Abstract
Background:
School-based interventions are crucial for promoting healthy behaviors in children and preventing the spread of diseases. This study aimed to enhance hygiene knowledge and practices (K&P) among school children through a school-based intervention.
Objective:
To improve personal and environmental hygiene K&P amongst primary and middle-grade students in urban squatter settlement schools in Karachi, Pakistan using school-based intervention.
Design:
Quasi-experimental study conducted in three schools over 2 years.
Setting:
Urban squatter settlement schools in Karachi, Pakistan, serving primary, and middle-grade students.
Participants:
A total of 156 students participated in the study, with a majority of 55.77% being girls (n = 87). Pre- and post-intervention assessments were conducted to evaluate the impact of the intervention.
Intervention:
Behavioral Change Communication (BCC) strategies aimed at improving school children’s hygiene K&P.
Primary Outcome Measures:
The primary outcome measures included changes in hygiene K&P pre- and post-intervention, specifically focusing on personal hygiene and environmental hygiene.
Results:
Significant improvements observed post-intervention. Mean knowledge score differences were 20.33 (SD = 5.85) for personal hygiene and 10.08 (SD = 7.72) for environmental hygiene. Practice scores also increased, with mean differences of 2.52 (SD = 1.98) and 2.47 (SD = 2.08) for personal and environmental hygiene, respectively. Statistically significant improvements (P < .05) were noted across most of the hygiene domains.
Conclusions:
The school-based intervention effectively improved personal and environmental hygiene K&P among primary and middle-grade children in urban squatter settlement schools. Key recommendations include integrating hygiene education into the curriculum, providing enabling environment to children and capacity building of school teachers to teach hygiene education.
Keywords: Children, schools, behavior, hygiene, school-based intervention
Background
Young school going children in low-and- middle-income countries (L&MICs) are reported to contact a variety of infectious diseases.1 -5 Potential risk factors that predispose school children to acquire infectious diseases are multifaceted. This comprises of poor hygiene knowledge and behaviors, an unconducive school environment to foster healthy habits, a lack of resources for healthcare services at schools, and an overall inadequate attention to improving health and hygiene of school children. Thus, school-based interventions to improve health and hygiene behavior among children has received attention in the literature.6,7,9,11-13
In L&MICs, school-based interventions with programs on water, sanitation, and hygiene (WASH) are commonly reported.6,7 These are aimed at enhancing school children’s knowledge, attitude and practice (KAP) on WASH, alongside an reduction in communicable diseases.6,7 Hygiene education for children continued to be an important element in such programs which aimed to enhance children’s awareness of healthy practices to prevent the spread of readily transmissible diseases.6,7 In Tanzania, the health education project with a focus on personal hygiene for the control of schistosomiasis and helminth infections showed improvement in mean knowledge scores of school children in the intervention group versus control group (74.2 vs 64.2). 8 Moreover, Khan et al., 2021 9 showed that Pakistani school children demonstrated an improvement in handwashing scores after the education program (P = .0000). In addition, a systematic review conducted in 2020 also showed that 20 out of 29 studies reported a significant increase in at least one measure of hand hygiene, i.e., handwashing, handwashing with soap, or handwashing at critical times (after defecation or before food preparation), compared to a control group. 10
Oral health education programs (OHEPs) have been reported to assess improvements in children’s KAP regarding oral hygiene, with the goal of fostering good dental hygiene.11-13 A meta-analysis of oral health education and promotion programs for school children showed that such programs are effective and improved dental visits, attitudes, as well as brushing and flossing behaviors for three months’ post-intervention among children. (Average OR = 0.67, CI: 0.34, 1.31; P = .23). 11 Another study demonstrated improved oral health indicators such as, brushing teeth twice a day with fluoride toothpaste after an oral health education program that was inclusive of videos, tutorials, and talks by dental hygienists. 12 In addition to improving school children’s hygiene, some studies have also focused on enhancing their eating habits. 13
School-based intervention programs have commonly demonstrated promising results. This overall includes improved knowledge about safe water handling and hygiene practices 14 , improved hand hygiene practices15-16, reduction in diarrhea and other communicable diseases,17 -18 reduced absenteeism rates in school-age children.17 -18 However, there is also an evidence of absence of significant differences between toothbrushing and handwashing between intervention and control groups 19 and factors hindering children’s hygiene practices such as inadequate WASH infrastructure. 20
Unfortunately, school health has not received adequate attention in Pakistan, and this results in a lack of targeted interventions and activities to improve the health and hygiene of school children. 21 Girls often drop out of school as they reach puberty due to inadequate sanitation facilities in their schools. 20 In the local context, KAP surveys have been conducted to assess some of the hygiene components. These, however, failed to capture a comprehensive hygiene assessment amongst younger school children and lacked the comprehensive hygiene intervention.
Rationale
To the best of our knowledge, there is a paucity of studies in Pakistan on school-based interventions to improve personal and environmental hygiene amongst school children. A qualitative study in the local context also pointed to gaps in the curriculum, poor attitudes of parents, teachers, and school management toward hygiene promotion among children, and absence of intersectoral collaboration between health and education departments. 21 The objective of this study was, therefore, to improve hygiene K&P among primary and middle grade school children in urban squatter settlement schools in Karachi, Pakistan using school-based intervention.
Methods
Study design and setting
This implementation research utilized a quasi-experimental study design (pre-post-intervention). The chosen design facilitated the evaluation of BCC interventions in improving hygiene knowledge and the adoption of hygiene practices in the selected school settings without randomization.
The study setting included three schools in Gaddap town, Malir district, in Karachi, Pakistan. The Gaddap town has eight union councils with over 400 villages. The district has approximately 350 primary schools with an average enrollment of 70 to 150 children per school. Sindh Education Textbook curriculum is followed in the schools. The government schools charge minimal fees. Except for a non-governmental organization (NGO) that adopted a government school in which a school health model has been implemented, the rest of the schools in the area lacked health services and health education for children. The socio-demography survey held in 2016 in the community revealed that 60% of the households fell under the lowest wealth quintile, with Sindhi ethnicity. 22 Most (57%) of the dwellings in the community were composed of pucca (concrete) houses. Wood remained the preferred method of cooking fuel; utilized by most households (99%), while the borehole system remained the preferred source of water. Due to the unavailability of public sector healthcare facilities, community members (98%) availed services from the private sector. 22
Sample size and sampling technique
The sample size of school children was calculated using Number Cruncher Statistical Systems (NCSS) Pass version 16 software. To determine the sample size, a mean difference of 5.0 and a standard deviation (SD) of 27 was used, reflecting the variability across the various hygiene domains. This approach aimed to achieve 80% power at a significance level (alpha) of .05. Using the paired means calculation, the estimated sample size was calculated as 231 participants. To account for a 20% dropout rate across three schools, the targeted sample size was rounded to 277 participants, ensuring sufficient power for pre- and post-intervention assessments.
