Abstract
Objective:
Recent studies found that recreational legalization of cannabis consumption for Canadian adults has increased presentation to the emergency department (ED) among children. In this descriptive study, our objectives were to (1) understand Canadian pediatric emergency medicine (PEM) providers' training and knowledge of clinical presentations associated with cannabis exposure in children and (2) describe pediatric ED presentations related to cannabis exposure across Canada following legalization in 2018.
Method:
In 2021, following ethics board approval, 230 Pediatric Emergency Research Canada (PERC) network pediatric emergency medicine (PEM) physicians were invited to share about their knowledge, training, and experience with patients presenting with cannabis-associated emergencies using an anonymized survey administered through REDCap.
Results:
In total, 84/230 (36.5%) invited physicians completed the survey. Almost 70% of the PEM physicians reported an increase in the number of cannabis-associated ED presentations they have seen since legalization, while only 15% reported no increase in presentations. More than 90% of the respondents reported an average or higher level of knowledge of cannabis-associated pediatric emergencies. More than half (n = 48, 57%) were interested in pursuing further training, preferring formal training opportunities. The main presentations to the ED were decreased level of consciousness, known unintentional (accidental) ingestion and vomiting. Significantly more tests were ordered when cannabis consumption was unknown at the beginning of the assessment, compared to when it was known, however, treatment plans were the same (mainly supportive measures).
Conclusions:
Most PEM providers are managing an increasing number of cannabis-associated ED presentations. PEM providers should improve communication with caregivers around household cannabis use. When caregivers feel comfortable disclosing cannabis presence at home, it can help prevent unnecessary tests and interventions for their children if they present to the ED.
Keywords: cannabis, pediatrics, emergency medicine, cannabis exposure, clinical knowledge
In Canada, the recreational use of cannabis amongst adults was legalized by the federal government in October 2018. However, the recreational use of cannabis is prohibited for those younger than 18–21 years, depending on the province (Cannabis Act, 2018). Since legalization of recreational cannabis, the rates of cannabis use among 16–19-year-olds has significantly increased. According to the 2023 Canadian Cannabis Survey, 43% of 16–19-year-olds reported using cannabis in the past 12 months, compared to 37% in 2022, and 36% in 2018 (Government of Canada, 2024).
Recent data from the US and Canada found that following cannabis legalization, emergency department (ED) presentations among children under 18 increased (Cohen et al., 2022; Kim & Monte, 2016; Thomas, Dickerson-Young, & Mazor, 2021; Yeung, Weaver, Hartmann, Haines-Saah, & Lang, 2021), as did intensive care unit (ICU) admissions for children related to cannabis exposures (Cohen et al., 2022). For Canadian children presenting to EDs, having a chronic disease or a history of psychiatric disorders and oral route of cannabis exposure have been shown to predict ICU admission (Cohen et al., 2022). A retrospective chart review found that the most frequently presenting symptoms were altered level of consciousness (76%), lethargy/somnolence (59%), and vomiting (30%; Coret & Rowan-Legg, 2022). Though knowledge about cannabis exposure in children is increasing, it remains important to determine how emergency physicians are currently diagnosing and treating these children in Canada.
Outcomes of cannabis ingestion in children include both potentially life-threatening adverse events and short-term toxicities (Campbell, Phillips, & Manasco, 2017; Schonhofen et al., 2018; Volkow, Baler, Compton, & Weiss, 2014). There is also the potential of long-term disruption of the endocannabinoid system, which may impair neurodevelopment (Campbell et al., 2017; Schonhofen et al., 2018; Volkow et al., 2014). As such, it is key that physicians are skilled in assessing and managing patients with cannabis-associated medical emergencies. We need to identify the knowledge baseline and the training for those who may respond to cannabis-related presentations in emergency settings.
Our goals with this cross-sectional study were to (1) understand Canadian pediatric emergency medicine physicians' training and knowledge of clinical presentations associated with cannabis exposure in children post-legalization and (2) describe pediatric emergency department presentations related to cannabis exposure across Canada.
METHODS
Study Design
We completed a cross-sectional survey of pediatric emergency medicine (PEM) physicians across Canada on their knowledge, training, and experience with patients presenting with cannabis-associated emergencies. The online survey was developed and tested with local faculty prior to being disseminated for a two-month data collection window. Ethics approval was obtained by the University of Manitoba Health Research Ethics Board.
