Abstract
Background:
In the context of left breast cancer radiotherapy, long term cardiopulmonary toxicity has been well-documented, significant efforts have been undertaken to mitigate such toxicity by using 4D gating, deep inspiration breath-hold(DIBH) and active breath control(ABC) techniques.
Purpose:
To evaluate and compare the cardio-pulmonary radiation doses incurred during postmastectomy radiotherapy (PMRT) in two distinct breathing conditions such as DIBH and Free Breathing (FB), with a specific focus on the left chest wall with comprehensive regional nodal irradiation.
Materials and methods:
A prospective dosimetric study was conducted on 15 patients who received adjuvant loco-regional radiotherapy of chest-wall (CW), supraclavicular fossa(SCF), and internal mammary region(IMC), with or without axilla. Two sets of planning CT scans were taken in DIBH and FB conditions. The dosimetric difference between DIBH CT and FB CT plans analyzed using Wilcoxon signed-rank test, employing SPSS software version 21.0.
Results:
Comparison of DIBH and FB parameters for target coverage revealed a statistically significant advantage with DIBH in SCF(D95, V90, p<0.017) and IMC(D98, V90 & V95, p<0.03). Dosimetric characteristics of heart and LAD exhibited statistically significant lower doses with DIBH (V20, V25, and Dmean, p<0.001) compared to FB plans. Lung doses were similar with no discernible advantage of one technique over the other. Other OARs such as contralateral breast (p=0.027) and esophagus (p=0.001) received lower doses with the DIBH technique while the spinal cord (p=0.691) and thyroid(p=0.496) showed no significant difference. Maximum heart distance (p= 0.001), central lung distance (p= 0.011) and Haller index (p= 0.001) exhibited statistical significance between the two techniques, whereas chest wall separation showed no significant statistical difference (p=0.629).
Conclusion:
DIBH demonstrates a substantial reduction in cardiac and LAD doses compared to the FB technique. This study underscores the efficacy of DIBH as a viable strategy for mitigating cardiac and LAD radiation doses in left-sided breast cancer patients undergoing PMRT of chest wall with comprehensive regional nodes.
Key Words: Cardiopulmonary toxicity, deep inspiration breath hold, free breathing, postmastectomy radiotherapy
Introduction
Breast cancer is the most frequently diagnosed cancer worldwide and the leading cause of cancer death among women. According to GLOBOCAN 2022, 2.296 million (23.8%) new breast cancer cases are diagnosed worldwide, and in India, the incidence rate is 192,020 (26.6%) cases per year [1]. Radiotherapy (RT) is an integral part of breast carcinoma management after modified radical mastectomy or breast conservation surgery as an adjuvant treatment. Postoperative radiotherapy for breast cancer reduces the risk of local recurrence and improves long-term survival [2]. Alongside improvements in breast cancer outcomes, there are also known long-term cardiac sequelae, in patients who have received radiation therapy for left-sided compared to right-sided breast cancer. During radiotherapy for the left-sided breast cancer, a significant dose is delivered to part of the anterior heart, including the left anterior descending coronary artery (LAD) [3].
The mean heart dose correlates with a proportional increase in the rate of major coronary events per Gray [4]. A pivotal study by Darby et al. observed that patients with breast cancer undergoing adjuvant radiotherapy exhibited a relative 7.4% rise in the rate of major coronary events per 1 Gy increase in mean radiation dose to the heart [5].
Breath-adapted radiotherapy takes advantage of the change in the patient’s anatomy during the respiratory cycle. In the Deep Inspiratory Breath Hold (DIBH) adapted delivery technique, as opposed to free breathing (FB), patients receive radiation only during deep inspiration, when the lungs are inflated, thereby maximizing the distance between the chest wall and heart. This movement causes the heart to shift posteriorly and inferiorly, effectively moving it out of the radiation field [6].
It is essential to ensure that radiation treatments for breast cancer patients are tailored to minimize dose to cardiovascular structures while ensuring adequate dose to the tumor volume and regional lymph nodes [2]. The extent of benefit is not well quantified or understood when comprehensive nodal irradiation, encompassing the internal mammary region with or without axilla, along with the supraclavicular region. The purpose of the study is to evaluate cardiac and lung doses between DIBH and standard FB techniques in patients undergoing postmastectomy radiotherapy (hybrid) for carcinoma of the left breast with comprehensive regional nodal involvement, without compromising on the target coverage.
Materials and Methods
Patient demographics
This hospital-based observational prospective study was conducted from March 2018 to August 2019 on patients diagnosed with left-sided carcinoma breast receiving adjuvant loco-regional radiotherapy after modified radical mastectomy (MRM), i.e., chest wall (CW), supraclavicular fossa (SCF), internal mammary region (IMC) with or without axilla. Fifteen patients were recruited for the study. All are postmastectomy patients.
Women with left-sided breast carcinoma who had undergone MRM and required adjuvant radiotherapy to the left chest wall and internal mammary chain, along with other nodal regions, were included in the study. The inclusion criteria included a performance status score of ECOG 1-2, the ability to reproduce breath-holding for >20 seconds, and willingness to consent. Patients with right-sided breast carcinoma, a history of previous RT to the breast, and known comorbidities (cardiac disease, COPD, Interstitial lung disease, bronchial asthma) were excluded from the study.
CT simulation and image acquisition
All the patients had a Computed tomography (CT) Simulation in a supine position over the Breast Board with the angle position, which brings the chest wall parallel to the treatment couch and the arm placed over the arm support with appropriate angle, ensuring there is no axillary fold. All the patients were trained to hold deep breaths for 20-30 seconds using an RPM (Real-time position monitoring) device. The respiratory cycle was tracked by placing the localizer box. Two sets of planning CT images in the treatment position, one during normal breathing (free breathing, FB) and the other during deep inspirational breath hold (DIBH) were acquired with 2mm slice thickness from the level of the 2nd cervical vertebra to the upper border of adrenals with field of view of 700mm using the Somatom Definition AS Open CT simulator (Siemens Medical Solutions, Germany).
