Abstract
Acute barium poisoning is a rare but life-threatening method of suicide attempt, and it is a challenging disease in the emergency department. We report a case of barium carbonate poisoning in a 21-year-old man who ingested a large dose to attempt suicide and presented with gastrointestinal symptoms, gradual muscular weakness, and severe hypokalemia (K+1.63 mmol/L). He was promptly managed with gastric lavage, respiratory support, and large doses of oral and intravenous potassium supplementation. In addition, intravenous sodium thiosulfate and continuous venovenous hemodiafiltration were administered to reduce the serum concentration of barium ions. Following comprehensive treatment, the patient recovered within 5 days and discharged home for 12 days. Clinicians should be vigilant when a patient presents gastrointestinal symptoms and limb weakness, associated with severe hypokalemia and cardiac arrhythmia over a short disease course as these may indicate potential barium poisoning. Furthermore, we advocate for paying more attention to the management of toxic substances and the mental health education of young adults.
Keywords: Barium carbonate, hypokalemia, sodium thiosulfate, gastric lavage, whole bowel irrigation, continuous venovenous hemodiafiltration
Introduction
Acute barium poisoning is a rare but life-threatening method of suicide, which can lead to severe hypokalemia and secondary malignant arrhythmias, systemic hypertension, progressive respiratory muscle weakness, or even cardiac arrest.1,2 While insoluble barium salts are not toxic, soluble barium compounds including barium chloride, barium carbonate, barium sulfide, and barium nitrate cause potassium dysregulation.1,3 Peak plasma concentration occurs 2 h after ingestion.1,2 The prompt and appropriate management would ensure successful rescue and prevent death.
Recent reports indicate an increasing prevalence of intentional ingestion of massive, and high chemical purity barium poisoning for suicide purposes. 4 Indeed, it is a challenging and noteworthy condition in the emergency department (ED). We here report a case of suicidal poisoning by ingestion of a potentially lethal dose of barium carbonate in a young man, and the early and aggressive therapeutic approach yields a favorable outcome.
Case
A 21-year-old previously healthy man (65 kg) was admitted to the ED 2 h after ingesting 20 g analytically pure barium carbonate with nausea, vomiting, heartburn, abdominal pain, dizziness, and gradual lower limb weakness. The patient, a chemistry student, reported that the offending chemical was purchased from an online store for the purpose of suicide; moreover, he bought an opened bottle of barium carbonate that missed approximately 20 g. He drank some milk and vomited once before the ED visit. He had multiple episodes of parasuicide. He was conscious and afebrile. He maintained normal saturation on room air but the respiratory rate was 20 per min, blood pressure 133/79 mmHg, and pulse 48 per min.
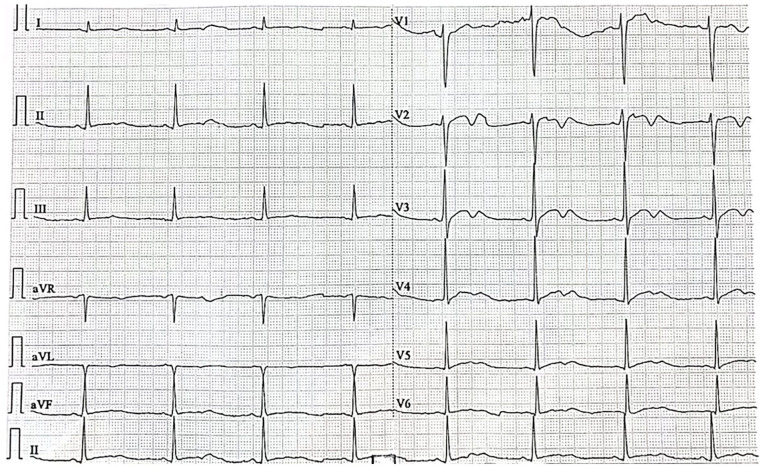
Neurologic examination showed generalized hypotonia and weakness (strength of 4/5) in the lower limbs with normal reflex, and otherwise unremarkable. His first arterial blood gas (ABG) showed pH 7.357 and K+ 2.3 mmol/L. The electrocardiogram (ECG) showed sinus bradycardia, prolongation of QT interval, ST segment depression with U waves, and T wave inversion (Figure 1). The patient was diagnosed with acute barium carbonate poisoning. He underwent gastric lavage under airway protection. Intravenous and enteral potassium supplements were administered to replenish deficits. Intravenous proton pump inhibitors were given to prevent barium dissociation in less acidic gastric conditions. The patient was then admitted to the ICU for further management.
