Abstract
On October 7, 2023, a large-scale attack in southern Israel and the subsequent war resulted in extensive loss of life and injuries, with many individuals experiencing traumatic losses, such as family members or close friends being killed or kidnapped. This study aims to longitudinally examine its effects on mental health, specifically, clinical symptoms of anxiety, depression, and posttraumatic stress disorder (PTSD). We anticipated greater symptom severity among individuals who experienced traumatic loss, were forcibly displaced, or suffered income loss, as well as among women and members of ethnic minorities. This three-wave online survey study assessed mental health symptoms in a sample of 1052 individuals, aged 18–40, residing in conflict zones in Israel from February 2024 (day 1), through March 2024 (day 30), to May 2024 (day 90). Symptoms of anxiety, depression, and PTSD were measured using the Generalized Anxiety Disorder-7 (GAD-7), Patient Health Questionnaire-9 (PHQ-9), and Primary Care PTSD Screen (PC-PTSD). Individuals experiencing traumatic losses, forced displacement, or economic hardships, as well as females, consistently demonstrated higher rates of anxiety, depression, and PTSD symptoms compared to those without such experiences or to males, across all time points (F values ranged from 17.7 to 215.3, p < .001). For ethnic minorities (Arab and other), as compared to Jewish, anxiety and depression symptoms were higher at every time point (F = 8.3–97.1, p = .004 to < .001). This study highlights the urgent need for targeted mental health interventions in conflict zones, particularly for affected individuals. Further research should expand these findings to broader populations.
Keywords: War, Terrorist attack, Anxiety, Depression, PTSD, Gender, Displacement
Subject terms: Psychology, Health care
Introduction
On October 7, 2023, a series of violent events led to significant casualties and displacement in Israel, with over 1000 individuals reported deceased and 251 taken captive1,2. Subsequent incidents along the northern border contributed to further civilian displacement, affecting approximately 100,000 individuals. Overall, the conflict has displaced between 200,000 and 500,000 people within Israel, leading to instability and difficulties in returning home3,4. These events have also resulted in economic challenges, including job losses and increased living expenses for those impacted. This study aims to assess the psychological and social consequences for those residing in conflict-affected areas. While this study focuses exclusively on the mental health and socioeconomic effects experienced by individuals in Israel, it acknowledges that this is only one aspect of a broader, multifaceted conflict.
Previous studies on the mental health effects of terrorist attacks have focused on directly exposed individuals, particularly those close to the events, such as New Yorkers during the September 11 terrorist attack5,6. Immediate proximity to traumatic events significantly increases the risk of developing serious mental health conditions, including posttraumatic stress disorder (PTSD), depression, and anxiety5–11. Traumatic and sudden loss of a loved one can contribute to prolonged periods of sorrow, symptoms of major depression, and uncomplicated or complicated grief12. Forced displacement often induces acute stress and anxiety, and feelings of insecurity and instability, which may worsen or precipitate mental health issues13. Financial burdens due to job or income loss can produce feelings of helplessness. Such ongoing stress exacerbates the risk of developing conditions such as depression and anxiety14. Each of these stressors can amplify the severity of existing psychopathology and increase the likelihood of new conditions, impairing mental health and well-being.
The global prevalence of anxiety, depression, and PTSD has already been slowly but significantly increasing among adults, especially younger adults15–17. For example, a recent study showed rates of 43% for anxiety and 40% for depression, more than twice the rates of older adults18. Specifically, studies have shown that younger individuals, including those exposed to conflict zones, are at higher risk for mental health disorders such as PTSD, major depressive disorder, and generalized anxiety disorder19,20. This group is particularly vulnerable to the psychological effects of terrorist attacks or war, including job loss or reduced hours, financial strains, and separation from loved ones. Therefore, this study focuses on individuals aged 18–40, based on evidence indicating the heightened vulnerability of younger adults in these contexts.
Gender and ethnicity also influence mental health outcomes. A systematic review and meta-analysis showed that women are more likely to develop depression and PTSD in war-afflicted regions21. Israeli women demonstrated higher vulnerability to traumatic stress-related symptoms following terrorist attacks on Israeli society in the early 2000s22. Similarly, minority ethnic groups are known to face higher risks for adverse mental health outcomes after exposure to major traumatic events23. Specifically, Israeli Arabs, who comprise 18.1% of Israel’s population (compared to 75% for Jews), were found in studies, including one conducted following the October 7 attack, to carry increased risks for several psychopathologies24,25. While Israeli Arabs have the same legal rights to access care, including mental health care, as other citizens, like many minoritized populations globally, they experience bias, stigmatization, and discrimination that significantly impact their access and quality of care26. This often results in state authorities giving less priority to minority needs, leading to poorer coping strategies and greater psychological burdens for Israeli Arabs compared to Israeli Jews27–29.
