Abstract
Background
The surgical complexity associated with the palatal roots of maxillary molars was considerably elevated. Previous studies on the relationships between maxillary molar roots and the maxillary sinus or cortical plates have focused on individual root observation without considering the positional relationship between buccal and palatal roots or analysing the surgical pathway of maxillary molar palatal roots. This study aimed to investigate the relationship between maxillary molar palatal roots and adjacent anatomical structures to provide a reference for performing palatal roots endodontic microsurgery.
Methods
Anatomical characteristics of the maxillary molar roots were determined using cone-beam computed tomography (CBCT) imaging data from 250 patients. The relationship between the root apex plane (RAP) and the maxillary sinus floor (MSF) was categorized into two types (Type I and Type II) based on whether the RAP was higher than the MSF or not. There were also two subclasses for Type I and Type II, which included Type I-a (RAP was lower than MSF), Type I-b (RAP and MSF were on the same plane), Type II-a (root apex protruded into the maxillary sinus) and Type II-b (root apex did not protrude into the maxillary sinus, but the RAP was higher than the MSF). Distances from the root apexes to the MSF and the cortical bone surface were measured.
Results
Of 500 teeth, 1352 roots were evaluated. Buccal roots obstruction 3 mm from the palatal root apex were present in almost all maxillary molars. The proportion of Type II-b cases in the palatal roots of three-rooted maxillary molars was significantly higher than that in the mesiobuccal (MB) and distalbuccal (DB) roots (P < 0.01). The distance from the root apex to the MSF increased with age and was significantly longer in females than in males (P < 0.05). The average distance from the apexes of palatal roots to the buccal cortical plate was 10.12 mm for first molars and 10.53 mm for the second molars. When measured through the MB roots, the distance to the buccal cortical plate was significantly shorter than that through the DB roots in the first molars (P < 0.05); however, the opposite was observed in the second molars (P < 0.05).
Conclusions
For determining the relationship between maxillary molar palatal roots and adjacent structures, CBCT provides reliable information, which acts as the basis for performing endodontic microsurgery of the palatal roots. Understanding the relationship between the roots of the maxillary molar and neighbouring anatomical structures helps surgeons evaluate potential difficulties, select optimal strategies, and reduce complications.
Clinical trial number
Not applicable.
Keywords: Endodontic microsurgery, CBCT, Maxillary sinus, Molars, Palatal roots
Background
Conventional nonsurgical endodontic treatment already boasts a high clinical success rate; however, persistent and complicated cases not responding to nonsurgical root canal treatment require surgical intervention. Endodontic microsurgery is a dependable treatment method with favourable initial healing and predictable outcomes [1]. Tooth survival rate ranged from 79 to 100%, with follow-up times of 2–13 years after endodontic microsurgery [2].
Tooth position influences the prognosis of endodontic microsurgery, with molars showing lower success rates [3]. Anatomical location, limited traction of the buccal mucosa, and root complexity make molar surgery more challenging than that of the anterior teeth. Notably, the palatal roots of maxillary molars have a complex anatomical position; they are distant from the buccal cortical plate and lie near critical anatomical structures, such as the major palatal vascular-nervous bundle and the maxillary sinus [4]. These factors complicate surgery. Despite these challenges, surgical endodontic treatment of maxillary molars, especially the palatal roots, is crucial and strategic to avoid tooth extraction.
Studies have highlighted the relationship between the root of the maxillary molars and the maxillary sinus floor (MSF), which can affect the incidence of odontogenic maxillary sinusitis [5–7]. The incidence of maxillary sinus perforation during endodontic microsurgery is higher in molars than in premolars [8]. Therefore, understanding the relationship between the roots, particularly the palatal roots of maxillary molars, and the MSF is essential for endodontic microsurgery. The relationship between maxillary molar roots and the MSF is diverse but inconsistent [9–11], complicating its use in apical surgical pathways. In this study, we simplified the classification, making it easier to remember and more convenient for clinical application in endodontic microsurgery.
Additionally, cortical bone thickness may be a concern during surgical endodontic procedures of the maxillary molars, as operative access and manipulation of surgical instruments are limited in a confined space. Although studies exist on the distance between maxillary molar roots and cortical plates [9, 12, 13], most focus on individual root observation without addressing the positional relationship between buccal and palatal roots or analysing the surgical pathway of maxillary molar palatal roots. In this study, we measured the distance from each maxillary molar root apex to the cortical plate and analysed the optimal surgical approach to the palatal root, providing valuable information for planning endodontic microsurgery.
Cone beam computed tomography (CBCT) offers non-invasive three-dimensional observation of roots and surrounding tissues [14–17]. For cases involving complex and difficult surgeries of the maxillary molars, preoperative CBCT analysis is effective in assessing risk factors, minimising complications, and improving therapeutic effects [17]. While CBCT facilitates observations across the coronal, sagittal, and axial planes, some physicians may still need to enhance their spatial visualisation abilities to grasp the intricate positional relationships. With its complex anatomy, the maxillary molar region demands a nuanced understanding. Our study expands upon traditional CBCT imaging by integrating three-dimensional reconstruction for a more vivid perspective to enhance the comprehension of root morphology and the interplay between the roots, maxillary sinus, and maxillae.
Therefore, this study utilised CBCT to observe the anatomical characteristics of maxillary molar roots, analyse the proximity of the palatal roots to the cortical bone surface and the MSF, and provide a reference for endodontic microsurgery of the palatal roots.
