Abstract
BACKGROUND
The authors report the first case of thoracic interdural spinal cysts presenting as radiculopathy attributed to overdrainage-related cervical venous plexus enlargement. This case emphasizes the importance of considering interdural spinal cysts and cerebrospinal fluid overdrainage in the differential diagnosis of radiculopathy.
OBSERVATIONS
A 37-year-old male patient with a history of orthostatic headache presented with bilateral deltoid muscle atrophy consistent with C5 radiculopathy. Postcontrast magnetic resonance imaging (MRI) revealed cervical epidural venous plexus enlargement and nerve root compression. Thoracic MRI showed an interdural cyst extending from C7 to T11. In addition, a small defect in the inner layer of the dura, which connects the subarachnoid space to the cyst at the T10 level, was detected on thin-slice MRI. Surgery was performed to close the dural defect, with endoscopic assistance facilitating definitive treatment. Postoperative MRI confirmed the resolution of the spinal cyst and epidural venous enlargement. Furthermore, the patient’s symptoms improved.
LESSONS
Evaluating the cervical spinal pathology is the common approach for cervical radiculopathy. However, in the authors’ case, the presence of thoracic lesions could have been an underlying cause. Hence, identifying this unique clinical presentation can raise awareness among neurosurgeons and lead to better patient outcomes by addressing the underlying pathology in a timely manner.
Keywords: interdural cyst, epidural venous enlargement, radiculopathy, endoscope, case report
ABBREVIATIONS: CSF = cerebrospinal fluid, MRI = magnetic resonance imaging.
Spinal meningeal cysts are typically classified into the epidural and intradural types.1, 2 However, several reports have revealed another rare type of cyst located in the interdural space.3–9 Thin-slice magnetic resonance imaging (MRI) can identify fistulous communications between the subarachnoid space and the interdural cyst.1 Cerebrospinal fluid (CSF) leaks through dural tears into the interdural cyst. CSF drainage can cause symptoms consistent with intracranial hypotension.3, 4, 10 Furthermore, Sato et al. revealed that hemorrhage from bridging veins between the dural layers causes superficial hemosiderosis.3
Herein, we report a unique case of a thoracic interdural cyst causing cervical epidural venous enlargement and radiculopathy. A dural tear was detected at the T10 level, and direct surgery was performed to close the tear. Postoperatively, the epidural venous enlargement immediately resolved, and cervical radiculopathy significantly improved. This case report underscores the importance of considering thoracic interdural cysts in the differential diagnosis of cervical radiculopathy. It is important to be aware of this rare pathology to provide a definite diagnosis and well-planned surgical management for patients.
Illustrative Case
History and Examination
A 37-year-old male patient who presented with bilateral upper-limb weakness was referred to our institution. The patient exhibited deltoid muscle atrophy and weakness (Fig. 1). T1-weighted MRI showed enlargement of the epidural venous plexus in the cervical region and compression of the bilateral C5 nerve roots (Fig. 2). Contrast-enhanced computed tomography scanning did not reveal any spinal vascular malformations. Importantly, thoracic MRI detected fluid accumulation ventral to the spinal cord (Fig. 3). T2-weighted 3T MRI showed a suspicious fistula on the inner layer of the dura at the T10 level. The CSF drainage through this dural fistula might represent the underlying pathology. Thus, to close this drainage route, direct surgery was planned.
FIG. 1.
Clinical presentation of the patient showing atrophy (arrows) of bilateral deltoid muscles. Images from the left (A), front (B), right (C), and back (D).
FIG. 2.
