Abstract
Background
The intricate anatomical variations in lung structure often perplex thoracic surgeons, and the accurate identification of these variations is closely associated with favorable surgical outcomes.
Case presentation
A 53-year-old female patient who underwent computed tomography (CT) examination due to chest discomfort, revealing the presence of a partial solid nodule highly suspected of early-stage lung cancer, measuring approximately 2.8 × 2.6 cm in the left lower lobe. Consequently, the patient underwent a single direction thoracoscopic left lower lobectomy and lymph node dissection. Intraoperatively, while attempting to dissect and free the left lower lobe vein from surrounding tissues, technical difficulties were encountered. Upon meticulous review of preoperative CT scans during surgery, an anomalous connection between the lingular vein of the left upper lobe and the left lower lobe vein was identified. Once this anatomical variation was confirmed, surgical intervention proceeded uneventfully without any significant complications.
Conclusion
Precise recognition of pulmonary anatomical structures before and during surgery is paramount in recognizing rare variations such as this one as it aids in preventing potential intraoperative injuries and minimizing postoperative complications.
Keywords: Lingular vein variation, Video-assisted thoracoscopic surgery, Lung cancer
Introduction
Video-assisted thoracoscopic surgery (VATS) lobectomy has become increasingly prevalent and is now considered the standard procedure for early-stage lung cancer due to its advantages over open-chest surgery, including reduced pain, lower complication rates, shorter hospital stays, and equivalent long-term survival rates [1, 2]. The presence of anatomical alterations in the pulmonary arteries and veins is associated with a potential risk of hemorrhage during lung resection. Preoperative identification of these vascular changes is of paramount importance for the safety and efficacy during lung surgery [3]. Anatomical variations in the pulmonary veins may lead to intraoperative misidentification of the veins, resulting in severe postoperative complications including vascular rupture, pulmonary congestion, and hemoptysis [4, 5]. In this report, we detail a case of a successful VATS-assisted left lower lobectomy where an anomalous lingular segment vein of the left superior lobe drains into the left inferior lobe vein.
Case presentation
A 53-year-old female patient who underwent computed tomography (CT) examination due to chest discomfort, revealing the presence of a partial solid nodule highly suspected of early-stage lung cancer, measuring approximately 2.8 × 2.6 cm in the left lower lobe (Fig. 1A). According to the NCCN Clinical Practice Guidelines in Oncology for Non-Small Cell Lung Cancer (NSCLC), which provide recommended management for patients with NSCLC [6], we have decided to perform a lower lobe resection of the left lung. The patient underwent a thoracoscopic pulmonary lobectomy under general anesthesia. The procedure involved inserting a single port thoracoscope through the fifth intercostal space. The examination revealed incomplete development of the lung fissure. Therefore, the patient underwent a thoracoscopic left lower lobectomy and lymph node dissection in a single-direction approach. It was decided to sequentially transect the left lower lobe vein, bronchus, and artery [1]. During the intraoperative phase, challenges arose while dissecting and freeing the left lower lobe vein from surrounding tissues, technical difficulties were encountered (Fig. 2A), and an unknown vessel was found to drain into the left lower lobe vein. Upon carefully identification of the anatomy and meticulous review of preoperative CT scans during surgery, an anomalous connection between the lingular vein of the left upper lobe and the left lower lobe vein was identified (Fig. 1B).
Fig. 1.