The current study
This study seeks to deepen understanding of the various war-related stressors and social determinants of health that affect the mental health of civilians in conflict zones. Specifically, it examines the impacts of traumatic loss, forced displacement, and income loss, which we anticipate having relatively high prevalence rates, among a substantial sample of individuals (N = 1052) living in war-affected areas in Israel. Additionally, the study aims to assess the role of gender and ethnicity on the severity of mental health symptoms in these populations. We conducted a longitudinal study with assessments starting in February 2024 (day 1), through March 2024 (day 30), to May 2024 (day 90). We hypothesized that (1) individuals who experienced traumatic loss, were forcibly displaced, or suffered income loss would exhibit greater psychopathology, as would (2) women and members of ethnic minorities.
Methods
Recruitment and participants
Recruitment occurred between February and May 2024. The study recruited Hebrew-speaking civilians aged 18 to 40 living in northern and southern Israeli conflict areas. The focus was on individuals (both Jewish and Arabs) from these regions because they were the ones most directly affected by the October 7 attacks and subsequent war. The study used Panel4all, an Israeli crowdsourcing tool commonly employed in medical and psychological research, which provides access to a probability-based pool panel of approximately 100,000 Israelis, thus ensuring representative sampling of the national population. The platform confirms consistency in demographic characteristics over time, blocks participants who use location masking tools, and runs tests to identify bots. To enhance the validity of results, we excluded individuals who attempted multiple survey completions. Compensation for participants included monetary vouchers provided through the platform based on the average length of the survey. The budget per participant was $2.50. The Ethics Committee of the School of Psychological Sciences at Tel Aviv University approved the study and waived the need to obtain informed consent. All research was performed in accordance with relevant guidelines and regulations. Before the study, participants received an information sheet/consent form outlining its purpose and assuring them of confidentiality, anonymity, and the option to withdraw at any stage. Participants who reviewed and agreed to the form provided their consent by proceeding to complete the study via the online platform, Qualtrics.com. The study was registered in advance on the As Predicted platform on February 2, 2024 (https://aspredicted.org/T2K_T53).
Assessments on study day 1 included demographic information such as age, gender, educational level, socioeconomic status, and war-related factors assessing loss of loved ones, forced displacement, and income loss. This was followed by measurements of clinical symptoms. Follow-up assessments, conducted 30 and 90 days later, included the same clinical measurements.
Instruments
The Generalized Anxiety Disorder-7 (GAD-7) assesses seven items to evaluate the likelihood of generalized anxiety symptoms over the previous two weeks. Each item is scored from 0 (“not at all”) to 3 (“nearly every day”), with a possible total ranging from 0 to 2130. GAD-7 scores of 5–9 suggest mild anxiety, 10–14 moderate anxiety, and 15–21 severe anxiety. Previous research has shown a threshold score of 10 has high sensitivity (89%) and specificity (82%)30. In the current study, Cronbach’s alpha for the first assessment was 0.94.
The Patient Health Questionnaire-9 (PHQ-9) is a self-report tool for probable major depression based on DSM-5 criteria, assessing symptoms over the last two weeks31. Its scoring system ranges from 0 (“not at all”) to 3 (“nearly every day”), totaling between 0 and 27. Scores on the PHQ-9 are interpreted as probable mild (5–9), moderate (10–14), moderate-to-severe (15–19), and severe (20–27) depression. High sensitivity (88%) and specificity (85%) have been reported for the cut-off score of 1032. Cronbach’s alpha for the first assessment was 0.91.
The five-item PC-PTSD-5 is a brief self-report tool used to screen for DSM-5 PTSD33. A positive response to three or more items indicates possible PTSD. The PC-PTSD-5 has demonstrated reliable performance in comparison to clinician-administered PTSD interviews34. For this study, items were modified to specifically address the events of October 7th and the subsequent war (e.g., “In the past month, had nightmares about the October 7 event(s)/the war or thought about these related events when you did not want to?”). Cronbach’s alpha for the first assessment was 0.75.
To assess the effects of the October 7 events and related war experiences, we included questions to determine if participants had experienced traumatic losses, such as a family member or close friend being killed, injured, or kidnapped to Gaza. We also added questions to explore temporary or ongoing forced displacement, and inquiries about economic impacts, including loss of income or job and increased expenses.
Data analysis
We used Pearson’s chi-square and independent t-tests to compare demographic (age, gender, ethnicity, education, income, residency) and war-related characteristics (traumatic loss, forced displacement, and income loss) between those who completed the study and those who did not to identify potential biases and ensure the representativeness of our sample and the generalizability of emerging findings.
Group differences in clinical symptoms over time were measured using Linear Mixed Models. We applied a full factorial model across the three time points (day 1, day 30, and day 90) for traumatic loss (yes/no), forced displacement (yes/no), income loss (yes/no), gender (female/male), and ethnicity (Jewish versus Arab and Other, which included Druze, non-Jewish, and unspecified). Random intercepts for participants were included to account for repeated measures design. All statistical tests were two-sided, with the alpha level set at < 0.01 to adjust for multiple comparisons using the Bonferroni correction (0.05 divided by 5). Data analysis was performed using IBM SPSS Statistics 29.