To achieve the desired sample of school children, three schools in the district of Malir (each with an average enrollment of 70–150 children) were purposively recruited for the study. The identified schools were endorsed by the Taluka Education Office (TEO), as all of them featured similar lower socio-economic situations. This included an NGO adopted (government school) and two government-managed schools. The NGO-adopted school underwent renovation in 2019. A school health program was implemented in collaboration with a private healthcare organization. The NGO adopted school offers education up to secondary grade. In contrast, the government-managed schools provide education only up to middle grade. The WASH infrastructure in the government schools was inadequate, while the NGO-adopted school had some basic WASH facilities.
Using the census approach, we recruited all enrolled students from primary to the middle grades at the three schools. Overall, 156 children completed the pre-post-intervention phases of the study.
Study participants and inclusion criteria
Study participants included school children. Inclusion criteria included children enrolled in the primary grade (class 1-5) and middle grade (6-8) with informed consent given by mothers, and assent given by children. Inclusion criteria for schools included their location in urban squatter settlements in Karachi, Pakistan, and the willingness of the school administration to execute the research activities by the study team.
Data collection methods
A structured survey questionnaire to measure hygiene K&P among school children was developed. For this study, the definition of hygiene provided by Boot and Cairncross (1993) 23 was used: “Hygiene is the practice of keeping oneself and one’s surroundings clean, especially to prevent illnesses or the spread of diseases.” Building on hygiene indicators used in previous studies,24,3,8,14 our tool measured a total of seven aspects of personal hygiene and three aspects of environmental hygiene. Personal hygiene assessed a total of 31 indicators across seven aspects: hand hygiene (7), sneezing and coughing etiquette (2), oral hygiene (10), ear hygiene (2), food hygiene (4), drinking water (3), and personal grooming (3). For environmental hygiene, there were a total of four indicators. All these indicators were used as proxies for the overall hygiene-related K&P of school children. The survey questionnaire had a separate set of questions for all indicators with closed-ended responses. Simple questions were included which children could easily comprehend and respond to. For example, “do you wash hands before eating at home? What do you use for hand washing at school? Do you take bath daily? What do you use to clean teeth? Do you throw trash/garbage outside the home/street/from vehicles?” The survey questionnaire also had questions requesting students to demonstrate the method of hand washing. The responses were captured to assess whether or not all six standard handwashing steps were performed by the students. The operational definitions of all the indicators are depicted in Table 1.
Table 1.
Operational definitions.
| Serial number | Hygiene DOMAINS |
|---|---|
| 1. | Personal hygiene |
| Personal grooming | |
| Knowledge | |
| ■ Benefits of taking bath | |
| Practice | |
| ■ Demonstration of overall good hygiene (wearing clean uniform, properly combed hairs, clean nails, and overall good hygiene) | |
| 2. | Hand hygiene |
| Knowledge | |
| ■ Use of soap for hand hygiene | |
| ■ Benefits of handwashing with soap | |
| ■ Use of nail cutter for nail hygiene | |
| Practice | |
| ■ Handwashing with soap pre &post meals and after using toilet (at home) | |
| ■ Handwashing pre &post meals and after using toilet (at school) | |
| ■ Use of nail cutter | |
| ■ Six handwashing steps | |
| 3. | Sneezing and coughing etiquette |
| ■ Cover cough and sneeze with elbow | |
| 4. | Food hygiene |
| Knowledge | |
| ■ Wash fruits and vegetables with water | |
| ■ Consider eating food from road hawkers as harmful to health | |
| 5. | Drinking water |
| Knowledge | |
| ■ Boiling as a method for water purification | |
| ■ Advantages of boiling water | |
| ■ Diseases that can be spread by drinking water directly from hand pump/boring/tap water/tanker | |
| 6. | Oral hygiene |
| Knowledge | |
| ■ Toothpaste for oral hygiene | |
| ■ Benefits of using toothpaste | |
| ■ Food items (sugary food, paan a , betel nuts, and gutka b ) harmful to oral hygiene | |
| ■ Knowledge about oral cancer by frequent consumption of paan, betel nuts, and gutka | |
| Practice | |
| ■ Use of toothpaste for oral hygiene twice a day | |
| ■ Rinse mouth after having breakfast, lunch, and dinner | |
| ■ Use of circular motion for tooth brushing | |
| ■ Limited consumption of food items (sugary food items such as candies, chocolates, ice creams etc.) | |
| ■ Avoiding paan, gutka, and betel nuts | |
| 7. | Ear hygiene |
| Knowledge and practice | |
| ■ Do not insert any objects into the ear | |
| 8. | Environmental hygiene |
| Knowledge | |
| ■ Diseases that can spread with dirty environment (This includes diarrhea, pneumonia, hepatitis, typhoid, malaria, dengue fever, and chikungunya) | |
| Practice | |
| ■ Practice of keeping the environment clean | |
| ■ Do not throw garbage in the school premises | |
| ■ Do not throw garbage outside the home or on the streets |
This includes areca nut, slaked lime, with or without betel nut and/tobacco product in a betel nut leaf. The composition of the mixture varies geographically. This can also include other substances for flavoring such as coconut, dates, sugar, menthol, saffron, cloves, aniseed, and cardamom. 25
Gutka is a form of smokeless tobacco. 26
Study duration
The study duration was two years (2019-2021) with a pre-intervention phase (December 2019-April 2020), intervention phase (February 2021-April 2021), and post-intervention phase (May 2021-July 2021).
Study Phases
Phase I: Pre-intervention
Before data collection, community stakeholders (teachers and school management) were taken on board, and oriented on the overall scope and objectives of the research to gain their cooperation. The survey tool was translated into the local languages (Urdu and Sindhi). This phase also involved pre-testing of the tools within the catchment area, followed by the necessary amendments to the tool. A workshop was held for the data collectors to train them in interviewing school children. Children were interviewed in the school setting during lunch break. Before initiating the interview, assent was obtained from them after an explanation on the types of questions the research team will ask. This explanation was given at their level of comprehension. Approximately 20 to 25 minutes were spent per child.