Participants
The study population was the 230 physician members of the Pediatric Emergency Research Canada (PERC) network who were invited to participate in an online, de-identified survey in 2021. “PERC is a well-established network of health care researchers across 15 Canadian children's hospitals that is dedicated to improving pediatric emergency care through collaborative multi-centre research” (PERC, 2023). The survey had a 36.5% response rate (84/230), comparable to other online survey studies (Cunningham et al., 2015; Wu, Zhao, & Fils-Aime, 2022).
Survey Development
The survey was adapted from an existing survey of Canadian pediatric oncologists and pediatric palliative care physicians caring for children with cancer (Oberoi et al., 2022). The existing survey was developed via a Delphi protocol (Burns et al., 2008), with item generation via literature review and expert opinion, then item reduction via expert panel focus groups at a 2019 in-person conference (Oberoi et al., 2022). Additional clinical survey items were added based on existing literature describing pediatric cannabis presentations (Cameron, Finkelstein, & Leslie, 2020; Richards, Smith, & Moulin, 2017) and focus groups between three investigators (SGP, LK, LW), as well as questions regarding knowledge and training. A panel of experts (Canadian PEM physicians, toxicologists, and researchers) reviewed the survey and provided feedback individually.
The survey was divided into three sections: (1) professional background and demographics; (2) cannabis knowledge and training; and (3) cannabis-associated pediatric emergencies. Examples of survey questions regarding cannabis knowledge and training include “How would you measure your current level of knowledge regarding cannabis-associated pediatric emergencies?” and “Would you be interested in pursuing further training about cannabis-associated pediatric emergencies?” Examples of survey questions regarding cannabis-associated pediatric emergencies include “How many patients have you cared for with cannabis-associated ED presentations since October 2018?” and “Please think of a case when cannabis consumption was known at the beginning of your assessment. In your evaluation of this patient, which investigations did you order?”
Lastly, we completed a pilot test of the survey with a group of 10 PEM physicians and subspecialty trainees. The survey was translated into French and was available in both official languages.
Survey Distribution
We contacted PERC members by e-mail, utilizing a database provided by the PERC coordinator. Upon registration, PERC members consent to being contacted by email for such research surveys; thus, consent was implied in completion of the survey. The survey was viewed and approved by the PERC Executive Committee prior to distribution. Data were collected and stored on the Research Electronic Data Capture (REDCap; Harris et al., 2009) secure web-based platform hosted at the University of Manitoba. An automated introductory e-mail describing the study and containing the survey link was sent to all PERC members. Two reminder e-mails were sent to non-respondents. The survey data collection concluded after 8 weeks. The de-identified survey responses were entered directly by the participants into REDCap.
Data Analysis
Frequency distributions and percentages were produced using REDCap. Response rate was calculated, and descriptive statistics were used to report on the respondents' demographic characteristics, their knowledge and training, as well as their experience with cannabis exposure in pediatric EDs. Descriptive tables and figures were generated using Excel.
RESULTS
Demographics
Table 1 presents the characteristics of the physicians who completed the survey. Ninety-one percent (n = 76) of respondents completed the survey in English and 9% (n = 7) completed the survey in French. Overall, the physicians who completed the survey worked across 15 children's hospitals in eight provinces. Eighty-six percent (n = 72) of respondents completed medical school in Canada, and 77% (n = 65) completed their postgraduate medical training in Canada. Regarding years of experience as a PEM attending physician, there was a wide range in career length. The number of shifts worked per month had similar wide variation.
Table 1.
