Abstract
Objective
To determine the seasonal differences in instrumental activities of daily living (IADL) and objective physical activity among older adults residing in non-urban areas in snowy and cold regions according to sex.
Patients and Methods
Fifty older adults aged ≥65 years were included in the present study. IADL was assessed using the revised Frenchay Activities Index (FAI), and physical activity was measured using a triaxial accelerometer. Comparisons were made between the snowy and non-snowy seasons based on sex.
Results
Compared to the non-snowy season, the female participants exhibited significantly lower scores for outdoor housework, outdoor activity, and overall scores on the FAI during the snowy season. In terms of physical activity, a decrease in the number of steps and light-intensity physical activity, accompanied by an increase in sedentary behavior, was observed in both sexes. High light-intensity physical activity decreased in the snowy season, especially in the female participants. In addition, the total moderate-to-vigorous physical activity (MVPA) and short-bout MVPA (intermittent and lasting <10 minutes) also decreased.
Conclusion
Considering the significant changes in lifestyle and physical activity during the cold snowy season, women should consider performing alternative physical activities other than indoor household chores. Furthermore, men should be encouraged to participate in indoor household chores they typically do not engage in, irrespective of the season.
Keywords: snowy and cold regions, instrumental activities of daily living (IADL), light-intensity physical activity (LPA), moderate-to-vigorous physical activity (MVPA), bout
Introduction
Individuals aged ≥65 years accounted for 29% of the population in Japan in 2022, with the number of individuals aged ≥75 years increasing by 15.5%1). The number of people requiring nursing care continues to increase with changes in the population structure2). Various causes, such as incapacity due to cerebrovascular disorders, fractures3), or sarcopenia; frailty due to aging and decreased physical activity (PA)3,4,5); and decreased skeletal muscle mass and muscle strength3, 6, 7), can lead to the need for nursing care. Decreased skeletal muscle mass is reportedly associated with reduced bone density8), impaired glucose metabolism, and lipid abnormalities9), which are risk factors for the development of lifestyle-related diseases. Thus, individuals with decreased skeletal muscle mass are at an increased risk of fractures, cerebrovascular disorders, and cardiovascular diseases owing to falls.
Active exercise and PA aid in minimizing risk factors that can be detrimental to health; therefore, maintaining a certain level of PA is encouraged, even in old age10). The World Health Organization (WHO) guidelines proposed in 2010 recommend performing long bouts (lasting at least 10 minutes) of moderate-to-vigorous PA (MVPA)11). Recent studies have shown that performing short periods of PA12, 13) or increasing light-intensity PA (LPA) in place of MVPA, in addition to performing longer periods of MVPA, can help maintain physical and cognitive function14,15,16,17).
The criteria for PA specified in the guidelines have changed; nevertheless, older adults are recommended to perform at least 150 min of MVPA per week10). A study of 70–80-year-old individuals in Japan who performed long- and short-bout (<10 minutes) MVPA revealed that approximately 75% of the study participants achieved this criterion, with short-bout MVPA accounting for the majority (approximately 75%)18). However, it was noted that the time of MVPA implementation and the percentage of long-bout MVPA varied according to the surrounding environment of the residential area. Specifically, the total MVPA of the participants residing in mountainous areas was higher than that of those residing in urban areas; however, long-bout MVPA was lower. These findings suggest that the surrounding environment of the residential area may affect the implementation status of MVPA18).
The walking environment, such as the road surface conditions in the residential area, reportedly influences the total amount of PA and the number of steps taken19). In addition to the differences in road surface conditions and other structures, the climate also influences PA20). Seasonal differences in outdoor temperature, snowfall, and hours of sunlight affect PA in regions with large seasonal climatic changes21,22,23,24). The amount of PA and the number of steps taken decrease significantly in winter; however, there are regional differences21,22,23,24). A study conducted in the United Kingdom, where average winter temperatures are lower, reported that the number of steps taken in winter was on average 13% lower than that in summer, with this difference being particularly pronounced on weekends25). Another study involving British adults reported that the duration of LPA decreased significantly in winter; however, no differences were observed in the duration of MVPA. Furthermore, the time spent in bed, including sedentary behavior (SB) and time not falling asleep, was significantly longer in winter26). Although many of these studies included relatively younger participants, their findings indicated that PA is affected by the season, emphasizing the requirement for formulating interventions that consider the seasonal decline in PA.
A Dutch study examining seasonal changes in PA among older adults reported that the duration of LPA and MVPA was longer in summer than that in winter among the younger participants; however, no differences were observed among the older participants regarding the amount of PA according to season27). These findings indicate that seasonal variation in PA decreases with age owing to the decrease in opportunities for work and household chores with advancing age27). Several studies have analyzed the seasonal changes in PA in Japan. A previous study involving older adults residing in non-urban areas in snowy and cold regions revealed that LPA and MVPA decreased and SB increased during winter, with particularly large changes being observed among men28). However, the study did not examine changes in the amount of PA, including changes in daily life roles and short bouts of PA.
Japan is an island nation with a long north–south axis; consequently, there are large climatic differences among the regions29). Tohoku and Hokkaido are categorized as snowy and cold regions, where snow accumulation and temperature drops are particularly pronounced in the winter30). The environment is more severe in winter than that reported overseas, which is expected to have a greater potential to affect people’s behavior in winter. Lifestyle behavior exhibits sex-based differences31), and seasonal changes in lifestyle behavior may be related to PA, including short bouts of PA.
LPA accounts for the majority of PA among older adults32,33,34), and even in MVPA, most activities are short-bout PA18). Performing prolonged or frequent LPA in daily life may prevent a decline in cardiac and metabolic functions35) and obesity36), has a positive effect on lower limb muscle strength and mobility33, 37), and reduces mortality in the long term32, 38). In MVPA, short-bout PA is associated with health benefits in old age12, 13). Therefore, it is important to examine the changes in PA among older adults, including LPA and short-bout MVPA, in winter to promote preventive support activities tailored to regional characteristics.
Previous studies have shown that seasonal climate changes affect the activity status of community residents; however, these seasonal changes in the amount of PA, including behavioral patterns, especially among older adults, have not been verified. Therefore, this study aimed to clarify the characteristics of seasonal changes in lifestyle behavior and PA, specifically, low-intensity and slice-of-life activities, among older adults according to sex.
Patients and Methods
Participants
This study included older adults who had participated in the Tobetsu Elderly Health Support (TEHS) program during the non-snowy season (June–September 2023) and undergone additional measurements during the snowy season (January–February 2024). Tobetsu, a rural region with a population of approximately 15,000, is located in Ishikari County, Hokkaido, Japan39). The annual snowfall and average temperature during the snowy season (December to March) are about 700 cm and −4 °C, respectively40).
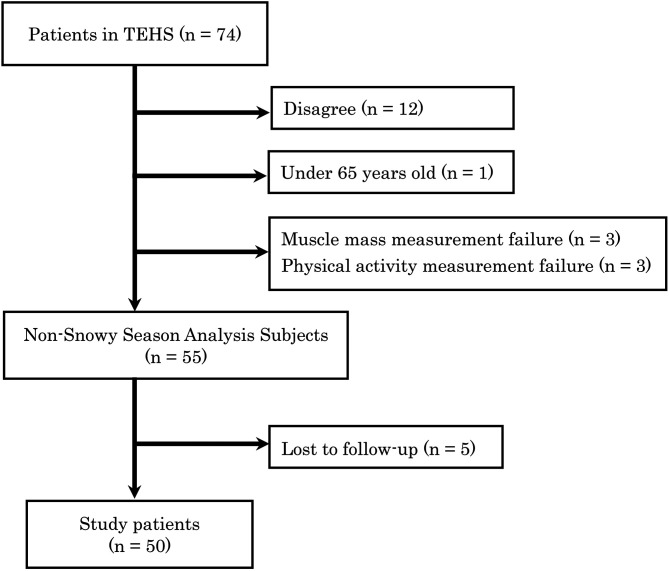
The TEHS program measures physical functions and provides health lectures conducted by specialists to deepen local awareness of health conditions. The program was planned and managed by four organizations: Tobetsu Town, Tobetsu Social Welfare Council, Tobetsu Community Care Center, and the Health Sciences University of Hokkaido. The study was explained orally and in writing to 74 TEHS participants at the beginning of the project. One participant aged <65 years was excluded. Among the 61 participants who consented to participate in the study, six participants with missing measurement data were excluded. Thus, among the remaining 55 participants, 50 participants who had undergone measurements during the winter season were included in the analysis (Figure 1).