Phase II: Intervention
The intervention included BCC through hygiene education sessions for school children. For this purpose, a BCC tool kit was developed with detailed instructions for the execution of eight modules (introduction to overall hygiene, ear hygiene, coughing and sneezing etiquette, oral hygiene, hand hygiene, food hygiene, safe drinking water, and environmental hygiene). 27 The intervention was conceptualized by utilizing Albert Bandura’s Social Learning Theory. 28 This theory postulates that learning takes place within a social context with three different modeling stimuli (live models, verbal instructions, and symbolic) and attention on four key factors (attention, retention, reproduction and motivation). 28
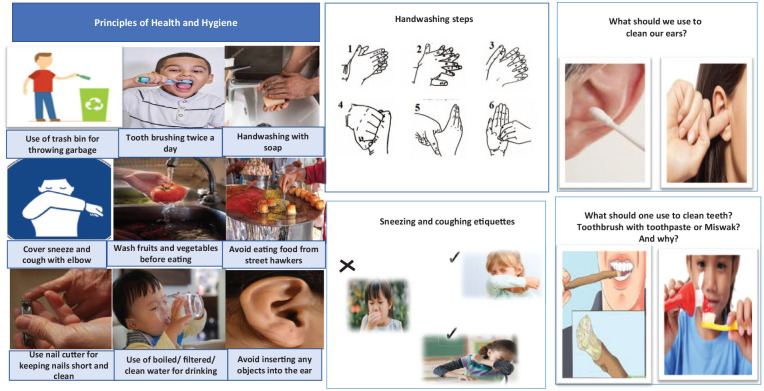
Hygiene behaviors were modeled by the health educators at the schools. 27 Information, education, and communication (IEC) material on personal and environmental hygiene was developed and displayed in school settings to facilitate verbal instructions. This includ hygeine posters. Hygiene games were also developed as part of IEC material, and a model for teeth and toothbrushes was used for oral hygiene component. Figure 1 depicts a snapshot of a few of the IEC materials developed and used to educate children on personal and environmental hygiene. By using IEC material, a series of health sessions were conducted across three schools.
Figure 1.
Behavior change communication tool kit.
This depicts the information, education and communication material used in the study. It consists of posters, picture cards and flyers for school children. Images used in Figure 1 has been taken from below mentioned sources.
https://www.wikihow.com/Use-Miswak#/Image:Use-Miswak-Step-2-Version-3.jpg
https://www.publicdomainpictures.net/en/view-image.php?image=57031&picture=how-to-wash-hands
https://www.moms.com/best-toothpaste-for-kids/
https://www.istockphoto.com/photo/girl-sneezing-into-crook-of-arm-gm182217012-10831985
https://www.freeimageslive.co.uk/free_stock_image/wax-removal-jpg
https://www.almrsal.com/wp-content/uploads/2015/01/Cover-your-mouth-when-coughing-or-sneezing.jpg
https://vectorportal.com/vector/recycling-trash-concept-vector/15918
https://commons.wikimedia.org/wiki/File:Covid_sneeze_etiquette_04.svg
https://www.publicdomainpictures.net/en/view-image.php?image=10739&picture=cutting-nails
https://depositphotos.com/251071372/free-stock-photo-cropped-view-man-holding-soap.html
https://www.flickr.com/photos/30478819@N08/51288109116
https://www.pexels.com/photo/a-person-washing-a-tomato-9831572/
https://www.mumbaionline.in/city-guide/street-food-of-mumbai
https://www.flickr.com/photos/avlxyz/7974322138
Efforts were made to create a school environment that symbolized hygiene practices, encouraging children to learn and adopt healthy behaviors. This was achieved through the display of posters in classrooms and by placing trash bins where needed around the school. Health education sessions focused on children’s cognitive and behavioral processes, helping them to learn hygiene knowledge and practice hygiene behaviors. Children were encouraged to learn and pay attention to hygiene behaviors through different teaching and learning strategies. Retention of key concepts was fostered by repeating the sessions at frequent intervals in school settings. Reproduction of the learned behaviors was ensured by encouraging children to practice hygiene behaviors both at school and at home. To motivate children to practice hygiene behaviors, an attempt was made to create school environment conducive to hygiene by ensuring a functional handwashing facility with soap and the availability of garbage disposal bins). Approximately 8 to 10 days were spent at each school to deliver 10 health education sessions.
Children’s attendance was closely monitored during the sessions. Children who were absent from specific sessions were followed up with to ensure they were also informed of the key messages from the specific modules.
Due to budget limitations, our intervention did not encompass structural enhancements in the schools, such as ensuring a water supply, improving sanitation facilities, and installing handwashing stations, or providing drinking water filters. These elements are typically central in studies assessing the impact of WASH interventions in school environments.6,7 Although our sampled schools had basic WASH infrastructure, upgradation was needed to better encourage hygiene practices among students. What distinguishes our intervention from the previous WASH studies is its holistic hygiene assessment (evaluating eight domains across personal and environmental hygiene) and the use of BCC strategies to actively engage school children.
Intervention fidelity
Intervention fidelity refers to the degree to which a specific intervention is implemented as intended. 29 In the context of this study, instructional modules were developed to ensure the correct execution of the BCC intervention, focusing on indicators related to personal and environmental hygiene mentioned in the earlier section. Each module included a series of steps for facilitators to implement the BCC sessions. This included step 1—Learner’s objectives, step 2— Brainstorming exercise, step 3—Health information specific to the module, step 4—Assessing knowledge retention through exercise/storytelling, step 5—Motivating children to share specific hygiene messages at home, and step 6—Facilitator self-evaluation on the conduct of the module. 27 All instructional modules were translated into the local language and were pre-tested in the neighboring schools to guage learners’ comprehension to understand the hygiene concepts. A workshop was held for the two health educators recruited to implement the hygiene modules in the school settings. A visit was held by the Principal Investigator (PI) during the execution of the intervention to ensure adherence to BCC sessions as laid out in the modules.