Demographic and Professional Background of Respondents
| Characteristic | Number of respondents (%) |
|---|---|
| Gender | |
| Female | 50 (59.5) |
| Male | 33 (39.3) |
| Prefer not to answer | 1 (1.2) |
| Medical practice location for PERC site | |
| British Columbia | 7 (8.3) |
| Alberta | 16 (19.0) |
| Saskatchewan | 3 (3.6) |
| Manitoba | 3 (3.6) |
| Ontario | 25 (29.8) |
| Quebec | 18 (21.4) |
| Nova Scotia | 8 (9.5) |
| Newfoundland and Labrador | 4 (4.8) |
| Highest level of Post Graduate Medical training | |
| Clinical fellowship (e.g. simulation, Point-of-care ultrasonography) | 2 (2.4) |
| Emergency medicine residency only | 11 (13.1) |
| Pediatric residency only | 9 (10.7) |
| Emergency medicine residency with pediatric emergency medicine fellowship | 3 (3.6) |
| Pediatric residency with pediatric emergency medicine fellowship | 56 (66.7) |
| Other | 3 (3.6) |
| Years practicing as an attending physician in PEM | |
| I am a trainee | 2 (2.4) |
| 0-5 years | 12 (14.3) |
| 6-15 years | 36 (42.9) |
| 16-30 years | 33 (38.1) |
| More than 30 years | 2 (2.4) |
| Shifts in PEM department in a typical month | |
| 1-5 | 15 (17.9) |
| 6-10 | 38 (45.2) |
| 11-15 | 29 (34.5) |
| More than 15 | 1 (1.2) |
| None | 1 (1.2) |
Out of the 84 respondents, 91.7% (n = 77) reported an average or higher level of knowledge on cannabis-associated pediatric emergencies. Only 8.3% (n = 7) of the physicians reported a poor level of knowledge.
Eighty-six percent (n = 72) of physicians responded that they had received some informal training such as personal reading, morning rounds, and discussion with a toxicologist. In comparison, 35% (n = 29) of respondents received some formal training in the form of grand rounds, conferences, workshops, and online approved courses. Most formal or informal training was within 1–5 years (n = 52, 64%) or within the last year (n = 29, 36%).
More than half (n = 48, 57%) reported to be interested in pursuing further training. Additionally, almost 28% (n = 23) said that they may be interested in further training, depending on the topic, and/or duration of the training session. When asked what learning topics would interest them, “clinical presentations and management recommendations” was selected as the topic of greatest interest (n = 77). “Review of federal and provincial cannabis legislation” (n = 26) and “pharmacology of cannabis” (n = 27) were selected by the respondents as the least interesting topics for training. See Table 2 for the full distribution of interest in different learning topics.
Table 2.
Topics in Which PEM Physicians in Canada Would Like More Training
| Topics for training | Number of respondents (%) |
|---|---|
| Clinical presentations and management recommendations | 77 (91.7) |
| Toxicology/pathophysiology | 52 (61.9) |
| Utilization of medical cannabis in the pediatric population | 45 (53.6) |
| Pharmacology of cannabis | 27 (32.1) |
| Review of federal and provincial cannabis legislation | 26 (31.0) |
| Other | 6 (7.1) |
| Don't know | 2 (2.4) |
Participants were also asked what format or method of training they would prefer. “Local PEM rounds, department grand rounds, or other scheduled department teaching” (n = 59) was the preferred method of training. “Videos” (n = 21) and “published literature” (n = 23) were the least preferred methods of training. See Table 3 for a full distribution of preferred method of training.
Table 3.
Physicians' Preferred Method or Format of Training
| Format of training | Number of respondents (%) |
|---|---|
| Local PEM rounds, grand rounds or other scheduled department teaching | 59 (70.2) |
| Live webinar | 39 (46.4) |
| In-person (e.g. at a conference, PERC meeting) | 35 (41.7) |
| Online print material/infographics | 33 (39.3) |
| Published literature (e.g. studies, systematic reviews) | 23 (27.4) |
| Video | 21 (25.0) |
| Do not feel additional training is needed | 2 (2.4) |
| Unsure | 2 (2.4) |
| Other | 1 (1.2) |
Experience With Cannabis-Associated Pediatric Emergencies
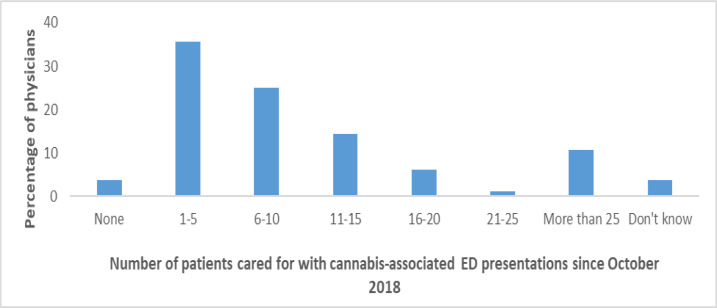
We asked respondents if they thought that they had seen an increase in the number of cannabis-associated ED presentations from October 2018 to the time of survey completion. Out of 84 respondents, 58 (69%) said yes, 13 (15.5%) said no, and 13 (15.5%) said that they do not know. Most respondents reported that they recall caring for 1–5 patients (n = 30, 35.7%) or 6–10 patients (n = 21, 25%) with cannabis-associated ED presentations since October 2018 (see Figure 1). Those who had cared for patients with cannabis-associated ED presentations (n = 81) indicated that most of their patients were adolescents, ages 13-18 (n = 54, 64.3%), and toddlers, ages 1-4 (n = 47, 56%). Less common were infant patients, 12 months and younger (n = 8, 9.5%), and young children, ages 5–12 (n = 8, 9.5%).