Methods
Participants
The Medical Ethics Committee of Beijing Stomatological Hospital, Capital Medical University, approved this study. CBCT images, alongside patient age and sex records, were obtained at Beijing Stomatological Hospital, Capital Medical University, from January 2021 to December 2022. The inclusion criteria were as follows: patients aged 21 years or older at the time of CBCT imaging [18]; images showing a complete view of the maxillary first and second molars and surrounding bone tissue, with clear and distinguishable anatomical structures; high-quality CBCT images without deformation; absence of root resorption, fractures, or root canal treatment in maxillary first and second molars; and absence of missing teeth among the maxillary posterior teeth, excluding the third molars.
Experimental design
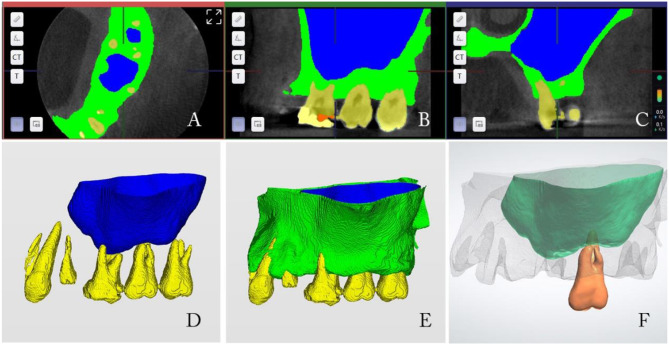
This study included CBCT images from 250 patients using a Kodak 9000 CBCT scanner (Eastman Kodak, USA). Patients were positioned upright, and the scanning plane was parallel to the orbitoauricular plane. Imaging parameters were set as follows: tube voltage of 70 kV, tube current of 10 mA, resolution of 76 μm, scan layer thickness of 0.2 mm, voxel size of 76 μm × 76 μm × 76 μm, and screen resolution of 1,280 × 1,024. CBCT data were imported into Dentalnavi 2.0 software (Yakebot, China) to automatically segment the maxillae, maxillary sinus, and roots. The segmented structures were then examined in the axial, coronal, and sagittal views of the CBCT scan to ensure segmentation accuracy across different planes. Following this, an automatic three-dimensional reconstruction of the segmented data was performed. The reconstructed data was subsequently imported into Exocad 3.0 (GmbH, Germany) software to smooth the surface and generate the final reconstruction images for observation (Fig. 1). The images were also imported into CS 3D Imaging Software 3.2.12 (Eastman Kodak, USA) for measurements. The examination of the segmented structures and subsequent measurements were conducted by two endodontists using serial axial, coronal and sagittal CBCT images. Additionally, 50 CBCT images were examined and measured twice, with a 1-week interval between measurements. Kappa values were calculated to assess reliability between the examiners, yielding values of 0.88. Following interobserver calibration, the study subjects were examined independently. Any disagreements were resolved through discussion between the two examiners.
Fig. 1.
Process of three-dimensional reconstruction. A, B, C: Segmentation and adjustment of the jawbone, maxillary sinus, and roots. D, E: Three-dimensional reconstruction of the segmented data. F: Smooth the surface of the three-dimensional reconstruction images
The number of roots and root morphology of the maxillary first and second molars were observed on serial axial CBCT images. Root length was recorded using Ren’s method [19], defined as the distance from the furthest root apex (maximum length) to the cemento-enamel junction plane. For maxillary molars with three roots, buccal roots were examined, and the distance between them was measured on the axial CBCT images at a slice 3 mm from the apex of the palatal root.
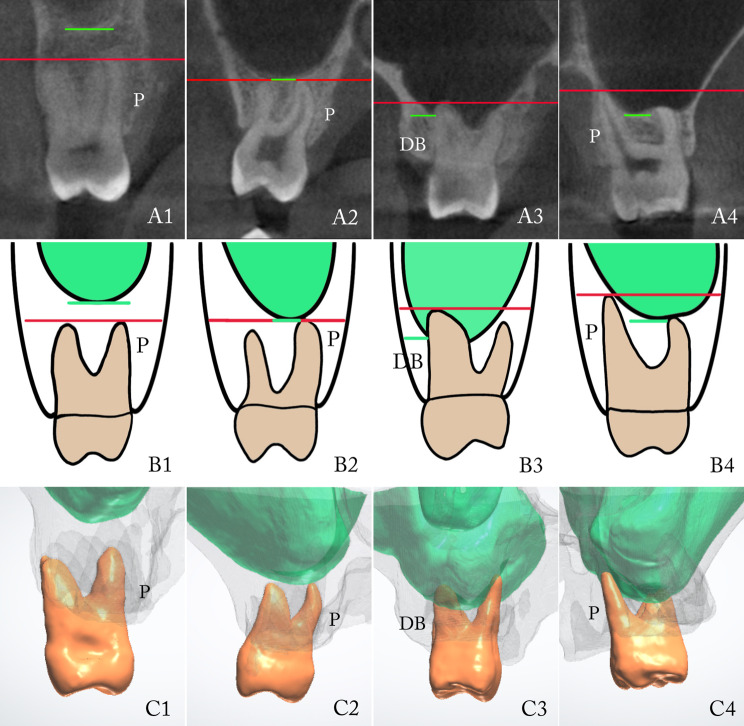
When designing treatment plans for endodontic microsurgery involving the maxillary sinus, the following factors must be considered: whether the roots were within the maxillary sinus and if a sinus lift procedure was necessary. Based on this, the relationship between the root apex and the MSF was classified as follows: a horizontal line was drawn from the root apex to the buccal cortical plate, forming the root apex plane (RAP). The corresponding illustrative diagrams and three-dimensional reconstruction images were shown in Fig. 2.
Fig. 2.
Cone beam computed tomography images, illustrative diagrams and three-dimensional reconstructions according to the classification of root apexes and maxillary sinus (A1—B4: Red line represented the root apex plane (RAP), and the green line represented the maxillary sinus floor (MSF); B1—C4: Green represented the MS, C1—C4: Grey represented the maxilla)
Type I: RAP was not higher than the MSF.
