CSF transport in the CNS is an old research topic, yet is decidedly contemporary. A question yet to be answered relates to the drainage of brain waste via the CSF: how does CSF containing waste products exit the brain barriers that shield the CNS? The nature of the anatomical structures that enable CSF exchange via the dura—which is the outer layer of the meninges in contact with the skull—is heavily debated. Up to now, the contact zone between the dura mater and the underlying leptomeninges has been considered a tight barrier.1,2 However, in the past year, research has changed this perspective. In 2023, a transcriptomics study was published in which five different fibroblast subtypes were identified across the meninges.3 Fibroblast subtype BFB5 expressing the gene Slc47a1 was exclusively associated with dural border cells, whereas BFB4 fibroblasts expressing Dpp4 were specific to the arachnoid barrier cells. The identification of these different patterns of gene expression can help to characterise CSF transport pathways.
CSF is mostly produced by the choroid plexuses in the cerebral ventricles and circulates in the subarachnoid space. From the subarachnoid space, the CSF can mix with brain interstitial fluid or undergo reabsorption into the systemic circulation. Reabsorption of CSF was previously assumed to occur directly from the subarachnoid space into the bloodstream via arachnoid granulations. However, this viewpoint changed over the past few years, when human MRI studies showed the dynamic passage of gadolinium-tagged tracers from the subarachnoid space into the parasagittal sinus of the dura4 and that arachnoid granulations touch but do not penetrate the dural venous sinuses,5 precluding a direct efflux of CSF into the bloodstream at this anatomical level.
At least two barriers shield the CNS: the first is the blood–brain barrier, which is formed by the endothelial cells of the brain; the second is the blood–CSF barrier, which comprises the choroid plexus and the arachnoid membrane—ie, the intermediate layer of the meninges that contains within it the circulating CSF. The outer perimeter of the subarachnoid space is the arachnoid membrane, which consists of an inner cell layer connected by adherens junctions and an outer continuous sheet of cells connected by tight junctions called the arachnoid barrier.
In Nature, Smyth and colleagues6 shed further light on CSF transport in the CNS and the cellular composition of the important meningeal blood barriers using a combination of genetic and imaging approaches in mice and MRI studies of the human brain. The authors first confirmed the earlier transcriptomics work, showing specific expression of Dpp4 in arachnoid barrier cells and Slc47a1 in dural border cells. Transgenic mouse lines were created, allowing detection of the expression of Dpp4 and Slc47a1 by production of a fluorescent signal exclusively in cells expressing these genes. This process allowed the authors to distinguish the arachnoid membrane from the dura mater, thereby allowing them to unambiguously characterise the contact zone of the arachnoid and dural membranes in vivo. Their findings showed that bridging veins, which drain cerebral blood into the dorsal dural sinus, had different cell coverage along their route towards the dural sinus. Initially, bridging veins are covered by arachnoid barrier cells and maintain blood–brain barrier properties; however, close to the dura, bridging veins lose the expression of arachnoid barrier cell markers, and the blood–brain barrier properties cease. Smyth and colleagues refer to the areas without expression of arachnoid barrier cell markers as arachnoid cuff exit (ACE) points. Through extensive analyses, the authors showed that tracers administered into CSF reached the dura exactly at the ACE points and could escape from there. Notably, not all ACE points appeared to vigorously transport CSF or tracer from the subarachnoid space to the dura, and transit through ACE points appears to be bidirectional. An experiment in a mouse model of autoimmune encephalomyelitis showed enhanced trafficking of immune cells mediated by laminin7 around ACE points and the leptomeninges, suggesting that these gateways might be exploited by myeloid and T cells entering the subarachnoid space in autoimmune and other infectious scenarios. To translate their mouse data to humans, Smyth and colleagues6 did MRI in ten healthy people using sequences that are sensitive to low levels of CSF contrast approximately 4 h after intravenous gadolinium administration. These results confirmed gadolinium signals around bridging veins and close by in the subarachnoid space.
The elegant work of Smyth and colleagues6 provides strong evidence that the tight arachnoid barrier cell membrane is remodelled at ACE points, which can serve for immune cell trafficking and as a gateway for CSF to exchange with dural interstitial fluid and, possibly, the neighbouring lymphatic vasculature. However, on the basis of the presented data, CSF transport was detected at only some of the ACE points of bridging veins, suggesting that this dorsal gateway might not be a major clearance pathway for CSF trafficking. It is highly likely that similar ACE points might exist at other cerebral veins near the skull base. Notably, approximately 30% of subdural haematomas are related to disruption of the bridging veins, especially in people with brain atrophy.8,9 A gap in knowledge exists on how bridging veins might shape cerebral pathology, including cerebral amyloid angiopathy. Crucially, this new work emphasising CSF-to-dura exchange via ACE points is conceptually prodigious for future investigations into understanding neurodegeneration and meningeal inflammatory processes.