Figure 1.
Physician Reported Number of Patients Cared for Cannabis-Associated ED Presentations Between October 2018 and July-September 2021
Respondents were asked to select all of the primary presenting complaints for the patients they have seen with cannabis-associated ED presentations. Responses were broken down into seven categories (cannabis use, neurologic, respiratory, gastrointestinal, cardiac, psychiatric, and injury), with a further 23 subcategories.
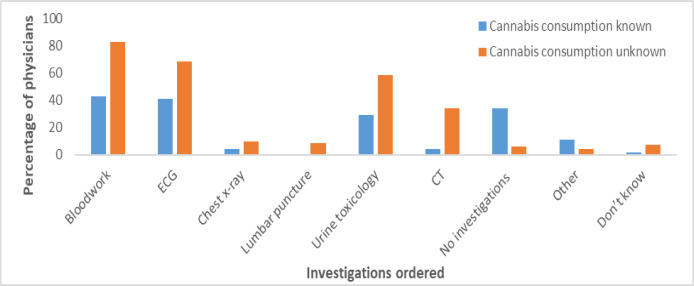
The top presenting complaints were decreased level of consciousness (neurologic; n = 64, 76.2%), known unintentional (accidental) ingestion (cannabis use; n = 59, 70.2%), and vomiting (gastrointestinal; n = 59, 70.2%). See Table 4 for additional presenting complaints. Physicians were asked which investigations they ordered for patients for whom cannabis consumption was not known (n = 70) at the beginning of the assessment. They reported ordering a total of 196 tests (average of 2.8 investigations per presentation). The most frequently ordered tests were bloodwork (n = 58, 82.9%), ECG (n = 48, 68.6%), and urine toxicology screen (n = 41, 58.6%).
Table 4.
Primary Presenting Complaints for Patients With Cannabis-Associated ED Presentations
| Primary presenting complaints | Number of respondents (%) |
|---|---|
| Cannabis use | |
| Known unintentional (accidental) ingestion, or advised by Poison Control/Public Health to present to the ED | 59 (70.2) |
| Cannabis intoxication | 52 (61.9) |
| Cannabis withdrawal | 11 (13.1) |
| Neurologic | |
| Decreased level of consciousness | 64 (76.2) |
| Agitation or hyperactivity | 31 (36.9) |
| Dizziness, Syncope | 23 (27.4) |
| Seizures | 7 (8.3) |
| Headache | 7 (8.3) |
| Respiratory | |
| Respiratory distress | 7 (8.3) |
| Apnea | 5 (6.0) |
| Cough | 4 (4.8) |
| Gastrointestinal | |
| Vomiting | 59 (70.2) |
| Abdominal pain | 26 (31) |
| Cardiac | |
| Palpitations | 23 (27.4) |
| Chest pain | 9 (10.7) |
| Psychiatric | |
| Anxiety | 44 (52.4) |
| Psychosis | 30 (35.7) |
| Paranoia | 29 (34.5) |
| Depression | 26 (31) |
| Suicidal ideation | 22 (26.2) |
| Injury | |
| Traumatic head injury | 6 (7.1) |
| Musculoskeletal injury | 4 (4.8) |
| Multi-trauma | 1 (1.2) |
Interestingly, similar results were observed when cannabis consumption was known at the start of the assessment (n = 72). Blood work (n = 31, 42.5%) and ECG (n = 30, 41.1%) were the most ordered tests for these patients; however, the total number of tests ordered when cannabis consumption was known was 122, for an average of 1.7 tests per presentation.
Additionally, 25 physicians reported that they conducted no investigations if the cannabis consumption was known at the beginning of the assessment, compared to four physicians who reported that they conducted no investigations if the cannabis consumption was not known at the beginning of the assessment. Figure 2 shows investigations that were ordered when cannabis consumption was known versus unknown.
