Abstract
Objective:
The physician order for life-sustaining treatment has been implemented in clinical practice for several years. However, the determination that a patient is in the terminal phase of life, a prerequisite for the withdrawal of life-sustaining treatment, lacks objective criteria. This study aimed to evaluate whether hyperlactatemia could serve as a reliable objective indicator for determining the terminal phase.
Methods:
In this retrospective cohort study, we included 73,927 patients admitted to our institution from 2018 to 2023 who had at least one blood lactate measurement. We collected data on the highest blood lactate level measured during hospitalization, mortality, medical department, and intensive care unit (ICU) details. The primary endpoint was 30-day mortality, and we analyzed how well the highest lactate level during hospitalization predicted 30-day mortality across different age groups, medical departments, and ICUs.
Results:
Among the patients, 5493 died within 30 days of the maximum lactate measurement. The area under the receiver operating characteristic curve (AUROC) for predicting 30-day mortality based on the maximum lactate level was 0.870 (95% confidence interval [CI] 0.865–0.875) in all patients, indicating high accuracy. Setting the cutoff for the maximum lactate level at 20 mmol/L resulted in a precision of 87% and specificity of 99.8%. Subgroup analyses by age, medical department, and ICU yielded consistent results.
Conclusions:
Severe hyperlactatemia during hospitalization showed high precision and specificity for predicting 30-day mortality across various patient groups. These findings suggest that hyperlactatemia could serve as an objective auxiliary indicator for determining the terminal phase, potentially improving consistency in end-of-life decision-making in clinical practice.
Keywords: Lactate, terminally ill, terminal care, resuscitation orders, data warehousing
Introduction
In order to respect patients’ wishes regarding the extent of life-sustaining treatment under terminal conditions, the physician order for life-sustaining treatment (POLST) law was established.1,2 Although POLST has been practised in several Western countries for more than 15 years, it has been legally implemented in South Korea only since 2018 marking the seventh year of its enforcement. According to the POLST law, futile life-sustaining treatment can be discontinued if the patient has previously expressed their wish not to receive such treatment in their advance directive or if the patient is unable to express their wishes and the family has stated that the patient had previously expressed a similar intent. For the cessation of futile life-sustaining treatment to be carried out, two physicians, including one specialist, must agree that the patient is in the terminal phase of life.
However, determining whether a patient is in the terminal phase can be challenging. Assessing whether a patient is in the terminal phase––where ongoing or future interventions and treatments will no longer be meaningful––is a complex process, and physicians often find it difficult to be confident in their decisions. The decision in the end-of-life care can be psychologically burdensome for health care providers. This consideration led the authors to explore the need for an objective indicator to help determine whether a patient is in the terminal phase or has a very high likelihood of dying soon.
A review of the literature reveals that there are currently no objective criteria for determining whether a patient is in the terminal phase, at which further medical interventions cannot prevent imminent death. While some studies mention subjective symptoms such as dyspnea, decreased consciousness, and hypotension, these findings are not based on objective, measurable criteria, making them less reliable and reproducible in clinical settings.3,4
Therefore, this investigation aimed to evaluate the possibility and appropriateness of using serum lactate levels––an important test in critical care for assessing patient status and prognosis––to determine the likelihood of imminent death. Additionally, if possible, we aimed to propose a lactate level threshold that is clinically practical.
Methods
Clinical data warehouse (CDW)
Seoul National University Bundang Hospital is a tertiary referral hospital that receives and treats patients transferred from university hospitals and small to medium-sized hospitals nationwide. The electronic medical records (EMRs) of our institution were integrated with the CDW database. The CDW database stores data collected since the hospital's opening in 2003 and allows data extraction based on EMRs generated up to the day before the extraction date. The current CDW database provides only encrypted virtual medical record numbers for each research session, without the patient's name or medical record number.
Study subjects
The data for this study were extracted from the CDW database linked to the EMR system of Seoul National University Bundang Hospital. The study subjects were patients admitted to the hospital between January 2018 and December 2023 who had at least one serum lactate measurement. The CDW provided data on patient age, sex, admission and discharge information, medical departments, and ICU admission and discharge histories. This study received approval from Seoul National University Bundang Hospital Institutional Review Board (SNUBH IRB) prior to initiation (title: Research on the Usefulness of Blood Lactate Concentration as a Predictor of Mortality Discharge: A CDW Based Study). As a retrospective cohort study, the requirement to obtain individual patient consent was waived by SNUBH IRB (IRB No. B-2402-882-003, approved on February 20, 2024). The authors conducted this study in accordance with the Declaration of Helsinki (1975, revised in 2013), and the reporting of this study conforms to STROBE guidelines. 5 Since the CDW provides encrypted virtual medical record numbers for the study, it was impossible to identify individual patients for chart review.