Phase III: Post-intervention
Post-intervention phase facilitated us to determine the effectiveness of the school-based interventions by measuring the level of change in the hygiene literacy and practices of school children through end line survey questionnaires (as executed in Phase I). On average, 8 to 10 days were spent at each school to trace school children who participated in the pre-intervention phase and interview them.
Data analysis
The study utilized Statistical Software Package (STATA) version 16.1. This is a widely used statistical tool for data processing and analysis. Initially, descriptive statistics were employed to characterize the data. To assess differences between pre-test and post-test scores of K&P, McNemar tests and paired sample t-tests were used as appropriate.
Scoring method
Our analysis begun by calculating the mean proportions from the pre- and post-survey results of school children, focusing on their K&P. To facilitate interpretation, these proportions were converted into scores and categorized into three levels: poor (<50), fair (50-75), and good (>75). This initial classification offered a clearer structure for understanding participants’ K&P levels, enabling us to capture and describe distinct ranges of K&P within the group.
Binary indicator for McNemar test
For the McNemar test, the “poor” and “fair” categories were combined into a group labeled “inadequate” and the “good” category was labeled “adequate.” This binary classification was necessary for the statistical test, which requires a dichotomous outcome. Our cutoff of 75% is justified, as achieving higher levels of knowledge is essential to practice hygiene behaviors.
Results
Demographic variables of the school children such as age, gender, and grades are illustrated in Table 2. The children enrolled in primary and middle grades had a mean age of 9.09 ± 2.56 years. Most of the chidlren were girls, accounting for 55.77% (n = 87). Furthermore, children were distributed across various grade levels, with Grade I represent the largest proportion at 35.26% (n = 55), followed by Grade III at 21.15% (n = 33), Grade II at 19.23% (n = 30), Grade IV at 13.46% (n = 21), and Grade V at 10.90% (n = 17).
Table 2.
Socio-demographic variables of participants.
| VARIABLES | n (%) |
|---|---|
| Age a | 9.09 + 2.56 |
| Sex | |
| Male | 69 (44.23) |
| Female | 87 (55.77) |
| Grade | |
| I | 55 (35.26) |
| II | 30 (19.23) |
| III | 33 (21.15) |
| IV | 21 (13.46) |
| V | 17 (10.90) |
Mean + SD for age.
Table 3 exhibits the mean differences and standard deviations of pre- and post-intervention K&P scores for environmental and personal hygiene. Mean difference in knowledge scores for personal hygiene was 20.33 (SD = 5.85), while for environmental hygiene, it was 10.08 (SD = 7.72). With regards to changes in practice, a slight increase was noted for personal hygiene 2.52 (SD = 1.98) and environmental hygiene 2.47 (SD = 2.08).
Table 3.
Assessment of mean differences in the knowledge and practice scores among participants (pre- and post-intervention).
| Variables | Mean difference | Standard deviation | P-value |
|---|---|---|---|
| Knowledge score for personal hygiene | 20.33 | 5.85 | <.001 |
| Knowledge score for environmental hygiene | 10.08 | 7.72 | <.001 |
| Practice score for personal hygiene | 2.52 | 1.98 | <.001 |
| Practice score for environmental hygiene | 2.47 | 2.08 | <.001 |
A statistically significant change (p < .05) was observed among most of the children’s K&P indicators post-intervention as shown in Tables 4 and 5 respectively.
Table 4.
Knowledge indicators related to hygiene.
| SERIAL NUMBER | Knowledge indicators | Adequate knowledge | ||
|---|---|---|---|---|
| Baseline | Endline | P-value | ||
| n (%) | n (%) | (<.05) | ||
| Personal grooming | ||||
| 1. | Benefits of taking bath | 141 (90.38) | 145 (92.95) | <.001 |
| Hand hygiene | ||||
| 2. | Use of soap for hand hygiene | 152 (97.44) | 156 (100) | <.001 |
| 3. | Benefits of handwashing with soap | 141 (90.38) | 149 (95.51) | <.001 |
| 4. | Use of nail cutter for nail hygiene | 150 (96.15) | 156 (100) | <.001 |
| Sneezing and coughing etiquette | ||||
| 5. | Cover cough and sneeze with elbow | 1 (0.64) | 145 (92.95) | .001 |
| Food hygiene | ||||
| 6. | Wash fruits and vegetables with water | 129 (82.69) | 156 (100) | .001 |
| 7. | Consider taking/eating food from road hawkers harmful to health | 121 (77.57) | 156 (100) | <.001 |
| Drinking water | ||||
| 8. | Use of boiling as a method for water purification | 73 (46.79) | 150 (96.15) | <.001 |
| 9. | Advantages of boiling water | 107 (68.59) | 146 (93.59) | <.001 |
| 10. | Diseases that can be spread by drinking the water directly from hand pump/boring/tap water /tanker a | 141 (90.38) | 156 (100) | <.001 |
| Ear hygiene | ||||
| 11. | Do not insert any objects into the ears | 5 (3.21) | 3 (1.92) | <.001 |
| Oral hygiene | ||||
| 13. | Toothpaste for oral hygiene | 146 (93.59) | 156 (100) | <.001 |
| 14. | Food items harmful to oral hygiene b | 148 (94.87) | 156 (100) | <.001 |
| 15. | Benefits of using toothpaste | 141 (90.38) | 156 (100) | <.001 |
| 16. | Knowledge about oral cancer by frequent consumption of paan, betel nuts, and gutka | 55 (35.26) | 143 (91.67) | .007 |
| Environmental hygiene | ||||
| 17. | Diseases that can spread with dirty environment c | 140 (89.74) | 156 (100) | <.001 |
This includes three diseases including diarrhea, hepatitis, and typhoid.
This includes at least two out of four food items that children must avoid. This includes paan, gutka, betel nuts and sugary food.
Knowledge about at least three out of seven diseases was assessed. This includes diarrhea, pneumonia, hepatitis, typhoid, malaria, dengue fever, and chikungunya.
Table 5.