Figure 2.
Investigations Ordered When Cannabis Consumption Known Versus Unknown
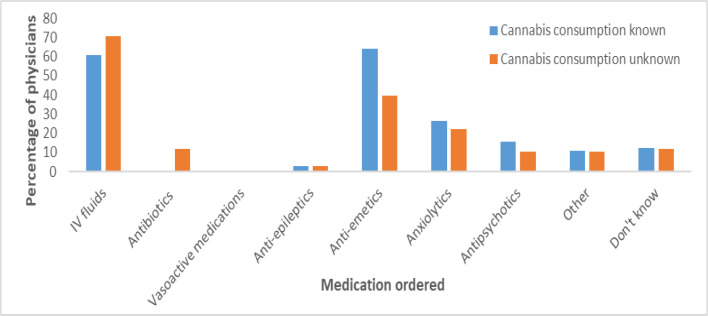
Physicians were asked which medications they ordered for patients with cannabis-related presentations, as shown in Figure 3. Overall, when consumption was not known at the beginning of their assessment, a total of 124 medications were ordered (n = 64), and when consumption was known, 122 medications were ordered (n = 68). More specifically, the results are very similar whether the cannabis consumption was known or not at the assessment. The most commonly ordered medications were IV fluids (n = 48, 70.6%; n = 39, 60.9%) and anti-emetics (n = 27, 39.7%; n = 41, 64.1%). Anti-emetics were ordered more frequently for patients with known cannabis consumption, and more IV fluids were ordered when cannabis consumption was not known.
Figure 3.
Medications Ordered When Cannabis Consumption Known Versus Unknown
Physicians were asked about the disposition plans for the patients they saw with cannabis-associated ED presentations (n = 80). The most common response was discharge (n = 71, 88.8%), followed by admission to medicine ward (n = 44, 55%; see Table 5).
Table 5.
Physician Reported Disposition Plan for Cannabis-Associated ED Presentations
| Disposition plans for the patients seen with cannabis-associated ED presentations | Number of responses (%) |
|---|---|
| Discharge home | 71 (88.8) |
| Admission to medicine ward | 44 (55) |
| Admission to psychiatric ward | 15 (18.8) |
| Admission to intensive care unit | 12 (15) |
| Transfer to another facility | 3 (3.8) |
| Other | 0 |
| Don't know | 0 |
DISCUSSION
Knowledge and Training in Cannabis-Associated Pediatric Emergencies
This is the first Canadian national survey on training and knowledge related to cannabis exposure in children. We learned that most PEM physicians believe they have an average or higher knowledge level on cannabis-associated pediatric emergencies, and about half are interested in pursuing further training. The most desirable subject for further training was “clinical presentations and management recommendations.” These results are noteworthy, as they show that PEM physicians want to learn about when cannabis can be used safely, in addition to what to do in cases of unsafe consumption. Clinical presentations and management recommendations along with other highly rated topics can inform the development of continuing education.
These results enhance our understanding of what and how PEM physicians want to learn about cannabis-associated pediatric emergencies. Physicians reported that training on cannabis-related emergencies was mostly informal within the last one to five years–a possible response to legalization, with physicians desiring more knowledge as access to cannabis increased. This finding also points to a potential gap in training opportunities for physicians–when asked their preferred method of training, most physicians selected formal training such as scheduled rounds and presentations. Universities and networks such as PERC and CAEP (Canadian Association of Emergency Physicians) should include cannabis as a subject in future educational activities, in addition to medical school training.
Experience With Cannabis-Associated Pediatric Emergencies
The main cannabis-related presentations to the pediatric ED were decreased level of consciousness and vomiting. Most patients experienced unintentional exposures and signs of intoxication. These findings are consistent with a retrospective cohort study in Canadian children (Cohen et al., 2022). This research contributes to the ongoing gathering of data describing how pediatric patients present with cannabis consumption. It also provides an insight into how physicians respond to these presentations, for example, what types of investigations and interventions they order. Bloodwork and ECG were the most commonly ordered investigations, whether cannabis consumption was known or unknown. A retrospective chart review found similar results, with bloodwork being most common, followed by cannabinoid urine toxicology and ECG (Coret & Rowan-Legg, 2022). Recent reports did not identify an effective anti-emetic for cannabis hyperemesis syndrome, and diagnosis of pediatric cannabis hyperemesis is not well characterized, highlighting an urgent need for pragmatic treatment solutions (Lonsdale et al., 2021).