Type I-a: RAP was lower than the MSF.
Type I-b: RAP and MSF were on the same plane.
Type II: RAP was higher than the MSF.
Type II-a: Root apex protruded into the maxillary sinus.
Type II-b: Root apex did not protrude into the maxillary sinus; however, RAP was higher than the MSF.
A1, B1,C1(Type I-a): RAP was lower than MSF. A2, B2,C2 (Type I-b): RAP and MSF were on the same plane. A3, B3,C3(Type II-a) Root apex protruded into the maxillary sinus. A4, B4,C4(Type II-b): Root apex did not protrude into the maxillary sinus; however, RAP was higher than the MSF.
The distance from the root apex to the MSF was measured in the coronal and sagittal planes of the CBCT, and the shorter value was recorded as the final distance. The distance for Type I-b was recorded as 0 and for Type II was recorded as a negative number. In Type I, roots with distances ranging from 0 to 2 mm were summarised.
The included patients were divided into four age groups (21–30, 31–40, 41–50, and 51–60 years) to compare the distance between RAP and MSF across age groups.
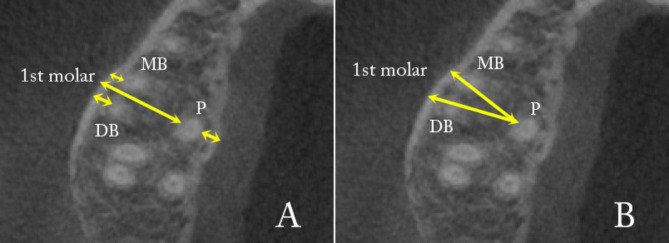
The shortest horizontal distance from the root apexes of the maxillary molars to the outer surface of the buccal cortical plate was determined using axial images. Additionally, the shortest distance between the apexes of palatal roots and the palatal cortical plate was measured. The distance from the palatal roots to the buccal cortical plate through the mesiobuccal (MB) and distobuccal (DB) roots was calculated for teeth with three roots (Fig. 3).
Fig. 3.
Maxillary axial CBCT view for measurements. A: The distances from the root apexes of the maxillary first molar to the buccal cortical plate, as well as the distance from the apex of the palatal root to the palatal cortical plate. B: The distances from the palatal roots to the buccal cortical plate, passing through the MB and DB roots, were calculated for teeth with three roots
Statistical analyses
Statistical analyses were performed using SPSS software (version 18.0; SPSS, Inc., Chicago, IL, USA). Root number and morphology were analysed, and root length was measured. The Wilcoxon Mann–Whitney U test assessed differences in root length between males and females. Chi-square tests were performed to analyse the relationship between RAP and MSF classification.
The distance from the RAP to the MSF was measured, and a one-way analysis of variance was used to determine if there were statistical differences among the different age groups.
The distances from the root apex to the buccal and palatal cortical plates were also statistically analysed. Comparisons were made according to the tooth position, side, and sex. An independent sample t-test was used for data following a normal distribution, while the Mann–Whitney U test was used for non-normally distributed data. Differences with a P value < 0.05 were considered statistically significant.
Results
In total, 500 maxillary molars (254 left, 246 right) with 1,352 roots from 250 patients (81 males, 169 females) met the inclusion criteria.
Root anatomy characteristics
The number of tooth roots ranged from one to four. Maxillary first and second molars with three roots had the highest proportions, at 97.2 and 57.6%, respectively. Two-rooted maxillary second molars constituted 27.2% (Fig. 4). Among these, the fusion of the buccal roots with a separate palatal root comprised 18%. Fusion of the palatal roots with either MB or DB roots made up 8% and 1.2%, respectively. One maxillary second molar with four roots, consisting of three buccal roots and one palatal root, was observed.
Fig. 4.
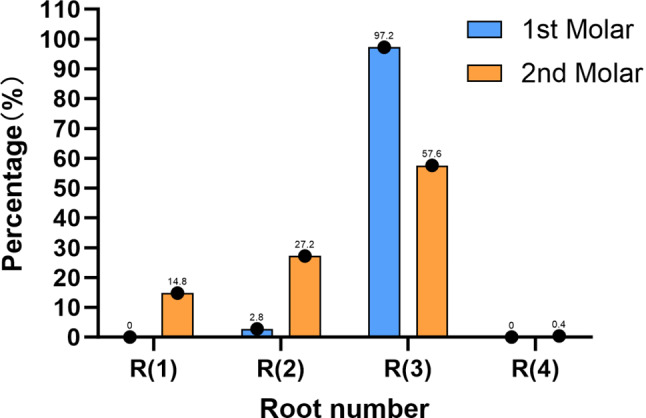
The percentage distribution of root numbers in the first and second maxillary molars
The average root lengths of the maxillary first and second molars were 12.22 ± 1.51 mm and 12.24 ± 1.47 mm, respectively. Males had an average root length of 12.65 ± 1.62 mm, which was significantly longer than that of females at 12.03 ± 1.39 mm (P < 0.05).
Of the 387 three-rooted maxillary molars, two lacked buccal root obstruction on the slice image below 3 mm from the palatal root apexes. The average distances between the MB and DB roots corresponding to the site 3 mm from the palatal root apexes of the three-rooted maxillary first and second molars were 1.88 ± 1.03 mm and 1.05 ± 0.70 mm, respectively, with maximums of 4.8 mm and 2.9 mm.
Relationship between root apexes and MSF
Classification of Relationships between RPA and MSF.
