Summary
Background
The WHO has highlighted that: “promotion of e-cigarettes has led to marked increases in e-cigarette use by children and adolescents.” The long-term neuropsychiatric and psychological consequences of substance abuse in adolescence is well recognised. Limited data exists on the adolescent burden of vaping-related nicotine addiction and behavioural and/or psychological dependence to guide pharmacological or behavioural interventions to stop electronic cigarette usage.
Methods
A self-administered brief electronic survey was provided to a large, sample of high school students from January to October 2023 in South Africa. Questions on vaping usage, initiation, reasons for continuation and indicators of physical and psychological dependence were asked. A mixed methods approach was used to obtain and analyse quantitative and qualitative responses.
Findings
25,149 students from 52 South Africa schools completed the survey. 45.8% identify as female, 51.7% male, 0.3% transgender, 2.1% do not identify with a gender. Current vaping was reported by 16.83% (95% CI: 16.47–17.30), with 36.71% reporting ever using a vaping product (95% CI: 26.06–37.36). The odds of vaping increased by grade but not with increasing school affluence. 47% vaped within the first hour of waking suggesting high nicotine addiction. Vaping initiation reasons of: ‘social influences’ and ‘curiosity’, changed significantly to ongoing motivations of: ‘enjoyment’, ‘managing mental distress’ and ‘addiction’ to nicotine. Paired quantitative/qualitative responses regarding stress and dependence showed inconsistencies at the individual student level.
Interpretation
Vaping in the schools surveyed was high and increased by grade but was not associated with school level affluence. Drivers for vaping initiation change significantly to persistence drivers with significant nicotine addiction. Adolescent perceptions (qualitative/quantitative) are frequently incongruent suggesting that mixed methods evaluations are required to understand individual level drivers of vaping. Urgent interventions tailored to this population are required. Nicotine addiction may require “off-label” pharmacotherapies alongside tailored behavioural interventions utilising the expressed concerns, psychological and dependence measures elicited from adolescents.
Funding
This study was funded in part by research grant from the Cambridge-Africa ALBORADA Research Fund G12753.
Keywords: Adolescent, Vaping addiction, Nicotine addiction, Mental health
Research in context.
Evidence before this study
Outside of high-income nations, the burden of vaping amongst high school students is largely unstudied. The tobacco and electronic cigarette industry are marketing vaping products globally, targeting youth in particular. Limited data exist as to the drivers of ongoing vaping amongst high school students, and the levels of nicotine addiction amongst adolescents who use electronic cigarettes.
Added value of this study
We provide an extensive survey (n >25,000) focusing on the burden and drivers of vaping among adolescents in South Africa. We show a high burden of addiction using a mixed methods approach and a novel addiction scoring algorithm, showing high levels of psychological distress and anxiety. We demonstrate that while most adolescents start vaping due to social influences a substantial number of adolescents continue to vape to cope with stress and anxiety and due to symptoms of dependency.
Implications of all the available evidence
Adolescent vaping is not restricted to high income countries and substantial burden of vaping exists in South African high school students. A tailored intervention addressing psychological/behavioural factors as well as “off label” pharmacological support for substantial vaping related nicotine addiction is likely needed to address the ongoing vaping health crisis and help adolescents to stop vaping.
Introduction
A recent 2023 World Health Organisation call to action has highlighted the concern that the promotion of e-cigarettes has led to a substantial rise in e-cigarette use by children and adolescents.1 In the USA, e-cigarette use amongst students in grades 6–12 has been declared ‘an epidemic’.2,3 Surveys from the UK indicate that 20.5% of children (aged 11–17) have tried vaping, and that 7.6% of children currently vape.4 Limited data from Asia and Africa exist but report similar figures of ranging from 3.3% to 11.8%.5,6 The widespread uptake of vaping by adolescents has ushered in a growing public health crisis.
Despite many unknowns around the long-term safety of e-cigarette use, the harms of nicotine to many organs are well documented.7, 8, 9 Adolescence represents a critical period of brain maturation, with ongoing myelination, cortical growth and synaptic pruning. Gradual and differential maturation of the limbic system and prefrontal cortex modulates reward, affective behaviour, and executive control. Substance use (SU) presents a challenge to neurodevelopment in this vulnerable stage of development. SU may impair young people's decision making and lower their inhibitions, leading to increased high-risk behaviours. In addition, long term neuropsychiatric and psychological disorders are well recognised as consequences of SU.10 Nicotine usage, not widely considered a SU disorder, has its own addictive properties and cognitive impacts such as poor memory and learning.11 Addictive behaviour or disorders are also associated with the development of mental illness, further fuelling the mental health challenges experienced by adolescents.10,12
The growing number of adolescent e-cigarette users globally should bring nicotine addiction amongst adolescents into the spotlight. While extensive research has informed the adoption of evidence-based approaches to support smoking cessation amongst adults,3 ‘vaping cessation’ in any age category is less well studied. Amongst adolescents (aged <18), for whom no pharmacotherapies have been approved to support nicotine withdrawal, there is no robust data. A recent Cochrane review13 reported no data available to support the adoption of strategies to support adolescent vaping cessation.
According to surveys conducted by the Centers for Disease Control (CDC) in the US and the Agency for Smoking and Health (ASH) in the UK, many adolescents start vaping for “fun”, “for the flavours” or “to join in/because a friend used them’’.4,14 These reasons speak to the initiation factors, but do not necessarily explain the reasons for continued vape use, nor reasons why adolescents may not be able to stop vaping. Data from the UK indicates that ∼30% of adolescents have strong/extremely strong urges to vape, while research from the US indicates that 20% of high school e-cigarette users vape within 30 min of waking. These behaviours are indicative of nicotine addiction. Additionally, psychological distress has been found to be a prominent feature amongst people who vape.3,15,16
For a ‘vaping cessation’ strategy to be successful, the balance of behavioural interventions (based on an understanding of the underlying reasons for continuation) and nicotine withdrawal support (based on managing the commonly reported physical and psychological symptoms) should be informed by the vaping behaviours of adolescents. Globally, data exploring why adolescents start and continue vaping is limited. Data on the degree of their addiction, and the role played by psychological distress (e.g. anxiety, depression) as potential drivers of addiction, is similarly sparse. As a result, little is known about the kind of behavioural support adolescents need to aid them in stopping e-cigarette use.
We administered a survey among South African high school students (grades 8–12) to investigate the burden of e-cigarette use, extent of nicotine dependence, and the mental health and social stressors associated with ongoing vaping.
Methods
This cross-sectional study was designed to document the extent of the burden of vaping amongst a large sample of high school students in South Africa. The sample frame was largely restricted to schools in major centres (see below), as well as schools identified through the National Department of Education website, and the National School Associations network to ensure variability in school-type by fees paid (both low and high fee schools) and the gender of students accommodated at the sampled schools (both single sex and co-education schools). The schools included in the study were from major centres such as Johannesburg, Pretoria, Cape Town, Durban, smaller centres such as Gqeberha, Bloemfontein, Pietermaritzburg, East London etc. Schools in outlying rural areas were not included in the study apart from Rural private boarding schools.