Figure 1.
Study patients selection flowchart.
Methods
Data regarding basic information such as age, sex, family members residing with the patient, and medical history were collected from June–September 2023 (non-snowy season). In addition, the status of instrumental activities of daily living (IADL) was measured using a questionnaire. Data regarding body composition parameters such as body mass index (BMI), body fat percentage, appendicular skeletal muscle mass index (ASMI), grip strength, and physical ability were also collected. PA at home was measured using an activity meter equipped with a triaxial accelerometer. The participants who underwent measurements during the non-snowy season were surveyed via questionnaires during the snowy season from January–February 2024, similar to the non-snowy season, to assess their PA at home and performance of IADL, among other factors. The activity meters and written correspondence were sent to the participants via mail during the snowy season.
The performance of IADL was assessed using the revised Frenchay Activities Index (FAI)41). The FAI was developed as an IADL assessment tool for patients with stroke; however, its use has expanded to include community-dwelling older adults42). Age-specific reference values for the FAI have been reported31, 43). The FAI comprises 15 items scored on a scale of 0 to 3, yielding a total score of 45 points, with higher values indicating higher performance of IADL31, 34). IADLs were categorized and calculated using five subscales: indoor household chores (meal preparation, cleaning after meals, laundry, cleaning and tidying, and manual labor), outdoor household chores (shopping, yard work, house, and car maintenance), outdoor activities (going out, outdoor walking, using transportation, and traveling), hobbies (hobbies, reading), and jobs (work).
Dietary intake was assessed using the Dietary Variety Score (DVS)44), which comprises 10 foods, including meat and green and yellow vegetables. The total DVS is 10, with 1 and 0 points corresponding to “eating almost every day” and “not eating on some days”, respectively44).
The Geriatric Depression Scale 15 (GDS) was used to assess depression45, 46). This scale comprises 15 questions with a “yes” or “no” response. The scores ranged from 0 to 15, with 1 point being added for each response indicating a depressive tendency. The total score was 15, with a cutoff value of ≥6 indicating depressive tendency46). The respondents were instructed to indicate the most recent conditions at the time of the survey in the non-snowy and snowy seasons.
The body fat percentage and ASMI were measured using a bioelectrical impedance-measuring device (InBody S10; InBody Japan Inc., Tokyo, Japan) with the participants in a seated position. Grip strength was measured twice in the standing position using a Smedley grip strength meter. The maximum value obtained was recorded as the reference value.
Physical functioning was assessed using the Short Physical Performance Battery (SPPB). SPPB was developed as a comprehensive assessment method for lower extremity function47) and incorporated into the diagnostic criteria48) of the Asian Working Groups for Sarcopenia 2019 Consensus (AWGS2019). SPPB comprises a standing balance test, gait test, and Five-times-sit-to-stand test (FTSST), with each test being scored on a scale of 0 to 4 points, according to the results of the measurement. The total score of SPPB is 12 points, with higher scores indicating better physical function47). Walking speed was calculated from the gait test, and the time required for the 5SST was recorded.
PA was measured using an activity meter equipped with a triaxial acceleration sensor (Active Style Pro HJA-750C; Omron, Kyoto, Japan). The device was worn by the participants from the time of waking up till bedtime; however, the device was removed while bathing and during other water-related activities. The measurements were conducted for seven consecutive days. The device was worn over the entire lumbar region, and the time taken to wear and remove it was recorded on a log form to ensure it was worn daily. Only the clock was displayed to minimize bias from wearing the device. The validity of the activity measured using the activity meter was confirmed49, 50), and the measurement epoch was set to 60 s. Only participants who wore the device for ≥10 h per day for at least 4 days were included in the analysis51). Periods during which the recorded activity remained at the zero count for ≥90 min were considered non-wearing periods52, 53). The total number of steps taken per day and the number of steps adjusted for wearing time were calculated using an activity meter. The time required per day for each activity was calculated.
The activity intensity was classified into SB (≤1.5 metabolic equivalents of task [METs]), LPA (1.6–2.9 METs), and MVPA (≥3.0 METs). Low light-intensity PA (LLPA [1.6–1.9Mets]) and high light-intensity PA (HLPA [2.0–2.9Mets]) were defined as described in a previous study54). The duration of each activity intensity was classified according to the time taken to perform the activity (bout), and the duration and number of times the activity was performed were calculated. SB was classified as <30 min, 30–59 min, and ≥60 min, and the time and number of times each bout was performed were calculated. The number of SB interruptions (breaks) was calculated. A break was defined as the number of times LPA or higher activity of ≥1 min occurred after SB of ≥1 min of duration55). The duration and number of times of LPA and MVPA performed in short-bout and long-bout, respectively, were determined as described in previous studies14, 18). Long-bout MVPA was evaluated without considering activities of <3 METs of ≤2 minutes duration in the present study18). Macro (ver. 1.0), provided free of charge by the Physical Activity Research Platform56), was used to process the data from the activity meters.
Statistical analysis
The Shapiro–Wilk test was used to confirm normality of consecutive data. Among the data measured during the non-snowy season, age; comorbidities; physical functions, such as grip strength and SPPB; and body composition data, such as muscle mass were compared according to sex. The chi-square test or Fisher’s exact test was used for nominal measures. An unpaired t-test was used to assess normally-distributed continuous data, whereas the Mann–Whitney’s U-test was used to assess non-normally-distributed data. The differences between the non-snow and snowy seasons in terms of the changes in the FAI and objective PA were compared for all participants and both sexes, respectively, using the paired t-test (normal data) and Wilcoxon rank sum test (non-normal data). All statistical analyses were performed using SPSS Statistics ver. 26 (IBM, Armonk, NY, USA). Statistical significance was set at 5%.
Research ethics
This study adhered to the principles of the Declaration of Helsinki. Written and verbal explanations of the purpose and objectives of the study were provided to all participants. Only data from participants who provided informed consent were included in the analysis. This study was approved by the Research Ethics Committee of the Health Sciences University of Hokkaido (23R179233).
Results
Table 1 presents the basic characteristics, body composition, and physical functions of the participants. The average age of the participants was 78.8 years. No significant differences were observed between the male and female participants in terms of the mean age, percentage of preexisting diseases, SPPB score, gait speed, or 5SST results. However, the maximum grip strength was significantly higher in the male participants. The male participants had a higher average height, whereas the female participants had significantly higher BMI and body fat percentage. According to the AWGS2019 criteria, 28.0%, 32.0%, and 18.0% of the participants had reduced skeletal muscle mass, reduced muscle strength, and sarcopenia, respectively; no significant sex differences were observed.