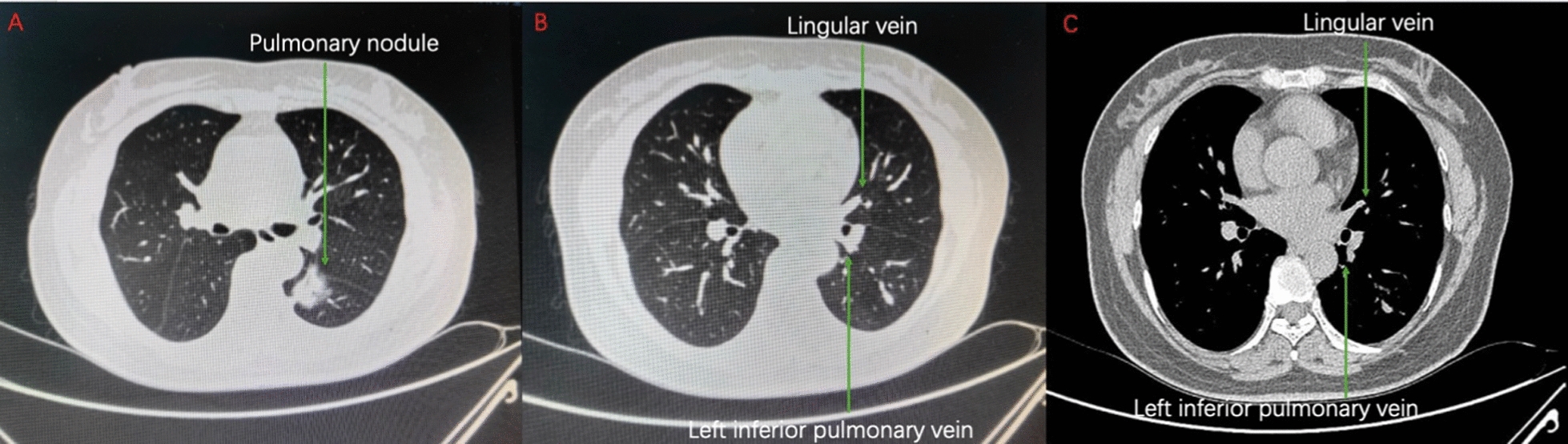
A The chest CT scan revealed a partial solid nodule measuring 2.8 × 2.6 cm in the left lower lobe. B The lingular vein was observed on CT to exhibit drainage into the left inferior pulmonary vein (pulmonary window). C The lingular vein was observed on enhanced CT to exhibit drainage into the left inferior pulmonary vein (mediastinal window)
Fig. 2.
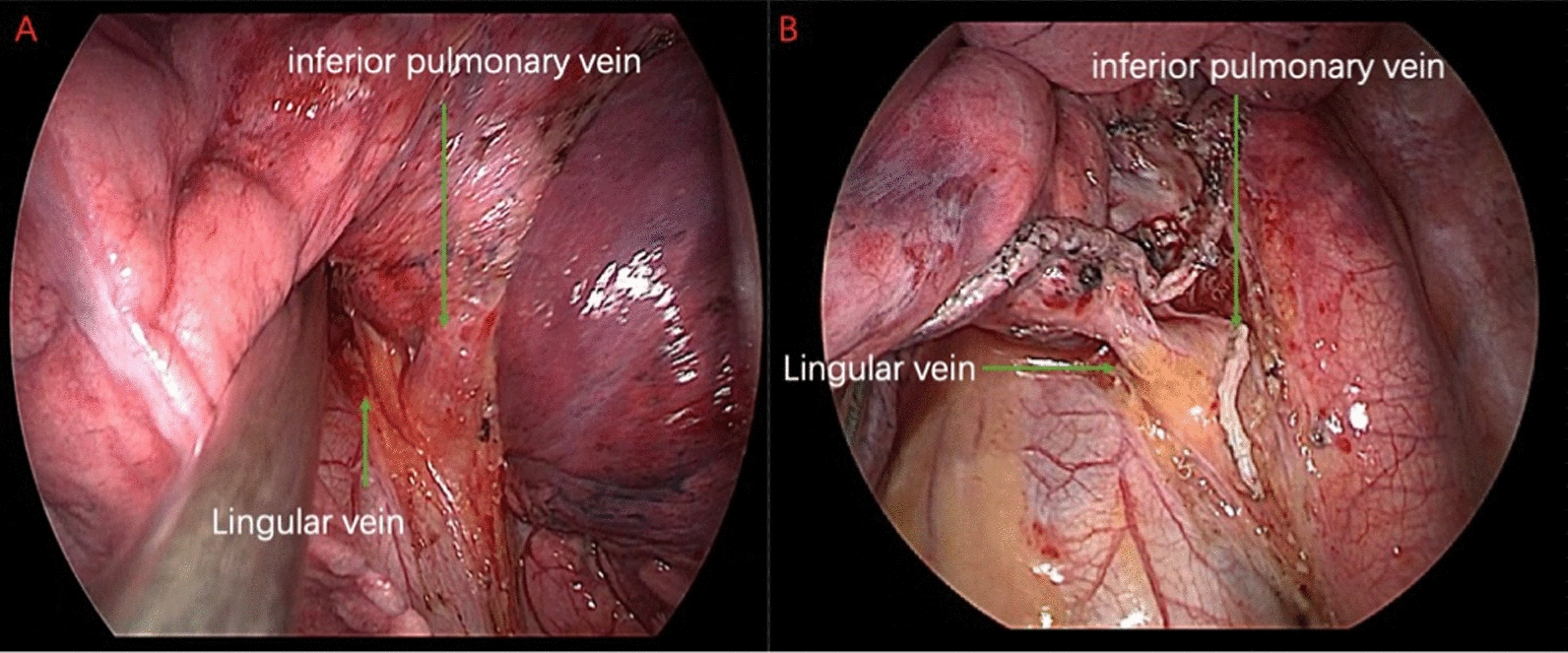
A The thoracoscopic view revealed that the lingular vein originating from the left superior lobe of the lung drained into the adjacent left inferior lobe, as evidenced by anatomical observations. B The lingular vein of the left superior lobe and the residual portion of the left inferior lobe were visually discernible
Once this anatomical variation was confirmed (Fig. 1C), surgical intervention proceeded uneventfully (Fig. 2B). The patient made an uneventful recovery and was discharged on postoperative day 3. The postoperative pathological staging revealed stage IB lung adenocarcinoma, classified as pT2aN0M0 according to the TNM classification system.
Discussion
The occurrence of variations in the venous drainage pattern, specifically the drainage of the left upper lobe vein into the left lower lobe vein, is relatively uncommon [4]. It is known that the left superior division veins and the lingular division veins are typically drained into the left upper lobe vein. In Li Z’s [7] study, three-dimensional computed tomography bronchography and angiography (3D-CTBA) was used to reconstruct lung images of 540 NSCLC patients. The research results show that patients with lingular vein variation draining into the left lower lobe vein accounted for 2.4% (including any lingular vein reflux into the left lower lobe vein), while those draining into the left upper lobe vein accounted for 96.3% [7]. The rarity of this lingular vein anatomical variation leads surgeons to overlook the potential existence of such minor venous anomalies when reviewing the patient's preoperative CT scans. Therefore