Abstract
The deployment of Health Information Systems (HIS) in Sri Lanka has been low in adoption compared to developed countries. There has been a dearth of studies to identify the factors that improve the adoption of HIS in developing countries. Thus, this study investigates the factors influencing the acceptance of HIS among public healthcare staff. A survey was administered among 170 medical professionals, including nurses and doctors. Partial Least Squares Structural Equation Modelling (PLS-SEM) was applied to the dataset with 5000 bootstrap subsamples. The research model was developed based on the prior literature and by extending the Technology Acceptance Model (TAM) to the context of public healthcare. A positive relationship was observed between the actual use of HIS and constructs such as perceived usefulness, perceived ease of use, attitude, behavioural intention, prior use of HIS by supervisors, computer anxiety and facilitating conditions. These findings confirm the applicability of the proposed extended TAM in the public healthcare system of a developing country. Furthermore, HIS practitioners and policymakers in the healthcare sector would find these results valuable.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-024-12173-8.
Keywords: Technology acceptance model, Health information systems, Electronic medical records, Electronic health records, Attitude, Behaviour intention
Introduction
Health Information Systems (HIS) were introduced to support the administrative tasks performed by various healthcare stakeholders [1]. Technological advancements have led to the transformation of HIS into powerful Information Systems (IS) in different forms such as Electronic Medical Records (EMR), Personal Health Records (PHR) and Electronic Health Records (EHR), which serve as the lifeblood of modern healthcare ecosystems. In many developed nations like the Nordic countries, adoption of HIS hovers closer to 100% [2, 3].
The global average doctor-patient ratio is 17 per 1000 population [4]. However, being a developing country, Sri Lanka’s doctor-patient ratio is 1.23 physicians per 1000 [5]. Due to this healthcare practitioners, administrators and patients face various issues such as overcrowding, long waiting times for appointments with general practitioners, delays in receiving reports of blood samples, difficulty in managing drug inventories and other health check-ups [6]. To overcome these issues, the Sri Lankan health sector requires the support of a highly efficient HIS to provide uninterrupted health services to the 22 million population [5]. Recognising the transformative potential of HIS, developing countries, including Sri Lanka have embarked on ambitious digitisation initiatives.
The Sri Lankan government has spearheaded numerous projects implementing EMRs, HIS, District Nutrition Management Systems, Hospital Health Information Systems (HHIS) and other Information Systems (IS) in public healthcare and the government contributes 4.1% of the Gross Domestic Product (GDP) towards the health sector [4, 7]. In the early stage of the implementation at the Dompe District Hospital in Sri Lanka reported lack of knowledge of IS among the staff, attitude towards the technology and complexity of the health sector as the key challenges for digital transformation [6]. To transform the healthcare staff, the hospital management initiated various workshops, lecture sessions, competitions, productivity programmes and outbound training. Furthermore, the Government of Sri Lanka (GOSL) released its policy brief on the digital transformation of the health sector in 2022 and published the Sri Lanka Digital Blueprint in 2024 as a road map for digitalisation [8, 9]. Despite the efforts of the GOSL, a compressive HIS does not exist in the public health sector connecting all the government hospitals across the county [10].
The current study concentrated on addressing the acceptance of HIS by healthcare stakeholders using the Technology Acceptance Model (TAM) as a base model. TAM has been expanded by additional constructs that influence the acceptance among healthcare stakeholders in the Sri Lankan public health sector. In this regard, various models were developed to assess technology acceptance, but none were developed specifically for the health sector [11]. Furthermore, extended TAM to the health sector was not extensively applied to the public health sector [12–14]. Factors influencing technology acceptance among the public and private sectors differ for several reasons. First, the organisational structure of the public sector is more hierarchical and bureaucratic which potentially creates internal barriers to technology acceptance [15]. Second, the culture of the public sector is more towards a traditional approach [16]. However, the private sector tends to experiment to introduce new technology. Third, the resource availability in the public sector may be low due to limited financial resources or budgetary constraints. Fourth, employees in the public sector may encounter more internal and external barriers to technological adoption [17]. Therefore, the present study is focused on the factors influencing the acceptance of HIS in public sector hospitals.
The existing studies that applied TAM focused on a single group of stakeholders like doctors, nurses, administrators and patients and very limited studies on multiple user groups. Thus, this study is unique as it is concentrated on two primary user groups of the HIS. This analyses the complexity of the factors which influence technology acceptance among the user groups and could help the management in formulating strategies and expediting progress. Furthermore, Sri Lankan government hospitals are unique as they are built to provide free medical care to all citizens including births to surgeries. They are categorised into National Hospitals, Teaching Hospitals, Provincial General Hospitals, District General Hospitals, Base Hospitals, Divisional Hospitals, Primary Medical Care Units, Maternity Homes and Dispensaries [10]. Furthermore, the Base Hospitals and Divisional Hospitals are further divided into subcategories A and B. These categories indicate the uniqueness of the public health sector of Sri Lanka compared to other countries which demand a unique model to assess the acceptance. Furthermore, developing countries have proven that HIS has increased efficiency and productivity in the health sector [18]. Therefore, the current study aims to enhance the TAM by incorporating social and human dynamic variables to address the existing research gap.
TAM was taken as a foundation by the researchers for the present study to assess the acceptance of HIS in Sri Lanka for various reasons. First, it is a simple model with two constructs and offers flexibility to customise for healthcare [1]. Second, research studies demonstrate that TAM has higher predictive power [19]. Third, TAM highlights that user acceptance is a key success factor in technology acceptance [11]. Fourth, TAM has demonstrated its suitability to the Sri Lankan context [20]. Fifth, it has been a model widely used in the health sector to the acceptance of technology [21]. Finally, the model allows it to expand by incorporating additional constructs focused on contexts, technologies and populations [22].
The study aimed to answer the following research questions (RQs):
RQ1: What are the social and human dynamic factors that influence the acceptance of HIS in the Sri Lankan public healthcare sector?
RQ2: What is the applicability of extended TAM in the Sri Lankan public healthcare sector?
This study employed a rigorously validated survey instrument designed to evaluate HIS acceptance in the Sri Lankan public healthcare context. Data was collected from doctors and nurses of 170 HIS users, ensuring robust and generalisable findings. The data underwent rigorous analysis using Partial Least Squares Structural Equation Modelling (PLS-SEM), a technique well-suited for complex models. The findings of the research will be useful in (a) developing an enriched TAM for public healthcare in Sri Lanka; (b) unveiling the interplay of complex dynamics factors influencing HIS adoption; (c) evaluating the cause and effect of the factors affecting the actual use of HIS; (d) creating a policy-driven implementation for policymakers and healthcare administrators in Sri Lanka and (e) provides a framework for other developing countries for digital transformation in the health sector.
The first section of the study is a thorough literature analysis that carefully constructs the state of knowledge regarding TAM in the context of healthcare. This critical study highlights well-established discoveries while also pointing out important areas that need more research. The research design is described in the methodology section, along with the methods used for gathering data and the specific assumptions that informed the investigation. The results section, which presents the results and encourages further investigation through a thorough discussion of the findings, derives from hypothesis testing. The work concludes with a summary of the main conclusions and highlights the important contributions this research has made to the field.
Theoretical background
Overview
Davis [23, 24] introduced TAM to evaluate the individual user's acceptance of the technology. TAM is a straightforward model which has two constructs: Perceived Ease of Use (PEOU) and Perceived Usefulness (PU) [25]. TAM was formulated with mediating variables such as attitude and behaviour intention which ultimately predict the actual use of technology [26]. Since TAM focuses on a user-centric approach it is widely applied to analysing technology acceptance across different contexts including healthcare [11, 27]. Moreover, it offers insights into the determinants of technology acceptability by critically examining the users' subjective judgment [28]. The construct PU is known as the degree to which individuals believe technology can enhance job performance, on the other hand, PU is known as the fact that the technology will be free of effort [27]. This model assists developers in improving user interfaces and technologies by identifying the crucial elements that influence user acceptability of the technology. Holden [29] discovered that the TAM can predict up to 70% of the user’s intention to use technology in healthcare settings.