Table 1. Basic information of the patients.
| Total (n=50) | Male (n=19) | Female (n=31) | P-value | |
|---|---|---|---|---|
| Age (years) | 78.8 (6.3) | 81.0 [77.0–84.0] | 78.1 (6.1) | 0.190a |
| Living together | 46 (87.3%) | 19 (100%) | 27 (87.1%) | 0.284b |
| Osteoarthritis (yes) | 11 (22.0%) | 3 (15.8%) | 8 (25.8%) | 0.498b |
| Neurological disease (yes) | 0 (0%) | 0 (0%) | 0 (0%) | – |
| Heart disease (yes) | 5 (10.0%) | 1 (5.3%) | 4 (12.9%) | 0.637b |
| Respiratory disease (yes) | 4/46 (8.0%) | 3 (15.8%) | 1 (3.3%) | 0.147b |
| Hypertension (yes) | 22 (44.0%) | 6 (31.6%) | 16 (51.6%) | 0.242b |
| Diabetes (yes) | 9 (18.0%) | 4 (21.1%) | 5 (16.1%) | 0.715b |
| Height (cm) | 156.4 (6.3) | 164.4 (7.9) | 151.6 (7.0) | <0.01c |
| Weight (kg) | 57.0 (9.0) | 59.2 (6.6) | 55.7 (10.1) | 0.137c |
| BMI | 23.3 (3.6) | 22.0 (2.8) | 24.2 (3.7) | 0.034c |
| Body fat rate (%) | 28.4 (8.9) | 21.6 (7.6) | 32.6 (6.8) | <0.01c |
| ASMI | 6.5 (0.90) | 7.1 (0.62) | 6.2 (0.76) | <0.01c |
| Max. grip strength (kgf) | 25.7 (7.7) | 31.5 (9.1) | 22.2 (3.8) | <0.01c |
| SPPB Balance test | 4.0 [4.0–4.0] | 4.0 [4.0–4.0] | 4.0 [4.0–4.0] | 0.959a |
| SPPB Gait speed test | 4.0 [4.0–4.0] | 4.0 [4.0–4.0] | 4.0 [4.0–4.0] | 0.519a |
| SPPB Chair stand test | 4.0 [4.0–4.0] | 4.0 [4.0–4.0] | 4.0 [4.0–4.0] | 0.071a |
| SPPB Total score | 12.0 [12.0–12.0] | 12.0 [12.0–12.0] | 12.0 [11.0–12.0] | 0.331a |
| Walking speed (m/sec) | 1.15 (0.21) | 1.20 (0.23) | 1.13 (0.20) | 0.233c |
| FTSST (sec) | 9.1 [7.7–9.9] | 8.6 [7.8–9.8] | 9.3 [7.4–10.4] | 0.896a |
| Low muscle mass | 14 (28.0%) | 8 (42.1%) | 6 (19.4%) | 0.110b |
| Weakened muscle | 16 (32.0%) | 9 (47.4%) | 7 (22.6%) | 0.117b |
| Sarcopenia | 9 (18.0%) | 4 (21.1%) | 5 (16.1%) | 0.715b |
a: Mann–Whitney’s U-test, b: chi-square test or Fisher’s exact test, c: unpaired t-test.
BMI: body mass index: ASMI; appendicular skeletal muscle mass index; SPPB: short physical performance battery; FTSST: five-times-sit-to-stand test.
The FAI scores for outdoor household chores, outdoor activities, and hobbies, as well as the total scores, in the snowy season were significantly lower than those in the non-snowy season. The median scores of the male participants were lower during the snowy season; however, the differences were not significant. The FAI scores for outdoor household chores and outdoor activities and the total scores of the female participants decreased significantly in the snowy season compared with those in the non-snowy season (Table 2). The DVS of the male participants decreased significantly in the snowy season; however, the GDS score exhibited no changes (Table 2).
Table 2. Measurements of Frenchay Activities Index (FAI), dietary variety score (DVS) and geriatric depression scale 15 (GDS).
| Overall (n=50) | P-value | Male (n=19) | P-value | Female (n=31) | P-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Non–snowy season | Snowy season | Non–snowy season | Snowy season | Non–snowy season | Snowy season | ||||
| FAI Household affair | 12.0 [6.0–15.0] | 12.0 [8.0–14.0] | 0.134 | 6.0 [3.0–9.0] | 6.0 [3.0–10.0] | 0.114 | 13.0 [12.0–15.0] | 13.0 [12.0–15.0] | 0.570 |
| FAI Outdoor household affair | 6.0 [4.0–7.0] | 4.0 [3.0–6.0] | <0.01 | 6.0 [4.0–8.0] | 5.0 [3.0–7.0] | 0.223 | 6.0 [4.0–7.0] | 4.0 [3.0–5.0] | <0.01 |
| FAI Outdoor activity | 8.0 [6.0–10.0] | 6.0 [4.0–8.0] | <0.01 | 8.0 [6.0–10.0] | 7.0 [3.0–9.0] | 0.234 | 8.0 [6.0–10.0] | 6.0 [4.0–8.0] | <0.01 |
| FAI Hobby | 5.0 [3.0–6.0] | 4.0 [2.0–5.3] | <0.01 | 5.0 [3.0–6.0] | 3.0 [2.0–5.0] | 0.08 | 5.0 [3.0–6.0] | 4.0 [2.0–6.0] | 0.055 |
| FAI Work | 0.0 [0.0–0.1] | 0.0 [0.0–0.0] | 0.063 | 0.0 [0.0–0.1] | 0.0 [0.0–0.1] | 0.50 | 0.0 [0.0–0.1] | 0.0 [0.0–0.0] | 0.25 |
| FAI Total score | 28.7 (28.7) | 25.1 (7.8) | <0.01 | 24.6 (10.0) | 22.1 (9.5) | 0.192 | 31.2 (6.8) | 27.0 (6.1) | <0.01 |
| DVS | 6.4 (2.4) | 6.1 (2.4) | 0.346 | 6.4 (2.4) | 5.4 (2.3) | 0.023 | 6.5 (2.5) | 6.6 (2.4) | 0.782 |
| GDS | 2.0 [1.0–4.0] | 1.5 [1.0–4.0] | 0.945 | 2.0 [1.0–4.0] | 2.0 [0.0–3.0] | 0.852 | 2.0 [1.0–4.0] | 1.0 [1.0–5.0] | 0.780 |
In terms of PA, the overall wearing time and number of steps decreased by approximately 40 minutes and 850 steps (−25%), respectively. Furthermore, the number of steps corrected for wearing time in the snowy season decreased significantly compared with that in the non-snowy season (Table 3).
Table 3. Physical activity measurements.