Target Volume Delineation and Treatment Planning
The target (chest wall, supraclavicular region, internal mammary region, and axilla when indicated), OARs (Organs at risk- ipsilateral lung, contralateral lung, heart, LAD, and contralateral breast) and other organs such as oesophagus, liver, thyroid, and spine were delineated as per the RTOG contouring guidelines. The single isocenter 3D conformal field in field (FiF) treatment plans were generated in the Eclipse TPS for both FB and DIBH images. Two conformal tangent beams for the chest wall and one direct anterior beam for the supraclavicular region were added and the FiFs were created in the tangential fields. Both 6MV /15MV photon beams were used for the chest wall and supraclavicular regions respectively. The standard fractionation prescription regimen of 50Gy in 25 fractions to target volume over 5 weeks was used for all the patients requiring comprehensive nodal irradiation. Target volume coverage parameters considered were V95-98%, D98-95%, V102<10%, Dmean of heart <4 Gy.
Dosimetric evaluation
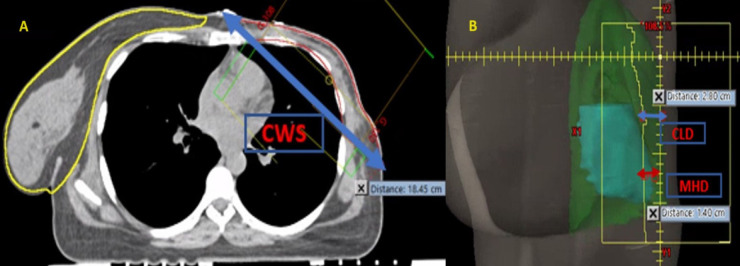
All the plans were evaluated by analyzing dose distribution and dose volume histogram (DVH). Figure 1 shows a dosimetric comparison between DIBH and FB techniques. For the target volumes, the dosimetric parameters such as D95%, D2%, D98%, V90, V95, V100, and Dmean were obtained from the cumulative DVH, and the comparison was made between the DVH of the FB and DIBH plans using Eclipse TPS. The parameters evaluated for the heart are V5, V10, V20, V25, and mean dose, and for the lung V5, V10, and V20.
Figure 1.
Dosimetric Comparison between A) Deep inspiration breath hold and B) Free breathing technique.
The homogeneity and conformity indices (HI and CI) of the FB and DIBH plans were determined and compared. The homogeneity index was calculated by the following formula recommended by the International Commission of Radiation Units and Measures (ICRU, report 83). In addition, the chest wall separation (CWS) (Figure 2A), central lung distance (CLD) and maximum heart distance (MHD) (Figure 2B) were measured as defined by Das et al. [7] (Table 1).
Figure 2.
Measurement Indices: A) Chest wall separation (CWS); B) Central lung distance (CLD) and maximum heart distance (MHD)
Table 1.
Measurement Indices of Various Breast Treatment Parameters [7]
| Parameter | Definition |
|---|---|
| Maximum heart distance (MHD) | The maximum distance of the cardiac silhouette perpendicular to the longitudinal edge of the treatment field. |
| Central lung distance (CLD) | The perpendicular distance from the edge of the tangential field to the posterior part of the anterior chest wall in the middle of the field. |
| Chest wall separation (CWS) | Defined as the non-divergent posterior field edge from the sternum to the lateral exterior aspect of the chest wall. |
| Haller index | Defined as the ratio between transverse diameter of the chest and shortest distance between sternum and vertebrae. The Haller index is measured at the deepest aspect of the thoracic curve, with a normal Haller index ratio calculated as 2 or less. |
| Conformity index (CI) | Conformity index (CI)= VI/TV, where, VI = Reference isodose volume and TV = Target volume. |
| Homogeneity index (HI) | HI = D2-D98/Dmean, where D2 and D98 are the doses received by 2% and 98% of the planned target volumes (PTV) respectively. |
Statistical analysis
Data was summarized as Mean and SD or Median (Inter Quartile Range - IQR) for continuous variables and categorical variables were reported by using numbers and percentages. The difference in parameters between baseline CT scan and DIBH CT, Wilcoxon-signed rank test was used. A p value of <0.05 was considered statistically significant. All the analyses were done by using SPSS software version 21.0
Results
Patient characteristics
All 15 patients received radiation therapy to their left chest wall, left supraclavicular region, and left internal mammary with or without axilla. The mean age of the patients was 48.6 years (range: 33-67 years). Ten out of 15 patients had a BMI >25, and the mean BMI was found to be 25.9 (ranging from 21.5 to 31.2).
Thirteen patients were in stage IIIB, and one patient each was in IIIC and stage IV respectively. In 8 patients tumor was located in the upper outer quadrant, followed by 3 in the lower inner quadrant, and others, the tumor involved more than one quadrant. Comorbidities include diabetes mellitus (4 patients), hypertension (6 patients), combined diabetes and hypertension (3 patients), and no comorbidities in 8 patients.
Treatment characteristics
Among 15 patients, 8 received RT to the chest wall, supraclavicular fossa, internal mammary region & axilla, and 7 to chest wall, supraclavicular fossa & internal mammary region with a radiation dose of 50Gy in 25 fractions over 5 weeks. All 15 patients received perioperative chemotherapy with anthracyclines, taxanes, Trastuzumab, and hormones based on ER, PR, and HER2neu status.