In classifying the relationship between RPA and MSF of the maxillary first and second molars (Table 1), Type I accounted for 78.9% and 83.4%, respectively, exceeding Type II. Type I-b was the most common in one-rooted maxillary second molars. Among three-rooted maxillary molars, Type I-b predominated in the DB roots over the MB or palatal roots. In Type II, the proportion of Type II-a was low, representing 3.1% and 3.9% for the first and second molars, respectively. Type II-b was significantly higher in the palatal roots of three-rooted maxillary molars than in the MB and DB roots (P < 0.01).
Table 1.
Classification of relationships between RPA and MSF in Maxillary First and Second molars
| Root | 1st molar (N = 250) | 2nd molar (N = 250) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| R(2),n(%) | R(3),n(%) | Total n(%) |
R(1) n (%) |
R(2),n(%) | R(3),n(%) | R(4),n(%) | Total n(%) |
|||||||||||
| B | P | MB | DB | P | B | P | MB | DB | P | MB | BM | DB | P | |||||
| I | I-a |
6 (85.71) |
3 (42.86) |
200 (82.30) |
192 (79.01) |
104 (42.80) |
505 (67.97) |
21 (56.76) |
50 (73.53) |
45 (66.18) |
105 (72.92) |
103 (71.53) |
89 (61.81) |
1 (100) |
1 (100) |
1 (100) |
1 (100) |
417 (68.47) |
| I-b |
1 (14.29) |
2 (28.57) |
31 (12.76) |
37 (15.23) |
10 (4.12) |
81 (10.90) |
11 (29.73) |
7 (10.29) |
5 (7.35) |
27 (18.75) |
30 (20.83) |
11 (7.64) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
91 (14.94) |
|
| II | II-a |
0 (0) |
0 (0) |
9 (3.70) |
9 (3.70) |
5 (2.06) | 23 (3.10) |
1 (2.70) |
2 (2.94) |
2 (2.94) |
9 (6.25) |
9 (6.25) |
1 (0.69) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
24 (3.94) |
| II-b |
0 (0) |
2 (28.57) |
3 (1.23) |
5 (2.06) |
124 (51.03) |
134 (18.03) |
4 (10.81) |
9 (13.24) |
16 (23.53) |
3 (2.08) |
2 (1.39) |
43 (29.86) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
77 (12.64) |
|
| Total |
7 (100) |
7 (100) | 243 (100) | 243 (100) | 243 (100) | 743 (100) |
37 (100) |
68 (100) | 68 (100) |
144 (100) |
144 (100) |
144 (100) |
1 (100) |
1 (100) |
1 (100) |
1 (100) |
609 (100) |
|
(2) Distance from Root Apexes to MSF.
The average distance ranged from 1.98 ± 1.78 mm to 3.66 ± 2.85 mm. Females had significantly longer distances than males (P < 0.05), with no significant differences between the left and right sides. In Type I, the distance ranged from 0 to 2 mm (Table 2), with the buccal roots of the maxillary molars having a higher proportion than the palatal roots.
Table 2.
The proportions of the cases with distances ranging from 0 to 2 mm in Type I
| Root | 1st molar (N = 250) | 2nd molar (N = 250) | Total n(%) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| R(2),n(%) | R(3),n(%) | Total n(%) | R(1) n(%) |
R(2),n(%) | R(3),n(%) | R(4),n(%) | |||||||||||
| B | P | MB | DB | P | B | P | MB | DB | P | MB | BM | DB | P | ||||
| 0–2 mm |
5 (71.43) |
3 (42.86) |
117 (42.86) |
132 (54.32) |
39 (16.05) |
296 (39.84) |
22 (59.46) |
39 (57.35) |
21 (30.88) |
85 (59.03) |
79 (54.86) |
46 (31.94) |
1 (100) |
0 (0) |
0 (0) |
1 (100) |
292 (47.95) |
The distance between the root apexes and the MSF increased with age in all roots of the maxillary molars, and significant differences were found among all groups except the 21–30 years group (P < 0.05).
Distance from root apexes to buccal and palatal cortical plates
The distances from the MB, DB, and palatal roots to the buccal cortical plate in three-rooted maxillary second molars were significantly longer than in maxillary first molars (P < 0.01). The average distances from the palatal roots to the buccal cortical plate in three-rooted maxillary first and second molars were 10.12 ± 1.39 mm and 10.53 ± 1.48 mm, respectively (Table 3). Males exhibited longer distances compared to females (P < 0.05), with no statistically significant difference observed between the right and left sides. Similarly, the distance from the DB roots to the buccal cortical plate was significantly greater in males than in females in the three-rooted maxillary second molars (P < 0.05).
Table 3.
Distance from Root apexes to Buccal Cortical Plates of Maxillary First and Second molars (mm)
| Root | 1st molar (N = 250) | 2nd molar (N = 250) | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| R(2) | R(3) | R(1) | R(2) | R(3) | R(4) | ||||||||||||||||
| MB and DB were fused | P fused with MB or DB | MB and DB were fused | P fused with MB or DB | ||||||||||||||||||
| B | P | Separate root | Fused root | Diameter of the fused root | MB | DB | P | B | P | Separate root | Fused root | Diameter of the fused root | MB | DB | P | MB | BM | DB | P | ||
| Males | 0 | 0 | 0.7 | 1 | 10.4 | 1.06 ± 1.06 | 1.67 ± 1.27 | 10.35 ± 1.42 | 4.44 ± 1.72 | 2.68 ± 1.69 | 10.21 ± 1.81 | 3.56 ± 1.40 | 4.80 ± 1.40 | 8.49 ± 1.96 | 3.37 ± 1.39 | 2.78 ± 1.21 | 11.10 ± 1.38 | - | - | - | - |
| Females | 1.43 ± 0.96 | 10.30 ± 0.62 | 1.10 ± 0.36 | 3.40 ± 0.20 | 8.17 ± 0.25 | 1.02 ± 0.94 | 1.56 ± 1.08 | 10.00 ± 1.37 | 3.53 ± 0.87 | 3.38 ± 1.97 | 10.02 ± 1.60 | 3.34 ± 0.80 | 4.11 ± 1.33 | 8.53 ± 1.49 | 2.96 ± 1.30 | 2.35 ± 1.35 | 10.19 ± 1.45 | 3.8 | 0.7 | 2.6 | 10.8 |
| Total | 1.43 ± 0.96 | 10.30 ± 0.62 | 1.00 ± 0.36 | 2.80 ± 1.21 | 8.73 ± 1.14 | 1.03 ± 0.98 | 1.59 ± 1.15 | 10.12 ± 1.39 | 3.80 ± 1.24 | 3.23 ± 1.91 | 10.06 ± 1.63 | 3.41 ± 0.99 | 4.32 ± 1.36 | 8.51 ± 1.60 | 3.11 ± 1.34 | 2.51 ± 1.31 | 10.53 ± 1.48 | 3.8 | 0.7 | 2.6 | 10.8 |
The distance from the palatal roots to the buccal bone plate through the MB roots was significantly shorter than through the DB roots in the three-rooted maxillary first molars (P < 0.05). Conversely, it was the opposite in the second molars (P < 0.05).