Predictive power of TAM
When predicting users' behaviour intention toward new technologies TAM has proven to be a reliable model [30]. For instance, TAM was demonstrated as a suitable theory to be considered in the healthcare sector [29]. A study carried out in Sri Lanka among healthcare practitioners [20] and a Jordanian study confirms the suitability of TAM in the healthcare sector [12] and it is important to note that it has been applied among different demographics [31]. Interestingly, another study on healthcare workers in Ethiopia found that the extended TAM accurately predicts 56.2% of behavioural intention [18]. Even though many studies have indicated the suitability of TAM in healthcare domains, several studies have indicated that the relationships may not be as significant as expected in some contexts. These findings may not be easily generalised to physicians, which shows the poor match purely due to differences in professional backgrounds [11, 12]. A study focused on physicians who had access to telemedicine in Hong Kong revealed that TAM was not a good fit for forecasting the patterns of technology adoption that the physicians had [29]. Even though studies highlight the predictive power of TAM [21], its applicability is limited in some contexts and among certain user groups. Consequently, it highlights the need to focus on diverse factors to assess the acceptance of technology among the different professions.
Social and human dynamics
Since TAM lacks social and human dynamics [21], several studies have been conducted extending the TAM in healthcare by incorporating additional constructs relating to the sector [29, 32] and based on the context [18, 33]. These extensions of TAM align with the Unified Theory of Acceptance and Use of Technology2 (UTAUT) models [34]. Researchers have considered constructs such as professional rank, price value [35], privacy, use resistance, anxiety, facilitating conditions [35, 36], experience [12, 18], support [33, 37], social influence [36, 38], computer skills [12], perceived risk [35, 36], managerial, organisational [32], strategic and technical infrastructure [18, 39] on the acceptance of technology in several studies. Since the HIS holds plenty of sensitive data, healthcare practitioners are highly concerned about data protection mechanisms. In the event of data leakage, re-gaining trust will be a huge challenge and the National Programme for Information Technology (NPfIT) is a good example where the practitioners resist changes due to data privacy and security issues [40]. Furthermore, experience in using HIS and computing skills are crucial, especially when the implementation takes place in rural areas may need extra attention. Thus, the level of IT experience among staff was not a significant construct in the study carried out on healthcare workers in Ethiopia [18] which underscores the importance of context-specific constructs in the extended TAM.
Organisational factors
The leadership commitment of higher management in digital transformation is a critical factor as it can influence the culture, motivation and attitude towards the technology adoption of the employees. Moreover, decisions on budget and resource allocation promote a favourable approach towards digitalisation within the institutions. For instance, a study on the application of Artificial Intelligence (AI) in the government healthcare sector in the United Arab Emirates (UAE) tested an extended TAM model that incorporates aspects such as managerial, operational, strategic, and IT infrastructure [39]. Introducing a system can affect the organisation’s existing workflow. It requires a careful assessment to redefine the workflow to ensure seamless integration of the HIS into daily operations. This highlights that organisational support in digital transformation contributes to several factors including facilitating training, workshops, resource allocation, workflow management and motivation [18, 32, 37, 38].
Usability
In HIS, technical problems have been focused extensively [41]. However, universally highlighted that usability issues limit the usage and implementation in healthcare [42, 43]. An assessment of EHR in three children’s hospitals in the United States (US) captured 36% of the issues from usability [43]. Due to the complex work nature of the health sector, the systems are expected to be designed in a user-friendly manner. This has been examined in several studies as in PEOU which echoes TAM [35] and system quality [44]. Due to the diverse age groups, and professional ranks among the healthcare practitioners, these HIS should allow a non-technical user to learn quickly by reducing complexity. In addition, the systems are expected to respond quickly and provide easy access to patient records securely [13].
Table 1 summarises the existing assessment of TAM and Extended TAM. Considering many positive findings related to TAM and its suitability to the Sri Lankan context, it was decided to use TAM as the base model to extend.
Table 1.
Summary of the application of TAM and extended TAM
| Focus | Population | Country | Results | Source |
|---|---|---|---|---|
| Acceptance of Telemedicine | 408 Physicians | Hong Kong | TAM is a Poor Fit for Physicians | [29] |
| Application of TAM for Electronic Health Records | 1539 Nurses | Jordan | Perceived Usefulness and Perceived Ease of Use | [12] |
| Implementation of AI in the Health Sector | 53 Health Sector Staff | United Arab Emirates | Perceived Usefulness, Perceived Ease of Use, Managerial, Operational, Organisational, IT infrastructure and Strategic | [39] |
| Adoption of eHealth Systems | 384 Healthcare Professionals | Ethiopia | Perceived Usefulness, Perceived Ease of Use, Technical Infrastructure and Staff IT Experience | [18] |
| Acceptance of Telemedicine Services | 226 Participants from Rural Area | Pakistan | Perceived Usefulness, Perceived Ease of Use, Trust, Social Influence, Facilitating Conditions, Technological Anxiety, Use Resistance, Perceived Risk and Privacy | [36] |
| Acceptance model for Telemedicine services | Telemedicine users aged above 18, 248 Participants | Turkey | Perceived Usefulness, Perceived Ease of Use, Self-efficacy, Trust, Price Value, Technology Anxiety, Facilitating Conditions, Use Resistance and Perceived Risk | [35] |
| Technology Acceptance of Personal Health Records | 389 Patients | Saudi Arabia | Perceived Usefulness, Perceived Ease of Use, Privacy, Usability and Security | [13] |
| Acceptance model of a Hospital Information System | 1983 Low-level and Mid-level Hospital Management Officers, Doctors, Nurses, and Administrative Staff | Indonesia | Perceived Usefulness, Perceived Ease of Use, Compatibility, Information Security, User Self Efficacy, Social Influence, Information Quality, System Quality, Management Support, Facilitating Conditions and User Involvement on HIS Implementation | [38] |
| Acceptance of Health Information System for Public Health Centre | 37 HIS users of the Public Health Center | Indonesia | Perceived Usefulness, Perceived Ease of Use, Job Relevance, Output Quality, Results Demonstrability, Screen Design, Terminology and Facilitating Conditions | [45] |
|
Customer Loyalty toward Mobile Wallet Services in Post-COVID-19 |
243 Customers | India | Perceived Usefulness, Perceived Ease of Use, Service Quality, Trust, Privacy and Security | [46] |
| Adoption of Social Commerce | 218 Users | Jordan | Perceived Usefulness, Security Concerns, Top Management Support, Organisational Readiness, Consumer Pressure and Trading Partner Pressure | [32] |
| Academics Toward Technology Acceptance in Accounting Education | 138 Academics | Yemen | Perceived Usefulness, Perceived Ease of Use, Social Influence and Self Efficiency | [24] |
| Intention to Continue Digital Accounting Systems | 308 Staff of Small and Medium Enterprises | Yemen | Perceived Usefulness, Perceived Ease of Use, System Quality, Information Quality, Satisfaction and Confirmation | [44] |
| Adoption of Block Chain Technology in Accounting Education | 191 Faculty Members | India | Perceived Usefulness, Perceived Ease of Use, and Organisational Support | [37] |
| Behaviour Intention to Use an E-pharmacy Service | 480 Clients | South Africa | Perceived Usefulness, Perceived Trust, Social Influence, Performance Expectancy and Technological Literacy | [30] |
| Acceptance of IOT based Healthcare | 257 Users | Jordan | Perceived Usefulness, Perceived Ease of Use, Individual Task Fit, Individual Task Technology Fit, Social Influence, Security and Privacy | [28] |
| Adoption of Smart Health Services | 1292 Retired Personnel | China | Perceived Usefulness, Perceived Ease of Use, Health Expectation, Technology Trust, Security Trust, Privacy Trust, Family Support, Community Support and Service Support | [33] |
| Telemedicine Adoption among the Physicians | 230 Physicians | Malaysia | Perceived Usefulness, Perceived Ease of Use, Reward, Sanction, Image, Information Influences, Self-Efficacy, Ability of the Patients and Accessibility of Records | [21] |
| Acceptance of OVO Application in the F&B industry in Indonesia | 400 Users | Indonesia | Perceived Usefulness, Perceived Ease of Use and Generation | [23] |
| Evolution of TAM AI in E-commerce | 220 Purchasers | Pakistan | Perceived Usefulness, Perceived Ease of Use, Subjective Norm, Trust | [47] |
Research model
Hypothesis development
PU is known as an individual’s perception that using technology can increase job performance [48, 49]. This construct has been reflected in various models including UTAUT2 [22, 27]. PU has been a strong predictor of behaviour intention across various contexts including voluntary and mandatory as it has played a pivotal role in technology acceptance [50]. However, the UTAUT model is formulated with age and gender to moderate the performance expectancy. Thus, UTAUT2 shows that it can directly impact the behaviour intention without the moderators [22]. This highlights that it is important to understand the complex character of PU. A research study on healthcare further highlights the complexity as it suggests convenience, outcome and time as moderators for performance expectancy [51]. The PU of technology is a dynamic construct. However, it can be influenced by specific contexts and individual needs. A closer look at the Indonesian study PU has been a mediator in technology acceptance in healthcare [45]. It is vital to recognise the crucial role of PU in the acceptance of technology use. Furthermore, in the health setup, the practitioners are keen to have a HIS which could benefit them in managing the patient. Therefore, PU can significantly impact patient care and staff work efficiency.