Results
Sample characteristics
Following the removal of 196 participants (16%) due to failed validity tests, our final sample comprised 1052 individuals who completed the first set of assessments. Of those, 792 (75%) completed the 30-day follow-up assessment and 689 (65%) completed the 90-day follow-up assessment. Baseline characteristics did not differ between completers and non-completers. Mean ± SD respondent age was 30.4 ± 5.9 (range 18–40). Slightly more than half of participants were female (n = 566, 54%); none identified as transgender or non-binary. Table 1 presents the sample’s ethnicities, education, income, residency, traumatic loss (i.e., family members or close friends being killed, injured, or kidnapped to Gaza) (n = 268, 26%), forced displacement since October 7 (n = 243, 23%), and income loss due to the war (n = 479, 45%).
Table 1.
Demographic characteristics.
| Items | Total (n = 1052) | Completers (n = 689) | Non-completers (n = 363) | Statistic | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | t-tests | p | |
| Agea | 31.3 | 5.6 | 28.7 | 6.1 | 30.4 | 5.9 | 6.86 | < .001 |
| n | % | n | % | n | % | X2 | p | |
| Gender | 6.97 | .008 | ||||||
| Women | 566 | 54 | 391 | 57 | 175 | 48 | ||
| Men | 486 | 46 | 298 | 43 | 188 | 52 | ||
| Transgender/non-binary/other | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Ethnicity | 4.65 | .098 | ||||||
| Jewish | 969 | 92 | 642 | 93 | 327 | 90 | ||
| Arab | 64 | 6 | 34 | 5 | 30 | 8 | ||
| Otherb | 19 | 2 | 13 | 2 | 6 | 2 | ||
| Education | 29.5 | < .001 | ||||||
| Never completed high school | 11 | 1 | 5 | 1 | 6 | 2 | ||
| High school graduate | 318 | 30 | 172 | 25 | 146 | 40 | ||
| Some college credit | 231 | 22 | 161 | 23 | 70 | 19 | ||
| Bachelor’s degree | 388 | 37 | 277 | 40 | 111 | 31 | ||
| Master’s degree | 100 | 10 | 71 | 10 | 29 | 8 | ||
| Doctorate degree | 4 | 0 | 3 | 0 | 1 | 0 | ||
| Income | 7.65 | .105 | ||||||
| Significantly below average | 246 | 23 | 153 | 22 | 93 | 26 | ||
| Below average | 283 | 27 | 179 | 26 | 104 | 29 | ||
| Average | 282 | 27 | 200 | 29 | 82 | 23 | ||
| Above average | 204 | 19 | 129 | 19 | 75 | 21 | ||
| Significantly above average | 37 | 4 | 28 | 4 | 9 | 3 | ||
| Residency | 2.75 | .097 | ||||||
| Northern Israel | 550 | 52 | 316 | 46 | 186 | 51 | ||
| Southern Israel | 502 | 48 | 373 | 54 | 177 | 49 | ||
| October 7 and war-related events | ||||||||
| Traumatic loss: A family member or close friend was killed, injured, or kidnapped to Gaza | 268 | 26 | 158 | 23 | 110 | 30 | 6.80 | .009 |
| Forced displacement | 243 | 23 | 160 | 23 | 83 | 23 | 0.01 | .896 |
| Income loss | 479 | 45 | 302 | 44 | 177 | 49 | 2.32 | .127 |
Pearson Chi-square; aIndependent t-tests; bOther: Druze (n = 5), Russian (n = 2), Christian (n = 3), no religion (n = 2), unspecified (n = 7).
Effects of October 7th and the ensuing war on clinical symptoms
Table 2 presents the clinical symptoms across time points. Of the 1052 individuals, 75% (n = 790) reported above threshold anxiety, depression, or PTSD symptoms at day 1, 69% (n = 548) reported these symptoms at day 30, and 67% (n = 464) at day 90. On the GAD-7 screen, 32% (n = 332) exceeded the moderate threshold (GAD-7 scores 10–21) at day 1, 29% (n = 228) on day 30, and 24% (n = 162) on day 90. For depressive symptoms, 36% (n = 374) exceeded the moderate threshold (PHQ-9 scores 10–27) at day 1, 33% (n = 255) on day 30, and 31% (n = 212) on day 90. Overall, 44% (n = 465) of respondents reported symptoms suggesting probable PTSD (PC-PTSD score ≥ 3) at day 1; 40% (n = 313) at day 30, and 37% (n = 250) at day 90.
Table 2.