In South African Schools are divided into 5 fee paying Quintiles. The Quintile brackets define how much financial support the Department of Education provides to the school. Quintiles 1 & 2 are non-fee-paying schools and quintiles 3–5 are fee paying schools. In our cohort all schools are in lower Governmental financial support quintiles, but school fees ranging from around R20,000 per annum to over R300,000 per annum (as reported on the individual school website). The median fee paid amongst the school in our sample is R 60,650 (interquartile range: R 70,185; coefficient of variation: 0.8961). To differentiate school fees and by proxy financial status of students' families, schools were divided into three groups. High income schools were defined as those with school fees of over ZAR90,000/year (n = 16), mean (SD) school fee ZAR185,831 (88,417). Medium income schools were defined as school fees ranging from ZAR40,000 per year to ZAR90,000 per year (n = 25), mean (SD) school fee ZAR56,338 (10,114). Lower income schools were defined as schools with a school fee of less than ZAR40,000 per year (n = 13), mean (SD) school fee ZAR27,975 (8385). The school fees were statistically significantly different (p < 0.0001) and represent an almost doubling of fees in each group. The high-income school bracket had greater variability in school fee with a range of over ZAR257,000 as some schools are boarding only schools. Although approached –it was not possible to include schools in rural areas without easy internet access and/or computer labs thus the lowest bracket of “non-fee-paying schools” are not represented in this survey. This was further limited due as no budget was available to provide internet access and devices to schools with which to complete the survey.
Ninety schools across South Africa were contacted with the request to participate in the research study and administer the survey on e-cigarette use to students in grades 7/8–12. Sixteen schools indicated they could not participate (no Wi-Fi, too busy, not interested). Six schools did not respond beyond the primary contact. Two additional school governing bodies refused permission, and 12 were prepared to participate but did not run the survey before the end of year closing date. The schools participating in the study came from 8 of nine provinces in South Africa. All data were self-entered electronically by the participants using a school specific link to a questionnaire programmed in SurveyMonkey. Students either completed the survey using their own device (mobile phone/tablet) or on a school computer.
For analysis, student observations from each school were appended to form a single cross-sectional data set. Overall, the survey was administered to students in 54 schools over a 12-month period in 2022–2023. Grade 7 students from 3 separate schools were not included in this manuscript.
The focus of this study was primarily on grade 8–12 students. 25,699 students provided the minimum data threshold to be included. 241 grade 7 students including 2 schools with only grade 7 learners, were further excluded to only include grade 8–12 students in this analysis of ‘high school’ students. Formal data cleaning identified entries that were highly incongruent (e.g. age 13 reported but responded to being in grade 12), and fictitious (e.g. reported daily/7 days a week use of all products: vape, smoke, use cannabis and hookah) or fanciful responses (e.g. foul/abusive language with incongruent answers throughout survey) to free text answers leaving a total of 52 individual schools and 25,149 valid responses for data analysis.
Our sample consists of 25,149 high-school students from 52 schools. Based on the reported number of learners present at school during the survey, the overall response rate by school was 82.4% with 97.3% valid responses provided.
Ethics
Permission to conduct the survey was provided by the South African Department of Basic Education, the Provincial Departments of Basic Education, school principals, and the school's governing body/board. Ethics approval was provided by the University of Cape Town Faculty of Health Sciences Human Research Ethics Committee (UCTHREC 248/2022).
The identity of the participant was protected by using anonymised entry into the database. No personal identifiers apart from age, gender and school grade were captured, and the identity of the school was coded to prevent any identification of the school participating. Participation in the survey was completely voluntary and explained prior to their participation in the survey. An informed consent explanation preceded the first data entry page of the survey, especially explaining that personal and information regarding substance usage would be asked. Encouragement to seek help if any of the questions raised concerns with the students was provided at the completion of the survey. The “opt-in” continuation for participation in the survey after the informed consent page, as well as the waiver of parental/guardian consent for this electronic survey in minors was formally approved by the University of Cape Town Faculty of Health Sciences Human Research Ethics Committee.
Our survey asked all students about their basic demographic information (gender, age, grade) and their use of four products in the 30-days preceding the survey: e-cigarettes, tobacco cigarettes, cannabis and hookah pipe. All students were also presented with three 10-point Likert scales that were used to evaluate: (1) students’ ability to concentrate while studying; (2) how stressed they feel about school/life; and (3) how harmful they believe vaping is relative to tobacco use. Questions asked to all students were informed by existing literature17 which shows variation in current vape use by demographic traits, physiological distress, and perceptions around the harm of using e-cigarettes relative to tobacco cigarettes.
Given our primary focus on vaping, students who indicated that they currently vape were asked additional questions about their vaping history and use patterns. They were further asked to provide yes/no responses to questions regarding their use of nicotine vapes, their need to vape during the school day, and their experience of symptoms suggestive of nicotine addiction. Students were further asked about their reasons for starting to vape, and their reasons for continuing to vape. The operationalization of survey responses for our analysis is described in the Online Supplement.
Our dataset includes four parameters of primary interest in this study:
Vape use: a binary indicator set equal to one if the student indicated that they used an e-cigarette on at least one day in the 30 days preceding the survey and set equal to zero if they did not.
Reasons for starting to vape: Responses for reasons for initiating vaping were adapted from the US National Youth Tobacco Survey (NYTS) questionnaire.18
Reasons for continuing to vape: open-ended responses to the question “Why do you continue to vape?”
Measures of addiction: The Fagerström Test for Nicotine Dependence (FTND) has not been applied to, nor validated for adolescent vaping. Our study evaluates two novel composite scores for adolescent vaping-related nicotine dependence. The first score includes the number of vaping days each week and time from waking to first vape use. The second score additionally incorporates nicotine withdrawal symptoms (Online Supplement).
Statistics
A minimum of 51 schools with a projected sample size of 18,031 students was needed to provide a sample powered to detect a relative 10% difference in incidence by sub-group of interest at an incidence rate of 15.5% (estimated by our initial pilot feasibility phase) across multiple comparisons. The initial feasibility pilot was conducted at 12 high schools located in three provinces before expanding the survey to schools across the country.
Our analysis follows a mixed methods approach in three steps. First, we ran a quantitative analysis that comprised both descriptive statistics for the full sample, and multilevel logistic regression analysis. Given the discrete/categorical nature of our analysis variables (Online Supplement), the descriptive analysis presents counts and proportions in each group (Logit 95% CIs are reported). Chi–Square tests inform preliminary assessments of differences in vape use across the analysis variables.