Data reconstruction and age-specific analysis
The data extracted from the CDW were analyzed using R 4.0.5 (R Statistics, Vienna, Austria). First, all serum lactate test results for all hospitalized patients during the study period were obtained, and the maximum lactate level for each patient was identified. These data were then merged with patient discharge status and date of death. Since this study focused on 30-day mortality, patients who died more than 30 days after the maximum lactate level measurement were considered not to have died within 30 days. A receiver operating characteristic (ROC) curve was drawn, and the area under the ROC curve (AUROC) was calculated for the model of estimating the 30-day mortality based on the maximum lactate level for the entire dataset. The ages of all patients were divided into 10-year intervals, and ROC curves and AUROCs were calculated for each age group. Additionally, sensitivity and specificity were calculated for thresholds ranging from 10 to 22 for predicting 30-day mortality based on the maximum lactate level.
Analysis by medical department and ICU
Using the admission and discharge data of all patients, data from the medical department during the hospitalization period, which included the date of the maximum lactate level measurement, were obtained. ROC curves and AUROCs were calculated for the departments with sufficiently high frequencies. ICU admission and discharge data were also used to identify the ICU in which a patient was hospitalized on the date of the maximum lactate level measurement. ROC curves and AUROCs were calculated for the most frequently appearing ICUs.
Calculation of precision based on the maximum lactate level threshold
Since the data in this study were imbalanced, with far fewer deceased patients compared to those who survived, precision‒recall (PR) curves and the area under the PR curve (AUPRC) were calculated. Graphs of precision, recall, and F1-score were plotted based on the threshold values of the maximum lactate level. The precision was calculated for maximum lactate level threshold values that increased from 0 to 23.
Results
Calculation of subject numbers and 30-day mortality counts
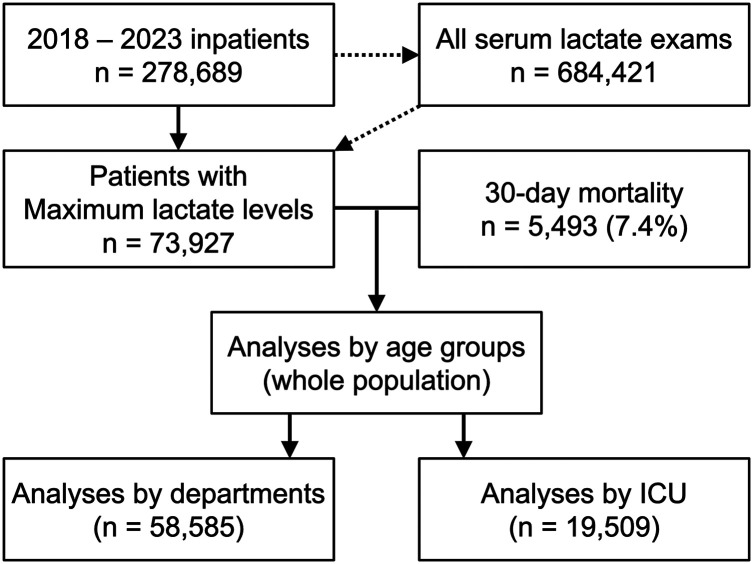
The overall flow of this study is summarized in Figure 1. From January 1, 2018, to December 31, 2023, a total of 278,689 patients were admitted to Seoul National University Bundang Hospital. Among these patients, 73,927 had at least one serum lactate measurement (mean age: 60.6 ± 20.5 years, men (n = 38,975, 52.7%) and women (n = 34,952, 47.3%)). From the 684,421 serum lactate tests performed on these 73,927 patients, the maximum lactate level and its measurement date for each patient were extracted. Among the 73,927 patients, 6686 (9.0%) were confirmed to have died during the study period. However, patients whose time interval from the maximum lactate level measurement to death was 31 days or more were not considered to have exhibited 30-day mortality. Overall, 5493 patients (7.4%) had cases classified as “death within 30 days of maximum lactate level measurement,” while 68,434 patients were counted as survivors.
Figure 1.