Clinical symptoms over time.
| Characteristic | Day 1 (n = 1052) | Day 30 (n = 792) | Day 90 (n = 689) | |||
|---|---|---|---|---|---|---|
| GAD-7 total score (range 0–21; Mean and SD) | 7.6 | 5.8 | 7.1 | 5.9 | 6.5 | 5.5 |
| n | % | n | % | n | % | |
| GAD-7 ≥ 5 | 678 | 64 | 484 | 61 | 400 | 59 |
| GAD-7 ≥ 10 | 332 | 32 | 228 | 29 | 162 | 24 |
| PHQ-9 total score (range 0–27; Mean and SD) | 8.2 | 8.1 | 7.6 | 6.6 | 7.3 | 6.4 |
| n | % | n | % | |||
| PHQ-9 ≥ 5 | 653 | 62 | 470 | 59 | 395 | 58 |
| PHQ-9 ≥ 10 | 374 | 36 | 255 | 32 | 212 | 31 |
| PC-PTSD total score (range 0–5; Mean and SD) | 2.2 | 2.2 | 2.1 | 1.7 | 1.9 | 1.7 |
| n | % | n | % | n | % | |
| PC-PTSD ≥ 3 | 465 | 44 | 313 | 40 | 250 | 37 |
GAD-7, Generalized Anxiety Disorder; PHQ-9, Patient Health Questionnaire; PC-PTSD, Primary Care PTSD Screen for DSM-5.
Figure 1 presents the mean GAD-7, PHQ-9, and PC-PTSD scores by traumatic loss, forced displacement, and income loss. At every time point, mean GAD-7 scores were consistently higher among individuals experiencing traumatic loss (F = 55.1, df = 1,2514, p < .001), forced displacement (F = 26.7, df = 1,2514, p < .001), and income loss (F = 215.3, df = 1,2514, p < .001). While we found a time effect only for traumatic loss, reflecting a statistically significant reduction in GAD-7 scores, we did not observe such an effect for forced displacement or income loss, nor did we find an interaction effect for any of the conditions. Similarly, mean PHQ-9 scores were consistently higher among individuals experiencing traumatic loss (F = 66.8, df = 1,2500, p < .001), forced displacement (F = 29.8, df = 1,2500, p < .001), and income loss (F = 214.2, df = 1,2500, p < .001). We found no time or interaction effect for any of these stressors. Mean PC-PTSD scores were higher at every time point among individuals experiencing traumatic loss (F = 108.1, df = 1,2495, p < .001), forced displacement (F = 49.6, df = 1,2495, p < .001), and income loss (F = 191.4, df = 1,2495, p < .001). As with the PHQ-9 scores, we found no time or interaction effect for any of the conditions.
Fig. 1.
Generalized Anxiety Disorder-7 (GAD-7), Patient Health Questionnaire-9 (PHQ-9), and the Primary Care PTSD (PC-PTSD) Scores by Traumatic Loss (TL), Forced Displacement (FD), and Income Loss (IL). Notes: TL, Traumatic Loss; FD, Forced Displacement; IL, Income Loss; GAD-7, Generalized Anxiety Disorder; PHQ-9, Patient Health Questionnaire; PC-PTSD, Primary Care PTSD Screen for DSM-5. Linear Mixed Models: F values ranged from 26.7 to 215.3, with all p < .001.
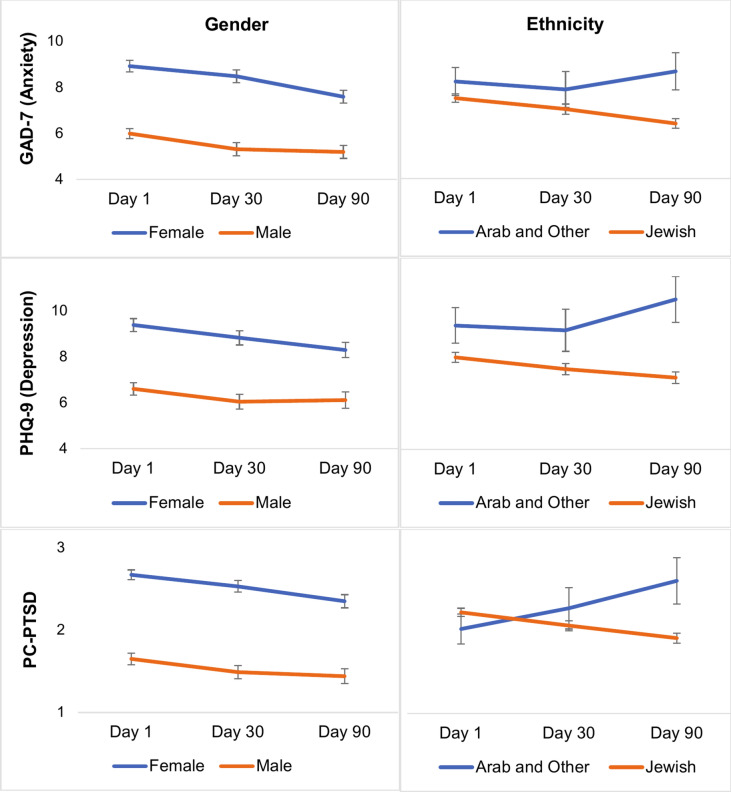
Figure 2 presents the mean GAD-7, PHQ-9, and PC-PTSD scores by gender and ethnicity. For gender, at every time point, women had consistently higher mean GAD-7 scores (F = 153.5, df = 1,2514, p < .001), mean PHQ-9 scores (F = 17.7, df = 1,2500, p < .001), and mean PC-PTSD scores (F = 213.9, df = 1,2495, p < .001). GAD-7 and PHQ-9 scores showed a temporal effect, reflecting a statistically significant reduction over time. However, none of the measurement scales showed an interaction effect. We conducted additional analyses to explore potential age-by-gender interactions; however, no significant results were observed, possibly due to the sample size limiting the ability to detect such effects. For ethnicity, at every time point mean GAD-7 scores were consistently higher among Arab and Other respondents (F = 8.3, df = 1,2514, p = .004). We found similar findings for mean PHQ-9 scores (F = 97.1, df = 1,2500, p < .001). We found no such effect for PC-PTSD scores, nor a time effect or interaction effect for any measurement scale.