The regressions examined the association between student and school-level attributes and the odds of vape use. Predictors included age, grade, gender, students' self-reported feelings of stress (‘stress’), ability to concentrate while studying (‘concentration’), and perceptions around the harms of vaping relative to cigarettes (‘perception of e-cigarettes'), as well as annual school fees (as a proxy for socioeconomic status). e adopted a multilevel logistic regression model with students nested within schools to analyse the association between these factors and the odds of vape use. A likelihood ratio test determined the appropriateness of the multi-level regression framework with random intercepts at the school level over a non-hierarchical logistic regression (p < 0.0001). Age is treated as continuous in the regressions. The linearity assumption underlying the multilevel logistic regression model for this predictor was validated using a Box–Tidwell test.19
For the analysis, predictors were grouped into four categories: demographics (age, grade and gender), physiological factors (stress and concentration), perception of e-cigarettes and school-fee brackets. The association between each of these groups of predictors and the odds of vape use were investigated using a stepwise approach involving four model specifications. Model 1 assesses the relationship between students’ demographic characteristics (age, grade and gender) and the odds of e-cigarette use. Model 2 includes students' self-reported feelings of stress and ability to concentrate while studying—in addition to controls used for in model 1. Model 3 adds students' perceptions around the harms of vaping relative to cigarettes to model 2. Our full model, Model 4, adds the school-level characteristic ‘fee bracket’ as a proxy for income to model 3 and thus controls for all parameters of interest. Likelihood ratio tests were used to compare the fit of these alternate model specifications.
No random coefficients were added to any of our models since we do not believe that any of our independent variables have a varying effect on vape use across schools. We validated this assumption through a series of likelihood ratio tests that compare model 4, which has random intercepts at the school level and no random coefficients, to iterative versions of model 4 with a random slope, assuming normal distribution, for grade, gender and cognitive traits, respectively.
Of the 24,894 students who provided information on their current vape use, 16.52% (n = 4114) have missing data on at least one of the predictors (Online Supplement Table S1). To assess the robustness of results based on complete cases in the full model (N = 20,780), we applied multiple imputation using chained equations (m = 20) (Online Supplement). The next phase of our analysis only uses responses from students who currently vape. First, we used our composite scores for adolescent vaping-related nicotine dependence to calculate the proportion of current vape users whose vaping behaviour indicates vaping dependence. We then ran a qualitative data analysis of students’ open-ended responses to gain insights into motives for starting and continuing to vape. The analysis consisted of the following steps: a) familiarisation with the data, b) developing an initial code frame which was revised throughout the initial coding phase, c) SK and AvdB applied the code frame independently to the whole dataset, to then d) identify latent themes20 from the codes. Intercoder reliability between AvdB and SK was good (Kappa = 0.816, CI: 0.800–0.828). We then used the qualitative themes and mapped them onto the adapted response options of the US NYTS.18 The NYTS allows for comparison between populations but its relevance to South African youth has not been formally evaluated.
Lastly, we combined qualitative and quantitative analysis for those students who vape by comparing the responses that they provided in the qualitative survey regarding their decision to start vaping, and their reasons for continuing to vape, to their self-reported levels of stress, and their implied vaping dependency scores.
Role of the funding source
The funders of this study had no role in the study design, data collection, analysis nor manuscript preparation.
Results
Our sample includes 25,149 high school students (grades 8–12) from 52 schools (Online Supplement), with a median response rate of 82.4% of students present at the school on the day of the survey.
Participant demographics
Grades 8–11 each compromise about 22% of the sample, while grade 12 represents 13%. Of the 24,953 students who provided information on their gender, 45.88% (n = 11,448) identify as female, and 51.72% (n = 12,906) identify as male, 2.06% (n = 515) did not identify as male or female and 0.34% (n = 84 identified as transgender) (Table 1). Most students (69.1%) in our sample attend a single-sex school. 18.7% of students attended schools with high annual fees, 64.2% of students attended mid-fee schools, and 17.1% of students attended lower-fee schools (Table 2).
Table 1.
Demographics of participants in vaping survey.
| N (%) | 95% CI | |
|---|---|---|
| School grade | 25,149 | |
| Grade 8 | 5719 (22.74) | [22.23–23.26] |
| Grade 9 | 5521 (21.95) | [21.45–22.47] |
| Grade 10 | 5400 (21.47) | [20.97–21.98] |
| Grade 11 | 5303 (21.09) | [20.59–21.59] |
| Grade 12 | 3206 (12.75) | [12.34–13.17] |
| Age | 25,149 | |
| 13 years old | 1195 (4.75) | [4.50–5.02] |
| 14 years old | 5430 (21.59) | [21.09–22.10] |
| 15 years old | 5566 (22.13) | [21.62–22.65] |
| 16 years old | 5527 (21.98) | [21.47–22.49] |
| 17 years old | 4961 (19.73) | [19.24–20.22] |
| 18 years old | 2400 (9.54) | [9.19–9.91] |
| 19 years old | 70 (0.28) | [0.22–0.35] |
| Gender | 24,953 | |
| Female | 11,448 (45.88) | [45.26–46.50] |
| Male | 12,906 (51.72) | [51.10–52.34] |
| Transgender | 84 (0.34) | [0.27–0.42] |
| Don't identify | 515 (2.06) | [1.89–2.25] |
| Ever vape useb | 21,121 | |
| Ever vaped | 7753 (36.71) | [36.06–37.36] |
| Any product usagea | 25,141 | |
| Uses any product | 4875 (19.39) | [18.91–19.88] |
| Current vape use | 24,894 | |
| Uses electronic cigarette | 4189 (16.83) | [16.37–17.30] |
| Current vape use: start age | 3032 | |
| 8 years-old or younger | 55 (1.81) | [1.40–2.36] |
| 9 years-old | 11 (0.36) | [0.20–0.65] |
| 10 years-old | 26 (0.86) | [0.58–1.26] |
| 11 years-old | 36 (1.19) | [0.86–1.64] |
| 12 years-old | 123 (4.06) | [3.41–4.82] |
| 13 years-old | 426 (14.05) | [12.86–15.33] |
| 14 years-old | 775 (25.56) | [24.04–27.15] |
| 15 years-old | 698 (23.02) | [21.56–24.55] |
| 16 years-old | 562 (18.54) | [17.19–19.96] |
| 17 years-old | 240 (7.92) | [7.01–8.93] |
| 18 years or older | 80 (2.64) | [2.12–3.27] |
| Tobacco cigarette use | 24,852 | |
| Uses tobacco | 517 (2.08) | [1.91–2.27] |
| Hookah use | 24,808 | |
| Uses hookah | 785 (3.16) | [2.95–3.39] |
| Cannabis use | 24,823 | |
| Uses cannabis | 1274 (5.13) | [4.86–5.41] |
N indicates number of total responses to specific question.
Has used vapes, tobacco, cannabis, or hookah on more than one day in the past 30 days.
Student has used an electronic cigarette at least once in their life.
Table 2.