H1: Perceived Usefulness has a significant positive effect on healthcare staff’s attitude.
H2: Perceived usefulness has a significant positive effect on healthcare staff’s Behaviour Intention to Use.
PEOU is known that using technology will be free of effort [48, 50]. The construct of PEOU appeared in various models from TAM to UTAUT2 [27]. This concept demonstrates that users are more likely to use technology as it is simple and reduces the workload [1]. However, a closer examination reveals that the PEOU is not only about simplicity [52]. The models including TAM, UTAUT and Innovation Diffusion Theory (IDT) identify its importance and impact on technology use. Similar to PU, UTAUT is incorporated by variables like age and gender as moderators. Thus, UTAUT2 highlights effort expectancy directly influences behaviour intention [22]. This highlights the importance of understanding effort expectancy or PEOU.
The Bangladesh study on healthcare identifies that poor user interfaces can lower the influence of effort expectancy. User interfaces are a key factor which reduces engagement in any sector, therefore, researchers recommend the importance of developing a good user interface to address the concern [31]. Another study on mHealth applications in China identifies that ease of learning and use can play a moderating role and highlights the importance of understanding user preferences and learning styles [34]. Since the health sector consists of diverse groups of users, the HIS should not increase the complexity. Therefore, to effectively leverage effort expectancy for successful technology adoption the hypothesis was formulated.
H3: Perceived Ease of Use has a significant positive effect on healthcare staff’s Attitudes.
H4: Perceived Ease of Use has a significant positive impact on Perceived Usefulness.
Attitude can be known as an individual’s target behaviour for using the technology [27, 53]. The definition of attitude captures its emotional aspect but overlooks its multi-faceted nature. Regarding technology use, attitude encompasses not only the affective (feelings) but also the cognitive (beliefs) and behavioural (tendencies) components. Individuals form an overall evaluative judgment about interacting with a system influenced by the perceived usefulness, complexity and alignment with the values. While attitude undeniably plays a crucial role in shaping behavioural intention, its influence is not confined to a simple linear path. Empirical findings suggest it can act as a mediator [52], bridging the gap between intention and actual use [31]. As observed positive attitudes towards a system can mediate the relationship between behaviour intention and actual use implying that even strong intentions may not translate into action without favourable emotional responses.
Furthermore, attitude can be influenced by various other internal and external factors. During the digital transformation process, the attitude of the users might resist the change. Therefore, healthcare administrators must play a pivotal role in shaping the attitude of the practitioners.
H5: Healthcare staff’s attitude has a significant positive impact on Behaviour Intention to Use.
H6: Healthcare staff’s Behavioural Intention to use has a significant positive impact on Actual Use.
Prior use of the HIS use by the Supervisor can be known as previous experience and familiarity of supervisors with similar technology [54]. Within any organisation, the pecking order plays a significant role in shaping employee behaviour. This fact is of utmost momentousness when it comes to the adoption of new technologies like HIS. Supervisor, by their position, can significantly impact subordinates' willingness and perception of new systems. If the unit head feels negative about HIS based on past experience, that could impact all the team members’ attitudes. Let's delve deeper into the mechanisms of this influence, where the supervisor wields the power of reward and punishment [54]. Praising can inspire adoption, while disapproval can dampen enthusiasm. Studies show that positive reinforcement, like highlighting the system's benefits positively influences HIS use among staff. This is consistent with Kelman's theory of social influence, particularly the notion of compliance. Individuals are more inclined to comply with using the system for prospective benefits when users feel pressured, regardless of the intrinsic drive [54]. Beyond overt sanctions, supervisor can subtly influence the subordinates' perceptions of the HIS. The user's actions and attitudes towards the system send powerful signals. If the users readily embrace the technology and showcase its advantages, users can instil positive beliefs and encourage adoption [55].
As described by Kelman, this process involves individuals assimilating the perceived value of the system based on the supervisor' behaviour. While the influence of supervisor is undeniable, social dynamics extend beyond the direct chain of command. Peers can also shape attitudes through shared experiences and discussions, while external influences like media coverage and broader professional networks can further moderate the overall HIS adoption [54]. By recognising the multifaceted nature of social influence and actively leveraging its power within the healthcare hierarchy, organisations can significantly boost the adoption and success of HIS, ultimately improving patient care and staff efficiency [34].
H7: Prior HIS use by the Supervisors has a significant positive impact on healthcare staff’s Attitude.
Computer anxiety is defined as a feeling of distress experienced when interacting with technology [56, 57]. Higher levels of computer anxiety directly translate to lower actual use of new systems. The fear of encountering technical difficulties, making mistakes, or appearing incompetent acts as a powerful deterrent, preventing individuals from engaging with technology that could significantly benefit them [56]. Computer anxiety can be contagious, so it is necessary to understand the root cause. This can be due to insufficient computer skills, fear of technology use, privacy concerns and language barriers. The management should facilitate the staff by providing adequate training and implementing security protocols in HIS. The apprehension felt by individuals with high anxiety can spread like a ripple effect, influencing colleagues, friends and even family members to resist using the technology. This social contagion can significantly hamper the diffusion of innovative systems, especially among close subordinates [56]. It fosters a resistance to technology, diminishing individuals' openness to trying new tools and platforms. This resistance becomes a self-fulfilling prophecy, leading to missed opportunities for personal and professional growth [35]. The avoidance triggered by computer anxiety can impact the attitude and non-use of the system over time. Furthermore, individuals consistently avoid technology due to anxiety and become accustomed to relying on alternatives [58]. Therefore, addressing computer anxiety is crucial for ensuring successful technology adoption across all demographics.
H8: Computer Anxiety has a significant negative impact on the healthcare staff’s Attitude.
Facilitating conditions refer to the degree to which a person trusts that an organisational and technical infrastructure will support to use of the system [48, 59]. User interfaces and features of the systems have been discussed extensively, yet facilitating conditions are an important factor in technology acceptance [60, 61]. It refers to the perceived availability of organisational and technical support that allows the smooth use of an IS [18, 27]. Exploring this construct in UTAUT models reveals its complex and deep impact on attitude. Moreover, it highlights the importance of organisational factors like infrastructure, technical support and leadership, alongside individual perceptions of control and system alignment with existing workflow [27]. The supportive infrastructure of organisations is the key factor in technology adoption. Due to the complex workflow of the health sector, other technical resources must support the daily operations. The facilitating conditions are not limited to the technical infrastructure, it demands training and technical support as well. In the event of a hardware or software failure, immediate attention by a dedicated support team is essential to run the operations smoothly. Thus, the study on older adults highlighted that facilitating conditions did not have an impact [31]. Conversely, a telemedicine study in Bangladesh paints a different picture. Here, facilitating conditions emerged as a key driver of technology adoption among healthcare staff [62]. This disparity highlights the crucial role of tailoring support and resources to the specific needs of different user group’s workflow [52, 63].
