Sepsis is a critical global health problem and one of the leading causes of mortality worldwide [1–5]. Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection [6]. It can lead to systemic inflammation, tissue injury, and ultimately organ dysfunction involving various system, which can progress to multi-organ failure and death [7,8]. Organ dysfunction in sepsis involves multiple complex mechanisms including hemodynamic instability and cellular dysfunction [9]. Early detection of organ dysfunction allows for the timely initiation of sepsis interventions, including fluid resuscitation, antimicrobial therapy, and necessary organ support, which can limit the further development of organ dysfunction [10–12]. Appropriate assessment of organ failure is also important for evaluating the severity of sepsis and monitoring the patient's response to treatment [9].
CLINICAL EVALUATION OF ORGAN FAILURE IN THE ED
In the emergency department (ED), clinicians must rely on a rapid, comprehensive clinical evaluation to suspect and identify organ dysfunction in sepsis patients. Vital signs such as hypotension and tachypnea are often the first indicators that prompt further management, as they suggest cardiovascular or respiratory compromise. Beyond vital signs, a focused physical examination is essential for detecting more specific signs of organ dysfunction. Signs such as altered mental status, poor peripheral perfusion (e.g., skin mottling or delayed capillary refill), myocardial dysfunction on echocardiography, decreased urine output, jaundice, bleeding tendencies, and ileus may raise suspicion for sepsis in patients with suspected infection (Fig. 1) [7,9].
Fig. 1.
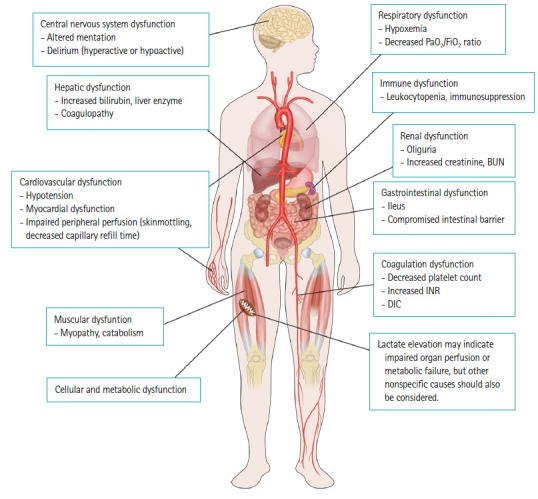
Sepsis-associated organ dysfunctions and signs. FiO2, fraction of inspired oxygen; BUN, blood urea nitrogen; INR, international normalized ratio; DIC, disseminated intravascular coagulation.
SOFA SCORE
The Sequential Organ Failure Assessment (SOFA) score was initially developed in 1994 by the Working Group of the European Society of Intensive Care Medicine during a consensus conference to objectively quantify the degree of organ dysfunction in intensive care unit (ICU) patients [13]. It assesses dysfunction across six essential organ systems: respiratory (PaO2 to fraction of inspired oxygen [FiO2] ratio), coagulation (platelet count), hepatic (bilirubin level), cardiovascular (mean arterial pressure, vasopressor and inotropic use), renal (creatinine and urine output), and central nervous system (Glasgow Coma Scale) function [14,15]. While the SOFA score was not originally designed to predict mortality, numerous studies have shown a significant correlation between higher SOFA scores and worse clinical outcomes [16–19]. Today, the SOFA score is widely used for assessing organ failure, prognostication, scientific research, and defining sepsis in both EDs and ICUs [6,15,17,18,20–26]. It is designed to be simple and easy to use, allowing for frequent reassessment of organ dysfunction over time. Its minimal number of variables makes it straightforward to compute with data that are readily available in most healthcare settings.
FUTURE PERSPECTIVES
While the SOFA score remains an important tool in assessing organ dysfunction, there may be a need for updates to better reflect recent advances and practices in critical care [14,19,27]. For instance, the SOFA score system does not incorporate certain aspects of current critical care practice. The Surviving Sepsis Campaign guidelines now recommend norepinephrine as the first-line vasopressor rather than dopamine, and vasopressin along with other agents have become more commonly used [11]. Additionally, extracorporeal membrane oxygenation (ECMO), cardiac assist devices, high-flow oxygen therapy, and noninvasive positive pressure ventilation are frequently used in managing critically ill patients. These aspects could be incorporated in the future update of the cardiovascular and respiratory SOFA components. Also, it would be helpful to develop strategies that allow for an alternative assessment of organ dysfunction based on clinical assessment or additional information in the ED (e.g., jaundice, oxygen saturation as measured by pulse oximetry [SpO2], and AVPU [alert, verbal, pain, unresponsive] system) [14,15,19,28]. Global collaborative efforts to collect and analyze large datasets from diverse clinical settings will be the first important step in developing a comprehensive and useful SOFA score update.