Fig. 2.
Generalized Anxiety Disorder-7 (GAD-7), Patient Health Questionnaire-9 (PHQ-9), and the Primary Care PTSD (PC-PTSD) Scores by Gender and Ethnicity. Notes: Arab (n = 64) and Other: Druze (n = 5), Russian (n = 2), Christian (n = 3), no religion (n = 2), unspecified (n = 7); GAD-7, Generalized Anxiety Disorder; PHQ-9, Patient Health Questionnaire; PC-PTSD, Primary Care PTSD Screen for DSM-5. Linear Mixed Models: F values ranged from 8.3 to 213.9, with p ranging from .004 to < .001.
Discussion
Our study assessed self-reported symptoms of anxiety, depression, and PTSD over 90 days among 1052 individuals living in conflict zones. We found above-threshold mental health symptoms in 75% of participants, which slightly decreased over three months. As hypothesized, individuals experiencing traumatic losses, forced displacement, or economic hardships demonstrated higher symptom rates across all measures (GAD-7, PHQ-9, PC-PTSD). This was evident in the consistently elevated mean scores among these groups, compared to those without such experiences, across all time points. In addition, women and members of ethnic minorities consistently reported higher distress levels than men and Jewish individuals. These patterns of elevated distress call for immediate attention to the mental health needs of those bearing the greatest burdens in conflict-affected regions.
Overall, 75%, 69%, and 67% of the participants reported symptoms of anxiety, depression, and/or PTSD on day 1, day 30, and day 90, respectively. Research on war-affected zones and psychological outcomes in the general population is limited. A systematic review and meta-analysis updated WHO estimates and found that the prevalence of mental disorders such as depression, anxiety, PTSD, bipolar disorder, and schizophrenia in conflict-affected populations is 22.1% at any given time35. A similar study of migrants exposed to armed conflicts found prevalences of 31% for current PTSD, 25% for major depressive disorder, and 14% for generalized anxiety disorder, based on standardized psychiatric interviews19. Younger migrants displayed higher incidences of PTSD and anxiety, while longer time since displacement correlated with lower lifetime prevalences of PTSD and depression19. A nationwide prospective study conducted in Israel after October 7 showed high levels of anxiety, depression, and PTSD compared to levels before October 736. However, this national study did not focus on conflict zones, nor on war-related stressors. Importantly, although we cannot compare our sample to population-based representative samples, other web-based self-reported opportunity samples have shown similarly high rates in war-affected zones37,38.
Specifically, our findings on elevated GAD-7, PHQ-9, and PC-PTSD scores among individuals living in war-affected areas in Israel who have experienced traumatic loss, forced displacement, or income loss align with existing literature5–11,13,14,39–41. These elevated symptoms reflect the profound mental health challenges individuals face in grappling with the immediate effects of war-related adversities. The clinically meaningful symptoms associated with these conditions highlight their role as critical factors in the exacerbation of mental health issues, calling for urgent and specialized interventions that address these specific sources of psychological strain42. Such interventions should be designed to address the specific needs of those most affected, considering factors such as the duration and intensity of exposure, age, and the nature of the adversity experienced. This targeted approach is crucial for mitigating the severe and prolonged impact on mental well-being in conflict settings.
Our findings of higher symptomatology among women corroborate extant literature21,43. For example, a systematic review of the psychological effects of COVID-19 on the general population identified a higher prevalence of mental health issues among women and pointed to gender as a risk factor43; however, research also suggests that gender differences disappear over time44. In combination these results suggest a heightened immediate vulnerability or willingness among women to experience and report symptoms of anxiety, depression, and PTSD in conflict-affected settings. These findings emphasize the opportunity for targeted evidence-informed mental health interventions that consider the specific immediate vulnerabilities and resilience factors present in female populations in these high-stress environments. For example, Interpersonal Psychotherapy (IPT) could be one effective method, focusing on interpersonal relationships and emotional responses to sometimes overwhelming life events45. It may also be that females are more willing to endorse symptoms of distress associated with armed conflicts, or that symptoms among males will emerge later46. The emergence of symptoms along different time-based trajectories has been identified among Veteran cohorts11. Continued longitudinal efforts are required to explore such possibilities.