In healthcare settings, facilitating conditions hold immense potential [10]. Imagine healthcare staff equipped with user-friendly devices, readily available technical support and training tailored to specific tasks. This creates an environment where staff feel empowered and confident to embrace HIS, ultimately improving patient care and healthcare delivery. Recognising context-specific nuances and crafting targeted support strategies to address the unique needs of diverse user groups is key to unlocking the full potential of any new technology, especially within healthcare settings.
H9: Facilitating Conditions have a significant positive impact on the healthcare staff’s Attitude.
Technological advancement demands the necessity of acquiring new skills and development [64]. The profession is not just a sole factor, it includes the educational background, skills, language fluency, decision-making capacity, generation and many more. Healthcare professionals at different levels in the organisational hierarchy may have different behavioural intentions towards the use of the HIS. For example, a healthcare professional belonging to Generation Z can adopt new technologies quickly [65]. In contrast, in Generation X, the senior roles like physicians and matrons may accept the HIS with caution.
H10: The influence of attitude on Behaviour Intention will be moderated by the Profession Type.
H11: The influence of Behaviour Intention on Actual Use will be moderated by Profession Type.
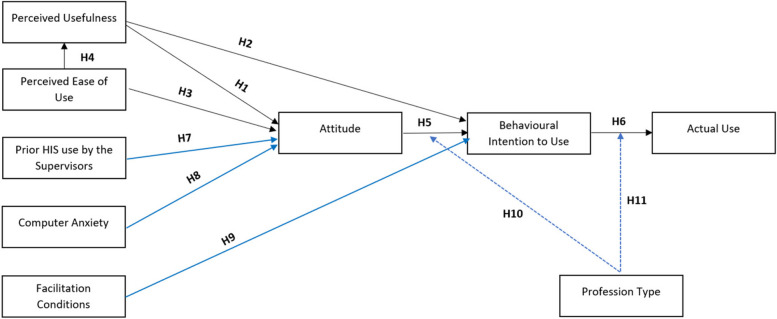
Figure 1 indicates the proposed research model of the study.
Fig. 1.
Research model (Note: blue lines indicate the newly introduced constructs and their relationships)
Control variable
In addition to the theoretical constructs, government policy can be considered a control variable. Government policy is known as the direction of citizens’ product use [31]. The adoption of new technologies in healthcare depends on the unseen hand of government policy which often plays a crucial role. These policies set clear direction and guidance for the use of products and organisations to shape internal policies and individual views on healthcare technologies like HIS. The government generally develops the legal framework for technology based on the guidelines, regulations and laws approved by a select committee. For example, when the government of Hong Kong mandated the use of EHR which resulted in increased acceptance among healthcare organisations [31]. Moreover, government policies have the characteristic to influence the attitude and perception toward using technology. Awareness programs on using HIS or other health technologies by government agencies will build strong trust in the technology among the citizens. When the government imposes high privacy policies or if concerns are raised about cybersecurity, it can change the view of health technology as it indicates the risks. So, government policies should have a balance of control of the technology and foster innovation.
The extensive regulations can limit innovation and disrupt the progress of the transformation process of digital technologies. However, too much freedom or uncontrolled processes can lead to breaches of data security and privacy on patients’ data. Identifying the optimal point is important through a comprehensive analysis of the potential benefits and risks associated with health technologies. Policymakers must develop strategies by understanding the effects of government policies on the actual use of health technologies as it will bring benefits to the sector. At the same time, it is essential to understand that the policies can impact the future of the health sector by giving adequate space for emerging new technologies [31]. Furthermore, a study on the adoption of E-learning systems in Sri Lanka emphasised the inadequacy of government policies at the IS [66].
Sampling and data collection
The study's sample consisted of doctors and nurses from two teaching hospitals located in the Western Province of Sri Lanka. The teaching hospitals offer a comprehensive range of services, supported by additional resources to enhance efficiency. Additionally, the teaching hospitals deal with any type of disease and the medical records of the patients are collected from various units including laboratories to the respective wards. At present, all hospital units and wards are not occupied by the HIS [10]. Thus, purposive sampling was utilised [47], with a criterion that participants had at least one year of expertise in HIS, in line with a previous study sampling method conducted in Indonesia and the UAE on TAM [23, 39].
The study focused on the quantitative approach; therefore, the researchers developed a self-administered questionnaire designed based on the TAM and UTAUT2 [22] and each of the questions was measured using a seven-point Likert scale. The data collection was carried out using a tablet via Google Forms and the criteria imposed by the researchers, the participants for the study were carefully questioned on their experience in using the HIS before filling out the questionnaire. Furthermore, the data collection was carried out in two teaching hospitals after the approval of the hospital directors and ethical review committees respectively. To mitigate the bias the researchers collected the data across the hierarchy among the doctors (House Officers, Relief House Officers, Registrar, Senior Registrar and Consultant) and nurses (Nursing Officer, Sister and Matron). This allowed us to collect data from different age groups, educational backgrounds, and gender and designations.
As per the rules of thumb, the sample size of 90 is adequate since the research model consists of nine variables and the statistical method (Eq. 1) highlights 96 as the minimum required sample size [67]. However, the researchers increased the sample size to 170 with the imposed criteria of a minimum of one year of experience in using HIS.
| 1 |
Where n is the number of samples, z is the confidence level, p is the estimated proportion, and e is the margin of error.
Data was collected from both teaching hospitals equally and out of 170 participants, 59.4% are doctors and 40.6% are nurses. 77.6% were female and 22.4% were male among the participants. Since the nursing staff is dominated by females, the variation represents the actual gender diversity in the healthcare sector. 54.7% of the participants had a bachelor’s degree as the highest educational qualification and 38.8% of the participants were aged between 21–30 years.
Data analysis
The analysed data demonstrates the significant relationship between the variables. PLS-SEM with 5000 bootstrap samples in SmartPLS4 for utilisation as the tool for performing the analysis. This tool was chosen for various reasons. First, PLS-SEM accurately evaluates the complex correlation between the variables [35]. Second, it can produce an accurate statistical result regardless of the sample size [30, 68]. Third, the incorporation of 5000 bootstrap subsamples improves the accuracy of standard error estimates and confidence intervals, which will enhance the validation and reliability of the results [69]. Fourth, SmartPLS allows visualisation and generation of complex models with several latent variables [30, 70]. Fifth, the inner and outer models can be assessed with minimum effort [45].
The factor loading results reveal that the value of the ATT2 indicator is below 0.7, which is considered to be the minimum acceptable value [69]. It is important to mention that the ATT2 was considered due to its value of 0.689 as it is closer to 0.7. Furthermore, Table 2 displays the outcomes of the validity and reliability tests and Table 3 demonstrates the outcomes of the hypothesis testing results. The fact that both the AVE and Cronbach Alpha are above the thresholds of 0.5 and 0.7, respectively indicates the reliability of the data.
Table 2.
