical Skill (Osats) for Surgical residents. Br. J. Surg.84, 273–278 (1997). [DOI] [PubMed] [Google Scholar]
- 12.Chang, O. H., King, L. P., Modest, A. M. & Hur, H. Developing an Objective Structured Assessment of Technical Skills for laparoscopic suturing and Intracorporeal Knot Tying. J. Surg. Educ.73, 258–263 (2016). [DOI] [PubMed] [Google Scholar]
- 13.Pintér, Z. et al. Effectivity of Near-peer teaching in training of Basic Surgical skills – a Randomized Controlled Trial. BMC Med. Educ.21, (2021). [DOI] [PMC free article] [PubMed]
- 14.Habti, M. et al. Hand Sewn Anastomosis Skill Acquisition and in vivo transfer using 3D-Printed small Bowel Simulator. J. Surg. Res.288, 225–232 (2023). [DOI] [PubMed] [Google Scholar]
- 15.Reznick, R. K. & MacRae, H. Teaching Surgical skills–changes in the wind. N. Engl. J. Med.355, 2664–2669 (2006). [DOI] [PubMed] [Google Scholar]
- 16.The, L. The best science for achieving healthy China 2030. Lancet388, 1851 (2016). [DOI] [PubMed] [Google Scholar]
- 17.Guerrero-Hernández, A. J., Palacios-Zertuche, J. T., Reyna-Sepúlveda, F. J. & Muñoz-Maldonado, G. E. Laparoscopic training by Use of a physical Simulator and its application in the general surgery residency. Med. Univ. 18, 189–193 (2016). [Google Scholar]
- 18.Giannopoulos, A. A. et al. Applications of 3D Printing in Cardiovascular diseases. Nat. Rev. Cardiol.13, 701–718 (2016). [DOI] [PubMed] [Google Scholar]
- 19.Lee, R. et al. A Systematic Review of Simulation-Based Training Tools for Technical and non-technical skills in Ophthalmology. Eye. 34, 1737–1759 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dehabadi, M., Fernando, B. & Berlingieri, P. The Use of Simulation in the Acquisition of Laparoscopic Suturing skills. Int. J. Surg.12, 258–268 (2014). [DOI] [PubMed] [Google Scholar]
- 21.Ghazi, A. A., Call for & Change Can 3D Printing Replace Cadavers for Surgical Training? Urol. Clin. N. Am.49, 39–56 (2022). [DOI] [PubMed] [Google Scholar]
- 22.Xu, X. et al. Multifunctional High-Simulation 3D-Printed Hydrogel Model Manufacturing Engineering for Surgical Training. Int. J. Bioprint. (2023). [DOI] [PMC free article] [PubMed]
- 23.Wei, F. et al. Reusable modular 3D-Printed Dry Lab Training models to simulate minimally invasive choledochojejunostomy. J. Gastrointest. Surg.25, 1899–1901 (2021). [DOI] [PubMed] [Google Scholar]
- 24.Sabharwal, S., MacKenzie, J. S., Sterling, R. S., Ficke, J. R. & LaPorte, D. M. Left-handedness among Orthopaedic surgeons and trainees. JBJS Open Access.5, e19–e20 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rodrigues, A. C. L. F. et al. 3D Versus 2D laparoscopic distal gastrectomy in patients with gastric Cancer: a systematic review and Meta-analysis. Surg. Endosc.37, 7914–7922 (2023). [DOI] [PubMed] [Google Scholar]
- 26.Restaino, S. et al. Three-Dimensional Vision Versus two-dimensional vision on laparoscopic performance of Trainee surgeons: a systematic review and Meta-analysis. Updates Surg.75, 455–470 (2023). [DOI] [PubMed] [Google Scholar]
- 27.Dawidek, M. T., Roach, V. A., Ott, M. C. & Wilson, T. D. Changing the learning curve in novice laparoscopists: incorporating direct visualization into the Simulation Training Program. J. Surg. Educ.74, 30–36 (2017). [DOI] [PubMed] [Google Scholar]
- 28.Harada, H. et al. The Learning Effect of using Stereoscopic Vision in the early phase of Laparoscopic Surgical training for novices. Surg. Endosc. 32, 582–588 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ajao, M. O. et al. Two-Dimensional (2D) Versus three-Dimensional (3D) laparoscopy for Vaginal Cuff Closure by surgeons-in-Training: a Randomized Controlled Trial. Surg. Endosc.34, 1237–1243 (2020). [DOI] [PubMed] [Google Scholar]
- 30.Schmidt, M. W. et al. Development and Validity evidence of an Objective Structured Assessment of Technical Skills Score for minimally invasive Linear-Stapled, Hand-sewn intestinal anastomoses: the a-Osats score. Surg. Endosc.36, 4529–4541 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Borgersen, N. J. et al. Gathering validity evidence for Surgical Simulation. Ann. Surg.267, 1063–1068 (2018). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All original data are available upon reasonable request to the corresponding authors.