Not surprisingly, most of the pediatric patients were adolescents (13–18yo) and toddlers (1–4yo). While it was beyond the scope of this initial study to account for the wide range of pediatric patients, a future study could compare tests and medications ordered, as well as outcomes for adolescents versus toddlers.
Significantly more tests were ordered when cannabis consumption was unknown at the beginning of the assessment compared to when it was known (as is standard of care for a pediatric patient presenting with severe symptoms of unknown etiology, such as altered level of consciousness). It is also not surprising that blood work and urine toxicology were ordered as part of the investigation when cannabis consumption was unknown. These patterns signal the need for strategies to improve disclosure rates, which could reduce unnecessary testing for children. The main disposition plan for patients who are seen with cannabis-associated ED presentations was discharge home; however, there were also patients requiring intensive care admission.
Limitations and Future Research
There are a few limitations of this study. First, we expected a higher response rate for our survey, given that the participant population was a network of academic pediatric emergency physicians. Our response rate did, however, align with other e-mail survey studies (Cunningham et al., 2015; Wu et al., 2022). The timing of data collection may have impacted our response rate; the survey was distributed over the summer months and 12 “out of office” emails were received. Second, the survey collected self-reported data that relied on recall, and participants might not have accurately remembered the past events or experiences. Third, this is a descriptive study that aimed to explore clinical presentations of cannabis exposure in children, and physicians' knowledge and training related to this topic. We wanted a comprehensive understanding as there is no available research on the training and education for ED physicians on cannabis exposure in children, particularly following legalization in 2018.
Future research should consider a quantitative approach to determine whether the number of children presenting to the ED with cannabis exposure is significantly different following legalization, and to test whether the management of cases is significantly different if cannabis exposure is known. Future research should also explore how physicians communicate with parents of children with cannabis-related emergencies: how cannabis ingestion is discussed, what resources are provided, and what tools could be developed to improve communication.
Conclusion
This report provides a snapshot of cannabis-related pediatric presentations to the emergency department post-legalization. We have learned that there is a need for more education opportunities for PEM physicians. Despite most respondents believing to have an average or higher level of knowledge on cannabis-associated pediatric emergencies, there is an interest for further formal training. PEM providers must improve communication with caregivers and on a societal level; it is prudent to reduce stigma of household cannabis use. If caregivers feel more comfortable disclosing the presence of cannabis products in the home, their child may avoid unnecessary tests and interventions.
Funding and Acknowledgements:
No funding was received for this project. Lauren E. Kelly is the Scientific Director for The Canadian Collaborative for Childhood Cannabinoid Therapeutics (C4T) academic research team. She holds funding from the Canadian Institutes of Health Research, Canadian Cancer Society, Research Manitoba, the Sick Kids Foundation, the Children's Hospital Research Institute of Manitoba, the University of Manitoba and a Mitacs Accelerate award in partnership with Canopy Growth. Dr. Kelly was a member of the Scientific Advisory Board for Health Products Containing Cannabis at Health Canada and is president elect for the Board of Directors of the Canadian Consortium for the Investigation of Cannabinoids (CCIC). She has no financial conflicts of interest related to this work. The other authors declare no conflicts of interest. We would like to thank all the physicians who completed the survey and PERC for facilitating the survey.