| Overall (n=50) | P-value | Male (n=19) | P-value | Female (n=31) | P-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Non-snowy season | Snowy season | Non-snowy season | Snowy season | Non-snowy season | Snowy season | ||||
| Wear time, min/day | 862.8 (98.9) | 819.9 (88.3) | <0.01 | 855.4 (84.0) | 814.4 (81.5) | <0.01 | 867.4 (108.1) | 823.3 (93.3) | <0.01 |
| Step count, steps/day | 3,427.9 [2,027.5–5,803.5] | 2,587.3 [1,671.7–3,975.9] | <0.01 | 3,822.5 [2,138.1–7,237.8] | 2,666.3 [1,715.7–7,030.5] | 0.014 | 2,488.6 [1,822.5–5,266.1] | 2,327.3 [1,549.6–3,361.0] | <0.01 |
| Step count, steps/wear time | 4.0 [2.4–7.5] | 3.3 [2.0–4.4] | <0.01 | 4.5 [2.7–8.2] | 3.7 [2.3–8.4] | 0.060 | 3.1 [2.1–6.6] | 2.9 [1.8–3.8] | <0.01 |
| SB, min/day | 476.2 (111.3) | 515.4 (100.8) | <0.01 | 497.0 (107.0) | 520.4 (86.7) | 0.179 | 463.4 (113.7) | 512.3 (109.9) | <0.01 |
| LPA, min/day | 349.4 (84.4) | 276.7 (76.0) | <0.01 | 317.2 (66.5) | 259.7 (67.5) | <0.01 | 369.1 (89.0) | 287.2 (80.0) | <0.01 |
| LLPA, min/day | 131.8 (41.4) | 103.2 (34.5) | <0.01 | 123.3 (36.4) | 97.3 (35.3) | <0.01 | 137.0 (44.0) | 106.7 (34.0) | <0.01 |
| HLPA, min/day | 217.6 (65.2) | 164.1 [134.1–202.9] | <0.01 | 193.9 (45.6) | 162.4 (43.0) | <0.01 | 232.1 (71.5) | 168.0 [133.4–203.8] | <0.01 |
| MVPA, min/day | 26.0 [13.8–52.1] | 17.0 [10.4–39.8] | <0.01 | 29.3 [11.7–67.1] | 23.9 [11.3–47.7] | 0.113 | 25.3 [18.3–43.4] | 15.0 [10.1–35.4] | 0.022 |
| SB, % of wear time | 0.55 (0.11) | 0.63 (0.10) | <0.01 | 0.58 (0.10) | 0.64 (0.09) | <0.01 | 0.53 (0.11) | 0.62 (0.10) | <0.01 |
| LPA, % of wear time | 0.41 (0.09) | 0.34 (0.09) | <0.01 | 0.37 (0.08) | 0.32 (0.08) | <0.01 | 0.43 (0.10) | 0.35 (0.09) | <0.01 |
| LLPA, % of wear time | 0.15 (0.04) | 0.13 (0.04) | <0.01 | 0.14 (0.04) | 0.12 (0.04) | <0.01 | 0.16 (0.05) | 0.13 (0.04) | <0.01 |
| HLPA, % of wear time | 0.25 (0.08) | 0.21 (0.07) | <0.01 | 0.23 (0.06) | 0.20 (0.05) | 0.051 | 0.27 (0.09) | 0.20 (0.07) | <0.01 |
| MVPA, % of wear time | 0.03 [0.02–0.06] | 0.02 [0.01–0.05] | 0.030 | 0.04 [0.01–0.08] | 0.03 [0.01–0.06] | 0.275 | 0.03 [0.02–0.05] | 0.02 [0.10–0.16] | 0.076 |
| WHO physical activity guidelines, achieved | 28 (56%) | 23 (46%) | <0.01 | 10 (52.6%) | 11 (57.9%) | 0.070 | 18 (58.1%) | 12 (38.7%) | 0.032 |
SB: sedentary behavior; LPA: light-intensity physical activity; LLPA: low light-intensity physical activity; HLPA: high light-intensity physical activity; MVPA: moderate-to-vigorous physical activity; WHO: World Health Organization.
The SB time and percentage increased significantly, with the SB percentage exceeding 60% during the snowy season. The time and percentage of LPA and MVPA decreased significantly during the snowy season. In addition, the duration of LLPA and HLPA also decreased by approximately 20% during the snowy season compared with that during the non-snowy season (Table 3). The wearing time and the number of steps decreased by approximately 40 minutes and 1,200 steps (−31%), respectively, in the male participants; however, no significant differences were observed in the number of steps per wearing time. The SB time did not exhibit any significant difference; in contrast, the SB percentage increased significantly during the snowy season. The LPA time and percentage decreased significantly during the non-snowy season, with the LLPA time and HLPA time decreasing by approximately 20% and 15%, respectively. No seasonal differences were observed in MVPA (Table 3). The time to perform SB and the percentage of SB increased significantly in the snowy season. The time to perform LLPA and the percentage of HLPA decreased significantly in the non-snowy season. The SB time and percentage increased significantly in the snowy season, whereas the LPA time and percentage decreased significantly. LLPA and HLPA decreased by approximately 23% and 28%, respectively. MVPA exhibited a significant decrease in duration, but not in percentage (Table 3).
Notably, the proportion of participants who met the WHO recommended PA standards for older adults10) decreased from 56% in the non-snowy season to 46% in the snowy season, with a significant decrease being observed among the female participants (Table 3).
No significant differences were observed between the male and female participants in terms of SB of <30 min duration during the two seasons (Table 4). However, SBs of 30–60 min and ≥60 min duration increased significantly, with particularly large changes being observed in the SB of 30–60 min duration among male participants and that of ≥60 min duration among the female participants (Table 4). Short- and long-bout LPA decreased significantly in the snowy season among male and female participants. The MVPA duration decreased significantly only in short-bout LPA in the male and female participants (Table 4).
Table 4. Seasonal differences in activity time per bout.
| Overall (n=50) | P-value | Male (n=19) | P-value | Female (n=31) | P-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Non-snowy season | Snowy season | Non-snowy season | Snowy season | Non-snowy season | Snowy season | ||||
| Bout of SB (0≤,<30) min/day | 285.1 (56.7) | 274.0 (66.0) | 0.197 | 290.2 (59.5) | 282.0 (66.0) | 0.522 | 281.9 (55.6) | 269.0 (66.6) | 0.271 |
| Bout of SB (30≤, <60) min/day | 104.1 (45.8) | 128.1 (44.8) | <0.01 | 109.3 (49.5) | 137.4 (44.3) | 0.013 | 100.9 (43.9) | 122.3 (44.9) | 0.015 |
| Bout of SB (60≤) min/day | 68.1 [36.3–112.2] | 83.3 [34.5–144.0] | <0.01 | 74.1 [40.9–118.9] | 75.1 [31.3–119.8] | 0.829 | 47.4 [25.7–102.6] | 97.1 [45.3–154.1] | <0.01 |
| SB total min/day | 476.2 (111.3) | 515.4 (100.8) | <0.01 | 497.0 (107.0) | 520.4 (86.7) | 0.179 | 463.4 (113.7) | 512.3 (109.9) | <0.01 |
| Short-bout LPA min/day | 197.9 (40.8) | 171.5 (42.4) | <0.01 | 198.1 (45.7) | 177.7 (47.5) | <0.01 | 197.8 (38.1) | 167.0 (39.3) | <0.01 |
| Long-bout LPA min/day | 151.5 (64.7) | 94.0 [68.2–132.4] | <0.01 | 119.1 (30.6) | 82.0 (32.6) | <0.01 | 171.3 (72.1) | 102.1 [72.4–136.9] | <0.01 |
| LPA total min/day | 349.4 (84.4) | 276.7 (76.0) | <0.01 | 317.2 (66.5) | 259.7 (67.5) | <0.01 | 369.1 (89.0) | 287.2 (80.0) | <0.01 |
| Short-bout MVPA min/day | 24.2 [13.4–32.0] | 16.2 [9.7–33.3] | <0.01 | 24.3 [11.7–31.7] | 23.9 [11.3–38.1] | 0.441 | 24.0 [13.7–33.0] | 15.0 [9.2–29.3] | <0.01 |
| Long-bout MVPA min/day | 0.0 [0.0–9.4] | 0.0 [0.0–3.6] | 0.163 | 1.4 [0.0–22.9] | 1.4 [0.0–7.9] | 0.366 | 0.0 [0.0–3.9] | 0.0 [0.0–3.1] | 0.319 |
| MVPA total min/day | 26.0 [13.8–52.1] | 17.0 [10.4–39.8] | <0.01 | 29.3 [11.7–67.1] | 23.9 [11.3–47.7] | 0.113 | 25.3 [18.3–43.4] | 15.0 [10.1–35.4] | 0.022 |
SB: sedentary behavior; LPA: light-intensity physical activity; MVPA: moderate-to-vigorous physical activity.