Our findings reveal persistent ethnic disparities in mental health symptoms, with members of Arab and other minority communities residing in conflict zones consistently showing higher GAD-7 and PHQ-9 scores. Despite a limited sample size (n = 83), the significant differences underscore the enhanced vulnerability of individuals from these groups compared to Israeli Jews. While Israeli Arabs have the same legal rights to access mental health care, as other citizens, this disparity is likely due to restricted access to resources, social strain, and discrimination26. Moreover, the sociopolitical situation of Israeli Arabs, including challenges related to perceived double allegiance (Israel vs. fellow Palestinians) and fear of being branded as enemies by Jews, may contribute to these disparities. These factors, compounded by limited resources, highlight the urgent need for targeted evidence-informed, culturally sensitive mental health interventions. Additionally, trends observed in the figures suggest opposing symptom trajectories over time for Jewish and Arab participants, potentially reflecting divergent vulnerabilities and a loss of resources among Arab individuals24,25,27–29.
To effectively address the mental health concerns identified in our study, proactive measures must be implemented to support individuals most at risk. Specifically, healthcare providers should prioritize those who have endured traumatic loss, those who have been forcibly displaced, and those suffering from war-related economic insecurity, as each of these experiences can lead to instability and acute stress reactions. These stressors should serve as critical markers to help healthcare providers prioritize and tailor treatment efforts, ensuring that those in greatest need receive focused evidence-informed and accessible care. Such targeted interventions are essential not only for the well-being of the individuals directly affected but also for the broader societal health, contributing to the overall stability and resilience of communities living in conflict-affected areas.
Our study has several limitations. First, Hebrew-speaking crowdsourcing users may differ socio-demographically from the population in southern and northern Israel, thus limiting generalizability, specifically including lower rates of Israeli Arabs compared to the general population. Future studies should aim to recruit a larger and more representative sample of non-Jewish minorities, including Israeli Arabs and other subgroups. Additionally, the recruitment method may have introduced biases, such as underrepresentation of individuals without internet access or those less likely to participate in online surveys. Second, we targeted the age range of 18–40 years, excluding older individuals, due to the higher incidence of psychopathology in the younger demographic; effects on older (and younger) populations also warrant exploration. Third, a notable study limitation is the absence of baseline data predating the October events, a common issue in research triggered by sudden, unexpected crises. We also did not inquire about non-war-related trauma since October 7. Fourth, clinical assessments based on self-report questionnaires rather than formal diagnostic interviews are subject to over- or underreporting. Lastly, while this study provides valuable insights into the perceptions of Israeli civilians, it is important to note that it does not address the effects on Palestinians, which represents a significant limitation in understanding the full scope of the conflict’s consequences.
Conclusions
This study underscores the urgent need for comprehensive mental health support systems in conflict zones. Evidence-informed services should be tailored to engage and address the needs of those at greatest immediate reported risk including women, members of ethnic minorities, and individuals facing traumatic losses, displacement, or economic hardship, with the goal of mitigating the development of persistent symptoms and/or psychiatric disorders. By highlighting the significant prevalence of anxiety, depression, and PTSD symptoms within these groups, our research reaffirms the necessity for targeted evidence-informed interventions specifically designed to support individuals with these demographic characteristics, or those who are facing such stressors. Further research is required to extend these findings to other populations and to include those older than 40 or younger than 18.
Acknowledgements
We thank the civilians who participated in the study.
Author contributions
D.A. wrote the first draft of this manuscript. D.A., S.H.N., A.L., Y.L.B., and Y.N. coordinated the trial, contributed to the design and implementation of the trial, and collected the data. D.A., S.H.N., and A.L. performed the statistical analyses. All authors reviewed and approved the manuscript.
Funding
Funding was provided by the HOMIYAH.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Vinograd, C. & Kershner, I. Israel’s Attackers Took Over 200 Hostages. Here’s What to Know About Them. The New York Times (2023).
- 2.Statista.com. (2023). Retrieved from. https://www.statista.com/statistics/1330395/deadliest-terrorist-attacks-worldwide-fatalities/
- 3.Around Half a Million Israelis Displaced Inside Israel: Military. Barron’s. 16 October 2023. Retrieved 18 November 2023.
- 4.Israel sharpens warning to Lebanon as cross-border hostilities spike. Reuters. 13 November 2023. Archived from the original on 13 November 2023. Retrieved 30 January 2024.