School-level attributes.
| N (%) | 95% CI | |
|---|---|---|
| School fees | 25,149 | |
| Lower annual fees (fees >R90,000 per annum) | 4312 (17.15) | [16.68–17.62] |
| Mid-range annual fees (R 40,000 per annum < fees R90,000 per annum) | 16,145 (64.20) | [63.60–64.79] |
| Higher annual fees (fees R40,000 per annum) | 4692 (18.66) | [18.18–19.14] |
| School type | 25,149 | |
| All-boys school | 10,227 (40.67) | [40.06–41.27] |
| All-girls school | 7152 (28.44) | [27.88–29.00] |
| Co-ed school | 7770 (30.90) | [30.33–31.47] |
| Province | 25,149 | |
| Eastern Cape | 4895 (19.46) | [18.98–19.96] |
| Free State | 629 (2.50) | [2.32–2.70] |
| Gauteng | 6307 (25.08) | [24.55–25.62] |
| Kwa-Zulu Natal | 2207 (8.78) | [8.43–9.13] |
| Limpopo | 424 (1.69) | [1.53–1.85] |
| Mpumalanga | 321 (1.28) | [1.14–1.42] |
| Northern Cape | 550 (2.19) | [2.01–2.38] |
| Western Cape | 9816 (39.03) | [38.43–39.64] |
Substance use
In the past 30 days, 19.39% of respondents (4875/25,141; 95% CI: 18.91–19.88) used any inhaled/tobacco product (tobacco cigarettes, cannabis, e-cigarettes, or hookah pipe) (Online Supplement Table S1). Current vaping was reported by 16.83% (4189/24,898; 95% CI: 16.37–17.30) with 36.71% (7753/21,121; 95% CI: 36.06–37.36) having ever tried a vaping product. Tobacco cigarette use in the past 30-days was reported by 2.08% (517/24,852; 95% CI: 1.91–2.27), cannabis use was reported by 5.13% (1274/24,823; 95% CI: 4.86–5.41); and hookah pipe use by 3.16% (785/24,808; 95% CI: 2.95–3.39) (Online Supplement Table S2). Vape use was reported by 17.82% (95% CI: 17.16–18.49) of students who identify as male, by 15.33% (95% CI: 14.68–16.00) of students who identify as female (p < 0.0001), and by 18.52% (95% CI: 11.48–28.48) of students who identify as transgender (Online Supplement Figure S2).
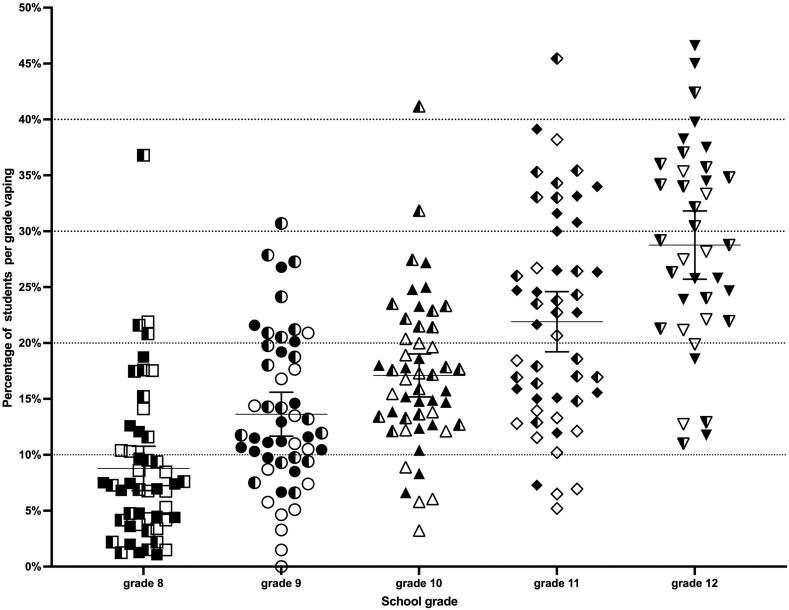
Vaping rates varied significantly by grade and schools (Fig. 1). Vaping increased with grade (p < 0.0001), from 8.47% (95% CI: 7.77–9.22) in grade 8–29.51% (95% CI: 27.94–31.13) in grade 12. Vaping among grade 8 students ranged from 1.07% to 36.80% across schools, and grade 12 vaping from 11% to 46.6%. The mean vaping rate across schools was 15.82% (95% CI: 14.80–18.30) ranging from 4.16% (95% CI: 2.67–6.43) to 31.00% (95% CI: 22.72–40.70). Tobacco, cannabis and hookah use, varied widely by school (Online Supplement Figure S1). E-cigarette use was highest amongst lower-fee schools at 19.49% (95% CI: 18.33–20.71); and lowest at 14.61% (95% CI: 13.63–15.66) amongst high-fee paying schools (p < 0.0001). The proportion of students that vape at mid-fee schools was 16.76% (95% CI: 16.19–17.35) (Online Supplement Figure S3). E-cigarette use ranged from 13.35% to 17.87% across provinces (Online Supplement).
Fig. 1.
Frequency of reported vaping across individual schools by grade. Each point represents an individual school: solid symbol = boys' school, clear symbol = girls' school, half-shaded symbol = co-ed school. Horizontal line depicts mean with 95% Confidence Interval bars depicted. Grade 8: mean 8.47% (482/5692; 95% CI: 7.77–9.22); grade 9: mean 13.32% (730/5481; 95% CI: 12.44–14.24); grade 10 mean: 17.28% (921/5329; 95% CI: 16.29–18.32); grade 11: mean 21.51% (1130/5254; 95% CI: 20.42–22.64); grade 12: mean 29.51% (926/3138; 95% CI: 27.94–31.13).
Cognitive factors and perceptions of the harms of vaping
Of 20,925 students, 79.57% (95% CI: 79.02–80.12) reported no difficulty concentrating while studying (Online Supplement Table S2). Among the 2818 students who currently vape that also provided an indication of their ability to concentrate while studying, 28.64% (95% CI: 27.00–30.34) reported a below-average ability to concentrate. Of the 21,429 students who provided a rating of their feelings of stress about school/life, 38.60% (95% CI: 37.95–39.25) indicated feeling above average levels of stress (Online Supplement Table S2). Among the 2894 students who currently use e-cigarettes that also provided an indication of their feelings of stress about school/life, 1115 (38.53%, 95% CI: 36.77–40.32) reported above-average levels of stress.
A total of 21,429 students rated the harmfulness of vaping relative to tobacco. Among these students, 1825 (8.52%, 95% CI: 8.15–8.90) perceived the harms of vaping as low, 7608 (35.50%, 95% CI: 34.87–36.15) rated the harms as moderate, while 11,996 students (55.98%, 95% CI: 55.31–56.64) considered the harms of vaping to be high relative to tobacco (Online Supplement Table S2).
Multivariable predictors of vape use
The full set of model results shown in Table 3 are discussed in the Online Supplement. From the full model (Table 3: Model 4), results indicate that the odds of vape use significantly increase with age (OR = 1.18, 95% CI: 1.08–1.29). Additionally, compared to students in grade 8, the odds of vape use rise significantly and monotonically with each grade level (grade 9: OR = 1.31, 95% CI: 1.10–1.56, grade 10: OR = 1.53, 95% CI: 1.22–1.93, grade 11: OR = 1.72, 95% CI: 1.28–2.32, grade 12: OR = 2.40, 95% CI: 1.65–3.51). Gender identity does not show a significant association with vaping odds, nor does stress. Conversely, students reporting above-average concentration abilities have lower odds of vaping (OR = 0.76, 95% CI: 0.69–0.84).
Table 3.