Maximum heart distance (MHD), central lung distance (CLD), chest wall separation (CWS), and Haller index were analyzed for free breathing and DIBH (Table 2). The mean of the MHD, CLD, CWS and Haller index in free breathing technique was found to be 2.57 cm (range 1.93-3.13cm), 2.59 cm (range 1.15-3.51cm), 21.60 cm (range 18.89-25.22cm) and 2.32 cm whereas in DIBH technique, it was noted as 1.57cm (range 0.87-2.17cm), 3.06 cm (range 2.18-4.00cm), 21.90cm (range 19.47-25.40cm) and 2.16cm respectively.
Table 2.
Patient Anatomical Parameters and Dosimetric Correlation (cm, centimeter)
| Parameter | Free breathing | Deep inspiratory breath hold | p value | ||
|---|---|---|---|---|---|
| Mean±SD | Median (IQR) | Mean±SD | Median (IQR) | ||
| Haller index | 2.32±0.19 | 2.2 (2.1, 2.4) | 2.16±0.18 | 2.1 | 0.001 |
| Maximum heart distance | 2.57±0.36 | 2.6 (2.3, 2.9) | 1.57±0.36 | (2.0, 2.3) | 0.001 |
| Central lung distance | 2.59±0.57 | 2.6 (2.3, 2.9) | 3.06±0.46 | 1.6 | 0.011 |
| Chest wall separation | 21.60±1.94 | 20.9 (20.3, 23.6) | 21.9±1.78 | (1.2, 1.8) | 0.629 |
| Conformity index | 1.19±0.15 | 1.2 (1.0, 1.3) | 1.20±0.16 | 1.1 (1.0, 1.3) | 0.615 |
| Homogeneity index | 0.23±0.14 | 0.1 (0.1, 0.2) | 0.13±0.02 | 0.1 (0.1, 0.1) | 0.002 |
Maximum heart distance (p= 0.001), central lung distance (p= 0.011), and Haller index (p= 0.001) showed statistical significance between the two techniques, whereas chest wall separation showed no significant statistical difference (p=0.629).
Conformity index (CI) and homogeneity index (HI)
The DIBH technique allowed more homogenous distribution with HI values of 0.23± 0.14 and 0.13± 0.02 for FB and DIBH techniques respectively (Table 2) and the difference was statistically significant p=0.002. The conformity index was similar for both FB and DIBH techniques (p=0.615). Figure 3A shows a dosimetric box plot of homogeneity index and Figure 3B shows dosimetric box plot of conformity index.
Figure 3.
Dosimetric Box Plot of Deep Inspiration Breath Hold and Free Breathing: A) Homogeneity index with significant p value (p=0.002); B) Conformity index with no significant p value (p=0.615).
Dosimetric characteristics of the heart and left anterior descending artery (LAD)
FB and DIBH plans were evaluated using parameters like V5, V10, V20, V25, and Dmean to the heart (Table 3). V5 corresponds to a low dose spread to the heart in percentage. Statistical analysis showed a significant reduction in dose to heart in the DIBH plans for the parameters (V20, V25, and Dmean) as compared to FB plans with significant difference (p-value 0.001).
Table 3.
Dosimetric Characteristics of Heart, Left Anterior Descending Artery (LAD) and Lungs (Gy- Gray)
| Region | Parameter | Free breathing | Deep inspiratory breath hold | p-value | ||
|---|---|---|---|---|---|---|
| Mean±SD | Median (IQR) | Mean±SD | Median (IQR) | |||
| Heart | V5 | 37.38±12.77 | 33.5 (29.7, 46.6) | 37.40±22.19 | 31.5 (17.0, 56.3) | 0.776 |
| V10 | 17.87±6.23 | 16.9 (13.1, 21.7) | 14.26±14.31 | 8.9 (7.4, 16.3) | 0.053 | |
| V20 | 12.83±3.53 | 13 (10.5, 15.3) | 6.15±2.77 | 5.7 (4.0, 7.3) | 0.001 | |
| V25 | 11.90±3.46 | 12.0 (9.6, 14.4) | 5.17±2.37 | 4.7 (3.4, 6.1) | 0.001 | |
| Dmean | 8.69±1.65 | 8.9 (7.58, 9.75) | 5.73±1.41 | 5.82 (5.16, 6.06) | 0.001 | |
| LAD | Dmax | 51.68±1.65 | 51.34 (50.73, 52.31) | 46.91±9.90 | 49.16 (47.67, 51.23) | 0.006 |
| Dmean | 29.05±7.38 | 29.08 (22.90, 32.93) | 20.95±7.65 | 23.10 (12.22, 25.97) | 0.001 | |
| Left lung | V5 | 56.32±9.93 | 54.9 (49.3, 58.2) | 58.31±11.49 | 56.1 (49.6, 67.4) | 0.394 |
| V10 | 40.04±6.14 | 39.9 (36.5, 42.9) | 38.86±6.48 | 37.2 (35.2, 44.1) | 0.307 | |
| V20 | 30.08±4.31 | 29.7 (27.0, 32.7) | 28.07±4.08 | 27.9 (25.8, 31.4) | 0.078 | |
| Right lung | V5 | 0.324±0.35 | 0.1 (0.0, 0.6) | 0.95±3.14 | 0.1 (0.0, 0.3) | 0.096 |
V20 and Dmean of heart with DIBH 6.15±2.77 and 5.73±1.41 compared to FB were 12.83±3.53 and 8.69±1.65 respectively. Figure 4A shows a dosimetric box plot of V20 of heart and Figure 4B shows dosimetric box plot of Dmean of heart.
Figure 4.