- 5.Lowell, A. et al. 9/11-related PTSD among highly exposed populations: A systematic review 15 years after the attack. Psychol. Med.48, 537–553 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bonanno, G. A., Galea, S., Bucciarelli, A. & Vlahov, D. Psychological resilience after disaster: New York City in the aftermath of the September 11th terrorist attack. Psychol. Sci.17, 181–186 (2006). [DOI] [PubMed] [Google Scholar]
- 7.Garfin, D. R., Poulin, M. J., Blum, S. & Silver, R. C. Aftermath of terror: a nationwide longitudinal study of posttraumatic stress and worry across the decade following the September 11, 2001 terrorist at- tacks. J. Trauma Stress31(1), 146–156 (2018). [DOI] [PubMed] [Google Scholar]
- 8.Boudoukha, A. H., Ouagazzal, O. & Goutaudier, N. When traumatic event exposure characteristics matter: impact of traumatic event exposure characteristics on posttraumatic and dissociative symptoms. Psychol. Trauma9(5), 561 (2017). [DOI] [PubMed] [Google Scholar]
- 9.Rigutto, C., Sapara, A. O. & Agyapong, V. I. Anxiety, depression and posttraumatic stress disorder after terrorist attacks: A general review of the literature. Behav. Sci.11(10), 140 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ozbay, F., der Heyde, T. A., Reissman, D. & Sharma, V. The enduring mental health impact of the September 11th terrorist attacks: Challenges and lessons learned. Psychiatr. Clin.36(3), 417–429 (2013). [DOI] [PubMed] [Google Scholar]
- 11.Donoho, C. J., Bonanno, G. A., Porter, B., Kearney, L. & Powell, T. M. A decade of war: Prospective trajectories of PTSD symptoms among deployed US military personnel and the influence of combat exposure. Am. J. Epidemiol.186(12), 1310–1318 (2017). [DOI] [PubMed] [Google Scholar]
- 12.Kristensen, P., Weisæth, L. & Heir, T. Bereavement and mental health after sudden and violent losses: A review. Psychiatry75(1), 76–97. 10.1521/psyc.2012.75.1.76 (2012). [DOI] [PubMed] [Google Scholar]
- 13.Porter, M. & Haslam, N. Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: a meta-analysis. JAMA294(5), 602–612. 10.1001/jama.294.5.602 (2005). [DOI] [PubMed] [Google Scholar]
- 14.Ruengorn, C., Awiphan, R., Wongpakaran, N., Wongpakaran, T., Nochaiwong, S., Health Outcomes and Mental Health Care Evaluation Survey Research Group (HOME‐Survey). Association of job loss, income loss, and financial burden with adverse mental health outcomes during coronavirus disease 2019 pandemic in Thailand: A nationwide cross‐sectional study. Depress. Anxiety38(6), 648–660 (2021). [DOI] [PMC free article] [PubMed]
- 15.Kujawa, A., Green, H., Compas, B. E., Dickey, L. & Pegg, S. Exposure to COVID-19 pandemic stress: Associations with depression and anxiety in emerging adults in the United States. Depress. Anxiety.37(12), 1280–1288 (2020). [DOI] [PubMed] [Google Scholar]
- 16.Hawes, M. T., Szenczy, A. K., Klein, D. N., Hajcak, G. & Nelson, B. D. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol. Med.52, 1–9 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Amsalem, D. et al. Anxiety and depression symptoms among young US essential workers during the COVID-19 pandemic. Psychiatric Serv.74(10), 1010–1018 (2023). [DOI] [PubMed] [Google Scholar]
- 18.Zhang, W., Walkover, M. & Wu, Y. Y. The challenge of COVID-19 for adult men and women in the United States: Disparities of psychological distress by gender and age. Public Health198, 218–222 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mesa-Vieira, C. et al. Mental health of migrants with pre-migration exposure to armed conflict: A systematic review and meta-analysis. Lancet Public Health7(5), e469–e481 (2022). [DOI] [PubMed] [Google Scholar]
- 20.Newnham, E. A., Pearson, R. M., Stein, A. & Betancourt, T. S. Youth mental health after civil war: The importance of daily stressors. Br. J. Psychiatry206(2), 116–121. 10.1192/bjp.bp.114.146324 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morina, N., Stam, K., Pollet, T. V. & Priebe, S. Prevalence of depression and posttraumatic stress disorder in adult civilian survivors of war who stay in war-afflicted regions. A systematic review and meta-analysis of epidemiological studies. J. Affect. Disord.239, 328–338 (2018). [DOI] [PubMed] [Google Scholar]
- 22.Bleich, A., Gelkopf, M. & Solomon, Z. Exposure to terrorism, stress-related mental health symptoms, and coping behaviors among a nationally representative sample in Israel. JAMA290(5), 612–620. 10.1001/jama.290.5.612 (2003). [DOI] [PubMed] [Google Scholar]
- 23.Brewin, C. R., Andrews, B. & Valentine, J. D. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J. Consult. Clin. Psychol.68(5), 748 (2000). [DOI] [PubMed] [Google Scholar]
- 24.Central Bureau of Statistics. (2023). Retrieved from https://www.cbs.gov.il/on February 13, 2024.