Regression results analysis of predictors of electronic cigarette usage using 4 stepwise models.
| Model 1a (demographics only—complete cases) |
Model 1b (demographics only—restricted samplea) |
Model 2 (demographics + stress and concentrate) |
Model 3 (Model 2+ perceived harms of vape use added) |
Model 4 (Model 3 + school-fee bracket) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N = 24,706 |
N = 20,780 |
N = 20,780 |
N = 20,780 |
N = 20,780 |
||||||
| OR [95% CI] | p-value | OR [95% CI] | p-value | OR [95% CI] | p-value | OR [95% CI] | p-value | OR [95% CI] | p-value | |
| Age (in years) | 1.30 [1.21–1.40] | <0.0001 | 1.23 [1.13–1.34] | <0.0001 | 1.22 [1.12–1.33] | <0.0001 | 1.19 [1.09–1.29] | 0.00016 | 1.18 [1.08–1.29] | 0.00019 |
| Grade (base = grade 8) | ||||||||||
| Grade 9 | 1.28 [1.11–1.47] | 0.00083 | 1.38 [1.17–1.64] | 0.00019 | 1.37 [1.15–1.62] | 0.00030 | 1.31 [1.10–1.56] | 0.0025 | 1.31 [1.10–1.56] | 0.0023 |
| Grade 10 | 1.37 [1.14–1.65] | 0.00082 | 1.56 [1.25–1.95] | <0.0001 | 1.55 [1.24–1.93] | 0.00010 | 1.53 [1.22–1.92] | 0.00025 | 1.53 [1.22–1.93] | 0.00022 |
| Grade 11 | 1.43 [1.12–1.82] | 0.0039 | 1.66 [1.25–2.22] | 0.0053 | 1.67 [1.25–2.22] | 0.00048 | 1.71 [1.27–2.31] | 0.00038 | 1.72 [1.28–2.32] | 0.00032 |
| Grade 12 | 1.71 [1.26–2.32] | 0.00063 | 2.20 [1.52–3.17] | <0.0001 | 2.22 [1.54–3.20] | <0.0001 | 2.38 [1.63–3.47] | <0.0001 | 2.40 [1.65–3.51] | <0.0001 |
| Gender (base = male) | ||||||||||
| Female | 0.91 [0.82–1.01] | 0.091 | 0.93 [0.82–1.06] | 0.28 | 0.940 [0.83–1.07] | 0.35 | 0.97 [0.85–1.11] | 0.68 | 0.96 [0.84–1.10] | 0.53 |
| Transgender | 1.08 [0.60–1.94] | 0.80 | 1.19 [0.59–2.42] | 0.62 | 1.14 [0.56–2.32] | 0.71 | 1.02 [0.49–2.13] | 0.96 | 1.01 [0.48–2.12] | 0.97 |
| Does not identify with a gender | 1.27 [1.01–1.59] | 0.038 | 1.32 [1.00–1.73] | 0.047 | 1.25 [0.95–1.64] | 0.11 | 1.18 [0.89–1.57] | 0.25 | 1.17 [0.88–1.55] | 0.28 |
| Cognitive factors | ||||||||||
| Above-average ability to concentrate (base = below-average ability to concentrate) | – | – | – | – | 0.63 [0.57–0.69] | <0.0001 | 0.76 [0.69–0.84] | <0.0001 | 0.76 [0.69–0.84] | <0.0001 |
| Above-average levels of stress (base = below-average levels of stress) | – | – | – | – | 0.97 [0.89–1.06] | 0.48 | 0.94 [0.86–1.03] | 0.20 | 0.94 [0.86–1.03] | 0.20 |
| Perceived harms of vape use relative to tobacco (base = relative to tobacco vaping is harmless) | ||||||||||
| Moderate perceived harm of vaping | – | – | – | – | – | – | 0.65 [0.57–0.74] | <0.0001 | 0.65 [0.57–0.74] | <0.0001 |
| High perceived harm of vaping | – | – | – | – | – | – | 0.16 [0.14–0.19] | <0.0001 | 0.16 [0.14–0.19] | <0.0001 |
| School fee brackets (base = high-fee schools) | ||||||||||
| Mid-range fee schools | – | – | – | – | – | – | – | – | 0.91 [0.65–1.26] | 0.57 |
| Low-range fee schools | – | – | – | – | – | – | – | – | 1.38 [0.94–2.04] | 0.10 |
| Residual intra class correlation [95% CI] | 0.055 [0.04–0.08] | 0.060 [0.04–0.09] | 0.058 [0.04–0.09] | 0.074 [0.05–0.11] | 0.064 [0.04–0.10] | |||||
| Model fit assessment | ||||||||||
| Log likelihood | −10545.20 | −7777.44 | −7735.18 | −7206.58 | −7203.64 | |||||
| Likelihood ratio test comparing current with previous model: χ2 (df) = likelihood ratio chi-square statistic (p-value) | – | – | χ2(2) = 84.51 (p < 0.0001) |
χ2(2) = 1057.21 (p < 0.0001) |
χ2(2) = 5.88 (p = 0.053) |
|||||
“–” indicates that the variable was not included in this version of the model specification.
Model 1b uses the same predictors as Model 1a but restricts the sample size to those 20 780 observations that have complete data on the predictor variables used in all other models (Models 2–4). Model 1b was estimated to enable a Likelihood–Ratio test to compare different model specifications across equal sample sizes.
Perceptions of the harm associated with vaping are significantly associated with current vape use. The odds of vape use are lower amongst students who perceive vaping as having moderate harm (OR = 0.65, 95% CI: 0.57–0.74) and amongst those who view vaping as highly harmful (OR = 0.16, 95% CI: 0.14–0.19), compared to learners who perceive it as relatively harmless. At the school-level, fee bracket is not significantly associated with the odds of vape use. Results displayed here use complete case analysis. The analysis deploying multiple imputation yields similar results (Online Supplement Table S3).
Indicators of addiction amongst students who vape
Among the 4189 students who indicated that they vape, the use of nicotine containing e-cigarettes was reported by 88.12% (95% CI: 86.67–89.43) of students. 47% vape within the first hour of waking. Daily vaping was reported by 38.34% (95% CI: 36.61–40.09) of students. More than half of these students (1647/2997, 5495%) report that they vape 4 or more days per week (Online Supplement Table S5). 1184% (95% CI: 1045–1339) of students indicated that they cannot get through the school day without vaping, and 24.89% (95% CI: 2285–2705) indicated that waiting a long time before they can vape makes them feel anxious or angry (Online Supplement Table S4).
Two novel composite scores for adolescent vaping dependence were evaluated, based on the FTND which, to date has not been applied or validated for adolescent vaping nicotine addiction (Online Supplement). Both scores indicate high levels of dependency. Dependence Score 1 (DS1) accounts for the number of vaping days each week and the time from waking to vaping and ranges between 2 (lowest level of dependence) and 10 (highest level of dependence), shows that 58.44% (95% CI: 55.56–61.27) student vape users are highly vape-dependent (DS1 > 6). Using Dependence Score 2, which supplements DS1 with students’ self-reported need for vaping during school and feelings of anxiety/anger when prevented from vaping, 60.70% (95% CI: 57.40–64.42) of vape users exhibit high vape dependence with score above the mid-point score of 7.5 (Online Supplement Table S5).