Flow diagram of the analyses. ICU: intensive care unit.
When the patients were divided into 10-year age intervals (0–10 years, 10–20 years, …, 80–90 years, ≥ 90 years), the highest number of patients was found in their 70 s (16,935; 22.9%), followed by those in their 60 s (16,758; 22.7%). The group aged 90 years or older had the lowest number of patients, at 1579 (2.1%) (Table 1). Patients in their 90 s also had the highest rate of 30-day mortality, at 19.1%, while the lowest 30-day mortality rate was observed among patients in their teens, at 0.8%.
Table 1.
Number of patients and deaths by age group and area under the ROC curve (AUROC).
| Age range (years) | No. of patients | 30-day Mortality | AUROC (95% CI) |
|---|---|---|---|
| 0–10 | 2735 (3.7%) | 28 (1.0%) | 0.957 (0.918–0.996) |
| 10–20 | 1800 (2.4%) | 14 (0.8%) | 0.902 (0.803–1.000) |
| 20–30 | 1917 (2.6%) | 34 (1.8%) | 0.940 (0.910–0.969) |
| 30–40 | 3817 (5.2%) | 88 (2.3%) | 0.917 (0.886–0.948) |
| 40–50 | 7041 (9.5%) | 256 (3.6%) | 0.895 (0.875–0.916) |
| 50–60 | 11,233 (15.2%) | 617 (5.5%) | 0.896 (0.883–0.909) |
| 60–70 | 16,758 (22.7%) | 1128 (6.7%) | 0.893 (0.883–0.903) |
| 70–80 | 16,935 (22.9%) | 1568 (9.3%) | 0.860 (0.850–0.870) |
| 80–90 | 10,112 (13.7%) | 1459 (14.4%) | 0.834 (0.822–0.846) |
| ≥90 | 1579 (2.1%) | 301 (19.1%) | 0.768 (0.736–0.800) |
| Total | 73,927 (100%) | 5493 (7.4%) | 0.870 (0.865–0.875) |
ROC: receiver operating characteristic; AUROC: area under the ROC curve; CI: confidence interval
Here, 30-day mortality refers to death within 30 days from the date of the maximum lactate level measurement.
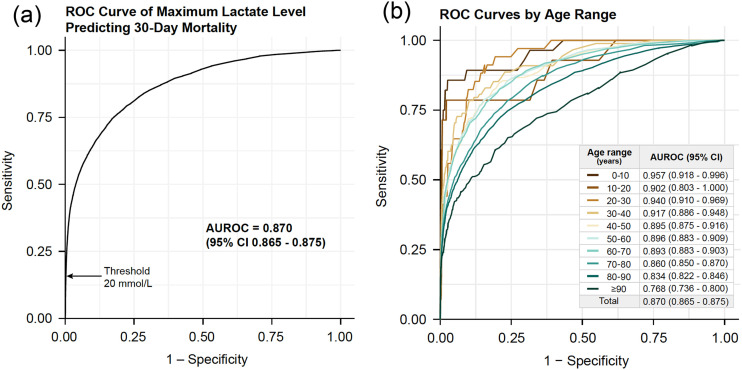
Overall and age-specific analysis
In all study patients, the ROC curve for predicting 30-day mortality based on the maximum lactate level had an AUROC of 0.870 (95% confidence interval [CI] 0.865–0.875), indicating very high accuracy (Figure 2(a)). Given that the focus of this study was to identify a maximum lactate level threshold with very high specificity for indicating that a patient is in the terminal phase, thresholds ranging from 10 to 22 mmol/L were applied incrementally (Table 2). Even at a threshold of 10 mmol/L, the specificity was 98.0%, and at 20 mmol/L, the specificity for predicting 30-day mortality reached 99.8%. This means that there were very few patients with a maximum lactate level above 20 mmol/L survived beyond 30 days.
Figure 2.
ROC curve and AUROC for predicting 30-day mortality based on the maximum lactate level. (a) For all patients, (b) Graphs drawn by age group. CI; confidence interval.
Table 2.