Figure 1.
Electrocardiogram showing sinus bradycardia (48 bpm), prolongation of QT interval, ST segment depression with U waves, and T wave inversion at 2 h post-ingestion.
After his admission to ICU, the patient deteriorated further by profound hypokalemia (K+ 1.63 mmol/L) and metabolic acidosis (pH = 7.314) (Figure 2 and Table 1), managed with rapid administration of potassium chloride via the central line (23 mmol/L per hour) continuously monitoring. He underwent repeated whole bowel irrigations and multiple doses of enteric magnesium sulfate when he was intubated during his first 4 days in ICU. Chest radiograph showed a large high-density mass in the stomach, suspicious of insoluble barium sulfate compounds (Figure 3). Hemodialysis and intravenous 5% sodium thiosulfate (6.4 g every 12 hours) were provided to remove barium ions in the blood. In addition, continuous venovenous hemodiafiltration (CVVHDF) with continuous potassium chloride was administered to stabilize serum potassium and improve strength. Amoxicillin-clavulanic acid was given for suspected mild aspiration pneumonitis.
Figure 2.
Changes in serum potassium, sodium, and creatine concentrations relative to the time post-ingestion.
Table 1.
Changes of serial laboratory data of patients at different times.
| Post-ingestion | ED | ICU | Day 3 | Day 4 | Day 5 | Day 6 | ED Ward | Range | Units | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Day 1 | Day 1 | Day 2 | Day 7–12 | |||||||||||
| 2H | 6H | 9H | 12H | 15H | 18H | 30H | ||||||||
| Serum parameters | ||||||||||||||
| Potassium | 2.31 | 1.75 | 1.63 | 3.27 | 5.09 | 4.07 | 4.11 | 3.97 | 3.76 | 3.71 | 3.5 | 3.73 | 3.5–5.1 | mmol/L |
| Sodium | 138 | 139 | 140 | 136 | 136 | 138 | 140 | 135 | 135 | 137 | 137 | 139 | 136–145 | mmol/L |
| Chloride | 97.7 | 104.7 | 104.5 | 109.7 | 109.7 | 105.7 | 103.4 | 101.8 | 100 | 99.3 | 102.8 | 101 | 98–107 | mmol/L |
| Magnesium | NA | NA | 0.82 | 0.86 | NA | 0.92 | 0.88 | 0.83 | 0.77 | 0.75 | 0.84 | 0.84 | 0.66–1.07 | mmol/L |
| Phosphorus | NA | NA | 0.7 | 0.45 | NA | 0.95 | 0.78 | 0.54 | 0.92 | 0.87 | 0.6 | 1.06 | 0.81–1.45 | mmol/L |
| BUN | 3.8 | 3.9 | 1.4 | 1.1 | 2.2 | 2 | 2.1 | 3.7 | 2.76–8.07 | mmol/L | ||||
| Creatine | 81 | 77 | 55 | 66 | 65 | 53 | 54 | 66 | 62–106 | umol/L | ||||
| Creatine kinase | 140 | 385 | 2471 | 2647 | 1234 | NA | 525 | NA | 0–190 | U/L | ||||
| Creatine kinase MB | 29.2 | 63.6 | 27.7 | 41.4 | NA | NA | NA | NA | 0–25 | U/L | ||||
| LDH | 181 | 167 | 204 | 260 | NA | NA | NA | NA | 135–225 | U/L | ||||
| ALT | 9.9 | 10.4 | 7.7 | 11 | 9.3 | 10.7 | 11.3 | 18.7 | 0–41 | U/L | ||||
| AST | 16.4 | 17.3 | 20 | 33.6 | 20.4 | 22.7 | 17.4 | 18 | 0–40 | U/L | ||||
| Albumin | 71.5 | 75.5 | 61 | 65 | 62.3 | 59.7 | 56 | 59.8 | 35–52 | g/L | ||||
| Arterial blood gas | ||||||||||||||
| PH | 7.345 | 7.314 | 7.387 | 7.298 | 7.386 | 7.350–7.450 | ||||||||
| pCO2 | 4.47 | 4.65 | 5.36 | 4.64 | 4.53 | 4.67–6.40 | kPa | |||||||
| pO2 | 27.8 | 12 | 15.9 | 16.9 | 16.6 | 11.1–14.4 | kPa | |||||||
| Saturation | 99.8 | 96.5 | 98.8 | 98.9 | 99.2 | 95–99 | % | |||||||
| cLac | 1.8 | 1.9 | 0.7 | 1 | 1.4 | 0.5–1.6 | mmol/L | |||||||
| cCa2+ | 1.18 | 1.09 | 1.16 | 1.16 | 1.08 | 1.15–1.29 | mmol/L | |||||||
| cHCO3- | 21.6 | 17.2 | 23.6 | 16.5 | 19.9 | 22.5–26.9 | mmol/L | |||||||