Practice indicators related to hygiene.
| Serial number | Practice indicators | Adequate practice | ||
|---|---|---|---|---|
| Baseline | Endline | P-value | ||
| n (%) | n (%) | (<.05) | ||
| Personal grooming | ||||
| 1. | Personal hygiene of the children a | 89 (57.05) | 128 (82.05) | <.001 |
| 2. | Taking bath daily | 87 (55.77) | 124 (79.49) | <.001 |
| Hand hygiene | ||||
| 3. | Six handwashing steps | 5 (3.21) | 92 (58.98) | .002 |
| 4. | Handwashing with soap pre &post meals and after using toilet (at home) | 137 (88.82) | 155 (99.36) | .052 |
| 5. | Handwashing pre &post meals and after using toilet (at school) | 36 (23.07) | 153 (98.08) | .045 |
| 6. | Use of nail cutter | 153 (98.08) | 155 (99.36) | <.001 |
| Sneezing and coughing etiquette | ||||
| 7. | Cover cough and sneeze with elbow | 11 (6.90) | 145 (93.10) | .001 |
| Food hygiene | ||||
| 8. | Wash fruits and vegetables with water | 133 (85.25) | 156 (100) | <.001 |
| 9. | Do not eat food items from road hawkers | 45 (28.85) | 91 (58.33) | .030 |
| Ear hygiene | ||||
| 10. | Do not insert any objects into the ears | 2 (1.28) | - | <.001 |
| Oral hygiene | ||||
| 11. | Use of toothpaste for oral hygiene | 142 (91.03) | 156 (100) | <.001 |
| 12. | Using toothpaste twice a day | 53 (33.97) | 127 (81.41) | .120 |
| 13. | Rinse mouth after having breakfast, lunch, and dinner | 61 (39.10) | 132 (84.62) | .020 |
| 14. | Use of circular motion for tooth brushing | 17 (10.90) | 74 (47.43) | <.001 |
| 15. | Daily consumption of food items (sugary food items such as candies, chocolates, ice creams etc.) | 132 (84.62) | 52 (33.33) | .002 |
| 16. | Daily consumption of paan, betel nut and gutka | 30 (19.23) | 19 (12.17) | <.001 |
| Environmental hygiene | ||||
| 17. | Practice of keeping environment clean b | 146 (93.59) | 156 (100) | <.001 |
| 18. | Do not throw garbage in the school premises c | 68 (43.58) | 135 (86.54) | .002 |
| 19. | Do not throw garbage outside the home/ street d | 55 (35.26) | 130 (83.33) | .056 |
This is demonstrated by children clean uniform, properly combed hairs, clean nails and overall good hygiene.
This includes three practices—encouraging others for using dustbins, not throwing garbage on streets, and not spiting on streets.
The assessment was carried out by asking children whether they engaged in the practice, with response options of ‘always,’ ‘most of the time,’ ‘sometimes,’ and ‘never.’ Children who responded ‘never’ were included.
Majority of the children (97.44%, n = 152) demonstrated good knowledge regarding the use of soap for hand hygiene pre-intervention which increased up to 100% (n = 156) post-intervention (p < .001). Improved knowledge of hand hygiene was also demonstrated by the six handwashing steps which improved from 3.21% (n = 5) at pre-intervention to 58.98% (n = 92) post-intervention (p = .002). Children’s exhibit of correct tooth brushing technique, i.e., a circular motion improved from 10.90% (n = 17) pre-intervention to 47.43% (n = 74) p-value <.001 post-intervention.
Oral hygiene assessments showed that children’s K&P regarding the use of toothpaste were generally high as 93.59% (n = 146) and 91.03% (n = 142) respectively at pre-intervention which significantly improved to 100% (n = 156) post-intervention (p =<0.001). In addition, children’s knowledge of the frequent consumption of paan, betel nuts, and gutka as underlying causes of oral cancer also improved (pre-intervention 35.26% (n = 55) to post-intervention 91.67% (n = 143), p = .007). Children’s awareness on food hygiene also demonstrated significant improvement with regards to avoiding food from road hawkers (pre-intervention = 77.57 (n = 121) to 100% (n = 156) at post-intervention p-value < 0.001). This was also reflected in their practice which improved in terms of avoiding food from road hawkers (pre-intervention 28.85% (n = 45) to post-intervention 58.33% (n = 91), p = .030). Furthermore, there was also significant improvement in sneezing and coughing etiquette amongst children. The knowledge improved from 0.64% (n = 1) pre-intervention to 92.95% (n = 145), p = .001 post-intervention. Improvement in practice was also noted from 6.90% (n = 11) pre-intervention to 93.10% (n = 145) post-intervention p-value (.001).
Of all the indicators assessed in personal hygiene, children’s K&P for ear hygiene remain unchanged. Knowledge (pre-intervention 3.21% (n = 5), post-intervention 1.92% (n = 3)); practice (pre-intervention 1.28% (n = 2), post-intervention (n = 0)).
It was found that the children had an overall good level of K&P regarding environmental hygiene at baseline. Children’s overall knowledge about preventable infectious diseases demonstrated improvement (pre-intervention 89.74% (n = 140), to post-intervention 100% (n = 156), p < .001). Regarding the practice of keeping the environment clean, post-intervention children’s responses also depicted improvement (pre-intervention 93.59% (n = 146), post-intervention 100% (n = 156), p < .001).
Discussion
The current study attempts to address the effectiveness of school-based BCC intervention in improving personal and environmental hygiene among children across three schools located in squatter settlements in Pakistan. The multi-component BCC intervention employed in the study was found to be effective in achieving statistically significant improvement in most of the K&P indicators for personal as well as environmental hygiene amongst young school children.
Adequate literacy and practices in personal hygiene amongst young children is highly effective in reducing infectious diseases.6 -8 Under personal hygiene, hand hygiene remains the most important component to be targeted among young school-going children. Our study demonstrated that a high proportion of children with adequate baseline knowledge about hand hygiene and personal grooming led to further enhancement of their K&P at the endline. The most significant change, with a notable p-value of .002, was observed in adherence to the six handwashing steps, with substantial increase from 3% at baseline to approximately 59% by the endline. The effectiveness of educational interventions to improve hand hygiene while reducing the transmission of infections is well documented.30 -32 Likewise, a systematic review also showed that handwashing interventions targeted at children have great potential for health improvement. 10 Improved handwashing behavior among children offers protection against infectious diseases. A study in Bangladesh also reported improvement in students’ practices of handwashing with soap (4% at baseline to 74% at six weeks post-intervention) in two primary schools using an intervention that included BCC, alongside environmental modifications. 15
It was highly appreciated to note that in the majority of the children, knowledge of the use of soap for handwashing at critical events was remarkably high at baseline (97%), which further increased to 100% at the endline. The handwashing practices at school were found to be lower as compared to home at the baseline (23.07% vs 88.82%). This improved post intervention (98.08% vs 99.36%).