Sensitivity and specificity for predicting 30-day mortality based on the maximum lactate level by age group and threshold.
| Maximum lactate level thresholds (mmol/L) | |||||||
| 10 | 12 | 14 | 16 | 18 | 20 | 22 | |
| Age ranges (years) | Sensitivities | ||||||
| 0–10 | 36.9% | 28.7% | 15.4% | 12.8% | 6.3% | 4.6% | 1.1% |
| 10–20 | 51.0% | 51.0% | 25.0% | 12.8% | 2.0% | 0.5% | 0.5% |
| 20–30 | 19.5% | 19.5% | 17.0% | 17.0% | 10.5% | 8.7% | 7.0% |
| 30–40 | 29.8% | 23.9% | 19.6% | 13.2% | 10.1% | 6.3% | 4.2% |
| 40–50 | 20.9% | 15.0% | 11.8% | 9.5% | 7.1% | 3.4% | 2.3% |
| 50–60 | 21.0% | 15.0% | 10.7% | 7.6% | 4.9% | 2.8% | 1.7% |
| 60–70 | 21.7% | 15.8% | 10.5% | 7.9% | 4.8% | 2.7% | 1.6% |
| 70–80 | 15.4% | 11.4% | 7.8% | 5.2% | 3.2% | 1.9% | 1.0% |
| 80–90 | 15.7% | 10.8% | 6.8% | 4.2% | 2.5% | 1.3% | 0.7% |
| ≥90 | 8.4% | 6.2% | 4.5% | 2.7% | 1.4% | 0.5% | 0.2% |
| Total | 41.8% | 35.6% | 29.3% | 24.2% | 19.1% | 14.2% | 10.6% |
| Specificities | |||||||
| 0–10 | 98.9% | 99.3% | 99.5% | 99.8% | 99.9% | 99.9% | 99.9% |
| 10–20 | 97.9% | 98.7% | 98.8% | 98.9% | 99.1% | 99.4% | 99.6% |
| 20–30 | 96.1% | 97.2% | 97.9% | 98.4% | 98.8% | 99.3% | 99.5% |
| 30–40 | 95.9% | 97.5% | 98.4% | 99.0% | 99.3% | 99.4% | 99.6% |
| 40–50 | 95.7% | 97.0% | 97.8% | 98.4% | 99.0% | 99.4% | 99.5% |
| 50–60 | 95.8% | 97.2% | 98.1% | 98.7% | 99.1% | 99.4% | 99.6% |
| 60–70 | 96.1% | 97.5% | 98.5% | 99.1% | 99.4% | 99.7% | 99.8% |
| 70–80 | 96.0% | 97.8% | 98.6% | 99.1% | 99.5% | 99.8% | 99.9% |
| 80–90 | 95.5% | 97.5% | 98.6% | 99.3% | 99.5% | 99.8% | 99.8% |
| ≥90 | 96.9% | 97.7% | 99.1% | 99.7% | 99.8% | 99.8% | 99.8% |
| Total | 98.0% | 98.8% | 99.2% | 99.5% | 99.7% | 99.8% | 99.9% |
When patients were divided into 10-year age intervals and ROC curves with corresponding AUROCs were calculated for each age group (Figure 2(b)), the AUROC was greater than 0.9 for all ages from 0 to 40 years and greater than 0.8 for ages ranging from 40 to 90 years. The AUROC for patients aged 90 years and older was 0.768 (95% CI 0.736–0.800). Using a maximum lactate level threshold of 20 mmol/L, the specificity was greater than 99% for all age groups (Table 2). This indicates that the prediction of 30-day mortality based on the maximum lactate level performs relatively consistently across different age groups.
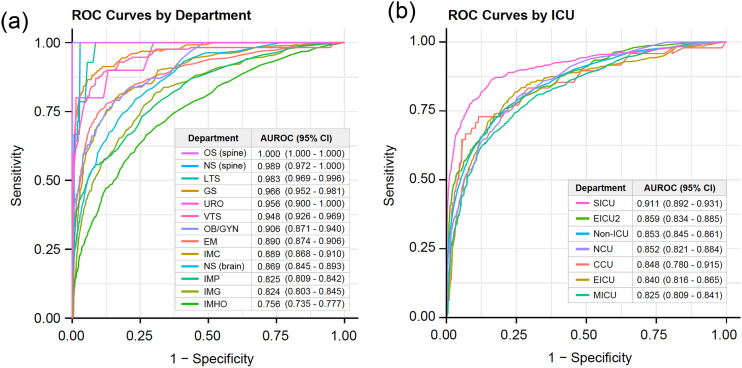
Analysis by medical department
Admission and discharge records were separately obtained, medical department information was collected when the maximum lactate level measurement date fell between the admission and discharge dates, and the medical record numbers were matched. This method allowed the identification of the medical department at the time of maximum lactate level measurement for 58,585 patients. The five departments with the highest frequencies were General Surgery, Thoracic Surgery (General Thoracic), Neurosurgery (Brain), Thoracic Surgery (Cardiovascular), and Obstetrics and Gynecology (Supplemental Material Table S1). ROC curves and AUROCs for predicting 30-day mortality based on maximum lactate levels were calculated for departments with more than 2000 patients (Figure 3(a)). The highest AUROC (1.000, 95% CI 1.000–1.000) was observed for Orthopedic Surgery (Spine), while the lowest AUROC (0.756, 95% CI 0.735–0.777) was observed for Hematology-Oncology. In general, surgical departments showed higher AUROCs compared to medical departments.