| cHCO3-, st | 23.3 | 18.3 | 23.8 | 17.7 | 21.3 | −1.5 to 3.0 | mmol/L | |||||||
| Base excess | −2.1 | −7.8 | −0.7 | −8.7 | −4.2 | 21–28 | mmol/L | |||||||
ALT: alanine transaminase; AST: aspartate aminotransferase; BUN: blood urea nitrogen; ED: Emergency Department; ICU: intensive care unit; LDH: lactate dehydrogenase; NA: not applicable.
Figure 3.
Chest X-ray showing a large radiopaque mass in the stomach at 7 h (a), less dispersed radiopaque substances at 37 h post-ingestion (b), and absent at 66 h (c) post-ingestion.
His serum potassium returned to normal on day 2. Elevated creatine kinases level peaked at 2647 IU/L at 42h post-ingestion was noted, suggesting secondary rhabdomyolysis, without causing acute kidney injury. He was extubated at 46h post-ingestion. Hemodialysis was ceased on day 3; and sodium thiosulfate on day 6. He regained full strength on day 5. He was discharged from the ICU on day 7 and was discharged home on day 12 after full recovery.
Discussion
Acute barium poisoning is a rare and challenging disease in the ED due to nonspecific symptoms, and rapid progression, especially poor history. Soluble barium compounds are common in modern life. They are used as pest control, explosives, and industrial reagents.1,3 Exposure to barium in the context of acute poisoning is either accidental or suicidal. In a systematic review of 39 case reports (226 human subjects) with acute barium poisoning from 1945 to 2012, Bhoelan et al. determined that the most common cause was accidental food poisoning (61.1%), followed by iatrogenic exposure (22.6%) and suicidal ingestion (10.6%). 4 Having considered the increasing incidence of deliberate self-harm during the COVID-19 pandemic,5–8 there is a concern over increased barium toxicity. In Copeland et al. latest reports on fatal BaCO poisoning, there have been 76.0% accidental in nature (38 cases), 18.0% suicidal (9 cases), 2% homicidal (1 case), and 4% undetermined (2 cases) intent in 50 published cases (from 1925 to 2021; 9 summary the characteristics in Supplemental Table 1). In addition to suicide by barium salt poisoning, Hikin et al. demonstrated 20 post-mortem cases in which intentional sodium nitrite ingestion was a suspected cause of death by the circumstances and biochemical analysis of post-mortem blood nitrite and nitrate levels between January 2020 and February 2022. Among them, 80% noted a history of mental health disorder, depression, self-harm, low mood, previous attempts at overdose, or suicidal ideation. 10 These cases highlight the metal salts such as sodium nitrite and barium carbonate sold as an alternative method of suicide and suggest that the regulation of chemicals is inadequate and psychoeducation requires more attention. Enhancing physician education in the recognition and treatment of depression, along with restricting access to lethal means, can effectively reduce suicide rates. 11 Furthermore, it is essential to implement stricter regulations to limit public access to hazardous chemicals; this includes improving the legal framework that governs the supervision of chemical substances. Additionally, optimizing the management and utilization of chemical drugs is crucial, as well as enforcing a real-name verification system for online purchases.