Dosimetric Box Plot of Deep Inspiration Breath Hold and Free Breathing: A) Dosimetric box plot of V20 of Heart with significant p value (p=0.001); B) Dosimetric box plot of Dmean of heart with significant p value (p=0.001); C) Dosimetric box plot of V90 of Internal mammary node with significant p value (p=0.008). (FB, Free breathing; DIBH, Deep inspiration breath hold)
LAD doses were evaluated in FB and DIBH plans with two different volume parameters (Dmax and Dmean). Delineation of LAD was restricted due to the slice thickness, and motion artifacts (DIBH). A significant reduction in doses to the LAD in the DIBH plan was observed in comparison to the FB plan (Table 3).
Dosimetric characteristics of left and right lungs
The mean of V5, V10, and V20 of the left lung showed only a small difference in DIBH in comparison with the FB plan, they were found to be statistically insignificant (p-value>0.05) (Table 3). There was a statistically insignificant difference between the FB and DIBH plans for V5 of the right lung (p-value 0.096) (Table 3).
Dosimetric characteristics of supraclavicular region
Among the V90, V95, V100, D2, D95 and D98 parameters, V90, D95, and D98 showed statistically significant advantages with DIBH in comparison to FB, whereas V95, V100, and D2 showed no statistical significance (Table 4).
Table 4.
Dosimetric Characteristics of Left Supraclavicular Region (SCL) and Internal Mammary Nodal (IMN) Region (Gy- Gray)
| Region | Parameter | Free breathing | Deep inspiratory breath hold | p-value | ||
|---|---|---|---|---|---|---|
| Mean±SD | Median (IQR) | Mean±SD | Median (IQR) | |||
| SCL | V90 | 93.75±2.85 | 94.30 (91.5, 96.7) | 95.67±2.09 | 96.20 (94.0, 97.2) | 0.017 |
| V95 | 86.16±7.62 | 88.50 (82.7, 90.9) | 88.77±5.94 | 88.90 (84.5, 93.6) | 0.307 | |
| V100 | 59.97±15.36 | 64.20 (53.8, 70.5) | 61.01±15.13 | 59.90 (50.2, 73.0) | 0.733 | |
| D2 | 53.22±0.76 | 53.09 (52.86,53.50) | 52.39±2.49 | 53.05 (52.62,53.59) | 0.363 | |
| D95 | 43.62±2.82 | 44.43 (42.57,45.92) | 47.61±8.45 | 45.72 (44.26,46.75) | 0.02 | |
| D98 | 38.03±4.54 | 38.16 (33.90,42.02) | 41.74±5.16 | 42.72 (38.12,43.83) | 0.027 | |
| IMN | V90 | 57.33±23.09 | 52.70 (49.3, 69.7) | 82.39 | 84.9 (69.5, 95.0) | 0.008 |
| V95 | 44.03±23.65 | 38.20 (20.5, 58.7) | 63.82 | 67.5 (50.0, 76.9) | 0.015 | |
| V100 | 25.42±19.72 | 21.80 (6.6,40.2) | 30.57 | 26.2 (13.0, 43.3) | 0.307 | |
| D2 | 52.59±2.11 | 52.66 (50.75,53.64) | 52.2 | 51.96 (51.45,53.35) | 0.82 | |
| D95 | 29.07±12.20 | 33.56 (17.82,35.20) | 37.19 | 43.17 (35.88,45.12) | 0.053 | |
| D98 | 25.87±11.35 | 30.35 (15.38,32.39) | 34.97 | 41.1 (30.18,43.89) | 0.031 | |
| Dmean | 42.51±7.03 | 44.23 (39.75,46.71) | 47.1 | 48.03 (46.32,48.77) | 0.041 | |
Dosimetric characteristics of the internal mammary nodal region (IMN)
Among the parameters analyzed, V90, V95, D98, and Dmean showed a statistically significant advantage with DIBH in comparison to FB, whereas V100, D2, and D95 showed no statistical significance (Table 4). Figure 4C shows higher dosimetric coverage of IMN V90 (median-85: IQR-70,95) in the DIBH technique compared to the Free breathing technique (median 52.7; interquartile range:49.3,70).
Dosimetric characteristics of organs at risk (OAR)
The Dmean parameter showed a lower dose with the DIBH technique for the right breast (FB vs DIBH, 0.76±0.42 vs 1.13±0.57, p-value 0.027) and oesophagus (FB vs DIBH, 10.60±3.17 vs 8.24±3.03, p-value 0.001). However, the spinal cord (Dmax; FB vs DIBH, 33.19±3.72 vs 31.30±6.64, p-value 0.691) and thyroid (Dmean; FB vs DIBH, 29.00±5.80 vs 29.24±8.60, p-value 0.496) showed no statistical difference.
Follow up
The follow-up ranged from 6 to 67 months (median 48 months). Four patients had disease progression in the entire cohort. One died of brain metastases at 6 months post-treatment, while three patients are alive with progressive disease (liver metastases at 5 and 25 months, lung metastases at 41 months) at 12, 35 and 50 months post-treatment, respectively. The remaining 11 patients were alive with no evidence of disease
The follow-up of cardiac and lung monitoring was disrupted due to the covid pandemic for most of patients. Twelve patients at 12 months, two at 24 months and 3 at 36 months showed no significant difference in ejection fraction in ECHO, FEV1 and FVC levels in spirometry compared to baseline.
Discussion
The study was performed to evaluate the efficacy of the DIBH technique and its dosimetric advantages over the free breathing technique when regional nodes including IMN were treated in left-sided post mastectomy with FiF conformal radiotherapy.
The effect of BMI
The mean age of patients in our study was 48.6 years (range: 33-67). Ten out of 15 patients had BMI >25 and the mean BMI was found to be 25.9 (ranging from 21.5 to 31.2) which was similar to a study done by Darapu et al. [6], where the mean age was 50 and the mean BMI was 26.
According to Tanguturi et al. [8] a beneficial effect was favored by younger age, greater body mass index (BMI), and larger inspirational lung volume changes which act as independent predictors for Dmean heart between DIBH and FB plans.