Outer loading test results
| Variable | Indicator | λ | AVE | α | rho_c |
|---|---|---|---|---|---|
| Perceived Usefulness | PU1: I find the HIS useful for my daily work | 0.915 | 0.850 | 0.941 | 0.942 |
| PU2: Using HIS increases my chances of achieving work that is important to me | 0.907 | ||||
| PU3: Using HIS helps me to accomplish things more quickly | 0.940 | ||||
| PU4: Using a HIS increases my productivity | 0.926 | ||||
| Perceived Ease of Use | PEOU1: Learning how to use a HIS is easy for me | 0.919 | 0.853 | 0.942 | 0.945 |
| PEOU2: My interaction with the HIS is clear and understandable | 0.895 | ||||
| PEOU3: I find the HIS easy to use | 0.950 | ||||
| PEOU4: It is easy for me to become skilful at using HIS | 0.930 | ||||
| Attitude | ATT1: The use of a HIS has become a habit for me | 0.841 | 0.641 | 0.813 | 0.833 |
| ATT2: I am addicted to using the HIS | 0.689 | ||||
| ATT3: I must use a HIS | 0.762 | ||||
| ATT4: Using a HIS has become natural to me | 0.895 | ||||
| Behaviour Intention to Use | BI1: I intend to continue using HIS in the future | 0.932 | 0.897 | 0.943 | 0.943 |
| BI2: I will always try to use HIS in my daily professional life | 0.954 | ||||
| BI3: I plan to continue to use the HIS frequently | 0.956 | ||||
| Actual Use | AU1: I consistently incorporate the HIS into the workflow | 0.915 | 0.875 | 0.928 | 0.930 |
| AU2: I regularly use HIS in my daily professional life | 0.943 | ||||
| AU3: I frequently use the HIS | 0.947 | ||||
| Prior HIS use by the Supervisors | PUS1: My supervisor uses the HIS to achieve daily tasks | 0.906 | 0.874 | 0.928 | 0.937 |
| PUS2: I got sufficient support and guidance from my supervisor to use the HIS | 0.958 | ||||
| PUS3: My supervisor will be available for assistance with system difficulty in using the HIS | 0.940 | ||||
| Computer Anxiety | CA1: I feel anxious about using the HIS | 0.883 | 0.794 | 0.915 | 0.953 |
| CA2: It scares me to think that I could lose a lot of information using the HIS by hitting the wrong key/button | 0.898 | ||||
| CA3: I hesitate to use the HIS for fear of making mistakes I cannot correct | 0.926 | ||||
| CA4: The HIS is somewhat scary to me | 0.855 | ||||
| Facilitating Conditions | FC1: I have the resources necessary to use the HIS | 0.742 | 0.670 | 0.837 | 0.867 |
| FC2: I have the necessary knowledge to use the HIS | 0.855 | ||||
| FC3: HIS is compatible with other technologies I use | 0.798 | ||||
| FC4: I can get help from others when I have difficulties using the HIS | 0.872 |
λ Factor Loading, α Cronbach’s Alpha, rho_c Composite Reliability
Table 3.
Hypothesis test results
| Hypothesis | T-Statistics | Path coefficient |
|---|---|---|
| H1 | 2.205 | 0.213* |
| H2 | 6.643 | 0.426*** |
| H3 | 2.968 | 0.339** |
| H4 | 16.221 | 0.745*** |
| H5 | 3.285 | 0.252*** |
| H6 | 53.271 | 1.002*** |
| H7 | 4.776 | 0.311*** |
| H8 | 3.793 | 0.226*** |
| H9 | 3.376 | 0.225** |
| H10 | 0.963 | (−0.163) |
| H11 | 1.447 | (−0.037) |
N=170, *p<0.05, **p<0.01, ***p<0.001 (2 tailed), t > 1.96 significant at 0.5
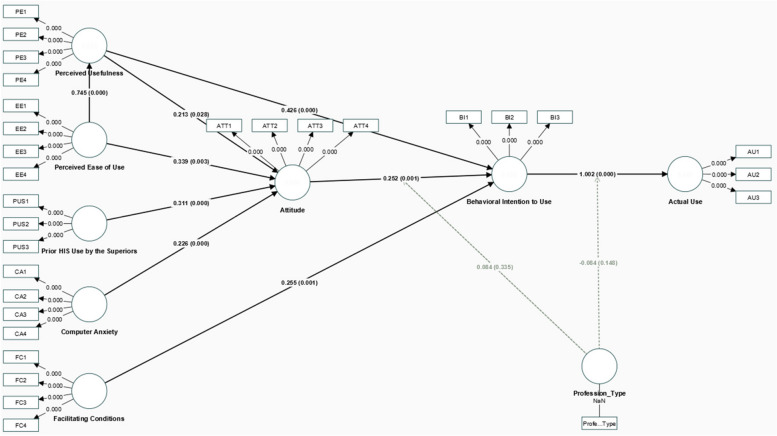
Figure 2 indicates the results of the formulated hypothesis of the extended TAM.
Fig. 2.
SEM model and results
As predicted by H1, PU emerged as a significant driver of positive attitudes towards HIS (coefficient = 0.213, p < 0.05). Similarly, H2 was supported, revealing a strong link between PU and the behaviour intention to actual use HIS (coefficient = 0.441, p < 0.001). PEOU, as expected in H3, also demonstrated a positive and significant relationship with attitude (coefficient = 0.339, p < 0.01). Interestingly, H4 revealed a strong positive correlation between PEOU and PU (coefficient = 0.745, p < 0.001), suggesting that user-friendly systems foster the perception of value. These results reinforce the applicability of TAM within the healthcare context.
The positive influence of attitude and behaviour intention to use (coefficient = 0.254, p < 0.001) confirms H5. This further translates into actual HIS use, as supported by H6 (coefficient = 0.969, p < 0.001). These findings highlight the crucial role of positive attitudes in bridging the gap between behaviour intention and actual use when it comes to HIS adoption.
This study also explored the impact of internal factors. H7 established a positive link between supervisors' prior HIS use and the attitude of healthcare staff (coefficient = 0.331, p < 0.001), suggesting that supervisors' familiarity with technology can positively influence the teams' perceptions. Similarly, H8 found that computer anxiety has a significant positive relationship with attitude (coefficient = 0.226, p < 0.001), implying that addressing anxiety surrounding technology could be beneficial for promoting positive attitudes towards HIS. Additionally, H9 confirmed a positive influence of facilitating conditions (coefficient = 0.243, p < 0.01), emphasising the importance of providing adequate resources and support for successful HIS implementation.
The results did not confirm the moderating effect of profession type on the relationships between attitude and behaviour intention; and behaviour intention and actual use, as indicated by path coefficient values of (−0.163) and (−0.037). The study demonstrates that the H10 and H11 are not supported and suggests that professional differences do not affect the behavioural intention and actual use of the HIS.
Discussion
The study presents significant findings. First, the findings strongly support the applicability of the extended TAM in explaining the acceptance of HIS by healthcare professionals. Hypothesis H1 to H9 constructs linked to technology adoption demonstrated a strong impact on the actual use of the HIS among doctors and nurses. The positive relationship between (H1) PU and Attitude and (H2) PU and Behaviour Intention explain that the healthcare practitioners anticipate the HIS to have useful functionalities which could result in reducing the workload in healthcare setup similar to the other studies [24, 37]. The positive relationship between (H3) PEOU and Attitude H4 PEOU and PU plays a crucial role and highlights the importance of a user-friendly system. If the system is complex with the day-to-day workflow, even though it has useful functionalities, it can frustrate the users and create a negative attitude [33, 36]. These findings align with the TAM and UTAUT2 and show that HIS not only be useful but also easy to use [22].
The positive relationship between (H5) Attitude and Behaviour Intention and (H6) Behaviour Intention and Actual Use are crucial in technology acceptance. A negative attitude toward using the HIS can change the behaviour intention and actual use which captures the interconnectivity of the constructs [28]. The positive relationship between (H7) Prior HIS use by the supervisor and attitude is interesting. If the head of the unit has had a bad experience in HIS, it can spread to the team which is headed. Furthermore, positional power and hierarchical structure can influence the team’s technology acceptance. This aligns with the importance of social influence in technology acceptance. Thus, this result underlines more specifics about the immediate supervisor’s influence on HIS acceptance [54, 55].