Assessment of organ failure in sepsis patients must begin as soon as they arrive in the ED. Early recognition, whether through clinical signs or scoring systems like SOFA, is crucial. Moving forward, the integration of more advanced and adaptable tools that combine clinical evaluation with real-time data analysis may offer even greater accuracy in identifying high-risk patients. Artificial Intelligence (AI) in sepsis care could aid sepsis identification, prediction of progression, phenotyping for personalized treatments, and clinical decision to prioritize interventions for those most likely to benefit [29,30]. In the future, AI could be further developed to create more advanced tools for assessing organ failure, improving the precision and speed of diagnostics and treatment strategies in sepsis.
Furthermore, beyond traditional organ failure assessments, future tools may incorporate cellular, metabolic, and immune markers of dysfunction [7,14,31]. Metabolic failure at the cellular level, such as impaired mitochondrial function, may provide early indicators of organ failure before clinical signs manifest. Currently, there are no widely implemented tools or markers for objective grading in clinical practice, but further research and development are essential, and these innovations could transform sepsis management.
Footnotes
Conflicts of interest
Tae Gun Shin is an Editorial Board member of Clinical and Experimental Emergency Medicine, but was not involved in the peer reviewer selection, evaluation, or decision process of this article. The author has no other conflicts of interest to declare.
Funding
The author received no financial support for this study.
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
REFERENCES
- 1.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–54. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 2.Fleischmann C, Scherag A, Adhikari NK, et al. Assessment of global incidence and mortality of hospital-treated sepsis: current estimates and limitations. Am J Respir Crit Care Med. 2016;193:259–72. doi: 10.1164/rccm.201504-0781OC. [DOI] [PubMed] [Google Scholar]
- 3.Stoller J, Halpin L, Weis M, et al. Epidemiology of severe sepsis: 2008-2012. J Crit Care. 2016;31:58–62. doi: 10.1016/j.jcrc.2015.09.034. [DOI] [PubMed] [Google Scholar]
- 4.Kadri SS, Rhee C, Strich JR, et al. Estimating ten-year trends in septic shock incidence and mortality in United States academic medical centers using clinical data. Chest. 2017;151:278–85. doi: 10.1016/j.chest.2016.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Namgung M, Ahn C, Park Y, Kwak IY, Lee J, Won M. Mortality among adult patients with sepsis and septic shock in Korea: a systematic review and meta-analysis. Clin Exp Emerg Med. 2023;10:157–71. doi: 10.15441/ceem.23.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:801–10. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gotts JE, Matthay MA. Sepsis: pathophysiology and clinical management. BMJ. 2016;353:i1585. doi: 10.1136/bmj.i1585. [DOI] [PubMed] [Google Scholar]
- 8.Mira JC, Gentile LF, Mathias BJ, et al. Sepsis pathophysiology, chronic critical illness, and persistent inflammation-immunosuppression and catabolism syndrome. Crit Care Med. 2017;45:253–62. doi: 10.1097/CCM.0000000000002074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lelubre C, Vincent JL. Mechanisms and treatment of organ failure in sepsis. Nat Rev Nephrol. 2018;14:417–27. doi: 10.1038/s41581-018-0005-7. [DOI] [PubMed] [Google Scholar]
- 10.Suh GJ, Shin TG, Kwon WY, et al. Hemodynamic management of septic shock: beyond the Surviving Sepsis Campaign guidelines. Clin Exp Emerg Med. 2023;10:255–64. doi: 10.15441/ceem.23.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47:1181–247. doi: 10.1007/s00134-021-06506-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369:840–51. doi: 10.1056/NEJMra1208623. [DOI] [PubMed] [Google Scholar]