- 25.Groweiss, Y., Blank, C., Hamdan, S., Neria, Y. & Levi-Belz, Y. The mental health impact of the October 7th terror attack on Jews and Arabs in Israel: A nationwide prospective study. Psychiatry Res.337, 115973 (2024). [DOI] [PubMed] [Google Scholar]
- 26.Pearlin, L. I., Schieman, S., Fazio, E. M. & Meersman, S. C. Stress, health, and the life course: Some conceptual perspectives. J. Health Soc. Behav.46(2), 205–219 (2005). [DOI] [PubMed] [Google Scholar]
- 27.Achdut, N. Ethnic inequality between Arabs and Jews in Israel in global life satisfaction: A social determinants examination among young adults. Am. J. Orthopsychiatry (2024). [DOI] [PubMed]
- 28.Hobfoll, S. E., Canetti-Nisim, D. & Johnson, R. J. Exposure to terrorism, stress-related mental health symptoms, and defensive coping among Jews and Arabs in Israel. J. Consult. Clin. Psychol.74(2), 207 (2006). [DOI] [PubMed] [Google Scholar]
- 29.Marciano, H., Kimhi, S. & Eshel, Y. Predictors of individual, community and national resiliencies of Israeli Jews and Arabs. Int. J. Psychol.55(4), 553–561 (2020). [DOI] [PubMed] [Google Scholar]
- 30.Spitzer, R. L., Kroenke, K., Williams, J. B. W. & Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med.166(10), 1092–1097. 10.1001/archinte.166.10.1092 (2006). [DOI] [PubMed] [Google Scholar]
- 31.Kroenke, K., Spitzer, R. L. & Williams, J. B. W. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med.16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Levis, B., Benedetti, A. & Thombs, B. D. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: Individual participant data meta-analysis. BMJ365, I1476. 10.1136/bmj.l1476 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Prins, A. et al. The primary care PTSD screen for DSM-5 (PC-PTSD-5): Development and evaluation within a veteran primary care sample. J. Gen. Intern Med.31(10), 1206–1211. 10.1007/s11606-016-3703-5 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ouimette, P., Wade, M., Prins, A. & Schohn, M. Identifying PTSD in primary care: Comparison of the Primary Care-PTSD Screen (PC-PTSD) and the General Health Questionnaire-12 (GHQ). J. Anxiety Disord.22(2), 337–343. 10.1016/j.janxdis.2007.02.010 (2008). [DOI] [PubMed] [Google Scholar]
- 35.Charlson, F. et al. New WHO prevalence estimates of mental disorders in conflict settings: A systematic review and meta-analysis. Lancet394(10194), 240–248 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Levi-Belz, Y., Groweiss, Y., Blank, C. & Neria, Y. PTSD, depression, and anxiety after the October 7, 2023 attack in Israel: A nationwide prospective study. EClinicalMedicine68, 102418 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zasiekina, L., Zasiekin, S. & Kuperman, V. Post-traumatic stress disorder and moral injury among Ukrainian civilians during the ongoing war. J. Community Health48(5), 784–792. 10.1007/s10900-023-01225-5 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scholte, W. F. et al. Mental health symptoms following war and repression in eastern Afghanistan. JAMA292(5), 585–593 (2004). [DOI] [PubMed] [Google Scholar]
- 39.Priebe, S. et al. Psychological symptoms as long-term consequences of war experiences. Psychopathology46(1), 45–54. 10.1159/000338640 (2013). [DOI] [PubMed] [Google Scholar]
- 40.Mollica, R. F. et al. Longitudinal study of psychiatric symptoms, disability, mortality, and emigration among Bosnian refugees. JAMA286(5), 546–554. 10.1001/jama.286.5.546 (2001). [DOI] [PubMed] [Google Scholar]
- 41.Miller, K. E. & Rasmussen, A. The mental health of civilians displaced by armed conflict: an ecological model of refugee distress. Epidemiol. Psychiatr. Sci.26(2), 129–138. 10.1017/S2045796016000172 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Siriwardhana, C., Ali, S. S., Roberts, B. & Stewart, R. A systematic review of resilience and mental health outcomes of conflict-driven adult forced migrants. Conflict Health8, 1–4 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xiong, J. et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord.277, 55–64 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fenollar-Cortés, J., Jiménez, Ó., Ruiz-García, A. & Resurrección, D. M. Gender differences in psychological impact of the confinement during the COVID-19 outbreak in Spain: A longitudinal study. Front Psychol.12, 682860. 10.3389/fpsyg.2021.682860 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Markowitz, J. C. In the Aftermath of the Pandemic: Interpersonal psychotherapy for Anxiety, Depression, and PTSD (Oxford University Press, 2021). [Google Scholar]
- 46.Boerma, T., Hosseinpoor, A. R., Verdes, E. & Chatterji, S. A global assessment of the gender gap in self-reported health with survey data from 59 countries. BMC Public Health16, 1–9. 10.1186/s12889-016-2767-x (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.