There is no significant correlation between BMI and mean heart dose (MHD). BMI negatively correlated with mean lung dose. Lung volume change from FB to DIBH showed a significant correlation with BMI (r=0.31, P<0.001). In patients with high BMI, the lungs expand more than those of low-BMI patients, resulting in a higher dose-sparing benefit [9]. Similarly in our study, patients with high BMI had higher dose-sparing benefits compared to patients with low BMI.
Haller index
According to Lowanichkiattikul et al. [10], the median lung volume was 3160.5cm3 (1830.8– 4754.0) and the median Haller index was 2.43 (1.92–3.56). There was no significant effect of the type of surgery, BMI, lung volume, and the Haller index on the distances of chest wall movement.
In our study, the median of the Haller index is 2.2 in free breathing compared to 2.1 in DIBH. Even though the difference in the median was 0.1, it showed itself to be statistically significant (p-value 0.001).
Heart radiation doses
In a study by Darapu et al. [6], there was a significant reduction in dose to the heart in the DIBH plans compared to the FB plans, with statistically significant p values for the V5, V10, V25, V30, and Dmean dosimetric parameters.
Al-Hammadi N et al. [11], showed voluntary DIBH resulted in a significant reduction of mean cardiac dose from 6.1±2.5 to 3.2±1.4Gy (p < 0.001), the maximum cardiac dose from 51.1±1.4 to 48.5±6.8Gy (p=0.005) and cardiac V25Gy from 8.5 ± 4.2 to 3.2 ± 2.5% (p< 0.001) when compared with FB. Heart volumes receiving high (30–50Gy) and low (10–20Gy) doses were also significantly reduced. The mean dose to the left anterior coronary artery was 23.0 ± 6.7Gy and 14.8 ± 7.6Gy on FB and V-DIBH, respectively (p< 0.001).
In a study by Vuong et al. [12], DIBH and FB plans showed a significant decrease in mean and maximum heart doses in all the patients with individual mean heart doses decreased by an average of 1.12Gy. The average mean heart dose for DIBH plans was significantly lower when compared to FB plans (1.02 vs. 2.12Gy; p <0.0001). Maximum heart dose was significantly lower in DIBH and decreased by an average of 11.88Gy when compared to FB plans (28.33 vs. 43.7Gy; p = 0.0001). In another study by Knöchelmann AC et al. [13], the mean dose of heart was significantly reduced by DIBH from 2.64 Gy to 1.39 Gy (p<0.001), and the mean dose to the LAD was also significantly reduced from 5.68 Gy to 3.88 Gy (p<0.001).
In our study, statistical analysis showed a significant reduction (mean difference of FB and DIBH doses in V20, V25 and Dmean were 12.83-6.15=6.33, 11.90-5.17=6.73 and 8.69-5.73=2.96 respectively) in dose to heart in the DIBH plans for the parameters (V20, V25 and Dmean) as compared to FB plans with statistically significant difference (p=0.001). V20, V25, and Dmean parameters for heart volume support the DIBH technique for left-sided breast cancer patients to reduce the dose to the heart without compromising the target coverage when comprehensive nodal region is treated.
Dosimetric characteristics of LAD showed statistically significant low dose with DIBH ([Dmax, FB vs DIBH, 51.68±1.65 vs 46.91±9.90; p=0.006] [Dmean, FB vs DIBH, 29.05±7.38 vs 20.95±7.65; p=0.001]) as compared to FB technique. Table 5 shows comparative dosimetry of Heart and LAD in left breast cancer with other studies.
Table 5.
Comparative Studies of Dosimetry of Heart and Left Anterior Descending Artery (LAD) (Gy- Gray)
| Study | Region | Parameter | Free breathing | Deep inspiratory breath hold | P value | ||
|---|---|---|---|---|---|---|---|
| Mean±SD | Median (IQR) | Mean±SD | Median (IQR) | ||||
| Knöchelmann et al. (2022)[13] | Heart | Dmean | 2.64±1.26 | -- | 1.39±0.47 | -- | <0.001 |
| V5 | 10.6 ± 12.4 | -- | 6.6 ± 8.5 | -- | <0.001 | ||
| V10 | 3.21±3.03 | -- | 1.26±1.21 | -- | <0.001 | ||
| V25 | 2.20±3.63 | -- | 0.67±0.80 | -- | <0.001 | ||
| LAD | Dmax | 12.43±12.18 | -- | 11.05±9.18 | -- | >0.05 | |
| Dmean | 5.68±5.24 | -- | 3.88±2.59 | -- | <0.001 | ||
| Darapu et al. (2017)[6] | Heart | V5 | 21.44±09.43 | -- | 15.74±9.15 | -- | 0 |
| V10 | 12.42±05.65 | -- | 7.72±5.98 | -- | 0 | ||
| V25 | 9.12±04.71 | -- | 4.85±5.21 | -- | 0 | ||
| V30 | 8.43±4.48 | -- | 4.71±04.57 | -- | 0 | ||
| Dmean | 6.827±2.69 | -- | 4.775±02.59 | -- | 0 | ||
| LAD | V5 | 25.24 ±53.47 | -- | 41.3±19.81 | -- | 0.03 | |
| V10 | 39.52±24.61 | -- | 19.94±15.43 | -- | 0.002 | ||
| V25 | 31.91±24.47 | -- | 12.48±15.74 | -- | 0.002 | ||
| Dmean | 17.84±10.73 | -- | 9.66±6.454 | -- | 0.001 | ||
| Al-Hammadi N et al. (2018)[11] | Heart | Dmean | 6.1±2.5 | -- | 3.2±1.4 | -- | < 0.05 |
| Dmax | 51.1± 1.4 | -- | 48.5±6.8 | -- | |||
| V50 | 0.7±1.1 | -- | 0.2±0.6 | -- | |||
| V40 | 6.2±3.5 | -- | 2.1±1.9 | -- | |||
| V30 | 7.8±4 | -- | 2.8±2.3 | -- | |||
| V25 | 8.5±4.2 | -- | 3.2±2.5 | -- | |||