- 13.Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–10. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 14.Moreno R, Rhodes A, Piquilloud L, et al. The Sequential Organ Failure Assessment (SOFA) Score: has the time come for an update? Crit Care. 2023;27:15. doi: 10.1186/s13054-022-04290-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lambden S, Laterre PF, Levy MM, Francois B. The SOFA score: development, utility and challenges of accurate assessment in clinical trials. Crit Care. 2019;23:374. doi: 10.1186/s13054-019-2663-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferreira FL, Bota DP, Bross A, Melot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286:1754–8. doi: 10.1001/jama.286.14.1754. [DOI] [PubMed] [Google Scholar]
- 17.Raith EP, Udy AA, Bailey M, et al. Prognostic accuracy of the SOFA Score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA. 2017;317:290–300. doi: 10.1001/jama.2016.20328. [DOI] [PubMed] [Google Scholar]
- 18.Jentzer JC, Bennett C, Wiley BM, et al. Predictive value of the Sequential Organ Failure Assessment Score for mortality in a contemporary cardiac intensive care unit population. J Am Heart Assoc. 2018;7:e008169. doi: 10.1161/JAHA.117.008169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee HJ, Ko BS, Ryoo SM, et al. Modified cardiovascular SOFA score in sepsis: development and internal and external validation. BMC Med. 2022;20:263. doi: 10.1186/s12916-022-02461-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nishimoto Y, Ohbe H, Matsui H, et al. Predictive ability of the sequential organ failure assessment score for in-hospital mortality in patients with cardiac critical illnesses: a nationwide observational study. Eur Heart J Acute Cardiovasc Care. 2022;11:312–21. doi: 10.1093/ehjacc/zuac011. [DOI] [PubMed] [Google Scholar]
- 21.Pellathy TP, Pinsky MR, Hravnak M. Intensive care unit scoring systems. Crit Care Nurse. 2021;41:54–64. doi: 10.4037/ccn2021613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schoe A, Bakhshi-Raiez F, de Keizer N, van Dissel JT, de Jonge E. Mortality prediction by SOFA score in ICU-patients after cardiac surgery; comparison with traditional prognostic-models. BMC Anesthesiol. 2020;20:65. doi: 10.1186/s12871-020-00975-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gupta T, Puskarich MA, DeVos E, et al. Sequential Organ Failure Assessment component score prediction of in-hospital mortality from sepsis. J Intensive Care Med. 2020;35:810–7. doi: 10.1177/0885066618795400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karakike E, Kyriazopoulou E, Tsangaris I, Routsi C, Vincent JL, Giamarellos-Bourboulis EJ. The early change of SOFA score as a prognostic marker of 28-day sepsis mortality: analysis through a derivation and a validation cohort. Crit Care. 2019;23:387. doi: 10.1186/s13054-019-2665-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jeong S. Scoring systems for the patients of intensive care unit. Acute Crit Care. 2018;33:102–4. doi: 10.4266/acc.2018.00185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cour M, Bresson D, Hernu R, Argaud L. SOFA score to assess the severity of the post-cardiac arrest syndrome. Resuscitation. 2016;102:110–5. doi: 10.1016/j.resuscitation.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 27.Bachmann KF, Arabi YM, Regli A, Starkopf J, Reintam Blaser A. Cardiovascular SOFA score may not reflect current practice. Intensive Care Med. 2022;48:119–20. doi: 10.1007/s00134-021-06536-6. [DOI] [PubMed] [Google Scholar]
- 28.Jeong D, Lee GT, Park JE, et al. Prognostic accuracy of SpO2-based respiratory Sequential Organ Failure Assessment for predicting in-hospital mortality. West J Emerg Med. 2023;24:1056–63. doi: 10.5811/westjem.59417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xu Z, Mao C, Su C, et al. Sepsis subphenotyping based on organ dysfunction trajectory. Crit Care. 2022;26:197. doi: 10.1186/s13054-022-04071-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yoon JH, Pinsky MR, Clermont G. Artificial intelligence in critical care medicine. Crit Care. 2022;26:75. doi: 10.1186/s13054-022-03915-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim K. Future of sepsis: perspective on diagnosis. Clin Exp Emerg Med. 2022;9:269–70. doi: 10.15441/ceem.22.392. [DOI] [PMC free article] [PubMed] [Google Scholar]