The average distance from the palatal root to the palatal cortical plate was 1.95 ± 0.98 mm (Table 4). In one-rooted maxillary second molars, the distance from the palatal root to the palatal cortical plate was greater than that of two- and three-rooted maxillary first and second molars. In two-rooted maxillary molars, the distance was shorter if the palatal root was independent. There was no significant difference in the distance from the palatal root to the palatal cortical plate between the three-rooted maxillary first and second molars. In the three-rooted maxillary first molars, males had significantly greater distances than females (P < 0.05). No statistically significant difference was observed between the right and left sides of the three-rooted maxillary molars.
Table 4.
Distance from Palatal Roots to Palatine Cortical Plate of Maxillary First and Second molars (mm)
| Root | 1st molar (N = 250) | 2nd molar (N = 250) | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| R(2) | R(3) | R(1) | R(2) | R(3) | R(4) | ||||
| Separate P | P fused with MB or DB | Separate P | P fused with MB or DB | ||||||
| Males | - | 2.1 | 1.88 ± 0.80 | 3.44 ± 1.15 | 2.36 ± 1.21 | 3.27 ± 0.68 | 1.84 ± 0.95 | - | 2.07 ± 1.01 |
| Females | 1.50 ± 1.10 | 2.77 ± 0.78 | 1.66 ± 0.69 | 3.66 ± 0.98 | 1.93 ± 0.98 | 2.33 ± 0.96 | 1.68 ± 0.84 | 1.6 | 1.89 ± 0.97 |
| Total | 1.50 ± 1.10 | 2.60 ± 0.72 | 1.74 ± 0.73 | 3.59 ± 1.02 | 2.12 ± 1.31 | 2.62 ± 0.97 | 1.74 ± 0.88 | 1.6 | 1.95 ± 0.98 |
Discussion
This study analysed the root anatomical characteristics of maxillary molars, the positional relationship between the palatal roots and the MSF, and the buccal and palatal cortical bone surface using CBCT. Unlike previous studies [9–14], we reconstructed the teeth, the maxillary sinus, and the maxillae using data derived from CBCT scans. This reconstruction allowed for the isolated or simultaneous visualisation of these anatomical structures, providing a clear and comprehensive examination of their interrelationships. Our method substantially enhances clinicians’ ability to intuitively understand the spatial orientation of the roots, maxillary sinus, and maxillae, offering value for the preoperative evaluation of endodontic microsurgery on palatal roots.
Downward growth of the maxillary sinus continues until 21 years of age [18]; therefore, all subjects in this study were at least 21 years old. Results showed an increasing distance between the RAP and the MSF with age, consistent with prior findings [10, 20, 21]. This may be due to reduced maxillary sinus volume with age, causing the MSF to move upward [18, 22]. This implies that when treating maxillary molars in young patients, maxillary sinus factors must be considered to prevent complications such as maxillary sinus perforation. Additionally, the distance from root apexes to MSF was shorter in males than in females, consistent with the findings of Von et al. [23] We also measured the root lengths, finding that the average root lengths of the maxillary first and second molars were 12.22 ± 1.51 mm and 12.24 ± 1.47 mm, respectively, consistent with the results of Ren et al. [19] The average root length in males was significantly greater than in females, which may explain the difference in the distance to the MSF between genders. However, a limitation of the present study is the disparity in the number of male and female patients. Future studies assessing gender differences should consider a larger sample size.
Given that the roots of the maxillary molars are adjacent to the maxillary sinus, this study classified the RAP–MSF relationship into two categories based on whether the RAP was higher than the MSF, aiding preoperative analysis and risk assessment in both nonsurgical and surgical treatment of maxillary molars. Approximately 20% of the maxillary molars exhibited a Type II relationship with the maxillary sinus, with Type II-b molars predominating, particularly in the palatal root of three-rooted maxillary first molar (51%), similar to the 45% reported by Kalender et al. [14] The proportion of Type II-b in the palatal roots of three-rooted maxillary molars was significantly higher than that in the MB and DB roots, consistent with previous studies [21, 24–26]. For such cases, maxillary sinus elevation should first be completed to locate the palatal root apexes and proceed with endodontic microsurgery. Azim et al. [27] reported two cases in which apicoectomy was needed on the palatal roots of maxillary molars. Surgical intervention includes a buccal approach to treat the buccal roots, sinus lift using piezosurgery, and palatal root resection. However, after maxillary sinus elevation, it becomes challenging to locate the palatal roots due to the distance from the surgical area to the buccal side and poor visibility. Recently, guided endodontics has been introduced, including static or dynamic for endodontic or surgical treatment of complex cases, in order to achieve predictable and safe outcomes. Static guided endodontics involves the fabrication of 3D-printed templates based on CBCT images, surface scans and virtual imaging software [28]. And the dynamic navigation system is a computer-aided technology that provides real-time feedback to the clinician regarding the drill path during treatment [29]. Guided endodontics shows promise as a technique for endodontic microsurgery of palatal roots.