| V20 | 9.2±4.4 | -- | 3.6±2.7 | -- | |||
| V15 | 10±4.6 | -- | 4.1± 2.9 | -- | |||
| V10 | 11.2±5 | -- | 4.9±3.2 | -- | |||
| LAD | Dmean | 23.0±6.7 | -- | 14.8±7.6 | -- | < 0.05 | |
| Dmax | 49.7±3.4 | -- | 44.3±12.2 | -- | |||
| D50 | 20.4±17.6 | -- | 8.4±11.1 | -- | |||
| Present study | Heart | V20 | 12.83±3.53 | 13.0 (10.5, 15.3) | 6.15±2.77 | 5.70 (4.0, 7.3) | 0.001 |
| V25 | 11.90±3.46 | 12.0 (9.6, 14.4) | 5.17±2.37 | 4.70 (3.4, 6.1) | 0.001 | ||
| Dmean | 8.69±1.65 | 8.9 (7.58, 9.75) | 5.73±1.41 | 5.82 (5.16, 6.06) | 0.001 | ||
| LAD | Dmax | 51.68±1.65 | 51.34 (50.73, 52.31) | 46.91±9.90 | 49.16 (47.67, 51.23) | 0.006 | |
| Dmean | 29.05±7.38 | 29.08 (22.90, 32.93) | 20.95±7.65 | 23.10 (12.22, 25.97) | 0.001 | ||
Joo et al. [4] in their study observed the dosimetric parameters of heart [(Dmean (cGy), V10, V20, V30, V40, V50 and MHD (cm)], lung [Dmean (cGy), V20, V40 and CLD (cm)] and LAD [Dmean (cGy) and Dmax (cGy)] showed significant reduction when compared DIBH with FB techniques. Al-Hammadi N et al. [11], demonstrated that there was no statistical difference in cardiac dose-volume histogram parameters among patients receiving left supraclavicular fossa radiotherapy and patients treated with breast/chest wall radiotherapy alone. Mean dose to the left lung and lung volumes receiving V10, V20, and V30, were statistically significant in the subgroup with the inclusion of supraclavicular fossa both in voluntary DIBH and FB treatment plans respectively.
In our study, V90, D95 and D98 of supraclavicular region showed statistically significant advantage while treating with DIBH in comparison to FB, whereas V95, V100 and D2 showed no statistical significance.
IMN irradiation and DIBH
Whelan et al. [14] demonstrated a reduced recurrence rate of breast cancer, improved disease-free survival, and distant disease-free survival after irradiation of the locoregional lymph nodal system in node-positive and node negative patients with risk factors. In another study [15], treatment of the IMN lymph nodes of right-sided disease compared to left-sided disease where IMNs were not treated showed a 3.7% 8-year OS benefit. In our study, patients with T4b and N2 disease received prophylactic IMN radiation. In our study, IMN coverage was better with DIBH than in the FB technique. Heart dose was reduced with DIBH than in FB technique even when IMN was treated.
Nguyen et al. [16] in their study, reviewed 49 patients who received nodal irradiation, either to a supraclavicular field (SCF) and IMN (16) or to the SCF alone (33) and compared mean heart dose and dose volumes between free breathing (FB) and DIBH treatment plans. DIBH significantly reduced the average mean heart dose (p<0.001) in both the IMN-treated group from 6.73Gy to 2.79Gy (−56.4%) and the IMN-untreated group from 4.77Gy to 1.55Gy (−63.7%). There was a discrepancy of 7.3% difference in relative reduction between IMN-treated and non-treated groups which was not statistically significant (p=0.216). Relative reductions in heart dose volumes were all significantly lower for IMN-irradiated patients (p≤0.012), with the greatest separation in relative heart sparing at low doses (V5, difference = −20.5%, p<0.001) that gradually diminished with increasing dose (V25).
Gaal et al. [17] observed that, among 130 patients enrolled in the study, 88 patients received 3DCRT under DIBH, MHD was reduced by >50%, the heart V25 Gy by >80%, the LAD mean dose by >60% and the LAD maximum dose by about 50% as compared to that under FB. Among the WBI cases, at least one heart/LAD dose parameter was more favorable in the prone or the supine FB plan in 15 and 4 cases, respectively. Nodal doses in a cohort of 30 WBI cases under FB vs. DIBH. WBI with DIBH delivered significantly larger doses to the interpectoral and internal mammary nodes, but a lesser dose to the level 1 axillary lymph nodes than WBI under FB.
In our study, the dosimetric parameters V90, V95, V100, D2, D95, D98, and Dmean were analyzed for the internal mammary nodal region and compared between FB and DIBH plans. Among these parameters, V90, V95, D98, and Dmean showed a statistically significant advantage with DIBH in comparison to FB, whereas V100, D2, and D95 showed no statistical significance.
Dose to contralateral breast and esophagus
Dumane VA et al. [18] demonstrated lower heart doses with DIBH and also V4 and V3 of the contralateral breast/implant. Organs at risk doses for oesophagus, thyroid, and brachial plexus showed a statistically insignificant difference between the FB and DIBH plans.
In our study, we evaluated the Dmean parameter of the contralateral breast, which showed a lower dose with the DIBH technique(p=0.027). Similarly, oesophagus also received a lower dose with the DIBH technique (p-value 0.001). However, the spinal cord and thyroid showed no statistical difference.