Figure 3.
ROC curve and AUROC for predicting 30-day mortality based on the maximum lactate level measured by the medical department and ICU. (a) ROC curves and AUROCs by medical department (only for departments with more than 2,000 patients); (b) ROC curves and AUROCs by ICU (including the top 6 ICUs by patient number and non-ICU patients). CI, confidence interval; OS, orthopedic surgery; NS, neurosurgery; LTS, thoracic surgery; GS, general surgery; URO, urology; VTS, cardiovascular surgery; OB/GYN, obstetrics and gynecology; EM, emergency medicine; IMC, cardiology; IMP, pulmonology; IMG, gastroenterology; IMHO, hemato-oncology; SICU, surgical ICU; EICU, emergency ICU; NCU, neurology ICU; CCU, coronary care unit; MICU, medical ICU.
Analysis by ICU
ICU admission and discharge data were used to determine whether a patient was in an ICU on the date of maximum lactate level measurement and, if so, which ICU. As a result, 19,509 of the 73,927 patients were in an ICU on the date of maximum lactate level measurement (Table 3). The ICU with the highest frequency was the surgical ICU (SICU). ROC curves and AUROCs for predicting 30-day mortality based on maximum lactate levels were calculated for the top six ICUs with more than 1000 patients and for non-ICU patients, forming seven groups in total (Figure 3(b)). The highest AUROC was 0.911 (95% CI 0.892–0.931), in the SICU, and the lowest AUROC was 0.825 (95% CI 0.809–0.841), in the medical ICU (MICU). Even for non-ICU patients, the AUROC was 0.853 (95% CI 0.845–0.861). The performance of the predictive model was slightly higher in the SICU compared to the MICU, but overall, it demonstrated very high performance regardless of the type of ICU or ward.
Table 3.
Intensive care unit (ICU) admission status on the date of the maximum lactate level measurement.
| ICU type | Number of patients |
|---|---|
| Surgical ICU | 6830 |
| Neurology CU | 4371 |
| Emergency ICU 2 | 3136 |
| Medical ICU | 2538 |
| Emergency ICU | 1229 |
| Coronary Care Unit | 937 |
| 121-ward ICU | 423 |
| Neonatal ICU | 30 |
| Neonatal ICU 2 | 15 |
| Total | 19,509 |
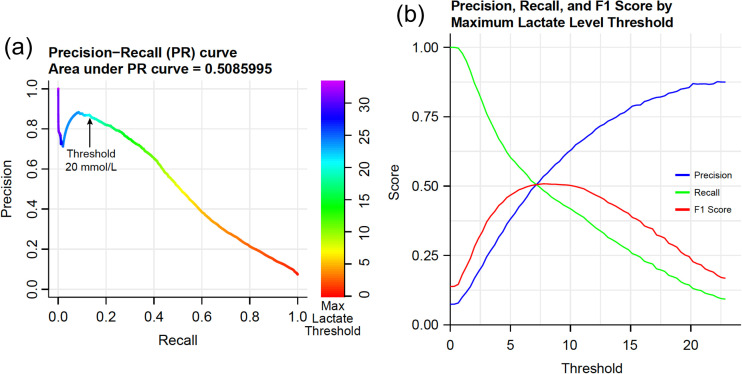
Precision
For all patients, the PR curve had an AUPRC of 0.509 (Figure 4(a)). When plotting the precision, recall, and F1-score graphs based on specific thresholds of the maximum lactate level, the maximum F1 score was slightly above 0.5 near the threshold of 7.5 mmol/L (Figure 4(b)). The precision (positive predictive value) increased with increasing maximum lactate level thresholds. At a threshold of 20 mmol/L, approximately 87% of patients who were predicted to expire within 30 days were found to have actually died.