The positive relationship between (H8) Computer Anxiety and Attitude highlights the critical barrier to technology use. The HIS users who are afraid of using the system will negatively affect the implementation process. Furthermore, due to collaborative work nature, it can negatively impact the subordinate’s attitude. It highlights understanding the root cause of computer anxiety could help to develop effective strategies to transform those users [36]. The positive relationship between (H9) Facilitating Conditions and Behaviour Intention highlights the need for all required resources including technical infrastructure, training and support [22, 38, 45]. In the case of low resource set-up, it will complicate the routine tasks and impact the patients negatively. This aligns with the theory of UTAUT2 [22] and shows a direction for the policymakers and the management to develop a comprehensive action plan to ensure the resource requirements.
Second, additional constructs added to TAM are specifically relevant to the healthcare context. These newly included constructs, such as prior HIS use by the supervisors, computer anxiety and facilitating conditions were discovered to exert a substantial impact on the adoption of HIS. This demonstrates the importance of customising TAM to specific contexts and expands the model's generalisability. Third, the results of this study mandate that the professional difference between the doctors and nurses does not moderate the behaviour intention and actual use of HIS. Thus, the research highlights the role of the profession in implementing a new technology [64], H10 and H11 the moderating effect of Profession Type with Attitude, Behaviour Intention and Actual Use of HIS was not supported in this study. It highlights that both the user group’s attitude and behaviour intention to use the system do not have any differences. This allows the management of the hospitals to develop a common strategy to accelerate the HIS implementation. Fourth, the government policy on the use of HIS in the healthcare sector in Sri Lanka can control all the variables. The finding indicates that policies have the potential to indirectly impact the uptake of technology by altering individuals' attitudes and providing direction to use HIS [33]. This underscores the need for additional investigation to comprehend the intricate interaction of policy, individual variables and the acceptance of healthcare technology. Fifth, it confirms the soundness of the extended TAM constructs and showcases the substantial impact on the practical utilisation of HIS. Based on the findings, it is evident that the proposed model can be implemented in the public healthcare sector in Sri Lanka.
The study’s findings hold important theoretical and practical implications. Theoretical implications are; (a) The proposed research model offers a valuable framework for investigating HIS adoption in diverse healthcare sectors for a developing country. (b) Its focus on variables specific to the healthcare domain such as government policy can guide future studies on adoption barriers and facilitators in different regions or medical specialties. (c) The findings increased the predictive power of TAM specifically to the healthcare setup. (d) The additional constructs of computer anxiety and prior HIS use by the supervisors incorporated into the model emphasise that the social and human dynamics will significantly influence the acceptance of HIS. (e) The model underscores that the TAM should be tailored to the country, population and context.
Practical implications are as follows; (a) the study's insights into the factors influencing HIS usage can inform strategies to maximise acceptance among healthcare practitioners. Addressing identified concerns around computer anxiety can help to increase the skills and acceptance of HIS. (b) The findings underscore the importance of providing adequate computing resources, technical support and access to training materials to ensure the successful integration of HIS into daily workflows. (c) Perceived Ease of Use emphasises that user-centric design would accelerate the acceptance of HIS and provides a direction for the developers to focus on user-friendly interfaces. (d) The government policy is a control variable that highlights the need for data protection acts and provides a direction for digital transformation. (e) The findings guide the hospital management in establishing strong communication with the unit heads to facilitate the implementation.
Conclusion
The adoption of HIS has almost reached 100% in the Nordic countries. Consequently, developing countries like Sri Lanka, have yet to connect all the public hospitals with the HIS. Several studies utilising TAM have been conducted to identify the factors influencing the acceptance of HIS among healthcare professionals. The present study aimed to explore the factors influencing Sri Lankan healthcare professionals and demonstrate a statistically significant positive relationship between various variables, including (a) Perceived Usefulness and Attitude, (b) Perceived Usefulness and Behavioural Intention, (c) Perceived Ease of Use and Perceived Usefulness, (d) Attitude and Behavioural Intention, (e) Behavioural Intention and Actual Use, (f) Prior Use of HIS by the Supervisor and Attitude, (g) Computer Anxiety and Attitude and (h) Facilitating Conditions and Behavioural Intention. Furthermore, the study highlights that the two user groups such as doctors' and nurses’ professional differences do not moderate the Behavioural Intention and Actual Use. Moreover, the study underscores the applicability of TAM and the suggested research model will guide policymakers, hospital directors and practitioners to streamline the process of adopting new technologies including HIS in the public health sector.
Limitations and future research
Although the study provides useful insights into the acceptance of HIS in Sri Lanka's Western Province, caution is required due to limitations in generalisability. First, limiting the analysis to only two public teaching hospitals hinders the generalisation of findings to healthcare settings that have different types of hospitals. This may not be impactful, since the government trials the new HIS with the teaching hospitals before expanding it to other hospital categories in the public sector. Also, the doctors complete the final year of study in the teaching hospitals and all the teaching hospitals offer the same services. Second, disregarding other personnel in the hospital such as technicians and administrators fails to acknowledge the vital functions and perspectives within the HIS ecosystem, potentially leading to an underestimation of the overall adoption trends. Thus, doctors and nurses are the primary users of HIS at present. Thus, limitations emphasise the necessity for additional research that includes a wide range of healthcare stakeholders to achieve a more comprehensive understanding of HIS acceptance in the public health sector. Several improvements and extensions can be made in future. First, future research should build upon these findings by incorporating organisational culture into the model to understand how those variables influence HIS adoption. Second, examining policy-related variables in greater detail. Third, expanding the study to include participants from diverse hospital units which occupy HIS. Fourth, assessing the factors in the rural area hospitals will offer a more understanding of factors influencing HIS adoption.
Supplementary Information
Acknowledgements
The authors are grateful to the hospital directors and ethical review committees of the university and the teaching hospitals for allowing us to conduct the research. Also, it is important to thank the doctors and nurses who spared their valuable time in participating in the research despite the workload they had.
Data collection instrument
The questionnaire was developed based on UTAUT2 and TAM existing surveys. However, questions were modified to relate to the Sri Lankan health sector. (Please click the below PDF to view).
Authors’ contributions
Thiviyan Senthilrajah and Supunmali Ahangama were involved in the ideation, design, analysis, and interpretation of the results. Thiviyan collected the data from the hospitals by conducting the survey. Both authors were involved in writing the manuscript and reviewing it. Supunmai supervised the project.
Funding
The research was not funded by any agencies or funding bodies.
Data availability
The questionnaire was developed based on UTAUT2 and TAM existing surveys. However, questions were modified to relate to the Sri Lankan health sector. It is uploaded as a supplementary file.
Declarations
Ethics approval and consent to participate
The research was carried out after the university and the two teaching hospitals' ethics review committee approvals (Ethics Review Committee of Colombo South Teaching Hospital, Dehiwala, Sri Lanka and Ethics Review Committee of Sri Jayewardenepura General Hospital, Thalpitiya, Sri Lanka). All the participants declared their consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pai FY, Huang KI. Applying the Technology Acceptance Model to the Introduction of Healthcare Information. Technological Forecasting & Social Change. 2011;78(4):650–60. [Google Scholar]
- 2.Haux R. Health Information Systems - Past, Present, Future. International Journal of Medical Informatics. 2006;75:268–81. [DOI] [PubMed] [Google Scholar]
- 3.Pitkänen J, Pitkäranta M. Improving Meaningful Use and User Experience of Healthcare Information Systems Towards Better Clinical Outcomes. Finnish Journal of eHealth and eWelfare. 2016;8(2–3):98–106. [Google Scholar]
- 4.Rajmohan P, Johar GM. Adoption of the Internet of Things in the Healthcare Services of Sri Lanka. International Journal of Recent Technology and Engineering. 2020;9(1):1095–104. [Google Scholar]
- 5.Central Intelligence Agency, “The World Factbook,” 20 December 2023. [Online]. Available: https://www.cia.gov/the-world-factbook/countries/sri-lanka. [Accessed 29 December 2023].
- 6.eHospital - Dompe Project – The Story of the Transformation of a District Hospital in Sri Lanka, 2013.
- 7.Central Intelligence Agency, “The World Factbook - Sri Lanka,” 28 October 2024. [Online]. Available: https://www.cia.gov/the-world-factbook/countries/sri-lanka/. [Accessed 6 11 2024].