The number of short SBs of <30 min duration decreased, and the number of SBs of >30 duration min increased significantly in the overall group and female participants (Table 5). In addition, the total number of breaks and the number of breaks per hour also decreased significantly (Table 5). The number of short SBs of <30 min duration decreased significantly, and the number of SBs of 30–60 min duration increased significantly among the male participants; no significant differences were observed in terms of the number of SBs of ≥60 min duration (Table 5). The total number of breaks tended to decrease; however, the difference was not significant. The number of breaks per hour exhibited a significant decrease (Table 5).
Table 5. Seasonal differences in the number of activities per bout.
| Overall (n=50) | P-value | Male (n=19) | P-value | Female (n=31) | P-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Non-snowy season | Snowy season | Non-snowy season | Snowy season | Non-snowy season | Snowy season | ||||
| Bout of SB (0≤, <30) number/day | 58.7 (13.8) | 52.6 (15.5) | <0.01 | 58.3 (14.2) | 52.8 (15.7) | 0.028 | 59.0 (13.8) | 52.5 (15.7) | <0.01 |
| Bout of SB (30≤, <60) number/day | 2.5 (1.1) | 3.1 (1.1) | <0.01 | 2.6 (1.1) | 3.3 (1.0) | <0.01 | 2.5 (1.0) | 2.9 (1.1) | 0.016 |
| Bout of SB (60≤) number/day | 0.85 [0.43–1.36] | 1.0 [0.43–1.63] | <0.01 | 1.0 [0.50–1.43] | 1.0 [0.43–1.43] | 0.883 | 0.67 [0.33–1.29] | 1.11 [0.57–1.86] | <0.01 |
| SB total number/day | 62.2 (13.5) | 57.0 (14.7) | <0.01 | 62.0 (13.4) | 57.3 (14.6) | 0.056 | 62.3 (13.7) | 56.8 (14.9) | 0.014 |
| Number of break/day | 61.7 (13.5) | 56.5 (14.8) | <0.01 | 61.6 (13.4) | 56.7 (14.9) | 0.052 | 61.8 (13.8) | 56.4 (15.0) | 0.016 |
| Number of break/h | 8.1 (2.3) | 6.8 (2.1) | <0.01 | 7.8 (2.2) | 6.8 (2.2) | <0.01 | 8.3 (2.3) | 6.9 (2.1) | <0.01 |
| Short-bout LPA number/day | 69.9 (15.4) | 62.4 (15.6) | <0.01 | 72.0 (17.6) | 66.2 (18.6) | 0.011 | 68.6 (14.1) | 60.1 (13.2) | <0.01 |
| Long-bout LPA number/day | 8.6 (3.3) | 6.3 (2.8) | <0.01 | 7.1 (1.9) | 5.1 (2.1) | <0.01 | 9.6 (3.6) | 7.1 (3.0) | <0.01 |
| LPA total number/day | 78.5 (15.9) | 68.8 (16.3) | <0.01 | 79.1 (18.5) | 71.3 (19.6) | <0.01 | 78.2 (14.5) | 67.2 (13.9) | <0.01 |
| Short-bout MVPA number/day | 16.3 [9.2–23.4] | 11.3 [7.3–18.5] | <0.01 | 17.2 [8.4–22.6] | 15.3 [8.9–23.4] | 0.210 | 16.2 [9.3–25.5] | 10.8 [6.6–17.1] | <0.01 |
| Long-bout MVPA number/day | 0.0 [0.0–0.7] | 0.0 [0.0–0.3] | 0.261 | 0.14 [0.0–1.0] | 0.14 [0.0–0.29] | 0.444 | 0.0 [0.0–0.29] | 0.0 [0.0–0.29] | 0.411 |
| MVPA total number/day | 16.5 [9.3–23.4] | 11.3 [7.3–19.3] | <0.01 | 18.4 [8.4–22.6] | 15.4 [8.9–23.7] | 0.156 | 16.2 [9.3–25.5] | 10.8 [6.7–17.6] | <0.01 |
SB: sedentary behavior; LPA: light-intensity physical activity; MVPA: moderate-to-vigorous physical activity.
The number of LPAs decreased significantly in the short- and long-bout sessions for the overall group, as well as the male and female participants (Table 5). The number of short-bout MVPA decreased significantly in the snowy season for both sexes (Table 5).
Discussion
The IADL practices and objective PA levels of older adults residing in rural areas in snowy and cold regions were measured in the non-snowy and snowy seasons in this study and the characteristics of seasonal changes and sex differences were examined. The results revealed that lifestyle behaviors and objective PA levels changed significantly in the snowy season compared with those in the non-snowy season and that these changes differed between men and women. IADL decreased only in the female participants during outdoor activities in the snowy season. The number of steps and LPA decreased in both sexes in the snowy season; however, MVPA decreased only in the female participants.
Studies investigating the seasonal changes in PA included self-report questionnaires21, 22) and measurements made using pedometers23, 24). These studies revealed significant decreases in PA and the number of steps taken in the winter season21,22,23,24). A study involving British adults with an average age of 41 years residing in an area with an average winter temperature of 4°C revealed an average decrease of 13% in the number of steps taken in winter compared with that in summer25). The number of steps decreased significantly during the snowy season in both sexes in the present study, with a median decrease of approximately 25%. This may be attributed to the decrease in outdoor activity owing to snowfall. Mizumoto et al. reported a decrease in the frequency of outings and a 20% decrease in outdoor activity time during periods of increased snowfall57). The FAI scores also decreased among the female participants, especially in the subcategories related to outdoor activities in the present study. A significant decrease in the subcategories related to outdoor activities was also observed. These results suggest that changes in daily activities owing to seasonal changes in cold, snowy regions may influence the decrease in the number of steps taken and the amount of PA, especially among women.
No seasonal differences in the FAI scores were observed among the male participants of this study. Men practice IADL to a lesser extent in the non-snowy season31, 43). Moreover, the number of men who continue to work decreases after their 60s. Notably, the time spent on work is not replaced by the time spent on housework and other household chores, and the time spent on household-related activities does not increase58). Men aged ≥70 years spend more time on excursions and walks than women58), and behaviors that do not correspond to FAI might be related to the number of steps taken and the amount of PA. Therefore, although the FAI score did not change in the snowy season, it was inferred that behaviors were not included in the FAI changed in the snowy season, resulting in a decrease in the number of steps taken and the amount of PA.
Arnardottir et al. examined the seasonal differences in the amount of PA in older adults with an average age of 80.3 years and reported that the duration of SB was approximately 4.4% and 2.2% higher in male and female individuals, respectively, in winter than that in summer59). In addition, a previous study in Japan revealed that SB in the snowy season increased by approximately 20% in men and 16% in women28). In the present study, SB increased by approximately 10% in men and 17% in women in the snowy season compared with that in the non-snowy season. In particular, the duration and frequency of SBs increased from 30 to 60 min for men and from 60 min or more for women, indicating a trend toward longer SBs among women. Additionally, the number of breaks per hour decreased significantly for both sexes, and SB interruptions were less likely to occur in the snowy season.
Previous studies on seasonal changes in LPA indicated that the time for LPA implementation decreased in winter compared with that in other seasons28, 60). Although differences in measurement time may be observed depending on the activity meter used, LPA decreased by approximately 20%28). The LPA in the snowy season decreased by 18.1% in male participants and 22.2% in female participants compared with that in non-snowy season in the present study, which is similar to the results of previous studies. The decrease in HLPA was particularly large in female participants, with a 28% decrease in HLPA being observed in female participants compared with a 15% decrease being observed in male participants. This HLPA is defined as 2.0–2.9 METs of activity, and housework activities are often included in this intensity49). However, indoor household activities were performed more frequently by the female participants, and there were no seasonal changes in the practice of indoor household chores. One possible reason for the greater decrease in HLPA among the female participants in this study could be attributed to the inclusion of gardening as an outdoor household chore. Although the activities related to gardening depend on the work style, many activities fall in the range of 2.0–2.9 METs61). The exercise intensity of activities wherein older adults carried planters, filled them with soil, and planted flowers is approximately 2.5 METs62). It was inferred that the inability to perform gardening in the snowy season had a significant effect on the decrease in the HLPA.