The frequent unavailability of soap and poor water and sanitation infrastructure at two out of three intervention schools were observed as potential barriers to handwashing practices amongst school children.
Diseases affecting oral cavities can be effectively prevented while maintaining good oral hygiene. At baseline, a high proportion of children reported good knowledge of oral hygiene, including the use of toothpaste, its benefits, and food items considered bad for oral hygiene. However, the need for regular oral health education sessions in schools cannot be neglected, especially where populations from lower socio-economic strata are catered to. Our multi-component intervention served to reinforce the existing knowledge amongst children and demonstrated 100% knowledge improvement (p value 0.001) in three out of four knowledge indicators related to oral hygiene.
Owing to the easy access to chewable tobacco for example, gutka (betel quid), betel nut, and paan it was reassuring that the majority (91.67%) of the children were aware of the harmful effects of its usage post-intervention as compared to slightly more than one-third of the children who had this information at baseline. Our intervention also targeted making children conscious and well-informed about the harmful effects of paan, gutka, betel nuts, and sugary food items and how they can potentially increase the risk of developing oral cancer and cavities. The awareness regarding tobacco products has not been underlined in previous studies in the local context and hence makes our study one of its kind. Under oral hygiene practices, a post-intervention improvement was demonstrated in the frequency of using toothpaste twice daily (33.97%, at baseline to 81.41% at endline, p value=0.120) and rinsing mouth after meals (39.10% at baseline to 84.62% at endline, p value=0.020). It was also observed that post-intervention, close to half (47.43%) of the participating children understood and were able to demonstrate the correct brushing technique (with p < .001).
Despite 100% of children being well informed about the food items that were considered harmful to dental hygiene at the end line, the easy availability, and accessibility of food items (paan, gutka, betle nuts, and sugary food) in the school surroundings and at home deters children from adapting positive dietary practices. Our intervention led to positive change in instilling in them the concept of harmfulness from such food items and practically avoiding the daily consumption of harmful food items in 51% of the sample post-intervention. This calls for attention from parents and teachers to reinforce healthy habits in classroom settings. The consumption of sugary foods not only predisposes to poor oral health but also aggravates the effects of leptin and insulin resistance leading to the development of obesity as well as early-onset of type 2 diabetes, especially in those with positive family history33,34 A study assessed the association between eating habits and oral health status in children who consumed sweets and fruit juices and did not follow adequate brushing techniques. These children were found to be at higher risk of developing carious lesions. 35
Though aural (ear) hygiene remains important for proper hearing, it is often neglected and remains unstudied in hygiene research conducted earlier in the local context. 36 Being a neglected aspect under personal hygiene, this not only exposes children but also adults at high risk of acquiring common ear problems including impaired hearing.37,38 Despite BCC efforts to educate children about the ear being a self-cleaning organ and increasing awareness about the risks of using cotton buds, there was no observed improvement in our cohort’s ear hygiene K&P post-intervention. Though our intervention to improve ear hygiene was not successful in terms of raising awareness among children, however, our findings aligned with the previous research which reported the use of cotton buds as the most common practice for ear hygiene.39 -42 The reason attributed to it could be the deeply rooted practice of inserting objects in ears for cleaning purposes which children continually observe in their home environment. To relieve itchiness caused by cerumen deposition in the ear, children usually insert objects which is easily accessible, such as pencils, pens, matchsticks, hairpins, and cotton buds, not knowing that these objects can harm the external auditory canal and lead to infections like otitis externa. 43 Awareness regarding the correct ear hygiene practices, which include refraining from inserting any foreign body inside the ear and using a finger or cloth to clean the ear, needs to be reinforced. A study to assess ear, hygiene practices amongst school children in Nigeria demonstrated that 51.7% of the respondents preferred using cotton buds, followed by other objects harmful to ear. 44
It was appreciated to observe post-intervention knowledge enhancement amongst children on communicable diseases. Environmental hygiene measures had a notable impact on children’s adoption of eco-friendly habits, such as avoiding littering at school and home and maintaining cleanliness by using trash bins. Overall, our study is distinctive not only for its holistic approach to personal hygiene but also for its focus on attention to improving children’s K&P regarding environmentally friendly hygiene. Improvement in personal and environmental hygiene K&P can potentially foster self-regulating and environmentally friendly behavior amongst school children.
Strengths and Limitations
One of the key strengths of this study is that school-based intervention proved to be an effective approach in improving school children’s hygiene literacy and behaviors. The utilization of diverse techniques such as health sessions, instructional modules, quizzes, and pictorial aids showcased variety of approaches towards promoting hygiene behavior change among children. Limitations include the prolonged school closures due to the COVID-19 pandemic, which led to students’ dropouts and impacted the sample size. Additionally, COVID-19 hygiene campaigns might have potentially influenced our study outcomes. Furthermore, the use of pre-post design without control group might have led to confounding variables that could have influenced the study outcomes.
Conclusion
A significant improvement was found in young children’s hygiene K&P after an educational intervention at three urban squatter settlement schools in Pakistan. This study offers some important policy implications and recommendations: (1) Provincial School Education & Literacy Department in Sindh must be sensitized to giving due attention to inculcating basic hygiene concepts and skills among children, (2) District and Taluka Education office must ensure to incorporate BCC on hygiene education in the teaching curriculum, (3) Need assessment of school teachers on building their capacity in delivering hygiene education sessions, (4) Provide an enabling environment to children by displaying hygiene messages to foster positive reinforcement and learning. Furthermore, (5) involving parents as important stakeholders in improving children’s hygiene behavior is crucial. Future research should focus on assessing the long-term sustenance of hygiene K&P among similar cohort.
Acknowledgments
The authors would like to appreciate Ms. Naseem Hashmani; School Lady Health Visitor at the Rural Educational Promotion and Development Society (REPDS), Pakistan for translating the study tools and providing needed assistance in conducting the study. We are grateful to Dr. Shagufta Perveen; Researcher at the South Australian Health and Medical Research Institute, Australia for assisting in data collection. We also thank Mr. Ghulam Issa Khan; Project Coordinator; REPDS, Pakistan, and Mr. Amin Lalani; Project Manager, Construction Management, AKU, Pakistan for providing logistics assistance in the identification of field sites and facilitating access to the key stakeholders in the community, respectively. Furthermore, we would like to express our gratitude to the research assistants for their valuable support in data collection. Special thanks to Ms. Sayeeda Reza for her assistance with language editing. We also appreciate the school children and their mothers for their full cooperation during the data collection process, both before and after the COVID-19 pandemic. Lastly, our acknowledgment goes to the school management of all three schools for their cooperation throughout the study.