- 8.Ministry of Health, “Policy Brief,” 2022. [Online]. Available: https://www.health.gov.lk/wp-content/uploads/2023/11/Digital-Trans.pdf. [Accessed 6 11 2024].
- 9.Ministry of Health, “Sri Lanka Digital Health Blueprint,” 2024. [Online]. Available: https://www.health.gov.lk/wp-content/uploads/2023/11/Digital-Health-Blue-Print-Full-Book-01.11.2023-Final.pdf. [Accessed 6 11 2024].
- 10.Jeyakodi T, Herath D. Acceptance and Use of Electronic Medical Records in Sri Lanka. Sci Res J. 2016;4(1).
- 11.Ammenwerth E. Technology Acceptance Models in Health Informatics: TAM and UTAUT. Studies in Health Technology and Informatics. 2019;263:64–71. [DOI] [PubMed] [Google Scholar]
- 12.Tubaishat A. Perceived Usefulness and Perceived Ease of Use of Electronic Health Records Among Nurses: Application of Technology Acceptance Model. Informatics for Health & Social Care. 2018;43(4):379–89. [DOI] [PubMed] [Google Scholar]
- 13.Alsyouf A, Lutfi A, Alsubahi N, Alhazmi FN, Al-Mugheed K, Anshasi RJ, Alharbi NI, Albugami M. The Use of a Technology Acceptance Model (TAM) to Predict Patients’ Usage of a Personal Health Record System: The Role of Security, Privacy, and Usability. International Journal of Environmental Research and Public Health. 2023;20(2):1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang H, Zhang J, Luximon Y, Qin M, Geng P, Tao D. The Determinants of User Acceptance of Mobile Medical Platforms: An Investigation Integrating the TPB, TAM, and Patient-Centered Factors. International Journal of Environmental Research and Public Health. 2022;19(17):10758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rehouma MB, Hofmann S. Government Employees’ Adoption of Information Technology - A Literature Review. in 19th Annual International Conference on Digital Government Research: Governance in the Data Age, Delft. 2018.
- 16.Melitski J, Gavin D, Gavin J. Technology Adoption and Organizational Culture in Public Organizations. Int J Organ Theory Behav. 2010;13(4).
- 17.Greenhalgh T, Wherton J, Papoutsi C, Lynch J, Hughes G, Court CA, Hinder S, Fahy N, Procter R, Shaw S. Beyond Adoption: A New Framework for Theorizing and Evaluating Nonadoption, Abandonment, and Challenges to the Scale-Up, Spread, and Sustainability of Health and Care Technologies. J Med Internet Res. 2017;19(11). [DOI] [PMC free article] [PubMed]
- 18.Kalayou MH, Endehabtu BF, Tilahun B. The Applicability of the Modified Technology Acceptance Model (TAM) on the Sustainable Adoption of eHealth Systems in Resource-Limited Settings. Journal of Multidisciplinary Healthcare. 2020;13:1827–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bazelais P, Doleck T, Lemay DJ. Investigating the Predictive Power of TAM: A Case Study of CEGEP Students’ Intentions to Use Online Learning Technologies. Education and Information Technologies. 2018;23:93–111. [Google Scholar]
- 20.Senthilrajah T, Ahangama S. An Analysis of the Use of Health Information Systems in Public Healthcare in Sri Lanka Using the Technology Acceptance Model. in 4th International Conference on Advanced Research in Computing (ICARC), Belihuloya, 2024.
- 21.Tan S-H, Wong C-K, Yap Y.-Y, Tan S-K. Factors Influencing Telemedicine Adoption Among Physicians in the Malaysian Healthcare System: A revisit. Digital Health. 1-26, 10. [DOI] [PMC free article] [PubMed]
- 22.Venkatesh V, Thong JYL, Xu X. Consumer Acceptance and Use of Information Technology: Extending the Unified Theory of Acceptance and Use of Technology. MIS Quarterly. 2012;36(1):157–78. [Google Scholar]
- 23.Susanto RD, Tjandinegara R, Iskandar V, Kartika EW. Technology Acceptance Model (TAM) Analysis of the Use of OVO Application in F&B Service Industry in Indonesia. J Tourism Culinary Entrepreneurship (JTCE), 2021;1(1):1-14.
- 24.Al-Hattami HM. Understanding Perceptions of Academics Toward Technology Acceptance in Accounting Education. Heliyon. 2023;9. [DOI] [PMC free article] [PubMed]
- 25.Balakrishnan J, Dwivedi YK, Hughes L, Boy F. Enablers and Inhibitors of AI-Powered Voice Assistants: A Dual-Factor Approach by Integrating the Status Quo Bias and Technology Acceptance Model. J Information Syst Front. 2021.
- 26.Barchielli C, Marullo C, Bonciani M, Vainieri M. Nurses and the Acceptance of Innovations in Technology-Intensive Contexts: The Need for Tailored Management Strategies. BMC Health Services Res. 2021;21:639. [DOI] [PMC free article] [PubMed]
- 27.Venkatesh V, Morris MG, Davis GB, Davis FD. User Acceptance of Information Technology: Toward a Unified View. MIS Quarterly. 2003;27(3):425–78. [Google Scholar]
- 28.Alkhwaldi AF, Abdulmuhsin AA. Understanding User Acceptance of IoT Based Healthcare in Jordan: Integration of the TTF and TAM. in Digital Economy, Business Analytics, and Big Data Analytics Applications. Studies in Computational Intelligence, Cham, 2022.
- 29.Holden RJ, Karsh BT. The Technology Acceptance Model: Its Past and its Future in Healthcare. Journal of Biomedical Informatics. 2009;43:159–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ezeudoka BC, Fan M. Determinants of Behavioural Intentions to Use An E-Pharmacy Service: Insights from TAM Theory and The Moderating Influence of Technological Literacy. Research in Social and Administrative Pharmacy. 2024;20:605–17. [DOI] [PubMed] [Google Scholar]
- 31.Liu JYW, Sorwar G, Rahman MS, Hoque MR. The Role of Trust and Habit in the Adoption of mHealth by older Adults in Hong Kong: A Healthcare Technology Service Acceptance (HTSA) Model. BMC Geriatrics. 2023;73(23). [DOI] [PMC free article] [PubMed]
- 32.Trawnih AA, Al-Adwan AS, Majali T, Al-Hattami HM. Investigating the Adoption of Social Commerce: A Case Study of SMEs in Jordan. Interdisciplinary J Information Knowledge Manag. 2023;18.
- 33.Li Y, Ma Y, Wang Y, Hong W, The Adoption of Smart Health Services by Older Adults in Retirement Communities: Analysis with the Technology Acceptance Model (TAM). Universal Access in the Information Society. 2024;1-17.
- 34.Zhu YZ, Zhao Z, Guo J, Wang Y, Zhang C, Zheng J, Zou Z, Liu W. Understanding Use Intention of mHealth Applications Based on the Unified Theory of Acceptance and Use of Technology 2 (UTAUT-2) Model in China. International Journal of Environmental Research and Public Health. 2023;20(4):3139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Serap T. An Investigation of Telemedicine Services, An Innovative and Technology-Based Healthcare Application, by Using the Extended Technology Acceptance Model (TAM2): An Example from Turkey. Eur J Appl Sci. 2023;11(1).
- 36.Kamal SA, Shafiq M, Kakria P, Investigating Acceptance of Telemedicine Services Through an Extended Technology Acceptance Model (TAM). Technol Soc. 2020;60.