Toxicity
Darby et al. [5] reported that radiation-related coronary heart disease (CHD) usually occurs after 10-20 years of completion of radiation therapy, and the relative risk of CHD increases with higher RT doses. Hooning et al. [19] studied the treatment-specific incidence of cardiovascular disease in 4,414 patients who had survived 10 years after treatment and showed that patients who received radiation to the internal mammary nodes as part of their treatment had an increased risk of myocardial infarction (HR 2.55), congestive heart failure (HR 1.72) and valvular dysfunction (HR 3.2) compared to patients with no radiotherapy to IMN.
Radiation pneumonitis is one of the long-term sequelae that will manifest atleast 5-6 years after radiotherapy. Lind Parm and Hardenberg et al. [20] demonstrated an increasing trend of radiation pneumonitis of 4%, 6%, and 14% with average of superior and inferior mid lung distance (ALD) values of 3cm, respectively, though not statistically significant.
Hence, reducing heart and lung doses are pertinent. DIBH should be considered for left-sided breast cancer when the patient can hold their breath as required. Dosimetric parameters for IMN compared between FB and DIBH showed that V90, V95, D98, and Dmean had statistically significant advantages with DIBH in comparison to FB, whereas V100, D2, and D95 showed no statistical significance.
IMN coverage also was better with DIBH than with FB technique. V90, D95, and D98 showed a statistically significant advantage while treating the supraclavicular region with DIBH in comparison to FB, whereas V95, V100, and D2 showed no statistical significance. DIBH technique is largely reproducible and stable during intra-fraction and inter-fraction treatments. It is important to explore the degree of dependence and association between dose-volume parameters and long-term cardiac and lung morbidity and mortality.
Studies showed in patients where dose constraints were not met in the supine 3DCRT+DIBH plans; these patients received irradiation using an alternative technique with improved dose parameters such as WB/CW+nodal IMRT, WB/CW+nodal 3DCRT and IMRT/prone [17]. Multiple techniques exist for sparing cardiac dose, including prone positioning, lateral decubitus positioning, and proton therapy, which can be used independently or in conjunction with DIBH.
If treating the regional lymph nodes without the inclusion of the IMC, cardiac sparing can be achieved using the prone technique. Continuous positive airway pressure (CPAP)with 10 cm H2O pressure has been shown to have similarity in both geometric and dosimetric aspects with DIBH and is currently being evaluated for those who are unable to hold breath adequately [21]. The dosimetric analysis demonstrated that for women receiving whole breast irradiation and regional lymph node irradiation, DIBH significantly decreased cardiac dose for protons and photons. However, due to the physical properties of protons, range uncertainty and variations of RBE and LET remain a challenge that can lead to increased toxicity. Customising planning techniques may help reduce uncertainties, but it may limit plan quality and clinical implementation [22]. The present study is limited by small sample size. A larger study with long follow-up duration is needed to validate the toxicity.
In conclusion, DIBH is an effective method to reduce cardiac and LAD doses while treating the left breast cancer patients under the Forward planning FiF (Field in Field) technique. DIBH showed a substantial reduction of cardiac and LAD doses, but an insignificant reduction of ipsilateral lung doses as compared with the FB technique when regional nodes including IMC are treated. DIBH technique requires appropriate patient selection, training, and technical expertise which can effectively reduce cardiac morbidity without compromising chest wall target coverage and improving regional node coverage including IMN. DIBH should be considered for left-sided breast cancer when the patient can adequately hold breath.
Acknowledgements
I would like to thank Dr Selvamani Backianathan, Dr Mohamathu Rafic K, Mr Joel T, Dr Sunitha Susan Varghese, Dr Patricia S, Dr Rajesh Balakrishnan, Dr Paul Ravindran B for their constant support and help regarding this research.
Approval
This research study was approved by the Institutional Review Board of Christian Medical College, Vellore (IRB no. 11029) and did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Ethics Approval and Participant Consent
This study was approved by the Institutional Review Board of Christian Medical College, Vellore (IRB no. 11029). Written informed consent was obtained from all participants.
Availability of data and materials
Due to the risk of compromizing the privacy of participants, the datasets utilized and/or analyzed during the present research are not accessible to the public. The data would be provided upon reasonable request from the corresponding author.
Conflict of Interest
The authors declare that they have no potential conflict of interest.
Author Contribution Statement
All authors contributed equally in this study.