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study is funded through the Faculty of Health Sciences Research Committee at AKU (PF 90/1016). The study has undergone peer review by the same institute and comments were incorporated before getting the final approval. Funding is approved for all the activities related to data collection, hiring of human resources, designing, and implementation of intervention, etc. The grant does not cover funds for publication fee charges.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Patient and Public Involevement: Patients and/or the public were not involved in the design, or conduct, reporting, or dissemination plans of this research.
Author Contributions: NAP is the Principal Investigator. NAP in consultation with TS and RK has designed the study protocol. Alongside NAP, MH, LH, and MU contributed to writing the sections in the manuscript. SI reviewed the intervention package and provided needed support in its field execution. LM analyzed the data set and wrote the data analysis and result section. MN and FBH provided needed support in sample size calculation and data analysis. TS and RK provided mentorship. All authors have reviewed the manuscript. All authors have read and approved the final manuscript.
Ethics Approval and Consent to Participate: All ethical considerations were duly taken care of. The study received ethical approval from the Ethics Review Committee (ERC), at Aga Khan University (AKU), Pakistan. (2019–0802-2753). Verbal and written approvals were obtained from the Taluka Education Office and selected schools’ administration before initiating the data collection. Informed consent was obtained from mothers, school children, and school administration. Upon obtaining consent from mothers, children were approached to obtain their assent. A copy of the signed consent form was handed over to the children. The approval process included verbal explanation to the participants on the purpose of the study and data collection methods followed by their written approval in form of signature/name (for children). All methods were carried out in accordance with relevant guidelines and regulations in the Declaration of Helsinki.
Consent for Publication: Consent for publication of the findings has been stated in the consent forms.
Trial Registration: The trial was retrospectively registered with ClinicalTrials.gov 08/05/2019 (https://clinicaltrials.gov/ct2/show/NCT03942523).
ORCID iDs: Nousheen Akber Pradhan  https://orcid.org/0000-0003-3141-2481
https://orcid.org/0000-0003-3141-2481
Muzna Hashmi  https://orcid.org/0009-0005-0090-4880
https://orcid.org/0009-0005-0090-4880
Muhammad Uzair  https://orcid.org/0000-0002-9764-2418
https://orcid.org/0000-0002-9764-2418
Availability of Data and Materials: Data can be available upon request from the corresponding author.
References
- 1. Guerrant R, Walker D, Weller P. Tropical Infectious Diseases: Principles, Pathogens and Practice. 2011:1-1130. [Google Scholar]
- 2. Niehaus MD, Moore SR, Patrick PD, et al. Early childhood diarrhea is associated with diminished cognitive function 4 to 7 years later in children in a northeast Brazilian shantytown. Am J Trop Med Hyg. 2002;66:590-593. [DOI] [PubMed] [Google Scholar]
- 3. Mbakaya BC, Lee PH, Lee RL. Hand hygiene intervention strategies to reduce diarrhoea and respiratory infections among schoolchildren in developing countries: a systematic review. Int J Environ Res Public Health. 2017;14:1-14. doi: 10.3390/ijerph14040371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Abdelsafi Gabbad S, Elawad MA. Prevalence of intestinal parasite infection in primary school children in Elengaz area. Acad Res Int. 2014;5(2):86-90. [Google Scholar]
- 5. Oliveira D, Ferreira FS, Atouguia J, et al. Infection by intestinal parasites, stunting and anemia in school-aged children from southern Angola. PLoS One. 2015;10:e0137327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McMichael C. Water, sanitation and hygiene (WASH) in schools in low-income countries: a review of evidence of impact. Int J Environ Res Public Health. 2019;16:1-21. doi: 10.3390/ijerph16030359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chard AN, Garn JV, Chang HH, Clasen T, Freeman MC. Impact of a school-based water, sanitation, and hygiene intervention on school absence, diarrhea, respiratory infection, and soil-transmitted helminths: results from the WASH HELPS cluster-randomized trial. J Glob Health. 2019;9:020402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wiedenmayer K, Msamba VS, Chilunda F, Kiologwe JC, Seni J. Impact of hand hygiene intervention: a comparative study in health care facilities in Dodoma region, Tanzania using WHO methodology. Antimicrob Resist Infect Control. 2020;9:80-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Khan S, Ashraf H, Iftikhar S, Baig-Ansari N. Impact of hand hygiene intervention on hand washing ability of school-aged children. J Family Med Prim Care. 2021;10:642-647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Staniford LJ, Schmidtke KA. A systematic review of hand-hygiene and environmental-disinfection interventions in settings with children. BMC Public Health. 2020;20:195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ghaffari M, Rakhshanderou S, Ramezankhani A, Noroozi M, Armoon B. Oral health education and promotion programmes: meta-analysis of 17-year intervention. Int J Dent Hyg. 2018;16:59-67. [DOI] [PubMed] [Google Scholar]
- 12. Swe KK, Soe AK, Aung SH, Soe HZ. Effectiveness of oral health education on 8- to 10-year-old school children in rural areas of the Magway Region, Myanmar. BMC Oral Health. 2021;21:2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shrestha A, Schindler C, Odermatt P, et al. Nutritional and health status of children 15 months after integrated school garden, nutrition, and water, sanitation and hygiene interventions: a cluster-randomised controlled trial in Nepal. BMC Public Health. 2020;20:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ismail SR, Radzi R, Megat Kamaruddin PS, et al. The effects of school-based hygiene intervention programme: systematic review and meta-analysis. Plos One. 2024;19(10):e0308390:1-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dreibelbis R, Kroeger A, Hossain K, et al. Behavior change without behavior change communication: nudging handwashing among primary school students in Bangladesh. Int J Environ Res Public Health. 2016;13. doi:10.3390/ijerph13010129:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Amudha K, Thulasingam M, Thomas B, et al. How does school based hand-washing promotion program affect the handwashing behavior of students at the urban slums in Puducherry, South India? Mixed method design. Int J Med Sci Public Health. 2018;7: 874-878. [Google Scholar]