The implant placement literature recommends maintaining a 2-mm safety zone between vital anatomic structures, such as nerve canals, and the implant site [30], which is also crucial for safe surgical access in endodontic microsurgery. Therefore, even with a RAP–MSF Type I relationship, caution is necessary to prevent perforation. This study calculated the proportions of cases with distances ranging from 0 to 2 mm in Type I. The proportion of buccal roots in three-rooted molars was higher than that of palatal roots, which aligns with the findings of Wang et al. [31]. Although the buccal surgical pathway is shorter for the buccal roots compared to palatal roots, precise operation is still required to minimise the risk of maxillary sinus perforation during surgery. In the event of an inadvertent maxillary sinus perforation, it is essential to prevent foreign objects from entering the sinus for subsequent operations.
Furthermore, this study measured the number of roots and positional relationships in maxillary molars. Most maxillary first molars had three separate roots, whereas a lower percentage of second molars had more fused roots. These results are consistent with previous studies [10, 19]. The higher frequency of three-rooted maxillary second molars reported in earlier studies may be attributed to ethnic and regional differences [32, 33]. In nearly all cases, the region 3 mm from the root apexes of the palatal roots of the three-rooted maxillary molars was obstructed by the buccal roots. The average distances between the two buccal roots were 1.88 ± 1.03 mm and 1.05 ± 0.70 mm for the first and second molars, respectively, with the maximum value reaching only 4.8 mm. Therefore, endodontic microsurgery on the palatal roots from the buccal side often requires microsurgery simultaneously on one or both buccal roots. The distance from palatal roots to the buccal bone plate through the MB roots was shorter than that through the DB roots in three-rooted first molars, indicating that in cases where both buccal roots lack periapical lesions, establishing a surgical pathway through the MB root should be prioritised to complete apicoectomy on the palatal roots. However, in three-rooted maxillary second molars, the opposite result was observed, complicating palatal root apical surgery.
The average distances from the palatal roots of three-rooted maxillary first and second molars to the buccal cortical bone surface were 10.12 and 10.53 mm, respectively, consistent with findings by Jin et al. [13] Kang’s study reported corresponding distances of 12.16 and 11.28 mm [9], and Lee et al. [34] noted significantly greater distances in second molars. Comparisons between sexes revealed that the distances from the palatal roots to the buccal cortical bone surface of three-rooted maxillary molars were significantly longer in males than in females, consistent with previous studies [9, 14], attributed to skeletal size differences between sexes. In two-rooted maxillary molars, when palatal roots were separate and buccal roots fused, the average distances from the palatal root to the buccal cortical plate were 10.30 and 10.06 mm, respectively. When the palatal root fused with the MB or DB root, the distances from the fused roots to the buccal cortical plate were only 2.80 and 4.32 mm, respectively, with the transverse diameters of the fused portions averaging 8.73 and 8.51 mm. Therefore, if a buccal surgical pathway is desired to remove lesions around the palatal root, the distance could still exceed 10 mm. Studies have shown significant deviations when insertion depths exceed 5 mm [35]. This makes it challenging to perform accurate osteotomy and root-end resection during palatal root endodontic microsurgery. Recently, guided endodontic microsurgery has been introduced, demonstrating precise osteotomy site, angulation depth, and diameter [36]. Giacomino et al. [37] reported a case that involved apical surgery addressing the fused DB and palatal root using three-dimensional printed surgical guides.
This study also measured the distance from the palatal roots of the maxillary molars to the palatal bone plate, which averaged 1.95 ± 0.98 mm. The distance in one-rooted maxillary second molars exceeded that in the double and triple-rooted maxillary molars. In three-rooted maxillary molars, the distance decreased when the palatal root was isolated. Thus, the insertion depth can be significantly reduced when surgery is performed from the palatal side. However, complex and critical anatomical structures present challenges. Relevant research indicated that targeted endodontic microsurgery (TEMS) of the maxillary palatal root, which combined the use of trephine burs and 3D-printed guided to perform flapless maxillary palatal root-end surgery, could achieve a 2-mm safety margin in 47% of first molars and 52% of second molars [38]. Some case reports have attempted palatal root endodontic microsurgery of maxillary molars on the palatal side [37]. However, another challenge is obtaining a clear view and adequate operating space. Static and dynamic navigation technologies can only assist in osteotomy and root-end resection [37, 39], but operators still rely on microscopes for root-end preparation and filling. Notably, the position of the operator remains challenging. Despite avoiding major blood vessels, bleeding after flipping the palatal flap is more frequent due to thicker gingiva, and this may obstruct the operational field of view. Therefore, future researches are needed to guide the process of real-time root-end preparation and filling under the navigation.
Conclusion
Within the scope of this study, the findings show that the buccal roots almost entirely obscure the palatal root apexes of the maxillary molars. The proportion of palatal root apexes positioned higher than the maxillary sinus floor is greater than that of other roots. Additionally, the distance between the palatal root apexes and the maxillary sinus increases with age, with an average distance of approximately 10 mm to the buccal cortical plate. CBCT proves to be a powerful tool for evaluating surgical cases with accurate measurements. Understanding the anatomical profile of the palatal roots of the maxillary molars and their relation to adjacent anatomical structures is beneficial for preoperative difficulty assessment, selecting optimal strategies, and preventing complications.