The clinical symptoms and signs of barium poisoning vary according to the amount ingested. A hallmark of life-threatening barium toxicity is severe hypokalemia which leads to malignant arrhythmias (such as ventricular tachycardiac), skeletal muscle weakness, and paralysis. By competitive antagonism of the potassium channel (the ability of the sodium-potassium pump (Na+–K+–ATP enzyme)) to interfere with K+ diffusion and cause a decrease in extracellular potassium; moreover, barium causes excessive stimulation and excitatory effects on muscles. With ingestion of barium, gastrointestinal manifestation appears within 1–2 h, which however, also aggravates extracellular potassium losses and exacerbates hypokalemia, followed by neuromuscular abnormalities and cardiac arrhythmias at 2–4 h post-ingestion. Patients progress to respiratory failure and cardiac arrest eventually.2,4,12 Secondary rhabdomyolysis with barium poisoning has also been reported. Rebound hyperkalemia is observed in multiple reports, by rhabdomyolysis or iatrogenic reasons.2,13,14 Our patient presented the typical manifestations. Barium poisoning is confirmed by spectrometric analysis of the serum concentrations. However, this was not available in this patient, as well as the emergency laboratory in most hospitals.
The management of barium poisoning includes decontamination, antidotes, the correction of electrolyte abnormalities, and life support. Early gastric lavage with 2%–5% solution of sodium sulfate or magnesium sulfate is effective.12,15 Charcoal is not indicated. Antidote may include sodium thiosulfate and magnesium sulfate. They effectively convert ingested barium to nontoxic insoluble barium sulfate. However, it has been reported that the deposition of barium salt in the renal tubules leads to acute renal injury. 16 It is known that a very high dose of potassium supplement (more than 400 mmol/L) daily is necessary, 12 but overcorrection causes rebound hyperkalemia which is potentially cardiotoxic. Continuous cardiac and electrolyte monitoring is necessary for safe practice.13,14,17 CVVHDF rapidly corrects serum potassium levels by replenishing potassium and reducing barium plasma half-life, 17 and may prevent secondary renal injury and rhabdomyolysis.2,14,16 Recently, Jamshidi et al. described gastroscopy-guided removal of retained precipitate in barium toxicity, suggesting the potential role of endoscopy in toxicology care 18 .
Conclusion
The diagnosis of poisoning is based on both clinical assessment and biochemical measurement. Early recognition has significant prognostic implications. However, early diagnosis is complicated by poor historians and concurrent suicidal acts. Clinicians should be vigilant when a patient presents gastrointestinal symptoms and limb weakness, associated with severe hypokalemia and cardiac arrhythmia in a short disease course, for suspected barium poisoning.
Supplemental Material
Supplemental material, sj-docx-1-sco-10.1177_2050313X241311316 for Non-fatal acute barium carbonate poisoning following suicidal ingestion: A case report by Waiian Leong, Chunlian Li, Yuhui Long, Yanli Wang, Abraham KC Wai, Yi Huang and Feilung Lau in SAGE Open Medical Case Reports
Footnotes
Author contributions: Together W.Y.L., L.C.L., and L.Y.H. treated the patient; L.W.I., H.Y., and L.F.L. made substantial contributions to conception and design; L.W.I. collected clinical data and wrote the original draft; W.A. and H.Y. revised the manuscript. All authors read and approved of the final manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval: Our institution does not require ethical approval for reporting individual cases.
Informed consent: Written informed consent was obtained from the patients for their anonymized information to be published in this article.
ORCID iDs: Waiian Leong  https://orcid.org/0000-0002-2530-8509
https://orcid.org/0000-0002-2530-8509
Supplemental material: Supplemental material for this article is available online.