Qualitative responses on reasons for vaping initiation and continuation
Just over half (50.6%) of the 4189 students who vape cited social influences (family/friends, peer pressure, the need to fit in) as reasons for starting. 19.6% indicated they started to cope with stress and anxiety, 16.2% due to general curiosity and 4.4% specifically due to flavours.
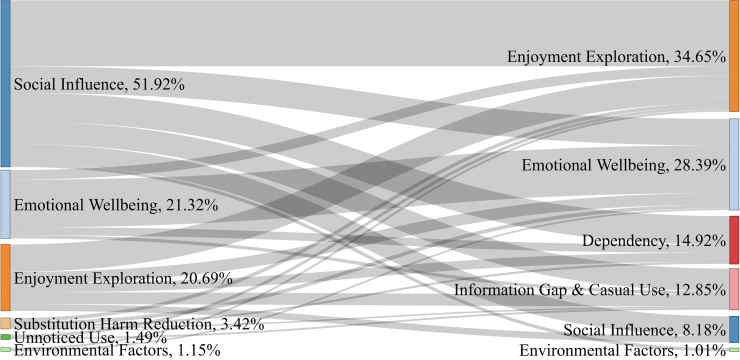
Eight themes for continued vaping were identified from 2432 responses (Online Supplement Figure S4) 33.1%, cited enjoyment, taste, and exploration as reasons, with 5.1% specifically mentioning flavours. Emotional wellbeing (coping, anxiety, mental health) was cited by 27.6%. Dependency as a reason for continued vaping was cited by 16.2%. Some explicitly stated addiction: “It's an addiction, no matter what I try I can't stop” (female, 17), while others describe it more as a habit: “It has become a habit. I have to consume something constantly” (female, 18). Less than 10% of students identified social influences as the reason why they continue to vape and only 16 adolescents (0.7%) indicated that they use vapes to substitute cigarettes and to reduce other harms. Fig. 2 shows how reasons for vaping initiation and continuation differ. For instance, 1078 students started due to social influences (51.92%), while 443 indicate emotional wellbeing as main reason for initiation (21.32%). From the students who started due to social influences, 185 (17.16%) continue due to dependency. Similarly, 52 out of those adolescents who started vaping for emotional wellbeing reasons, developed dependency (11.72%). 23.21% of students indicated they did not wish to stop vaping, 40.3% were currently interested in stopping and the remainder (36.47%) indicated they ‘don't know’ if they want to stop.
Fig. 2.
Sankey plot representing thematic reasons for initiating vaping transitioning to reasons for continuing to vape in high school leaners currently vaping (n = 2077).
Mixed methods analysis of qualitative and quantitative responses relating to vaping dependence
Of 1139 students who provided quantitative and qualitative information on their vaping behaviour, 49.43% provided qualitative responses that matched their primary self-reported vaping behaviour used in the construction of DS1. Specifically, 12.73% of these students listed addiction as reason for continuing to vape and reported vaping behaviour that indicates a high-level of addiction (DS1 >6); while 36.70% of students did not list and congruently reported vaping behaviour that indicates lower levels of addiction (DS1 <6) (Table 4). However, 45.74% of students did not list dependence/addiction as a reason for continuing to vape, but self-reported vaping behaviour that exhibits high levels of vape dependency (DS1 >6) (Table 4). Inconsistencies in students’ qualitative and behaviour-based responses remain with Dependence Score 2 (Online Supplement Table S6).
Table 4.
Comparison of students’ qualitative indication of vaping dependence as a reason for continued vaping and their level of vaping dependence based on self-reported vaping behaviour (Vaping DS1) (N = 1139).
| Qualitative (reason for continuing) | Quantitative (vaping dependence score—DS1) | Count (%) | Comment |
|---|---|---|---|
| Dependence/addiction listed as a reason for continuing | High dependence (DS1 score >6) | 145 (12.73%) | Congruent qualitative reported dependence and quantitative dependence score. |
| Dependence/addiction NOT listed as a reason for continuing | High dependence (DS1 score >6) | 521 (45.74%) | Incongruent qualitative reported low nicotine dependence but high quantitative dependence score. |
| Dependence/addiction NOT listed as a reason for continuing | Low dependence (DS1 score <6) | 418 (36.70%) | Congruent qualitative low reported nicotine dependence and low quantitative dependence score. |
| Dependence/addiction listed as a reason for continuing | Low dependence (DS1 score <6) | 55 (4.83%) | Incongruent high qualitative nicotine dependence with low quantitative nicotine dependence score. |
Discussion
This survey of over 25,000 South African adolescents is the first to investigate the burden of electronic cigarette use amongst high school learners in the country. In our sample, 16.8% of high school students reported that they vape. This is substantially higher than the vaping prevalence of 2.2% reported amongst adults (aged ≥15) in the country's 2021 Global Adult Tobacco Survey21 and the prevalence estimate of 2.5% among a cohort of 15–19 year-olds reported in the country's 2016 Demographic and Health Survey.22 The highest frequency of vaping reported by any school grades in our sample were 45.5% for a grade 11 year, and 46.6% for a grade 12 year. We had a median response rate of 82.4% across the schools surveyed, and showed great variability in burden, thus high burden cannot simply be assumed in every school. Furthermore, schools with very low or no-school-fee were not included in our study, limiting our ability to understand the potential burden of vaping amongst the lowest socio-economic bracket. These data do however highlight the public health crisis unfolding in many of the country's high schools.
The burden of vaping was not higher in more affluent schools merely based on access and affordability, as was expected when initiating this study. It is likely that our lowest school fee (R20,000 per annum) paying school is above the threshold where poverty and a very low socio-economics bracket would impact on access to ‘relatively’ more expensive vaping products. The burden of vaping across affluent schools varied even amongst similar schools within a city the size of Cape Town. Explorative evaluations of language, community, school policies etc. did not reveal any clear explanations for the variability and require more detailed research to understand why similar schools have vastly different reported vaping burden.
Results showed that the primary reasons for vaping initiation differ substantially from the dominant reasons for ongoing vaping. Adolescents predominantly start vaping out of curiosity, or because of social influences, but continue vaping as a coping strategy for anxiety/depression/stress, to relax or because they are addicted. The responses to the qualitative/mixed methods analysis had fewer respondents given the need to have answered multiple questions. Careful evaluation of the reasons expressed for continued vape use, and the markers of nicotine addiction that reflect the need pharmacological therapy to prevent withdrawal, are required to tailor an effective strategy to help adolescents to stop vaping.