Figure 4.
Additional performance metrics for all patients. (a) Precision-recall (PR) curve. (b) Precision, recall, and F1 score by maximum lactate threshold.
Discussion
The primary aim of this study was to evaluate the reproducibility and reliability of using maximum serum lactate levels as a predictor of 30-day mortality, ultimately suggesting a practical threshold for clinical use. The findings support the hypothesis that serum lactate levels, particularly those above a certain threshold, are highly indicative of a poor prognosis in critical care settings. Specifically, a lactate level of 20 mmol/L was shown to be associated with an 87% precision and 99.8% specificity for predicting 30-day mortality. This threshold can be valuable for clinicians in determining when to initiate discussions regarding the potential terminal nature of a patient's condition, providing an objective basis for making difficult decisions around end-of-life care.
The importance of serum lactate levels and their clearance in assessing patient status and prognosis in critical care has been well documented over the past decade.6–11 The serum level of lactate, a major metabolic product of anaerobic metabolism, is normally below 3 mmol/L. However, when tissue oxygen delivery fails to meet oxygen demand, as in heart failure or hypoxia, anaerobic metabolism increases serum lactate production. Historically, the emphasis has been on lactate clearance rather than absolute values. When lactate production outpaces clearance, the serum lactate level increases. 12 However, unless controlled for timing in clinical research, quantifying lactate clearance based on sporadically conducted serum lactate level tests presents challenges.
High serum lactate levels in critical care practice often indicate a poor prognosis, despite efforts to reverse the patient's condition. Many critical care physicians have observed that extremely high serum lactate levels often correlate with eventual death, suggesting that such levels may indicate irreversible systemic tissue damage.13,14 The authors hypothesized that a certain ‘absolute’ threshold of serum lactate could predict a high likelihood of death within 30 days and serve as a basis for determining whether a patient is in the terminal phase. This study aimed to evaluate the reproducibility and reliability of using single maximum lactate levels to predict 30-day mortality and to propose a practical threshold with high precision.
An interesting finding from this study is the variation in the AUROC among different departments. Surgical departments generally had greater AUROCs than did medical departments. Orthopedic (spine) surgery departments had an AUROC of 1.000, indicating complete separation of 30-day mortality and survival based on a specific maximum lactate level threshold. The lowest AUROC among departments with more than 2000 cases was found in Hematology-Oncology, with an AUROC in the 0.7 range. Differences were also observed among ICUs, with the SICU having the highest AUROC, at 0.911, and the MICU having the lowest, at 0.825. These results suggest that the maximum lactate level may predict 30-day mortality more accurately in surgical patients.
This suggests that the maximum lactate level may serve as a more reliable predictor of mortality in surgical settings, possibly due to the particular nature of perioperative metabolic disturbances. Patients in the Surgical Intensive Care Unit (SICU), especially those undergoing cardiothoracic procedures, often experience severe lactic acidosis due to pre-existing cardiovascular limitations, intraoperative factors such as prolonged cardiopulmonary bypass, or postoperative complications. These conditions are typically less reversible, and thus the corresponding lactate values may better reflect irreversible systemic tissue damage.
The significance of these findings lies in their potential application in the decision-making process for critical care. Identifying a practical lactate level threshold helps to establish a clearer and more consistent approach to managing patients whose prognosis is poor, potentially aiding in the allocation of limited medical resources and improving communication with family members regarding treatment expectations.
As shown in Figure 4, the AUPRC of the model for predicting 30-day mortality based on maximum lactate levels was 0.509, which is not very high. From a general diagnostic perspective, this is not ideal. However, the focus of this study was to identify a maximum lactate level threshold with clinically practical precision and specificity for predicting 30-day mortality. At a threshold of 20 mmol/L, the precision was 87%, and the specificity was 99.8%, indicating that patients with serum lactate levels exceeding this threshold have an extremely high likelihood of dying within 30 days. The high specificity indicates a very low false-positive rate, meaning that very few patients with maximum serum lactate levels above 20 mmol/L survived.
However, there are limitations to this study that must be acknowledged. First, this study relied on retrospective data from the Clinical Data Warehouse (CDW), which restricted our ability to conduct detailed chart reviews that would help clarify the clinical context of each hyperlactatemia case. While the majority of the patients in the study cohort were classified as having type A hyperlactatemia, it was challenging to differentiate between the various hyperlactatemia types (e.g. type A versus type B1, B2, or B3). This lack of differentiation means that the data may include confounding elements that could affect the prognostic accuracy of the lactate threshold. Thus, while the threshold demonstrated high specificity, its overall utility as a standalone prognostic tool should be approached cautiously.
