Abstract
This is a novel case of idiopathic chylopericardium and chylothorax in a young male who had no significant medical history. He first presented with dyspnea due to idiopathic chylopericardium, which was refractory to medical and surgical treatments, including a medium-chain triglyceride diet, octreotide, and video-assisted pericardial window. The chylopericardium persisted and progressed to concomitant left-sided chylothorax. He subsequently underwent multiple imaging studies, including lymphoscintigraphy and an intranodal lymphangiogram, both of which confirmed leakage in the thoracic duct. Finally, thoracic duct embolization was performed via a retrograde transvenous approach, which was successful, with good results. Although idiopathic chylopericardium and chylothorax are extremely rare, it can greatly impact patient quality of life if left undiagnosed and untreated. While surgery can relieve cardiac tamponade, lymphatic imaging and intervention are key in diagnosing and treating the root cause of the condition. This case highlights the importance of multidisciplinary efforts in managing rare cases and how interventional radiology is a minimally invasive but effective way to treat thoracic duct leakage. Retrograde thoracic duct embolization is technically challenging but safe and effective.
Keywords: Chylopericardium, Chylothorax, Thoracic duct leakage, Lymphoscintigraphy, Intranodal lymphangiogram, Thoracic duct embolization, Retrograde
Background
Chylopericardium and chylothorax are conditions characterized by the accumulation of chyle in the pericardial and pleural cavities, respectively. Chyle accumulation is resultant of the damage to or obstruction of the thoracic duct due to trauma, malignancies, infections or iatrogenic disease; it is extremely rare for the condition to be idiopathic. The authors present a case of idiopathic chylopericardium and chylothorax that was difficult to diagnose and manage but was successfully treated with a multidisciplinary approach involving minimally invasive interventions.
Case presentation
A 26-year-old man with no significant medical history presented with dyspnea and was found to have chylopericardium. The patient was recently diagnosed with COVID-19 but initially misdiagnosed with viral pericarditis and inflammation related to pericardial effusion. Pericardiocentesis yielded chyle. He was put on a medium-chain triglyceride diet and prescribed a short course of octreotide, both of which failed. Cardiothoracic surgeons then created a pericardial window using video-assisted techniques. However, the chylopericardium persisted, and he developed high-output chylothorax refractory to pleurodesis.
Imaging findings
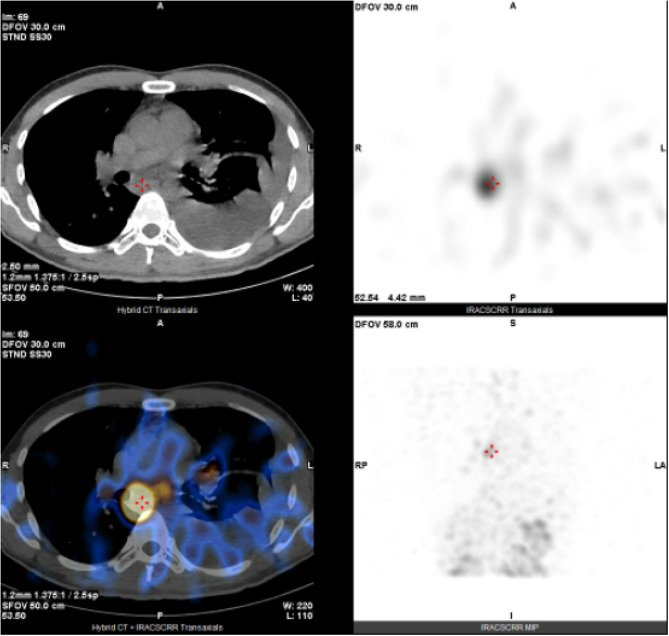
The patient underwent lymphoscintigraphy and single-photon emission computed tomography (SPECT) and computed tomography (CT) fusion imaging. Technetium-99 m sulfur colloid activity was detected in the pericardial and left pleural cavities 6 h after the scan, and dynamic images of the thorax revealed an accumulation of radiotracers in the posterior mediastinum at the mid-thoracic level 8 h thereafter (Fig. 1). The findings suggested thoracic duct leakage.
Fig. 1.