The evaluation of nicotine addiction in adult smokers is primarily evaluated using the FTND, which has also been validated for use in adolescent (14–20 years) smokers.23 However, to the best of our knowledge no nicotine (tobacco smoking) dependence tests have been formally evaluated in adolescent e-cigarette users. The USA NYTS uses cravings as a proxy for nicotine addiction and found that 27.1% of high school students have had cravings in the past month and that 21.8% students vape within 30 min of waking.18 The UK's ASH survey reported that 29% of UK adolescents had ‘strong to extremely strong urges’ to smoke.4 In our sample, nearly half of student e-cigarette users vape within the first hour of waking and our composite dependence scores suggest that close on 60% of students are highly addicted. These levels of “dependence” reflect both chemical (nicotine) and behavioural (compulsion) elements of addiction and need to be better understood and explored to inform intervention strategies with and without pharmacological support for nicotine withdrawal. Our novel score used common simple questions that incorporate both behaviour and potential withdrawal symptoms to overcome the FTND applicability to adolescent vaping but requires validation with respect to it predictive need for pharmacotherapy in assisting adolescents to stop vaping.
Our results also showed that a considerable proportion of students (∼46%) do not qualitatively identify addiction as a reason why they continue to vape, despite that they exhibit behaviour of someone who is ‘highly addicted’ (high quantitative scores). This suggests a lack of awareness about what constitutes addiction. Consistent with research from surveys conducted in the USA,18 UK,4 and Canada,16 high levels of psychological distress are also evident in the quantitative and qualitative evaluations of students who vape, with some inconsistencies suggesting students may not be fully aware of the connection between their nicotine use and levels of distress. The discordance between reporting the presence of behavioural withdrawal symptoms, such as the need to vape soon after waking up and the self-reporting of addiction to vaping is an interesting inconsistency that warrants further exploration in future studies. Studies using qualitative methodologies such as in-depth interviews could explore whether the inconsistency is based on lack of education about addiction, is the awareness of the inconsistency conscious and how the students are resolving this cognitive dissonance.
In this study we did not conduct focus groups nor individual interviews which are likely to be needed to further explore the interplay of the aspects of addiction, both chemical and psychological, the role that nicotine plays and the role of social stressors, engagement and personal perceptions of addiction and coping. Furthermore, the lower numbers of participants answering in sufficient detail for our mixed-methods analysis will necessitate further studies.
Prevention is critical to prevent the uptake of vaping amongst adolescents. Many programmes have been developed to address this issue. Along with education on tobacco, alcohol and narcotics drugs. Basic education around the harms of vaping will be important, and the multivariate model suggests that lack of belief in the harms of vaping is associated with active vaping. It is likely that these preventative interventions will need to be implemented in younger grades given the early age of onset of usage. However, interventions for the initiators and drivers of persistent vaping are likely more pressing, given the levels of addiction and expressed emotional distress reported by respondents in our sample. In-depth interviewing/focus groups may be required to fully understand the interplay between distress/addiction and mental health as drivers of vaping continuation. To understand the relationship between nicotine use and anxiety and depression would require well designed longitudinal studies, as the current study is cross-sectional and therefore the direction of the relationship between the two is not answered here. Our findings indicate that interventions to engage the large proportion of vaping high school students will require a targeted nicotine addiction support strategy alongside psychological and behavioural support to address the challenges faced by adolescent vapers.
There are currently limited studies on the efficacy of strategies to address adolescent vaping. A recent Cochrane review concluded that no robust data meeting their RCT criteria had been published but other non-randomised data may assist in guiding interventions.13 A recent RCT conducted in the US shows an encouraging 37% self-reported abstinence rate at 7 months using a text messaging intervention amongst adolescent vapers.24 It is unclear how much of our knowledge around adult tobacco smoking interventions translates to adolescent vaping. Our findings suggest that, in the context of addressing adolescent vaping specifically, behaviour/addiction/mental health/social influences need to be clearly defined to develop evidence-based interventions. There is no validated tool to define nicotine addiction/dependence amongst adolescent vapers. No pharmacological therapies are licensed for use in under 18-year-olds, and any behavioural/cognitive interventions are currently inferred from adult smoking or adolescent substance (non-nicotine) usage. In many contexts, nicotine is often not considered a “substance use disorder”.
The high burden of vaping amongst high school students requires urgent intervention but with limited research on the most effective and evidence-based strategies to assist students break free from the nicotine addiction and manage their daily life stressors in a less harmful way. Additionally, engagement with an intervention requires identification of vaping amongst adolescents attending for health care, acknowledgement of addiction in ‘healthy’ adolescents vaping and adherence to any intervention such as patches or oral withdrawal medications.25 Thus, a pragmatic intervention is likely required, extrapolating from adult or adolescent tobacco addiction principles and adapting them as adolescent-specific vaping data is gathered. This approach ensures that interventions consider both inherent similarities and the unique differences of adolescents. Accurate identification of nicotine dependence will be needed to guide “off-label” pharmacotherapies in this age group, and our proposed nicotine dependence scoring framework may assist in this process.
This study has several limitations. The inherent nature of an online survey although providing large numbers of responses, lacks the ability to corroborate and validate individual responses. The study may have both an incidence-prevalence bias in addition to unmeasured confounders and reverse causality. Additionally, selection bias towards schools with higher prevalence of vaping is possible given the non-probability sampling strategy. Minor entry inconsistencies are likely to have limited impact given the large sample size, and data cleaning excluded clearly implausible/impossible answers. The survey was designed to be brief, self-administered using a personal device, and to have limited impact on school activities to increase acceptability to school management. While some respondents indicated that they started vaping because of stress, the association of nicotine usage and mental health distress needs further study to understand any causal link and the direction of such causality if present. Furthermore, the psychological construct of stress was not formally measured using validated scales. We used a one question Likert scale thereby limiting conclusions regarding its potential relationship with vaping. It unfortunately was not accessible to schools without on-site internet access, which will induce a socioeconomic bias by not included the lowest socioeconomic groups within our country The brief (5–7 min) survey lacks the details and depth of responses such as of choice of products, advertising exposure etc. like the (45 min) USA NYTS.
This study focused on specifically on the burden of vaping amongst high school students and the associated addiction and mental health aspects. Comparisons with published data are additionally limited by the various study sampling strategies, particularly age groups and a lack of global data on youth e-cigarette use. Previous data on tobacco and vaping in South Africa excluded all private/non-government schools which are included in our cohort and make trends in tobacco use difficult to evaluate. Validation of our nicotine dependence score was not undertaken in this sample but presented rather with comparisons of two scores and the relationship with qualitative responses regarding addiction.
E-cigarette use is high among adolescents in South African high schools. Social influence and curiosity as initiating influences are quickly replaced by enjoyment/pleasure, emotional wellbeing and nicotine addiction in continued adolescent vaping. Data is needed on measures of nicotine dependence and their predictors for need of pharmacological support to successfully stop vaping. Addressing vaping amongst adolescents will require education on harms of vaping, the nature and extent of nicotine addiction, as well as tailored evidence based behavioural interventions based on the expressed concerns, psychological and dependence measures elicited from adolescents. Off-label pharmacological interventions may be needed given the high levels of apparent nicotine addiction.
Contributors
RNvZS: Conceptualization, Methodology, Software, Validation, Formal Analysis, Investigation, Resources, Data Curation, Writing—Original Draft, Writing—Review & Editing, Visualization, Supervision, Project administration, Funding Acquisition.