Also, there may be criticisms that setting the threshold of maximum serum lactate levels at 20 mmol/L is arbitrary. However, according to the precision-recall curve, a positive correlation between the threshold and precision is maintained in the range of 0–25 mmol/L. Additionally, several commercially available testing equipment declare ‘uncheckable’ for lactate levels above 21 mmol/L. Considering this, 20 mmol/L was suggested as an appropriate threshold example. We have also provided tables and graphs that allow readers to examine the sensitivity, specificity, and precision for each threshold, enabling them to make their own judgments about the appropriate threshold (Table 2 and Figure 4). In this study, more than 70,000 patients were analyzed and we expect our results to serve as a reference.
Additionally, the variation in the AUROC among different departments and ICUs may be partially attributable to differences in patient populations and care protocols. For example, in the Hematology-Oncology department, where the AUROC was relatively low, patients often present with multiple metabolic and systemic challenges that may confound the relationship between lactate levels and mortality outcomes. Similarly, the discharge diagnoses recorded in the hospital information system often did not adequately reflect the patient's status at the time of peak lactate measurement, which may have further limited the analysis.
Another limitation was the inability to clearly determine 30-day mortality in a small number of cases where patients were discharged with a poor prognosis. This ambiguity, though infrequent, underscores the complexity of utilizing lactate levels as a definitive predictor of short-term mortality. Moreover, the lack of analysis on lactate clearance, which has been highlighted as significant in previous studies, and the fact that this study was conducted at a single institution, must also be taken into consideration. Furthermore, according to previous studies, differences in lactate levels based on whether the sampling site was capillary or serum, whether the patient was septic or not, and whether the patient was an emergency room visitor or an inpatient could influence the diagnostic value of lactate levels. 14 However, these factors were not addressed in this study, representing another limitation.
The authors do not claim that serum lactate levels alone can definitively indicate that a patient is in the terminal phase or will die shortly. Determining that a patient is in the terminal phase requires a comprehensive evaluation, including the severity of the patient's disease or injury and hemodynamic and neurological assessments. To promote dignified death and the appropriate implementation of life-sustaining treatment decisions, the use of objective indicators should minimize arbitrariness and reduce practice variation among physicians. Serum lactate level testing is simple and inexpensive, with results available within 3 to 30 min, making it practical for most hospitals.
Future research should focus on refining the patient population to include only those with clearly defined causes of death, which could improve the robustness of the predictive model. Moreover, conducting prospective studies that allow for more granular clinical data collection, including specific details of each patient's medical history, surgical outcomes, and cardiopulmonary function, would provide a stronger foundation for validating the findings of this study. Such efforts may ultimately lead to the development of a more nuanced understanding of the role of lactate in different clinical contexts, thereby improving the ability to use this biomarker effectively.
Conclusions
A threshold of 20 mmol/L was proposed as an indicator of high likelihood of mortality within 30 days, and it might be considered as part of a comprehensive assessment rather than a standalone criterion. The simplicity and rapid availability of lactate testing make it an attractive tool for most hospitals, but clinicians must continue to rely on a multifaceted evaluation, including hemodynamic and neurological assessments, when determining whether a patient is in the terminal phase. Addressing the limitations of the current study in future research will enhance the reliability and clinical utility of serum lactate measurements in critical care decision-making.
Supplemental Material
Supplemental material, sj-docx-1-sci-10.1177_00368504241311966 for Peak serum lactate as a robust predictor of imminent death in life-sustaining treatment decisions: A study of 73,927 patients by Dong Jung Kim, Hyun Joo Kim and Hyoung Woo Chang in Science Progress
Supplemental material, sj-docx-2-sci-10.1177_00368504241311966 for Peak serum lactate as a robust predictor of imminent death in life-sustaining treatment decisions: A study of 73,927 patients by Dong Jung Kim, Hyun Joo Kim and Hyoung Woo Chang in Science Progress
Acknowledgments
Not applicable.
Footnotes
Authors contributions: DJK participated in the conception and design of the study, and the establishment of the analysis plan. He also contributed to the interpretation and inference of the analysis results and participated in drafting the manuscript. HJK participated in the conception and design of the study, the establishment of the analysis plan, and was involved in data collection and analysis. She also participated in drafting the manuscript. HWC was responsible for the conception and design of the study, conducted data collection and analysis, interpreted the analysis results, and drafted, reviewed, and revised the manuscript to its final form. All authors read and approved the final manuscript.