prior to the procedure, it is crucial to repeatedly review chest-enhanced CT scans to ensure a smooth and successful operation,particularly when the thoracoscopic guidance reveals evident branches of the targeted vein. During surgery, timely identification of venous alterations is crucial to avert potential complications. Compared to open surgery, thoracoscopic thoracic surgery offers superior visualization of the local operative field compared to open surgery [8],but may not provide the comprehensive anatomical details required by surgeons [5]. Moreover, in this patient's case, there was an incomplete development of the pulmonary fissure, which significantly increased the surgical complexity. The presence of incomplete pulmonary fissure development further compounds the challenge of identifying variant bronchi and the trachea [8]. Consequently, the recognition of lingular vein variations is of clinical importance during video-assisted thoracoscopic surgical lobectomy [9]. During lobectomy procedures, surgeons necessitate repetitive evaluation of bronchial and vascular anatomy to prevent inadvertent damage caused by erroneous incisions. Therefore, even experienced surgeons should refrain from relying solely on personal experience when performing surgery. Additionally, continuous confirmation of anatomical structures during the surgery is essential to achieve the best possible surgical outcomes.
Currently, CT technology has reached a high level of advancement, enabling rapid and precise visualization of the pulmonary vein structure. The employment of three-dimensional 64-row multidetector computed tomography (3D-MDCT) and 3D-CTBA facilitates clear visualization of the bronchial, pulmonary arterial, and venous anatomical structures, thus facilitating the identification of congenital variations [7, 10]. These advanced technologies assist surgeons in precise lesion localization prior to surgery, enhancing the likelihood of accurate surgical resection while minimizing operative errors and tissue damage.