- 17. Joshi A, Amadi C. Impact of water, sanitation, and hygiene interventions on improving health outcomes among school children. J Environ Public Health. 2013;1:984626:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Talaat M, Afifi S, Dueger E, et al. Effects of hand hygiene campaigns on incidence of laboratory-confirmed influenza and absenteeism in schoolchildren, Cairo, Egypt. Emerging Infectious Diseases. 2011;17(4):619-625. doi:10.3201/eid1704.101353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duijster D, Buxton H, Benzian H, et al. Impact of a school-based water, sanitation and hygiene programme on children’s independent handwashing and toothbrushing habits: a cluster-randomised trial. International journal of public health. 2020;65:1699-1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oxfam. Gender, WASH and Education Case Study. Enhancing girls’ participation in schools in Pakistan. https://oxfamilibrary.openrepository.com/bitstream/handle/10546/142170/cs-wash-girls-participation-pakistan-130911-en.pdf;jsessionid=6F2C4185201C0E6A0DCAD269E0F7A205?sequence=1
- 21. Pradhan NA, Haider F, Khudadad U, et al. Gaps in hygiene promotion at schools in Pakistan: qualitative descriptive research. Health Promot Int. 2023;38:1-12. doi: 10.1093/HEAPRO/DAAC046 [DOI] [PubMed] [Google Scholar]
- 22. Pradhan NA, Ali TS, Hasnani FB, Bhamani SS, Karmaliani R. Measuring socio-economic status of an urban squatter settlement in Pakistan using WAMI index. J Pak Med Assoc. 2018;68:709-714. [PubMed] [Google Scholar]
- 23.Boot MT, Cairncross S. (eds) (1993) Actions speak: The study of hygiene behaviour in water and sanitation projects. IRC International Water and Sanitation Centre and London School of Hygiene and Tropical Medicine. Accessed September 27, 2022. https://www.ircwash.org/sites/default/files/Boot-1993-Actions.pdf
- 24. Vivas AP, Gelaye B, Aboset N, et al. Knowledge, attitudes, and practices (KAP) of hygiene among school children in Angolela, Ethiopia. J Prev Med Hyg. 2010;51:73-79. [PMC free article] [PubMed] [Google Scholar]
- 25. Cirillo N, Duong PH, Er WT, et al. Are there betel quid mixtures less harmful than others? A scoping review of the association between different betel quid ingredients and the risk of oral submucous fibrosis. Biomolecules. 2022;12:664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Niaz K, Maqbool F, Khan F, et al. Smokeless tobacco (paan and gutkha) consumption, prevalence, and contribution to oral cancer. Epidemiol Health. 2017;39:e2017009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pradhan NA, Hashmani N, Ali T, et al. Behavioral change communication tool kit to promote hygiene among school children. 2023.
- 28. Grusec JE. Social learning theory and developmental psychology: the legacies of Robert sears and Albert bandura. Dev Psychol. 1992;28:776-786. [Google Scholar]
- 29. Ibrahim S, Sidani S. Intervention fidelity in interventions: an integrative literature review. Res Theory Nurs Pract. 2016;30:258-271. [DOI] [PubMed] [Google Scholar]
- 30. Schmidtke KA, Drinkwater KG. A cross-sectional survey assessing the influence of theoretically informed behavioural factors on hand hygiene across seven countries during the COVID-19 pandemic. BMC Public Health. 2021;21:1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Watson JA, Ensink JHJ, Ramos M, et al. Does targeting children with hygiene promotion messages work? The effect of handwashing promotion targeted at children, on diarrhoea, soil-transmitted helminth infections and behaviour change, in low- and middle-income countries. Trop Med Int Health. 2017;22:526-538. [DOI] [PubMed] [Google Scholar]
- 32. Younie S, Mitchell C, Bisson MJ, et al. Improving young children’s handwashing behaviour and understanding of germs: the impact of a germ’s journey educational resources in schools and public spaces. PLoS One. 2020;15:e0242134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Vasselli JR. The role of dietary components in leptin resistance. Adv Nutr. 2012;3:736-738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Malik VS, Popkin BM, Bray GA, Després JP, Hu FB. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;121:1356-1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Vozza I, Capasso F, Calcagnile F, et al. School-age dental screening: oral health and eating habits. Clin Ter. 2019;170:E36-E40. [DOI] [PubMed] [Google Scholar]
- 36. Bhat A, Ray T, Sahni J. Aural hygiene practices among underprivileged children of Delhi. Natl Med J India. 2015;28:280-281. [PubMed] [Google Scholar]
- 37. Eksteen S, Eikelboom RH, Kuper H, Launer S, Swanepoel W. Prevalence and characteristics of hearing and vision loss in preschool children from low income South African communities: results of a screening program of 10,390 children. BMC Pediatr. 2022;22:22-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Czechowicz JA, Messner AH, Alarcon-Matutti E, et al. Hearing impairment and poverty: the epidemiology of ear disease in Peruvian schoolchildren. Otolaryngol Head Neck Surg. 2010;142:272-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bukhari SM, Aslam S, Riaz N, et al. Management of cotton bud induced otitis externa by unique method. Pak Armed Forces Med J. 2021;71(Suppl-3):S448-S451. [Google Scholar]
- 40. Khan NB, Thaver S, Govender SM. Self-ear cleaning practices and the associated risk of ear injuries and ear-related symptoms in a group of university students. J Public Health Afr. 2017;8:149-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ahmed A, Gadanya M, Abubakar S, Maje A. Prevalence and attitude of self-ear cleaning with cotton bud among doctors at aminu kano teaching hospital, Northwestern Nigeria. Niger J Surg Res. 2016;17:43. [Google Scholar]
- 42. Alruwaili H, Dar U, Alshammari A, et al. Knowledge and practices regarding ear hygiene among Saudi adolescents. Int J Med Dev Ctries. 2021;224-228. doi: 10.24911/IJMDC.51-1606825984 [DOI] [Google Scholar]
- 43. Bhisitkul DM, Dunham M. An unsuspected alkaline battery foreign body presenting as malignant otitis externa. Pediatr Emerg Care. 1992;8:141-142. [DOI] [PubMed] [Google Scholar]
- 44. Olajide TG, Olajuyin OA, Eletta AP, et al. Self ear cleaning: prevalence and profile among school children in Ekiti, Nigeria. J Biosci Med. 2019;07:25-32. [Google Scholar]