LPA was significantly reduced in both short and long bouts; however, the amount of change was particularly large in the long bouts. A study examining the relationship of air temperature inside a house with SB and PA reported that a smaller temperature difference between the living and non-residential rooms suppressed SB and promoted PA63). Most houses in Hokkaido are well insulated; however, the difference in room temperature inside the house increases in winter when the outside temperature is below freezing. In addition to a decrease in outdoor activities, differences in room temperature in winter may prolong SB and decrease long bouts of LPA.
Increasing the break frequency is recommended to reduce SB; however, replacing SB with LPA may be beneficial for health outcomes14, 64). In contrast, replacing LPA with SB in the snowy season may hurt health outcomes.
No seasonal differences in MVPA were observed among the male participants; however, the duration and frequency of short bouts of MVPA decreased among the female participants. This may be attributed to the decrease in outdoor activity opportunities during winter. A report examining the relationship between participation in community activities and the amount of PA revealed that participation in community activities increased LPA in addition to short bouts of MVPA, especially among women65). Furthermore, they explained that hobbies did not cause differences in the amount of PA in personal activities as they included activities that did not involve PA65). The present study did not consider participation in community activities; however, the limited opportunities to go outside in the snowy season, such as decreased outdoor household chores and outdoor activities in FAI among the female participants, may have led to a decrease in LPA and short-term MVPA.
A report examining the differences in the number of steps taken in early winter and severe winter and changes in walking speed 1 year later among older adults residing in snowy and cold regions with an average age of 78.4 years revealed that maintaining the number of steps in severe winter had a positive effect on walking speed 1 year later66). The number of steps decreased, SB increased, and LPA decreased in the snowy season in both sexes in this study; however, a decrease in MVPA was observed in the female participants. In addition, the proportion of older adults who performed MVPA for ≥150 minutes per week, as recommended by WHO, decreased from 56% in the non-snowy season to 46% in the snowy season, with a significant decrease being observed only in female participants. These changes may have negative short-term effects on the physical and mental functions of older adults.
DVS decreased only in the male participants, indicating a change other than those in IADL and PA. DVS tends to be low among older men. In addition, factors such as residing alone influence this phenomenon67). However, all male participants of this study had a family member residing with them, suggesting that their diet could change depending on the season even if they had a family member residing with them. The eating environment may have an influence on diet even if a family member is residing with men. Further verification of this possibility is warranted.
Changes in lifestyle and PA during the snowy season must be considered to support the health of older adults residing in snowy and cold regions. However, adhering to the PA recommended by WHO in the snowy season is difficult. In particular, since older adults have difficulty with continuous MVPA18), it is important to provide opportunities for short-bout PA indoor activities that can be traded off with outdoor activities practiced in the non-snowy season. Furthermore, seasonal changes in activity; measures to incorporate break opportunities into daily life to reduce long hours of SB, especially for women; measures to supplement PA that is lacking in indoor household chores only; and measures to increase IADL that men do not practice with individualized support must also be considered.
This study has some limitations. The small sample size of 50 participants is not representative of older adults residing in snowy and cold regions. Thus, caution should be exercised when interpreting the results. In particular, the results may differ from those obtained in urban areas, as this study was conducted in a rural area. The FAI was used to assess lifestyle behaviors; however, the IADL related to the snowy season were not specified. Therefore, the FAI may have underestimated IADL practices in the snowy season. It will be necessary to increase the number of participants and examine whether there are differences in seasonal variations in daily and physical activities among older adults residing in urban and rural areas in snowy and cold regions in the future. Furthermore, IADL assessments suitable for snowy and cold regions to capture daily activities in the snowy season must also be developed.
Conclusion
Seasonal variations in IADL practices and objective PA among older adults residing in non-urban areas of snowy and cold regions were investigated in this study. Compared with those in the non-snowy season, outdoor household chores, outdoor activities, and total FAI scores were significantly lower in the female participants in the snowy season. In terms of PA, the number of steps and LPA decreased and SB time increased in both sexes. HLPA decreased in the female participants in the snowy season; similarly, total and short-bout MVPA were also reduced.
Large changes in lifestyle and PA are observed in the snowy season in snowy and cold regions; thus, it is necessary to formulate strategies to replace PA that is insufficient for women to practice indoor household chores. Participation in indoor household chores that are not practiced by men is considered important.
Conflict of interest
There is no conflict of interest in this study.
Funding information
This study was funded by a research grant from the Center for Advanced Medical Research and Education, Health Sciences, University of Hokkaido.
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee of the Health Sciences University of Hokkaido (23R179233). Informed consent was obtained from all participants after a full disclosure of the aims and procedures of the study.
Consent for publication
Consent was obtained from all co-authors.
Data availability statement
The data that support the findings of this study are available from the corresponding author, Tomohito Tadaishi, upon reasonable request.
Author contributions
T.T.: performed the study, statistical analysis, and wrote the manuscript. J.H. and H.S.: provided critical comments, and approved the final version.
Acknowledgments
The authors would like to express their gratitude to the Senior Citizen Care and Assistant Section of the Town of Tobetsu, Tobetsu Social Welfare Council, and Tobetsu Community Care Center for jointly running the TEHS, which served as the basis of this study.
References
- 1.Cabinet Office White Papers. Annual Report on the Ageing Society. https://www8.cao.go.jp/kourei/english/annualreport/2022/pdf/2022.pdf. Accessed April 1, 2024.
- 2.Ministry of Health, Labour and Welfare. White Papers & Reports. Annual Health, Labour and Welfare Report 2021. Health and welfare services for the elderly. https://www.mhlw.go.jp/english/wp/wp-hw14/dl/10e.pdf. Accessed April 1, 2024.
- 3.e-Stat. National Living Standards Survey 2022. Accessed April 1, 2024 (in Japanese).
- 4.Kojima G, Iliffe S, Taniguchi Y, et al. Prevalence of frailty in Japan: a systematic review and meta-analysis. J Epidemiol 2017; 27: 347–353. doi: 10.1016/j.je.2016.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ensrud KE, Ewing SK, Taylor BC, et al. Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch Intern Med 2008; 168: 382–389. doi: 10.1001/archinternmed.2007.113 [DOI] [PubMed] [Google Scholar]
- 6.Tanaka T, Takahashi K, Akishita M, et al. “Yubi-wakka” (finger-ring) test: a practical self-screening method for sarcopenia, and a predictor of disability and mortality among Japanese community-dwelling older adults. Geriatr Gerontol Int 2018; 18: 224–232. doi: 10.1111/ggi.13163 [DOI] [PubMed] [Google Scholar]
- 7.Yeung SSY, Reijnierse EM, Pham VK, et al. Sarcopenia and its association with falls and fractures in older adults: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle 2019; 10: 485–500. doi: 10.1002/jcsm.12411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim S, Won CW, Kim BS, et al. The association between the low muscle mass and osteoporosis in elderly Korean people. J Korean Med Sci 2014; 29: 995–1000. doi: 10.3346/jkms.2014.29.7.995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sanada K, Miyachi M, Tanimoto M, et al. A cross-sectional study of sarcopenia in Japanese men and women: reference values and association with cardiovascular risk factors. Eur J Appl Physiol 2010; 110: 57–65. doi: 10.1007/s00421-010-1473-z [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Guidelines on Physical Activity and Sedentary Behaviour. https://www.who.int/publications/i/item/9789240015128. Accessed March 25, 2024.