- 37.Al-Hattami HM. What Factors Influence the Intention to Adopt Blockchain Technology in Accounting Education? Humanities and Social Sciences Communications. 2024;11(1):1–11. [Google Scholar]
- 38.Handayani PW, Hidayanto AN, Pinem AA, Hapsari IC, Sandhyaduhita PI, Budi I. Acceptance Model of a Hospital Information System. International Journal of Medical Informatics. 2017;99:11–28. [DOI] [PubMed] [Google Scholar]
- 39.Alhashmi SF, Salloum SA, Mhamdi C. Implementing Artificial Intelligence in the United Arab Emirates Healthcare Sector: An Extended Technology Acceptance Model. International Journal of Information Technology and Language Studies. 2019;3(3):27–42. [Google Scholar]
- 40.Hendy J, Reeves BC, Fulop N, Hutchings A, Masseria C. Challenges to Implementing the National Programme for Information Technology (NPfIT): A Qualitative Study. BMJ. 2005;331-336. [DOI] [PMC free article] [PubMed]
- 41.Andargolia AE, Scheepers H, Rajendran D. Health Information Systems Evaluation Frameworks: A Systematic Review. International Journal of Medical Informatics. 2017;97:195–209. [DOI] [PubMed] [Google Scholar]
- 42.Jeddi FR, Nabovati E, Bigham R, Farrahi R. Usability Evaluation of a Comprehensive National Health Information System: A Heuristic Evaluation. Informatics in Medicine Unlocked. 2020;13: 100332. [Google Scholar]
- 43.Carayon P, Hoonakker P. Human Factors and Usability for Health Information Technology: Old and New Challenges. Yearbook of Medical Informatics. 2019;28(1):71–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Al-Hattami HM, Almaqtari FA. What Determines Digital Accounting Systems’ Continuance Intention? An Empirical Investigation in SMEs. Humanities and Social Sciences Communications. 2023;10(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kusumawati NI, Sulistyawati. Acceptance of Health Information System for Public Health Centre in North Borneo, Indonesia. Int J Public Health Sci. 2018;7(3):168-174.
- 46.Al-Hattami HM, Al-Adwan AS, Abdullah AAH, Al-Hakimi MA, Determinants of Customer Loyalty toward Mobile Wallet Services in Post-COVID-19: The Moderating Role of Trust. Human Behav Emerg Technolog. 2023;1.
- 47.Wang C, Ahmad SF, Ayassrah AYABA, Awwad EM, Irshad M, Ali YA, Al-Razgan M, Khan Y, Han H. An Empirical Evaluation of Technology Acceptance Model for Artificial Intelligence in E-commerce. Heliyon. 2023;9(8). [DOI] [PMC free article] [PubMed]
- 48.Zobair KM, Sanzogni L, Sandhu K, Islam MJ. Health Seekers’ Acceptance and Adoption Determinants of Telemedicine in Emerging Economies. Australasian J Information Syst. 2021;25.
- 49.Sharma SK. Integrating Cognitive Antecedents into TAM to Explain Mobile Banking Behavioral Intention: A SEM-Neural Network Modeling. J Int Front. 2019;815-827.
- 50.Chowa M, Herold DK, Choo T-M, Chan K. Extending the Technology Acceptance Model to Explore the Intention to Use Second Life for Enhancing Healthcare Education. Computers & Education. 2012;59:1136–44. [Google Scholar]
- 51.Slade EL, Williams W, Dwivedi D. An Extension of the UTAUT 2 in a Healthcare Context. in UK Academy for Information Systems Conference, Oxford, 2013.
- 52.Zin KSLT, Kim S, Kim H.-S, Feyissa IF. A Study on Technology Acceptance of Digital Healthcare among Older Korean Adults Using Extended Tam (Extended Technology Acceptance Model). Administrative Sci. 2023;13(42).
- 53.Ngusie HS, Kassie SY, Chereka A. A, Enyew EB. Healthcare Providers’ Readiness for Electronic Health Record Adoption: a Cross-Sectional Study During Pre-Implementation Phase. BMC Health Serv Res. 2022;22(282). [DOI] [PMC free article] [PubMed]
- 54.Wang Y, Meister DB, Gray PH. Social Influence and Knowledge Management Systems Use: Evidence from Panel Data. MIS Quarterly. 2013;37(1):299–313. [Google Scholar]
- 55.Malhotra Y, Galletta DF. Extending the Technology Acceptance Model to Account for Social Influence: Theoretical Bases and Empirical Validation. in 32nd Annual Hawaii International Conference on Systems Sciences, Muai, 1999.
- 56.Cimperman M, Brencic MM, Trkman P. Analyzing Older Users’ Home Telehealth Services Acceptance Behavior-Applying an Extended UTAUT Model. International Journal of Medical Informatics. 2016;90:22–31. [DOI] [PubMed] [Google Scholar]
- 57.Diel S, Doctor E, Reith R, Buck C, Eymann T. Examining Supporting and Constraining Factors of Physicians’ Acceptance of Telemedical Online Consultations: A Survey Study. BMC Health Serv Res. 2023;23(1128). [DOI] [PMC free article] [PubMed]
- 58.Ludwick DA, Doucette J. Adopting Electronic Medical Records in Primary Care: Lessons learned from Health Information Systems Implementation Experience in Seven Countries. International Journal of Medical Informatics. 2009;78:22–31. [DOI] [PubMed] [Google Scholar]
- 59.Wu P, Zhang R, Luan J, Zhu M. Factors Affecting Physicians Using Mobile Health Applications: An Empirical Study. BMC Health Serv Res. 2022;22(24). [DOI] [PMC free article] [PubMed]
- 60.Rehouma MB, Hofmann S. Government Employees’ Adoption of Information Technology - A Literature Review. in 19th Annual International Conference on Digital Government Research: Governance in the Data Age, 2018.
- 61.Zhang Q, Zhang R, Lu X, Zhang X. What Drives the Adoption of Online Health Communities? An Empirical Study from Patient-Centric Perspective. BMC Health Serv Res. 2023;23(524). [DOI] [PMC free article] [PubMed]
- 62.Kowitlawakul Y, Sally CCW, Pulcini J, Wang W. Factors Influencing Nursing Students’ Acceptance of Electronic Health Records for Nursing Education (EHRNE) Software Program. Nurse Education Today. 2015;35:189–94. [DOI] [PubMed] [Google Scholar]
- 63.Tam C, Santos D, Oliveria T. Exploring the Influential Factors of Continuance Intention to use Mobile Apps: Extending the Expectation Confirmation Model. J Information Syst Front. 2018;243-257.
- 64.Lester S. New Technology and Professional Work. Professions and Professionalism. 2020;1:10. [Google Scholar]
- 65.Szymkowiak A, Melović B, Dabić M, Jeganathan K, Kundi GS. Information Technology and Gen Z: The Role of Teachers, The Internet, And Technology in The Education of Young People. Technol Soc. 2021;65.
- 66.Nawaz SS, Thowfeek M. H, Rashida MF. School Teachers’ Intention to Use E-Learning Systems in Sri Lanka: A Modified TAM Approach. Information Knowledge Manag. 2015;5(4).
- 67.Ranatunga RVSPK, Priyanath HMS, Megama RGN. Methods and Rule-Of-Thumbs in The Determination of Minimum Sample Size When Appling Structural Equation Modelling: A Review. Journal of Social Science Research. 2020;15(2):102–9. [Google Scholar]
- 68.Kock N, Hadaya P. Minimum Sample Size Estimation in PLS-SEM: The Inverse Square Root and Gamma-exponential Methods. Information Systems Journal. 2018;28(1):227–61. [Google Scholar]
- 69.Ramli NA, Latan H, Nartea GV. Why Should PLS-SEM Be Used Rather Than Regression? Evidence from the Capital Structure Perspective. in International Series in Operations Research & Management Science book series. Cham, Spring; 2018. vol. 267, pp. 171-209.
- 70.Hooi TK, Abu NHB, Rahim MKIA. Relationship of Big Data Analytics Capability and Product Innovation Performance using SmartPLS 3.2.6: Hierarchical Component Modelling in PLS-SEM. International Journal of Supply Chain Management. 2018;7(1):51–64. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The questionnaire was developed based on UTAUT2 and TAM existing surveys. However, questions were modified to relate to the Sri Lankan health sector. It is uploaded as a supplementary file.