Conclusion
Accurate identification of lingular vein before and during surgery is paramount in recognizing rare variations such as this one as it aids in preventing potential intraoperative injuries and minimizing postoperative complications.
Abbreviations
- CT
Computed tomography
- VATS
Video-assisted thoracoscopic surgery
- NSCLC
Non-small cell lung cancer
- 3D-CTBA
Three-dimensional computed tomography bronchography and angiography
- 3D-MDCT
Three-dimensional 64-row multidetector computed tomography
Author contributions
C.G. wrote the main manuscript text. W.D. and Q.L. obtained the funding. All authors have reviewed and approved the final manuscript.
Funding
This work was supported by Sichuan Science and Technology Program [2023YFH0075] and Sichuan Province Key Clinical Specialty Construction Project (no grant number).
Data Availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Our study was approved by the Ethics Committee for Medical Research and New Medical Technology of Sichuan Cancer Hospital (No. SCCHEC-02-2024-137). Written patient consent for participation was obtained.
Consent for publication
Written informed consent has been obtained from the patient and their family members for publication of relevant clinical information by the authors in pertinent medical publications.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Chenyang Guo, Yadi Zhang, and Haoqian Zheng contributed equally to this work.
References
- 1.Liao H, Mei J, Lin F, Liu C, Pu Q, Liu L. Single-direction thoracoscopic lobectomy: left side. J Thorac Dis. 2018;10:5932–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wei X, Yu H, Dai W, Mu Y, Wang Y, Liao J, et al. Patient-reported outcomes of video-assisted thoracoscopic surgery versus thoracotomy for locally advanced lung cancer: a longitudinal cohort study. Ann Surg Oncol. 2021;28:8358–71. [DOI] [PubMed] [Google Scholar]
- 3.Ishikawa Y, Iwano S, Usami N, Yokoi K. An anomalous segmental vein of the left upper lobe of the lung: preoperative identification by three-dimensional computed tomography pulmonary angiography. Interact Cardiovasc Thorac Surg. 2012;15:512–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akiba T, Marushima H, Morikawa T. Confirmation of a variant lingular vein anatomy during thoracoscopic surgery. Ann Thorac Cardiovasc Surg. 2010;16:351–3. [PubMed] [Google Scholar]
- 5.Yamada S, Suga A, Inoue Y, Iwazaki M. Importance of preoperative assessment of pulmonary venous anomaly for safe video-assisted lobectomy. Interact Cardiovasc Thorac Surg. 2010;10:851–4. [DOI] [PubMed] [Google Scholar]
- 6.Ettinger DS, Wood DE, Aisner DL, Akerley W, Bauman JR, Bharat A, et al. Non-small cell lung cancer, version 3.2022, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2022;20:497–530. [DOI] [PubMed] [Google Scholar]
- 7.Li Z, Wu W, Kong Y, Chen S, Zhang X. Analysis of variations in the bronchovascular pattern of the lingular segment to explore the correlations between the lingular segment artery and left superior division veins. Front Surg. 2023;10:1173602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Subotich D, Mandarich D, Milisavljevich M, Filipovich B, Nikolich V. Variations of pulmonary vessels: some practical implications for lung resections. Clin Anat. 2009;22:698–705. [DOI] [PubMed] [Google Scholar]
- 9.Asouhidou I, Karaiskos T, Natsis K. Pulmonary vein anatomical variation during videothoracoscopy-assisted surgical lobectomy. Surg Radiol Anat. 2017;39:229–31. [DOI] [PubMed] [Google Scholar]
- 10.Akiba T, Marushima H, Kamiya N, Odaka M, Kinoshita S, Takeyama H, et al. Thoracoscopic lobectomy for treating cancer in a patient with an unusual vein anomaly. Ann Thorac Cardiovasc Surg. 2011;17:501–3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.