References
- 1.Available from: https://gco.iarc.fr/today/online, authors. Cancer today: global cancer observatory [Internet] Lyon: International Agency for Research on Cancer: World Health Organization; 2022. [Google Scholar]
- 2.Kunheri B, Kotne S, Nair SS, Makuny D. A dosimetric analysis of cardiac dose with or without active breath coordinator moderate deep inspiratory breath hold in left sided breast cancer radiotherapy. J Cancer Res Ther. 2017;13(1):56–61. doi: 10.4103/jcrt.JCRT_1414_16. [DOI] [PubMed] [Google Scholar]
- 3.Correa CR, Litt HI, Hwang WT, Ferrari VA, Solin LJ, Harris EE. Coronary artery findings after left-sided compared with right-sided radiation treatment for early-stage breast cancer. J Clin Oncol. 2007;25(21):3031–7. doi: 10.1200/JCO.2006.08.6595. [DOI] [PubMed] [Google Scholar]
- 4.Joo JH, Kim SS, Ahn SD, Kwak J, Jeong C, Ahn SH, et al. Cardiac dose reduction during tangential breast irradiation using deep inspiration breath hold: a dose comparison study based on deformable image registration. Radiat Oncol. 2015;10:264. doi: 10.1186/s13014-015-0573-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, Bronnum D, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368(11):987–98. doi: 10.1056/NEJMoa1209825. [DOI] [PubMed] [Google Scholar]
- 6.Darapu A, Balakrishnan R, Sebastian P, Hussain MR, Ravindran P, John S. Is the Deep Inspiration Breath-Hold Technique Superior to the Free Breathing Technique in Cardiac and Lung Sparing while Treating both Left-Sided Post-Mastectomy Chest Wall and Supraclavicular Regions? Case Rep Oncol. 2017;10(1):37–51. doi: 10.1159/000453607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Das IJ, Andrews JZ, Cao M, Johnstone PA. Correlation of 2D parameters to lung and heart dose-volume in radiation treatment of breast cancer. Acta Oncol. 2013;52(1):178–83. doi: 10.3109/0284186X.2012.673737. [DOI] [PubMed] [Google Scholar]
- 8.Tanguturi SK, Lyatskaya Y, Chen Y, Catalano PJ, Chen MH, Yeo W, et al. Prospective assessment of deep inspiration breath hold using 3-dimensional surface tracking for irradiation of left-sided breast cancer. Pract Radiat Oncol. 2015;5(6):358–65. doi: 10.1016/j.prro.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Koide Y, Shimizu H, Aoyama T, Kitagawa T, Miyauchi R, Watanabe Y, et al. Preoperative spirometry and BMI in deep inspiration breath-hold radiotherapy: the early detection of cardiac and lung dose predictors without radiation exposure. Radiat Oncol. 2022;17(1):35 . doi: 10.1186/s13014-022-02002-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lowanichkiattikul C, Dhanachai M, Sitathanee C, Khachonkham S, Khaothong P. Impact of chest wall motion caused by respiration in adjuvant radiotherapy for postoperative breast cancer patients. SpringerPlus. 2016;5:144 . doi: 10.1186/s40064-016-1831-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Hammadi N, Caparrotti P, Naim C, Hayes J, Rebecca Benson K, Vasic A, et al. Voluntary Deep Inspiration Breath-hold Reduces the Heart Dose Without Compromising the Target Volume Coverage During Radiotherapy for Left-sided Breast Cancer. Radiol Oncol. 2018;52(1):112–20. doi: 10.1515/raon-2018-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vuong W, Garg R, Bourgeois DJ, Yu S, Sehgal V, Daroui P. Dosimetric comparison of deep-inspiration breath-hold and free-breathing treatment delivery techniques for left-sided breast cancer using 3D surface tracking. Med Dosim. 2019;44(3):193–8. doi: 10.1016/j.meddos.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Knöchelmann AC, Ceylan N, Bremer M. Left-sided Breast Cancer Irradiation with Deep Inspiration Breath-hold: Changes in Heart and Lung Dose in Two Periods. In vivo. 2022;36(1):314–324. doi: 10.21873/invivo.12704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Whelan TJ, Olivotto IA, Parulekar WR, Ackerman I, Chua BH, Nabid A, et al. Regional nodal irradiation in early-stage breast Cancer. N Engl J Med. 2015;373(4):307–16. doi: 10.1056/NEJMoa1415340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thorsen LB, Thomsen MS, Berg M, Jensen I, Josipovic M, Overgaard M, et al. CT-planned internal mammary node radiotherapy in the DBCG-IMN study: benefit versus potentially harmful effects. Acta Oncol. 2014;53(8):1027–34. doi: 10.3109/0284186X.2014.925579. [DOI] [PubMed] [Google Scholar]
- 16.Nguyen MH, Lavilla M, Kim JN, Fang LC. Cardiac sparing characteristics of internal mammary chain radiotherapy using deep inspiration breath hold for left-sided breast cancer. Radiat Oncol. 2018;13(1):103 . doi: 10.1186/s13014-018-1052-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gaál S, Kahán Z, Paczona V, Kószó R, Drencsényi R, Szabó J, et al. Deep-inspirational breath-hold (DIBH) technique in left-sided breast cancer: various aspects of clinical utility. Radiat Oncol. 2021;16(1):89 . doi: 10.1186/s13014-021-01816-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dumane VA, Saksornchai K, Zhou Y, Hong L, Powell S, Ho AY. Reduction in low-dose to normal tissue with the addition of deep inspiration breath hold (DIBH) to volumetric modulated arc therapy (VMAT) in breast cancer patients with implant reconstruction receiving regional nodal irradiation. Radiat Oncol. 2018;13(1):187 . doi: 10.1186/s13014-018-1132-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hooning MJ, Botma A, Aleman BM, Baaijens MH, Bartelink H, Klijn JG, et al. Long-term risk of cardiovascular disease in 10-year survivors of breast cancer. J Natl Cancer Inst. 2007;99(5):365–75. doi: 10.1093/jnci/djk064. [DOI] [PubMed] [Google Scholar]
- 20.Lind PARM, Marks LB, Hardenbergh PH, Clough R, Fan M, Hollis D, et al. Technical factors associated with radiation pneumonitis after local +/- regional radiation therapy for breast cancer. Int J Radiat Oncol Biol Phys. 2002;52(1):137–43. doi: 10.1016/s0360-3016(01)01715-1. [DOI] [PubMed] [Google Scholar]
- 21.Choi MS, Park RH, Lee J, Cho Y, Chang JS, Kim J, et al. Dosimetric Comparison of CPAP and DIBH for Left sided Breast Cancer Radiotherapy. Adv Radiat Oncol. 2024;9(6):101478. doi: 10.1016/j.adro.2024.101478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stowe HB, Andruska ND, Reynoso F, Thomas M, Bergom C. Heart Sparing Radiotherapy Techniques in Breast Cancer: A Focus on Deep Inspiration Breath Hold. Breast cancer. 2022;14:175–186. doi: 10.2147/BCTT.S282799. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to the risk of compromizing the privacy of participants, the datasets utilized and/or analyzed during the present research are not accessible to the public. The data would be provided upon reasonable request from the corresponding author.