Acknowledgements
The authors wish to express gratitude to those who have contributed in various ways to the field of research presented in this article.
Abbreviations
- CBCT
Cone Beam Computed Tomography
- MSF
Maxillary Sinus Floor
- RAF
Root Apex Plane
Author contributions
XXH, JX and BXH contributed to the study conception and design. Data analysis were performed by XXH and JX. YW provided technical support. XXH wrote the manuscript. BXH revised the manuscript. All authors read and approved the final manuscript.
Funding
This study was supported by the Beijing Municipal Science & Technology Commission (No. Z191100006619037).
Data availability
The data sources utilised and interpreted during the present research are accessible upon reasonable request from the corresponding author.
Declarations
Ethics approval and consent to participate
The Medical Ethics Committee of Beijing Stomatological Hospital, Capital Medical University, approved this study (approval number: CMUSH-IRB-KJ-PJ-2023-11). The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments. Written informed consent was obtained from all participants prior to the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kang M. In Jung H, Song M, Kim SY, Kim HC, Kim E. Outcome of nonsurgical retreatment and endodontic microsurgery: a meta-analysis. Clin Oral Investig. 2015;19:569 – 82. [DOI] [PubMed]
- 2.Pinto D, Marques A, Pereira JF, Palma PJ, Santos JM. Long-term prognosis of endodontic microsurgery-a systematic review and meta-analysis. Med (Kaunas). 2020;56:447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou W, Zheng Q, Tan X, Song D, Zhang L, Huang D. Comparison of mineral trioxide aggregate and iRoot BP plus root repair material as root-end filling materials in endodontic microsurgery: a prospective randomised controlled study. J Endod. 2017;43:1–6. [DOI] [PubMed] [Google Scholar]
- 4.Yu SK, Lee MH, Park BS, Jeon YH, Chung YY, Kim HJ. Topographical relationship of the greater palatal artery and the palatal spine. Significance for periodontal surgery. J Clin Periodontol. 2014;49:908–13. [DOI] [PubMed] [Google Scholar]
- 5.Ariji Y, Obayashi N, Goto M, Izumi M, Naitoh M, Kurita K, Shimozato K, Ariji E. Roots of the maxillary first and second molars in horizontal relation to alveolar cortical plates and maxillary sinus: computed tomography assessment for infection spread. Clin Oral Investig. 2006;10:35–41. [DOI] [PubMed] [Google Scholar]
- 6.Oberli K, Bornstein MM, von Arx T. Periapical surgery and the maxillary sinus: radiographic parameters for clinical outcome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:848–53. [DOI] [PubMed] [Google Scholar]
- 7.Hauman CH, Chandler NP, Tong DC. Endodontic implications of the maxillary sinus: a review. Int Endod J. 2002;35:127–41. [DOI] [PubMed] [Google Scholar]
- 8.Freedman A, Horowitz I. Complications after apicoectomy in maxillary premolar and molar teeth. Int J Oral Maxillofac Surg. 1999;28:192–4. [PubMed] [Google Scholar]
- 9.Kang SH, Kim BS, Kim Y. Proximity of posterior teeth to the maxillary sinus and buccal bone thickness: a biometric assessment using cone-beam computed tomography. J Endod. 2015;41:1839–46. [DOI] [PubMed] [Google Scholar]
- 10.Tian XM, Qian L, Xin XZ, Wei B, Gong Y. An analysis of the proximity of maxillary posterior teeth to the maxillary sinus using cone-beam computed tomography. J Endod. 2016;42:371–77. [DOI] [PubMed] [Google Scholar]
- 11.Pagin O, Centurion BS, Rubira-Bullen IR, Alvares CA. Maxillary sinus and posterior teeth: accessing close relationship by cone-beam computed tomographic scanning in a Brazilian population. J Endod. 2013;39:748–51. [DOI] [PubMed] [Google Scholar]
- 12.Porto O, Silva B, Silva JA, Estrela C, Alencar AHG, Bueno M, Estrela C. CBCT assessment of bone thickness in maxillary and mandibular teeth: an anatomic study. J Appl Oral Sci. 2020;7:28e20190148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jin GC, Kim KD, Roh BD, Lee CY, Lee SJ. Buccal bone plate thickness of the Asian people. J Endod. 2015;31:430–34. [DOI] [PubMed] [Google Scholar]
- 14.Kalender A, Aksoy U, Basmaci F, Orhan K, Orhan AI. Cone-beam computed tomography analysis of the vestibular surgical pathway to the palatal root of the maxillary first molar. Eur J Dent. 2013;7:35–40. [PMC free article] [PubMed] [Google Scholar]
- 15.Regnstrand T, Ezeldeen M, Shujaat S, Alqahtani KA, Benchimol D, Jacobs R. Three-dimensional quantification of the relationship between the upper first molar and maxillary sinus. Clin Exp Dent Res. 2022;8:750–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rigolone M, Pasqualini D, Bianchi L, Berutti E, Bianchi SD. Vestibular surgical access to the palatal root of the superior first molar: low-dose cone-beam CT analysis of the pathway and its anatomic variations. J Endod. 2003;29:773–75. [DOI] [PubMed] [Google Scholar]
- 17.Low KM, Dula K, Bürgin W, von Arx T. Comparison of periapical radiography and limited cone-beam tomography in posterior maxillary teeth referred for apical surgery. J Endod. 2008;34:557–62. [DOI] [PubMed] [Google Scholar]