- 11.World Health Organization. Global recommendations on physical activity for health. https://iris.who.int/bitstream/handle/10665/44399/9789241599979_eng.pdf?sequence=1. Accessed December 2, 2023. [PubMed]
- 12.Jefferis BJ, Parsons TJ, Sartini C, et al. Does duration of physical activity bouts matter for adiposity and metabolic syndrome? A cross-sectional study of older British men. Int J Behav Nutr Phys Act 2016; 13: 36. doi: 10.1186/s12966-016-0361-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jakicic JM, Kraus WE, Powell KE, et al. 2018 PHYSICAL ACTIVITY GUIDELINES ADVISORY COMMITTEE*Association between bout duration of physical activity and health: systematic review. Med Sci Sports Exerc 2019; 51: 1213–1219. doi: 10.1249/MSS.0000000000001933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen T, Honda T, Chen S, et al. Dose-response association between accelerometer-assessed physical activity and incidence of functional disability in older Japanese adults: a 6-year prospective study. J Gerontol A Biol Sci Med Sci 2020; 75: 1763–1770. doi: 10.1093/gerona/glaa046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jefferis BJ, Parsons TJ, Sartini C, et al. Objectively measured physical activity, sedentary behaviour and all-cause mortality in older men: does volume of activity matter more than pattern of accumulation? Br J Sports Med 2019; 53: 1013–1020. doi: 10.1136/bjsports-2017-098733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stubbs B, Chen LJ, Chang CY, et al. Accelerometer-assessed light physical activity is protective of future cognitive ability: a longitudinal study among community dwelling older adults. Exp Gerontol 2017; 91: 104–109. doi: 10.1016/j.exger.2017.03.003 [DOI] [PubMed] [Google Scholar]
- 17.Johnson LG, Butson ML, Polman RC, et al. Light physical activity is positively associated with cognitive performance in older community dwelling adults. J Sci Med Sport 2016; 19: 877–882. doi: 10.1016/j.jsams.2016.02.002 [DOI] [PubMed] [Google Scholar]
- 18.Machida M, Takamiya T, Amagasa S, et al. [Descriptive epidemiology of accelerometer-measured moderate to vigorous physical activity in Japanese older adults]. Nihon Ronen Igakkai Zasshi 2018; 55: 584–593 (in Japanese, Abstract in English). doi: 10.3143/geriatrics.55.584 [DOI] [PubMed] [Google Scholar]
- 19.Barnett DW, Barnett A, Nathan A, et al. Council on Environment and Physical Activity (CEPA) – Older Adults working groupBuilt environmental correlates of older adults’ total physical activity and walking: a systematic review and meta-analysis. Int J Behav Nutr Phys Act 2017; 14: 103. doi: 10.1186/s12966-017-0558-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turrisi TB, Bittel KM, West AB, et al. Seasons, weather, and device-measured movement behaviors: a scoping review from 2006 to 2020. Int J Behav Nutr Phys Act 2021; 18: 24. doi: 10.1186/s12966-021-01091-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matthews CE, Freedson PS, Hebert JR, et al. Seasonal variation in household, occupational, and leisure time physical activity: longitudinal analyses from the seasonal variation of blood cholesterol study. Am J Epidemiol 2001; 153: 172–183. doi: 10.1093/aje/153.2.172 [DOI] [PubMed] [Google Scholar]
- 22.McCormack GR, Friedenreich C, Shiell A, et al. Sex- and age-specific seasonal variations in physical activity among adults. J Epidemiol Community Health 2010; 64: 1010–1016. doi: 10.1136/jech.2009.092841 [DOI] [PubMed] [Google Scholar]
- 23.Tudor-Locke C, Bassett DR, Swartz AM, et al. A preliminary study of one year of pedometer self-monitoring. Ann Behav Med 2004; 28: 158–162. doi: 10.1207/s15324796abm2803_3 [DOI] [PubMed] [Google Scholar]
- 24.Clemes SA, Hamilton SL, Griffiths PL. Summer to winter variability in the step counts of normal weight and overweight adults living in the UK. J Phys Act Health 2011; 8: 36–44. doi: 10.1123/jpah.8.1.36 [DOI] [PubMed] [Google Scholar]
- 25.Hamilton SL, Clemes SA, Griffiths PL. UK adults exhibit higher step counts in summer compared to winter months. Ann Hum Biol 2008; 35: 154–169. doi: 10.1080/03014460801908058 [DOI] [PubMed] [Google Scholar]
- 26.O’Connell SE, Griffiths PL, Clemes SA. Seasonal variation in physical activity, sedentary behaviour and sleep in a sample of UK adults. Ann Hum Biol 2014; 41: 1–8. doi: 10.3109/03014460.2013.827737 [DOI] [PubMed] [Google Scholar]
- 27.Cepeda M, Koolhaas CM, van Rooij FJA, et al. Seasonality of physical activity, sedentary behavior, and sleep in a middle-aged and elderly population: The Rotterdam study. Maturitas 2018; 110: 41–50. doi: 10.1016/j.maturitas.2018.01.016 [DOI] [PubMed] [Google Scholar]
- 28.Amagasa S, Inoue S, Murayama H, et al. Changes in rural older adults’ sedentary and physically-active behaviors between a non-snowfall and a snowfall season: compositional analysis from the NEIGE study. BMC Public Health 2020; 20: 1248. doi: 10.1186/s12889-020-09343-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Japan Meteorological Agency. Climate of Japan. https://www.jma.go.jp/jma/kishou/know/kisetsu_riyou/tenkou/Average_Climate_Japan.html. Accessed April 2, 2024 (in Japanese).
- 30.Miyamoto Y. An outline of policy on road management in winter. Journal of Snow Engineering of Japan. 1998; 14: 58–60 (in Japanese). doi: 10.4106/jsse.14.58 [DOI] [Google Scholar]
- 31.Hachisuka K, Saeki S, Tsutsui Y, et al. Gender-related differences in scores of the Barthel Index and Frenchay activities index in randomly sampled elderly persons living at home in Japan. J Clin Epidemiol 1999; 52: 1089–1094. doi: 10.1016/S0895-4356(99)00085-2 [DOI] [PubMed] [Google Scholar]
- 32.Matthews CE, Keadle SK, Troiano RP, et al. Accelerometer-measured dose-response for physical activity, sedentary time, and mortality in US adults. Am J Clin Nutr 2016; 104: 1424–1432. doi: 10.3945/ajcn.116.135129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Osuka Y, Yabushita N, Kim M, et al. Association between habitual light-intensity physical activity and lower-extremity performance: a cross-sectional study of community-dwelling older Japanese adults. Geriatr Gerontol Int 2015; 15: 268–275. doi: 10.1111/ggi.12268 [DOI] [PubMed] [Google Scholar]
- 34.Buman MP, Hekler EB, Haskell WL, et al. Objective light-intensity physical activity associations with rated health in older adults. Am J Epidemiol 2010; 172: 1155–1165. doi: 10.1093/aje/kwq249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chastin SFM, De Craemer M, De Cocker K, et al. How does light-intensity physical activity associate with adult cardiometabolic health and mortality? Systematic review with meta-analysis of experimental and observational studies. Br J Sports Med 2019; 53: 370–376. doi: 10.1136/bjsports-2017-097563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bann D, Hire D, Manini T, et al. LIFE Study Group.Light Intensity physical activity and sedentary behavior in relation to body mass index and grip strength in older adults: cross-sectional findings from the Lifestyle Interventions and Independence for Elders (LIFE) study. PLoS One 2015; 10: e0116058. doi: 10.1371/journal.pone.0116058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Prizer LP, Gay JL, Gerst-Emerson K, et al. The role of age in moderating the association between disability and light-intensity physical activity. Am J Health Promot 2016; 30: e101–e109. doi: 10.4278/ajhp.140225-QUAN-85 [DOI] [PubMed] [Google Scholar]
- 38.Frith E, Loprinzi PD. Accelerometer-assessed light-intensity physical activity and mortality among those with mobility limitations. Disabil Health J 2018; 11: 298–300. doi: 10.1016/j.dhjo.2017.08.007 [DOI] [PubMed] [Google Scholar]
- 39.Ministry of Internal Affairs and Communications Japan. Population, demographics and number of households based on the Basic Resident Ledger. https://www.soumu.go.jp/main_sosiki/jichi_gyousei/daityo/jinkou_jinkoudoutai-setaisuu.html. Accessed April 2, 2024 (in Japanese).