Consent to participate: As a retrospective study, the requirement to obtain individual patient consent was waived by SNUBH IRB (IRB No. B-2402-882-003, approved on February 20, 2024).
Consent for publication: Not applicable.
Data availability: The datasets generated and/or analysed during the current study are not publicly available due to institutional policies but are available from the corresponding author on reasonable request.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical considerations: This study received approval from Seoul National University Bundang Hospital Institutional Review Board (SNUBH IRB) prior to initiation (title: Research on the Usefulness of Blood Lactate Concentration as a Predictor of Mortality Discharge: A CDW Based Study). As a retrospective study, the requirement to obtain individual patient consent was waived by SNUBH IRB (IRB No. B-2402-882-003, approved on February 20, 2024). The authors conducted this study in accordance with the Declaration of Helsinki (1975, revised in 2013). Since the CDW provides encrypted virtual medical record numbers for the study, it was impossible to identify individual patients for chart review.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Dong Jung Kim https://orcid.org/0000-0003-0332-3430
Hyoung Woo Chang https://orcid.org/0000-0001-5516-0333
Supplemental material: Supplemental material for this article is available online.
References
- 1.Bomba PA, Kemp M, Black JS. POLST: an improvement over traditional advance directives. Cleve Clin J Med 2012; 79: 457–464. [DOI] [PubMed] [Google Scholar]
- 2.Hickman SE, Keevern E, Hammes BJ. Use of the physician orders for life-sustaining treatment program in the clinical setting: a systematic review of the literature. J Am Geriatr Soc 2015; 63: 341–350. [DOI] [PubMed] [Google Scholar]
- 3.Kennedy C, et al. Diagnosing dying: an integrative literature review. BMJ Support Palliat Care 2014; 4: 263–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taylor P, Dowding D, Johnson M. Clinical decision making in the recognition of dying: a qualitative interview study. BMC Palliat Care 2017; 16: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.von Elm E, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 2007; 147: 573–577. [DOI] [PubMed] [Google Scholar]
- 6.Mikkelsen ME, et al. Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med 2009; 37: 1670–1677. [DOI] [PubMed] [Google Scholar]
- 7.Jansen TC, et al. Prognostic value of blood lactate levels: does the clinical diagnosis at admission matter? J Trauma 2009; 66: 377–385. [DOI] [PubMed] [Google Scholar]
- 8.Attanà P, et al. Lactate and lactate clearance in acute cardiac care patients. Eur Heart J Acute Cardiovasc Care 2012; 1: 115–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lucas D, H E, et al. Lactate and lactate clearance in critically burned patients: usefulness and limitations as a resuscitation guide and as a prognostic factor. Burns 2020; 46: 1839–1847. [DOI] [PubMed] [Google Scholar]
- 10.Chavez J, Glaser S, Krom Z. Continuous lactate measurement devices and implications for critical care: a literature review. Crit Care Nurs Q 2020; 43: 269–273. [DOI] [PubMed] [Google Scholar]
- 11.Tamakawa T, Endoh H, Kamimura N, et al. Impact on outcomes of measuring lactates prior to ICU in unselected heterogeneous critically ill patients: a propensity score analysis. PLoS One 2022; 17: e0277948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones AE, et al. Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA 2010; 303: 739–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang Z, Xu X, Chen K. Lactate clearance as a useful biomarker for the prediction of all-cause mortality in critically ill patients: a systematic review study protocol. BMJ Open 2014; 4: e004752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guarino M, et al. Comparison between Capillary and Serum Lactate Levels in Predicting Short-Term Mortality of Septic Patients at the Emergency Department. Int J Mol Sci 2023; 24: 9121. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sci-10.1177_00368504241311966 for Peak serum lactate as a robust predictor of imminent death in life-sustaining treatment decisions: A study of 73,927 patients by Dong Jung Kim, Hyun Joo Kim and Hyoung Woo Chang in Science Progress
Supplemental material, sj-docx-2-sci-10.1177_00368504241311966 for Peak serum lactate as a robust predictor of imminent death in life-sustaining treatment decisions: A study of 73,927 patients by Dong Jung Kim, Hyun Joo Kim and Hyoung Woo Chang in Science Progress