- 18.Ariji Y, Ariji E, Yoshiura K, Kanda S. Computed tomographic indices for maxillary sinus size in comparison with the sinus volume. Dentomaxillofac Radiol. 1996;25:19–24. [DOI] [PubMed] [Google Scholar]
- 19.Ren HY, Kum KY, Zhao YS, Yoo YJ, Jeong JS, Perinpanayagam H, Wang XY, Li GJ, Wang F, Fang H, Gu Y. Maxillary molar root and canal morphology of neolithic and modern Chinese. Arch Oral Biol. 2021;131:105272. [DOI] [PubMed] [Google Scholar]
- 20.Pei J, Liu J, Chen Y, Liu Y, Liao X, Pan J. Relationship between maxillary posterior molar roots and the maxillary sinus floor: cone-beam computed tomography analysis of a western Chinese population. J Int Med Res. 2020;48:300060520926896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gu Y, Sun C, Wu D, Zhu Q, Leng D, Zhou Y. Evaluation of the relationship between maxillary posterior teeth and the maxillary sinus floor using cone-beam computed tomography. BMC Oral Health. 2018;18:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ariji Y, Kuroki T, Moriguchi S, Ariji E, Kanda S. Age changes in the volume of the human maxillary sinus: a study using computed tomography. Dentomaxillofac Radiol. 1994;23:163–68. [DOI] [PubMed] [Google Scholar]
- 23.von Arx T, Fodich I, Bornstein MM. Proximity of premolar roots to maxillary sinus: a radiographic survey using cone-beam computed tomography. J Endod. 2014;40:1541–48. [DOI] [PubMed] [Google Scholar]
- 24.Jang JK, Kwak SW, Ha JH, Kim HC. Anatomical relationship of maxillary posterior teeth with the sinus floor and buccal cortex. J Oral Rehabil. 2017;44:617–25. [DOI] [PubMed] [Google Scholar]
- 25.Nino-Barrera JL, Ardila E, Guaman-Pacheco F, Gamboa-Martinez L, Alzate-Mendoza D. Assessment of the relationship between the maxillary sinus floor and the upper posterior root tips: clinical considerations. J Investig Clin Dent. 2018;9:e12307. [DOI] [PubMed] [Google Scholar]
- 26.Themkumkwun S, Kitisubkanchana J, Waikakul A, Boonsiriseth K. Maxillary molar root protrusion into the maxillary sinus: a comparison of cone beam computed tomography and panoramic findings. Int J Oral Maxillofac Surg. 2019;48:1570–76. [DOI] [PubMed] [Google Scholar]
- 27.Azim AA, Wang HH, Serebro M. Selective retreatment and sinus lift: an alternative approach to surgically manage the palatal roots of maxillary molars. J Endod. 2021;47:648–57. [DOI] [PubMed] [Google Scholar]
- 28.Moreno-Rabié C, Torres A, Lambrechts P, Jacobs R. Clinical applications, accuracy and limitations of guided endodontics: a systematic review. Int Endod J. 2020;53:214–31. [DOI] [PubMed] [Google Scholar]
- 29.Vasudevan A, Santosh SS, Selvakumar RJ, Durga Tharini Sampath DT, Natanasabapathy V. Dynamic Navigation in guided endodontics - a systematic review. Eur Endod J. 2022;7:81–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Greenstein G, Tarnow D. The mental foramen and nerve: clinical and anatomical factors related to dental implant placement: a literature review. J Periodontol. 2006;77:1933–43. [DOI] [PubMed] [Google Scholar]
- 31.Wang S, Wang X, Jiang J, Tiwari SK, Xiao Y, Ye L, Peng L. Relationship between the surgical access line of maxillary posterior teeth and the maxillary sinus floor. J Endod. 2022;48:509–15. [DOI] [PubMed] [Google Scholar]
- 32.Buchanan GD, Gamieldien MY, Fabris-Rotelli I, Van Schoor A, Uys A. Root and canal morphology of maxillary second molars in a black South African subpopulation using cone-beam computed tomography and two classifications. Aust Endod J. 2023;1:217–27. [DOI] [PubMed] [Google Scholar]
- 33.Rwenyonyi CM, Kutesa AM, Muwazi LM, Buwembo W. Root and canal morphology of maxillary first and second permanent molar teeth in a Ugandan population. Int Endod J. 2007;40:679–83. [DOI] [PubMed] [Google Scholar]
- 34.Lee HS, Kim D, Kim SK. Proximity of maxillary molar apexes to the cortical bone surface and the maxillary sinus. Restor Dent Endod. 2022;47:e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dianat O, Nosrat A, Mostoufi B, Price JB, Gupta S, Martinho FC. Accuracy and efficiency of guided root-end resection using a dynamic navigation system: a human cadaver study. Int Endod J. 2021;54:793–801. [DOI] [PubMed] [Google Scholar]
- 36.Strbac GD, Schnappauf A, Giannis K, Moritz A, Ulm C. Guided modern endodontic surgery: a novel approach for guided osteotomy and root resection. J Endod. 2017;43:496–501. [DOI] [PubMed] [Google Scholar]
- 37.Giacomino CM, Ray JJ, Wealleans JA. Targeted endodontic microsurgery: a novel approach to anatomically challenging scenarios using 3-dimensional-printed guides and trephine burs-a report of 3 cases. J Endod. 2018;44:671–77. [DOI] [PubMed] [Google Scholar]
- 38.Smith BG, Pratt AM, Anderson JA, Ray JJ. Targeted endodontic microsurgery: implications of the greater palatal artery. J Endod. 2021;47:19–27. [DOI] [PubMed] [Google Scholar]
- 39.Chen C, Zhang R, Zhang W, Li F, Wang Z, Qin L, Chen Y, Bian Z, Meng L. Clinical and radiological outcomes of dynamic navigation in endodontic microsurgery: a prospective study. Clin Oral Investig. 2023;27:5317–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sources utilised and interpreted during the present research are accessible upon reasonable request from the corresponding author.