- 40.Japan Meteorological Agency various data. https://www.data.jma.go.jp/stats/etrn/index.php. Accessed April 2, 2024 (in Japanese).
- 41.Suenaga H, Miyanaga K, Chisaka H, et al. Modified version of the self-rating frenchay activites index and its reliability and validity. Jpn J Occup Med Traumatol 2000; 48: 55–60 (in Japanese, Abstract in English). [Google Scholar]
- 42.Holbrook M, Skilbeck CE. An activities index for use with stroke patients. Age Ageing 1983; 12: 166–170. doi: 10.1093/ageing/12.2.166 [DOI] [PubMed] [Google Scholar]
- 43.Hachisuka K, Chisaka H, Kawazu T, et al. Applied activities of daily living and its standard value determined according to frenchay activities index scores for randomly sampled middle and advanced age people living at home. Jpn J Rehabil Med 2001; 38: 287–295 (in Japanese, Abstract in English). doi: 10.2490/jjrm1963.38.287 [DOI] [Google Scholar]
- 44.Kumagai S, Watanabe S, Shibata H, et al. [Effects of dietary variety on declines in high-level functional capacity in elderly people living in a community]. Nihon Koshu Eisei Zasshi 2003; 50: 1117–1124 (in Japanese, Abstract in English). [PubMed] [Google Scholar]
- 45.Burke WJ, Roccaforte WH, Wengel SP. The short form of the Geriatric Depression Scale: a comparison with the 30-item form. J Geriatr Psychiatry Neurol 1991; 4: 173–178. doi: 10.1177/089198879100400310 [DOI] [PubMed] [Google Scholar]
- 46.Sugishita M, Asada T. Development of the Geriatric Depression Scale-Short Version-Japan (GDS-S-J). Jpn J Cognitive Neurosience 2009; 11: 87–90 (in Japanese). [Google Scholar]
- 47.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 1994; 49: M85–M94. doi: 10.1093/geronj/49.2.M85 [DOI] [PubMed] [Google Scholar]
- 48.Chen LK, Woo J, Assantachai P, et al. Asian working group for sarcopenia: 2019 Consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc 2020; 21: 300–307.e2. doi: 10.1016/j.jamda.2019.12.012 [DOI] [PubMed] [Google Scholar]
- 49.Ohkawara K, Oshima Y, Hikihara Y, et al. Real-time estimation of daily physical activity intensity by a triaxial accelerometer and a gravity-removal classification algorithm. Br J Nutr 2011; 105: 1681–1691. doi: 10.1017/S0007114510005441 [DOI] [PubMed] [Google Scholar]
- 50.Park J, Ishikawa-Takata K, Tanaka S, et al. Accuracy of estimating step counts and intensity using accelerometers in older people with or without assistive devices. J Aging Phys Act 2017; 25: 41–50. doi: 10.1123/japa.2015-0201 [DOI] [PubMed] [Google Scholar]
- 51.Mâsse LC, Fuemmeler BF, Anderson CB, et al. Accelerometer data reduction: a comparison of four reduction algorithms on select outcome variables. Med Sci Sports Exerc 2005; 37(Suppl): S544–S554. doi: 10.1249/01.mss.0000185674.09066.8a [DOI] [PubMed] [Google Scholar]
- 52.Chudyk AM, McAllister MM, Cheung HK, et al. Are we missing the sitting? Agreement between accelerometer non-wear time validation methods used with older adults’ data. Cogent Med 2017; 4: 1313505. doi: 10.1080/2331205X.2017.1313505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Heesch KC, Hill RL, Aguilar-Farias N, et al. Validity of objective methods for measuring sedentary behaviour in older adults: a systematic review. Int J Behav Nutr Phys Act 2018; 15: 119. doi: 10.1186/s12966-018-0749-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Izawa KP, Shibata A, Ishii K, et al. Associations of low-intensity light physical activity with physical performance in community-dwelling elderly Japanese: a cross-sectional study. PLoS One 2017; 12: e0178654. doi: 10.1371/journal.pone.0178654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Owen N, Healy GN, Matthews CE, et al. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev 2010; 38: 105–113. doi: 10.1097/JES.0b013e3181e373a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Japan Physical Activity Research Platformhttp://paplatform.umin.jp. Accessed March 1, 2024.
- 57.Mizumoto A, Ihira H, Makino K, et al. Interpreting the NHK Japanese Time Use Survey [Part I]. The Lives of the Elderly in Japan’s “Super-Graying Society”.. BMC Geriatr 2015; 15: 43. doi: 10.1186/s12877-015-0034-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yoshifuji M, Watanabe Y. Reading from the national living time survey (1) life in old age in “super-aging society” nippon. The NHK Monthly Report on Broadcast Research 2017; 67: 2–19 (in Japanese, Abstract in English). [Google Scholar]
- 59.Arnardottir NY, Oskarsdottir ND, Brychta RJ, et al. Comparison of summer and winter objectively measured physical activity and sedentary behavior in older adults: age, gene/environment susceptibility Reykjavik study. Int J Environ Res Public Health 2017; 14: 1268. doi: 10.3390/ijerph14101268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nakashima D, Kimura D, Watanabe H, et al. Influence of seasonal variations on physical activity in older people living in mountainous agricultural areas. J Rural Med 2019; 14: 165–175. doi: 10.2185/jrm.3003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Park SA, Shoemaker CA, Haub MD. A preliminary investigation on exercise intensities of gardening tasks in older adults. Percept Mot Skills 2008; 107: 974–980. doi: 10.2466/pms.107.3.974-980 [DOI] [PubMed] [Google Scholar]
- 62.Knaggs JD, Larkin KA, Manini TM. Metabolic cost of daily activities and effect of mobility impairment in older adults. J Am Geriatr Soc 2011; 59: 2118–2123. doi: 10.1111/j.1532-5415.2011.03655.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ito M, Ikaga T, Oguma Y, et al. Heating use and sedentary behavior and physical activity at home among adults in winter: a cross-sectional analysis of the nationwide smart wellness housing survey in Japan. Jpn Assoc Exercise Epidemiology 2021; 23: 45–56 (in Japanese, Abstract in English). [Google Scholar]
- 64.Diaz KM, Howard VJ, Hutto B, et al. Patterns of sedentary behavior and mortality in U.S. middle-aged and older adults: a national cohort study. Ann Intern Med 2017; 167: 465–475. doi: 10.7326/M17-0212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Amagasa S, Kikuchi H, Fukushima N, et al. Types of social participation and patterns of objectively determined sedentary behavior and physical activity in community-dwelling older adults. Jpn Assoc Exercise Epidemiology 2018; 20: 5–15 (in Japanese, Abstract in English). [Google Scholar]
- 66.Mizumoto A, Ihira H, Makino K, et al. Physical activity during winter in old-old women associated with physical performance after one year: a prospective study. Curr Gerontol Geriatr Res 2015; 2015: 253451. doi: 10.1155/2015/253451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yokoro M, Otaki N, Yano M, et al. Associations between dietary variety and frailty in community-dwelling older people who live alone: gender differences. J Frailty Aging 2023; 12: 30–36. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, Tomohito Tadaishi, upon reasonable request.