SF: Conceptualization, Methodology, Software, Validation, Formal Analysis, Investigation, Data Curation, Writing—Original Draft, Writing—Review & Editing, Visualization.
GS: Conceptualization, Methodology, Software, Investigation, Data Curation, Writing—Review & Editing.
JH: Conceptualization, Methodology, Writing—Review & Editing.
AvDB: Validation, Formal Analysis.
SK: Conceptualization, Methodology, Software, Validation, Formal Analysis, Writing—Original Draft, Writing—Review & Editing, Visualization, Supervision, Funding Acquisition.
RNvZS, SF and SK have verified the underlying data.
All authors have read and approved the final version of the manuscript.
Data sharing statement
Data collected from this study are from minors, collected with permission from the South African Government Department of Basic Education (DOE) and under the supervision of the University of Cape Town Faculty of Health Sciences Huma Research Ethics committee (UCT FHS HREC). Data collection forms, and the data dictionary, will be provided on request. Access to the anonymised data will require permission from both the DOE and UCT FHS HREC as the research was conducted with minors, within the educational environment and consent was only provided for the aims listed in the original study protocol provided aims.
Declaration of interests
No authors declare any conflicts of interest relating to this manuscript. No authors have any relationship with the tobacco or electronic cigarette industry. RNvZS reports r Payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Aspen, Pfizer, Astra-Zeneca, Novartis, Cipla, MSD, J&J, Glenmark, Boehringer Ingelheim, Macloeds, Sanofi, Sandoz, and consulting fees from Macloeds Pharmaceutical outside of this study.
Acknowledgements
We are grateful to the schools and participants who agreed to participate in this study.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2024.102970.
Appendix A. Supplementary data
References
- 1.World Health Organisation . 2023. Urgent action needed to protect children and prevent the uptake of e-cigarettes. [Google Scholar]
- 2.Cullen K.A., Gentzke A.S., Sawdey M.D., et al. E-cigarette use among youth in the United States, 2019. JAMA. 2019;322(21):2095–2103. doi: 10.1001/jama.2019.18387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Owotomo O., Walley S. The youth e-cigarette epidemic: updates and review of devices, epidemiology and regulation. Curr Probl Pediatr Adolesc Health Care. 2022;52(6) doi: 10.1016/j.cppeds.2022.101200. [DOI] [PubMed] [Google Scholar]
- 4.Action on Smoking and Heatlh (ASH) 2023. Use of e-cigarettes (vapes) among young people in Great Britain. [Google Scholar]
- 5.Stone E., Evison M., van Zyl-Smit R.N., Andarini S., Shah S., Vandeleur M. Recreational vaping ban in Australia-policy failure or masterstroke? Lancet. 2024;404(10452):504–506. doi: 10.1016/S0140-6736(23)02298-5. [DOI] [PubMed] [Google Scholar]
- 6.Jane Ling M.Y., Abdul Halim A.F.N., Ahmad D., Ahmad N., Safian N., Mohammed Nawi A. Prevalence and associated factors of E-Cigarette use among adolescents in Southeast Asia: a systematic review. Int J Environ Res Public Health. 2023;20(5):3883. doi: 10.3390/ijerph20053883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benowitz N.L. Nicotine addiction. N Engl J Med. 2010;362(24):2295–2303. doi: 10.1056/NEJMra0809890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benowitz N.L. Clinical pharmacology of nicotine: implications for understanding, preventing, and treating tobacco addiction. Clin Pharmacol Ther. 2008;83(4):531–541. doi: 10.1038/clpt.2008.3. [DOI] [PubMed] [Google Scholar]
- 9.Benowitz N.L. Clinical pharmacology of nicotine. Annu Rev Med. 1986;37:21–32. doi: 10.1146/annurev.me.37.020186.000321. [DOI] [PubMed] [Google Scholar]
- 10.Steinfeld M.R., Torregrossa M.M. Consequences of adolescent drug use. Transl Psychiatry. 2023;13(1):313. doi: 10.1038/s41398-023-02590-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goriounova N.A., Mansvelder H.D. Short- and long-term consequences of nicotine exposure during adolescence for prefrontal cortex neuronal network function. Cold Spring Harb Perspect Med. 2012;2(12) doi: 10.1101/cshperspect.a012120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gunnell D., Kidger J., Elvidge H. Adolescent mental health in crisis. BMJ. 2018;361 doi: 10.1136/bmj.k2608. [DOI] [PubMed] [Google Scholar]
- 13.Barnes C., Turon H., McCrabb S., et al. Interventions to prevent or cease electronic cigarette use in children and adolescents. Cochrane Database Syst Rev. 2023;11(11) doi: 10.1002/14651858.CD015511.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gentzke A.S., Wang T.W., Jamal A., et al. Tobacco product use among middle and high school students - United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(50):1881–1888. doi: 10.15585/mmwr.mm6950a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Soin G., Filby S., van Zyl Smit R.N. The nature and extent of vaping and tobacco use amongst SouthAfrican high school learners. Am J Respir Crit Care Med. 2023;207:A2611–A. [Google Scholar]
- 16.To T., Borkhoff C.M., Chow C.-W., et al. E-cigarette use and quality of life in young adults: a Canadian health measure survey study. Eur Respir J. 2023;62(suppl 67) [Google Scholar]
- 17.Han G., Son H. A systematic review of socio-ecological factors influencing current e-cigarette use among adolescents and young adults. Addict Behav. 2022;135 doi: 10.1016/j.addbeh.2022.107425. [DOI] [PubMed] [Google Scholar]
- 18.Centre for Disease control National youth tobacco survey 2023. https://www.cdc.gov/tobacco/data_statistics/surveys/nyts/data/index.html
- 19.Box G.E.P., Tidwell P.W. Transformation of the independent variables. Technometrics. 1962;4(4):531–550. [Google Scholar]
- 20.Kiger M.E., Varpio L. Thematic analysis of qualitative data: AMEE Guide No. 131. Med Teach. 2020;42(8):846–854. doi: 10.1080/0142159X.2020.1755030. [DOI] [PubMed] [Google Scholar]
- 21.Council SAMR . 2022. Global adult tobacco survey. [Google Scholar]
- 22.National Department of Health (NDoH) South Africa Demographic and Health Survey 2016; Pretoria, South Africa: 2019. Statistics South Africa (stats SA), South African medical research council (SAMRC), ICF. [Google Scholar]
- 23.Carpenter M.J., Baker N.L., Gray K.M., Upadhyaya H.P. Assessment of nicotine dependence among adolescent and young adult smokers: a comparison of measures. Addict Behav. 2010;35(11):977–982. doi: 10.1016/j.addbeh.2010.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Graham A.L., Cha S., Jacobs M.A., et al. A vaping cessation text message program for adolescent E-cigarette users: a randomized clinical trial. JAMA. 2024;332(9):713–721. doi: 10.1001/jama.2024.11057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dai H.D., Hanh P., Guenzel N., Morgan M., Kerns E., Winickoff J.P. Adoption of vaping cessation methods by US adolescent E-cigarette users. Pediatrics. 2023;152(5) doi: 10.1542/peds.2023-062948. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.