REFERENCES
- Burns, K. E., Duffett, M., Kho, M. E., Meade, M. O., Adhikari, N. K., Sinuff, T., & Cook, D. J. (2008). A guide for the design and conduct of self-administered surveys of clinicians. Canadian Medical Association Journal, 179(3), 245–252. doi: 10.1503/cmaj.080372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron, C., Finkelstein, Y., & Leslie, K. (2020). The impact of cannabis use—a tertiary care paediatric hospital's experience and approach. Paediatrics & Child Health, 25(Supplement_1), S10–S13. 10.1093/pch/pxaa040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, C. T., Phillips, M. S., & Manasco, K. (2017). Cannabinoids in pediatrics. The Journal of Pediatric Pharmacology and Therapeutics, 22(3), 176–185. 10.5863/1551-6776-22.3.176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Canada. (2024, January 18). Canadian Cannabis Survey 2023: Summary. https://www.canada.ca/en/health-canada/services/drugs-medication/cannabis/research-data/canadian-cannabis-survey-2023-summary.html#s5
- Cannabis Act, S.C. 2018, c. 16 (2018). https://laws-lois.justice.gc.ca/eng/acts/C-24.5/
- Cohen, N., Galvis Blanco, L., Davis, A., Kahane, A., Mathew, M., Schuh, S., Kestenbom, I., Test, G., Pasternak, Y., Verstegen, R. H. J., Jung, B., Maguire, B., d'Astous, S. R., Rumantir, M., & Finkelstein, Y. (2022). Pediatric cannabis intoxication trends in the pre and post-legalization era. Clinical Toxicology, 60(1), 53–58. 10.1080/15563650.2021.1939881 [DOI] [PubMed] [Google Scholar]
- Coret, A., & Rowan-Legg, A. (2022). Unintentional cannabis exposures in children pre- and post-legalization: A retrospective review from a Canadian paediatric hospital. Paediatrics & Child Health, 27(5), 265–271. 10.1093/pch/pxab090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham, C. T., Quan, H., Hemmelgarn, B., Noseworthy, T., Beck, C. A., Dixon, E., … Jetté, N. (2015). Exploring physician specialist response rates to web-based surveys. BMC Medical Research Methodology, 15(1), 32. 10.1186/s12874-015-0016-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, H. S., & Monte, A. A. (2016). Colorado Cannabis Legalization and Its Effect on Emergency Care. Annals of Emergency Medicine, 68(1), 71–75. 10.1016/j.annemergmed.2016.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lonsdale, H., Kimsey, K. M., Brown, J. M., Dey, A., Peck, J., Son, S., & Wilsey, M. (2021). Pediatric cannabinoid hyperemesis: A single institution 10-year case series. Journal of Adolescent Health, 68(2), 255–261. 10.1016/j.jadohealth.2020.09.024 [DOI] [PubMed] [Google Scholar]
- Oberoi, S., Protudjer, J. L., Rapoport, A., Rassekh, S. R., Crooks, B., Siden, H., … Balneaves, L. G. (2022). Perspectives of pediatric oncologists and palliative care physicians on the therapeutic use of cannabis in children with cancer. Cancer Reports, 5(9), e1551. 10.1002/cnr2.1551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pediatric Emergency Research Canada (PERC). About Us. (n.d.). https://perc-canada.ca/
- Richards, J. R., Smith, N. E., & Moulin, A. K. (2017). Unintentional cannabis ingestion in children: a systematic review. The Journal of Pediatrics, 190, 142–152. 10.1016/j.jpeds.2017.07.005 [DOI] [PubMed] [Google Scholar]
- Schonhofen, P., Bristot, I. J., Crippa, J. A., Hallak, J. E. C., Zuardi, A. W., Parsons, R. B., & Klamt, F. (2018). Cannabinoid-based therapies and brain development: potential harmful effect of early modulation of the endocannabinoid system. CNS drugs, 32(8), 697–712. 10.1007/s40263-018-0550-4 [DOI] [PubMed] [Google Scholar]
- Thomas, A. A., Dickerson-Young, T., & Mazor, S. (2021). Unintentional pediatric marijuana exposures at a tertiary care children's hospital in Washington State: A Retrospective Review. Pediatric Emergency Care, 37(10), e594–e598. 10.1097/pec.0000000000001703 [DOI] [PubMed] [Google Scholar]
- Volkow, N. D., Baler, R. D., Compton, W. M., & Weiss, S. R. (2014). Adverse health effects of marijuana use. New England Journal of Medicine, 370(23), 2219–2227. 10.1056/NEJMra1402309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, M.-J., Zhao, K., & Fils-Aime, F. (2022). Response rates of online surveys in published research: A meta-analysis. Computers in Human Behavior Reports, 7, 100206. 10.1016/j.chbr.2022.100206 [DOI] [Google Scholar]
- Yeung, M. E. M., Weaver, C. G., Hartmann, R., Haines-Saah, R., & Lang, E. (2021). Emergency Department Pediatric Visits in Alberta for Cannabis After Legalization. Pediatrics, 148(4). 10.1542/peds.2020-045922 [DOI] [PubMed] [Google Scholar]