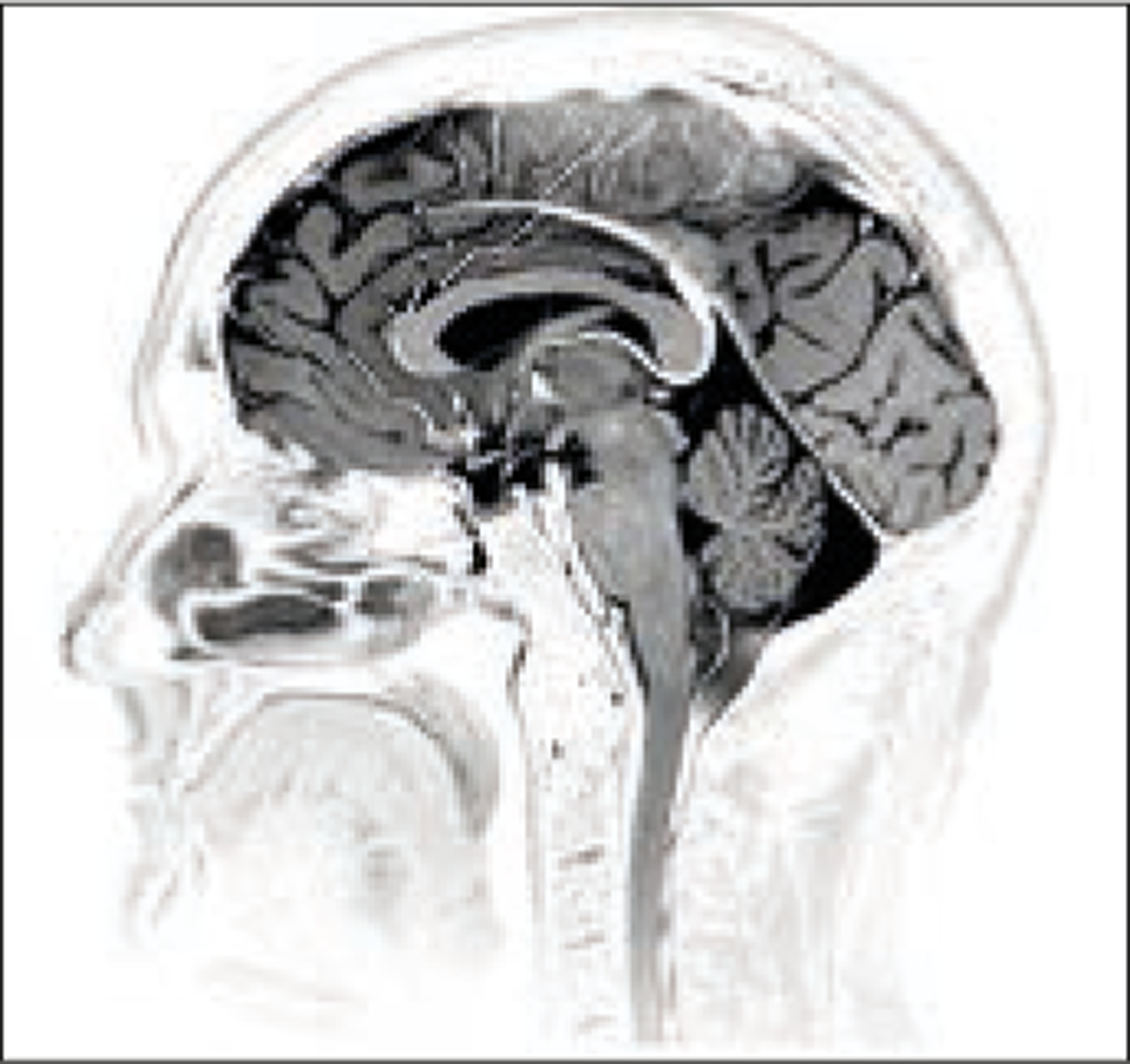
Living Art Enterprises/Science Photo Library
Acknowledgments
HB declares research grant support from the US National Institutes of Health, the Leducq Foundation, and Cure Alzheimer’s Fund. J-LT declares research grant support from the US National Institutes of Health and Monitoring Neuroinflammation supported by the Fonds Recherche Neurosciences.
Contributor Information
Helene Benveniste, Department of Anesthesiology, Yale School of Medicine, New Haven, CT 06519, USA; Department of Biomedical Engineering, Yale University, New Haven, CT, USA.
Jean-Leon Thomas, Department of Neurology, Yale School of Medicine, New Haven, CT 06519, USA; Paris Brain Institute, Université Pierre et Marie Curie Paris 06 UMRS1127, Sorbonne Université, Paris, France.
References
- 1.Nabeshima S, Reese TS, Landis DM, Brightman MW. Junctions in the meninges and marginal glia. J Comp Neurol 1975; 164: 127–69. [DOI] [PubMed] [Google Scholar]
- 2.Brochner CB, Holst CB, Mollgård K. Outer brain barriers in rat and human development. Front Neurosci 2015; 9: 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pietilä R, Del Gaudio F, He LQ, et al. Molecular anatomy of adult mouse leptomeninges. Neuron 2023; 111: 3745–64. [DOI] [PubMed] [Google Scholar]
- 4.Ringstad G, Eide PK. Cerebrospinal fluid tracer efflux to parasagittal dura in humans. Nat Commun 2020; 11: 354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah T, Leurgans SE, Mehta RI, et al. Arachnoid granulations are lymphatic conduits that communicate with bone marrow and dura-arachnoid stroma. J Exp Med 2022; 220: e20220618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smyth LCD, Xu D, Okar SV, et al. Identification of direct connections between the dura and the brain. Nature 2024; 627: 165–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yao H, Price TT, Cantelli G, et al. Leukaemia hijacks a neural mechanism to invade the central nervous system. Nature 2018; 560: 55–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller JD, Nader R. Acute subdural hematoma from bridging vein rupture: a potential mechanism for growth. J Neurosurg 2014; 120: 1378–84. [DOI] [PubMed] [Google Scholar]
- 9.Mortazavi MM, Denning M, Yalcin B, Shoja MM, Loukas M, Tubbs RS. The intracranial bridging veins: a comprehensive review of their history, anatomy, histology, pathology, and neurosurgical implications. Childs Nerv Syst 2013; 29: 1073–78. [DOI] [PubMed] [Google Scholar]