Lymphoscintigraphy with SPECT/CT revealed an accumulation of radiotracers in the posterior mediastinum at the T6 level, as well as in the pericardial and left pleural cavities, suggesting thoracic duct leakage causing chylopericardium and chylothorax
Eleven milliliters of lipiodol was injected in to the lymphatic system via a node in the right side of the groin for an intranodal lymphangiogram. The intra-abdominal lymphatics (Fig. 2) up to the lymphovenous junction became opaque. An abnormal accumulation of lipiodol was noted in the mediastinum at the mid-thoracic level, corresponding to the location previously pinpointed by lymphoscintigraphy. This was later confirmed on a plain CT scan (Fig. 3), which also revealed the collection of lipiodol in the pericardial and left pleural cavities.
Fig. 2.

The intra-abdominal lymphatics were delineated via an intranodal lymphangiogram performed by injecting lipiodol through a groin node. The intra-abdominal lymphatics must be opacified to identify the presence and location of the cisterna chyli in case of a future need for puncture, as well as to detect any intra-abdominal lymphatic leaks
Fig. 3.
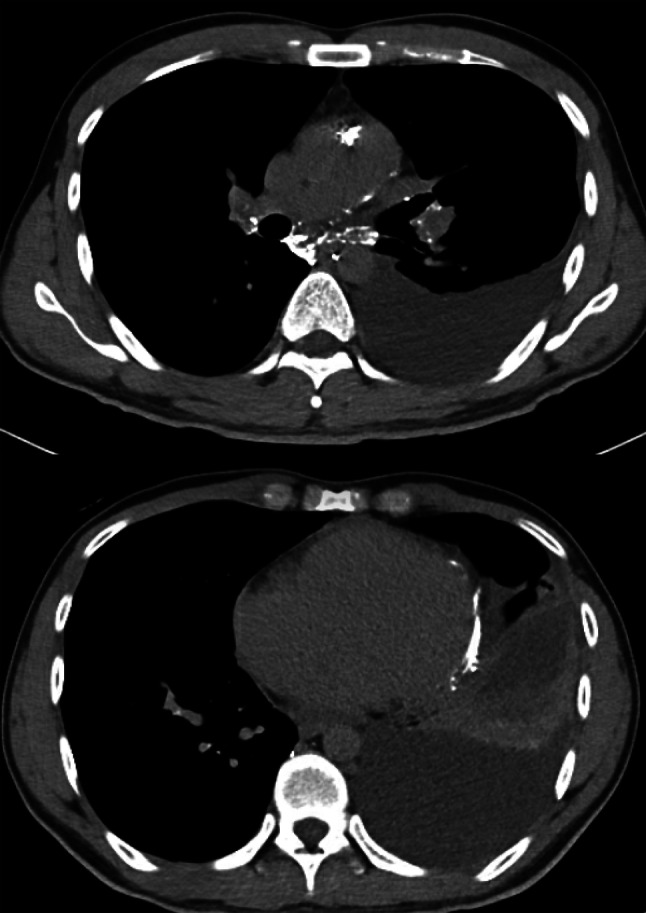
Axial plain CT image of the patient’s thorax after intranodal lymphangiogram, showing an abnormal accumulation of lipiodol in the posterior mediastinum paraesophageal region at the T6 level. An accumulation of lipiodol was observed in the pericardial cavity, confirming chylopericardium
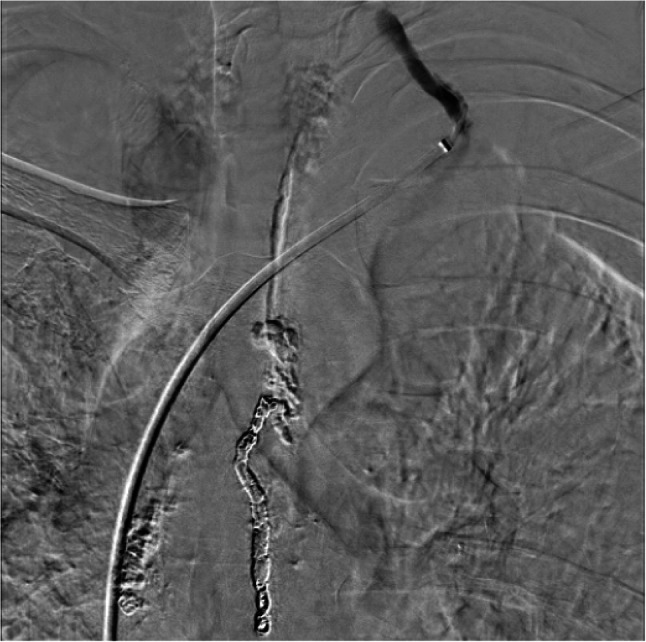