References
- 1. Schorn TF, Olbricht C, Schüler A, et al. Barium carbonate intoxication. Intensive Care Med 1991; 17: 60–62. [DOI] [PubMed] [Google Scholar]
- 2. Johnson CH, Vantassell VJ. Acute barium poisoning with respiratory failure and rhabdomyolysis. Ann Emerg Med 1991; 20: 1138–1142. [DOI] [PubMed] [Google Scholar]
- 3. Nordberg GF, Costa M, Oskarsson A. Handbook on the toxicology of metals (fifth edition): volume II: specific metals. Academic Press, 2021. [Google Scholar]
- 4. Bhoelan BS, Stevering CH, van der Boog AT, et al. Barium toxicity and the role of the potassium inward rectifier current. Clin Toxicol (Phila) 2014; 52: 584–593. [DOI] [PubMed] [Google Scholar]
- 5. Hill RM, Rufino K, Kurian S, et al. Suicide ideation and attempts in a pediatric emergency department before and during COVID-19. Pediatrics 2021; 147: e2020029280. [DOI] [PubMed] [Google Scholar]
- 6. O'Connor RC, Wetherall K, Cleare S, et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry 2021; 218: 326–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shi L, Que J, Lu Z, et al. Prevalence and correlates of suicidal ideation among the general population in China during the COVID-19 pandemic. Eur Psychiatry 2021; 64: e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wathelet M, Duhem S, Vaiva G, et al. Factors associated with mental health disorders among university students in france confined during the COVID-19 pandemic. JAMA Network Open 2020; 3: e2025591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Copeland CS, Rock KL, Pinhal A, et al. A fatal case report of barium chloride toxicity. J Anal Toxicol 2023; 47: e33–e41. [DOI] [PubMed] [Google Scholar]
- 10. Hikin LJ, Ho J, Morley SR, et al. Sodium nitrite poisoning: a series of 20 fatalities in which post-mortem blood nitrite and nitrate concentrations are reported. Forensic Sci Int 2023; 345: 111610. [DOI] [PubMed] [Google Scholar]
- 11. Mann J, Apter A, Bertolote J, et al. Suicide prevention strategies a systematic review. JAMA 2005; 294: 2064–2074. [DOI] [PubMed] [Google Scholar]
- 12. Gould PD, Sorrell AM, Lupariello AD. Barium sulfide poisoning. Some factors contributing to survival. Arch Intern Med 1973; 132: 891–894. [DOI] [PubMed] [Google Scholar]
- 13. Koch M, Appoloni O, Pharm VH, et al. Acute barium intoxication and hemodiafiltration. J Toxicol Clin Toxicol 2003; 41: 363–367. [DOI] [PubMed] [Google Scholar]
- 14. Sigue G, Gamble L, Pelitere M, et al. From profound hypokalemia to life-threatening hyperkalemia: a case of barium sulfide poisoning. Arch Intern Med 2000; 160: 548–551. [DOI] [PubMed] [Google Scholar]
- 15. Yu D, Yi M, Jin L. Incorrigible hypokalemia caused by barium chloride ingestion. Am J Med Sci 2015; 349: 279–281. [DOI] [PubMed] [Google Scholar]
- 16. Wetherill SF, Guarino MJ, Cox RW. Acute renal failure associated with barium chloride poisoning. Ann Intern Med 1981; 95: 187–188. [DOI] [PubMed] [Google Scholar]
- 17. Wells JA, Wood KE. Acute barium poisoning treated with hemodialysis. Am J Emerg Med 2001; 19: 175–177. [DOI] [PubMed] [Google Scholar]
- 18. Jamshidi N, Dhaliwal N, Hearn D, et al. Life-threatening barium carbonate poisoning managed with intravenous potassium, continuous veno-venous haemodialysis and endoscopic removal of retained ceramic glazes. Clin Toxicol (Phila) 2022; 60: 974–978. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sco-10.1177_2050313X241311316 for Non-fatal acute barium carbonate poisoning following suicidal ingestion: A case report by Waiian Leong, Chunlian Li, Yuhui Long, Yanli Wang, Abraham KC Wai, Yi Huang and Feilung Lau in SAGE Open Medical Case Reports