This patient was referred for interventional radiology. Retrograde thoracic duct cannulation and embolization were performed. An 8Fr sheath was inserted into the right common femoral vein, and a 5Fr H1 catheter (Cordis, U.S.) was inserted into the left clavicular region, supported by a NeuronMax-088 catheter (Penumbra, U.S.). The lymphovenous junction was well visualized on ultrasound of the neck, the location of which was indicated with an opaque marker. We successfully cannulated the thoracic duct ostium under the guidance of fluoroscopy and advanced an Excelsior 1018 microcatheter (Stryker, U.S.) over a 0.018” Glidewire GT microguidewire (Terumo, Japan). A thoracic ductogram clearly delineated the leakage point. We were then able to manipulate our microsystem across the leakage site and embolize it with 16 detachable Target Nano coils (Stryker, U.S.) ranging from 3 to 5 mm in diameter (Fig. 4), followed by 33% histoacryl glue in a lipiodol mixture. A post-embolization thoracic ductogram revealed successful obliteration of the leakage (Fig. 5, 6).
Fig. 4.
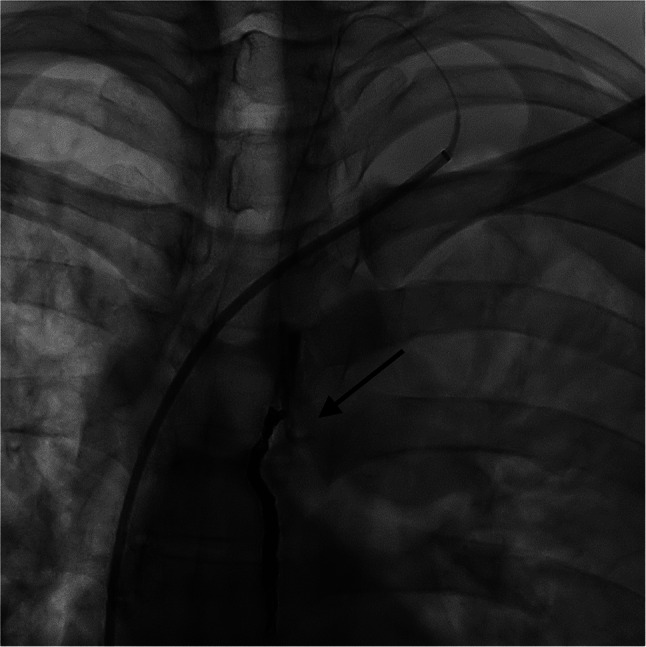
Coil embolization of the thoracic duct caudal to the leakage point (arrow)
Fig. 5.
Post-embolization thoracic ductogram showing complete obliteration of the leak
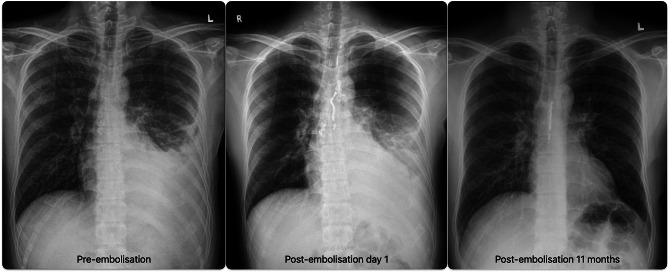
Fig. 6.
From left to right: pre-embolization, post-embolization day 1 and post-embolization 11-month chest radiographs showing immediate post-procedure resolution of the chylothorax, with good post-embolization results
There were no procedure-related complications. The patient was discharged on post-embolization day 5 after a normal chest radiograph and complete symptom resolution. Follow-up examinations were performed at 1, 3, 5, and 11 months after the procedure in the outpatient clinic, at which time the patient’s clinical condition, serial chest radiographs and interval CT scans of the thorax were assessed, all of which revealed good post-embolization results.
Discussion and conclusions
Chylopericardium is a rare pathological condition [1], and idiopathic thoracic duct leakage causing reflux into the pericardial cavity is even rarer. Only 10% of chylothorax cases are idiopathic. In our case, the patient had a history of COVID-19 prior to presentation, although it is unclear whether this contributed to his case of chylopericardium. There has been one report of a case of idiopathic chylopericardium in a patient postulated to be in a prothrombotic state due to COVID-19, leading to venous congestion and lymphatic pressure buildup [2]. These uncommonly observed conditions can be difficult to diagnose and treat but can be potentially life-threatening due to severe malnutrition and disruption of the immune system. This case is an accurate account of a series of investigations that helped diagnose and formulate a treatment plan. Compared with novel minimally invasive lymphatic interventions, traditional open thoracic duct ligation after failed dietary therapy and pleurodesis is invasive and may be a less attractive option [3]. Thoracic duct embolization is associated with a lower risk of morbidity and better clinical success than both conservative and surgical management in traumatic and nontraumatic cases of chylothorax [4]. Moreover, thoracic duct embolization may be the preferred option for patients with a complex thoracic duct anatomy, such as the plexiform type.
While cisterna chyli puncture and antegrade thoracic duct cannulation remain the primary approaches for embolization, there is a risk of transecting important intra-abdominal structures, including the small bowel, colon and aorta. In most cases of antegrade thoracic duct embolization, the liver is inadvertently punctured. Retrograde thoracic duct cannulation and embolization can be technically challenging but is safe and equally effective. A literature review in 2024 [5] revealed that the success rates of cannulation and lymphatic leakage embolization were 73.6% and 80.0%, respectively; the clinical success rate was 75.0%, and the complication rate was 2.8% (thoracic valve injury).
The origin of the thoracic duct may be difficult to identify, and one must advance a microcatheter and guidewire into an invisible thoracic duct through a valve at the ostium [6]. One technique involves identifying the lymphovenous junction on ultrasound and marking the area with an opaque pointer, which aids fluoroscopic cannulation. If the retrograde approach is used, the cannula must be advanced past the leakage point to seal both the “front” and “back doors” of the leak, as plugging the venous side of the leak cannot solve the problem. Moreover, it is important to exclude the coexistence of intra-abdominal chyle leaks because retrograde thoracic duct embolization in these patients could lead to worsening of chylous ascites.
While retrograde thoracic duct embolization is safe and effective, it may not be the standard of care in institutions that do not specialize in lymphatic interventions. Multidisciplinary discussion is therefore imperative for the successful management of these rare cases of lymphatic leakage.
Acknowledgements
Nil.
Author contributions
RKM was the primary interventionist in this case, and was the major contributor in writing the manuscript. The manuscript was supervised and edited by HSF. All authors read and approved the final manuscript.
Funding
No funding was obtained for this case report.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
The local institutional review board (IRB) at the participating institution does not require approval for the type of research being performed.
Consent for publication
Consent for publication has been obtained from the patient.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rochefort M. Review of chylopericardium. Mediastinum. 2022. 10.21037/med-20-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garg R. A Fat Lot nothing. A case of idiopathic chylopericardium. Journal of the American College of Cardiology 2024, Apr; 83(13 Supplement); 10.1016/S0735-1097(24)06025-X
- 3.Itkin M. Lymphatic Intervention is a New Frontier of IR. J Vasc Interv Radiol. 2014;25(9):1404–5. 10.1016/j.jvir.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Nadolski G, Itkin M. Thoracic duct embolisation for the management of chylothorax. Curr Opin Pulm Med. 2013;19(4):380–6. 10.1097/MCP.0b013e3283610df2. [DOI] [PubMed] [Google Scholar]
- 5.Kinoshita G, Morisaki K, Okamoto D, et al. R etrograde transvenous thoracic duct embolization for lymphatic leakage after retroperitoneal tumor and lymph node resection: a case report and literature review. Surg case Rep. 2024;10:53. 10.1186/s40792-024-01856-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lymphatic Intervention for Various Types of Lymphorrhea, Inoue M, et al. Access and Treatment. Radiographics. 2016. 10.1148/rg.2016160053. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.