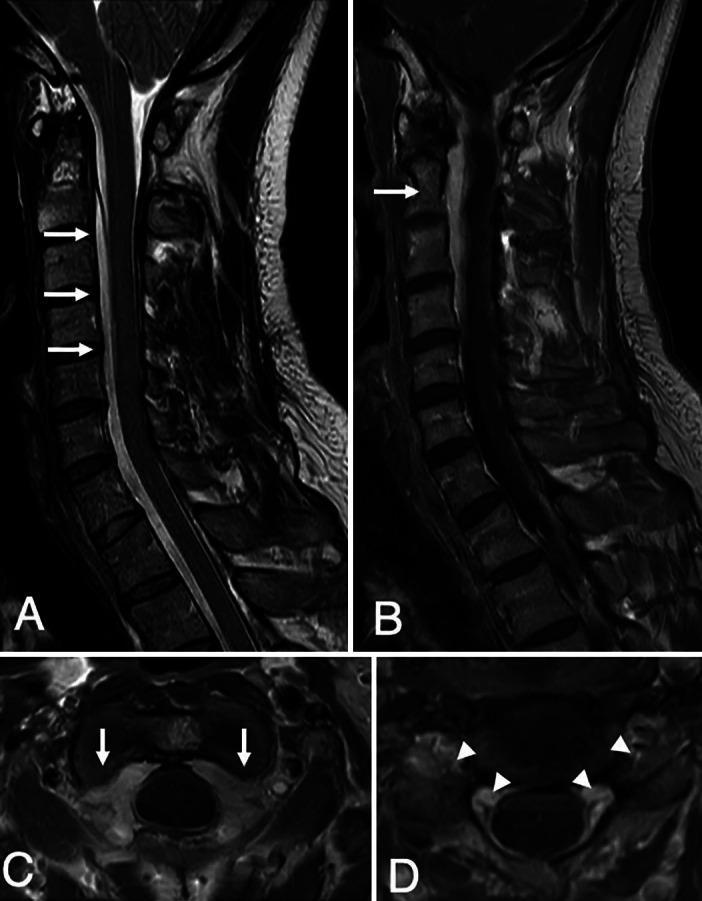
Preoperative cervical MRI. Sagittal T2-weighted MRI demonstrating an interdural cyst, starting from C2 and extending to the thoracic level (arrows, A). Note that no lesions were compressing the spinal cord. Sagittal postcontrast T1-weighted MRI demonstrating enhancement of the epidural venous plexus in the cervical region (arrow, B). Postcontrast axial T1-weighted MRI demonstrating enhancement of the epidural venous plexus at the C2 (arrows, C) and C4–5 (D) levels. Note the compression of the C5 nerve roots (arrowheads, D).
FIG. 3.
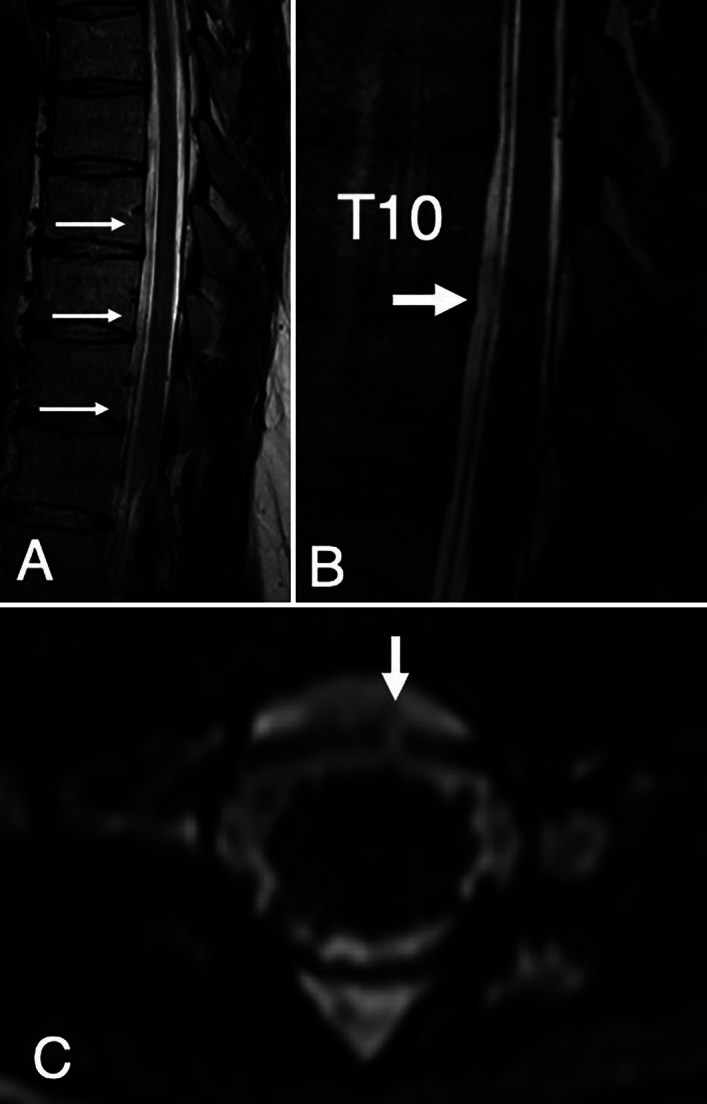
Preoperative thoracic MRI. Conventional sagittal T2-weighted MRI demonstrating extension of the interdural cyst to the L1 level (arrows, A). Sagittal (B) and axial (C) heavily T2-weighted MRI indicating a dural defect in the left ventral dura at the T10–11 level (arrows).
Operation
The patient was placed prone. A T10 and T11 laminectomy was performed, and the dura was opened. Using an angled endoscope, the dural fistula was found ventral to the spinal cord, as shown on preoperative MRI. Furthermore, endoscopy provided a view via the defect, which confirmed the diagnosis of an interdural cyst. The fistula was successfully closed (Fig. 4).
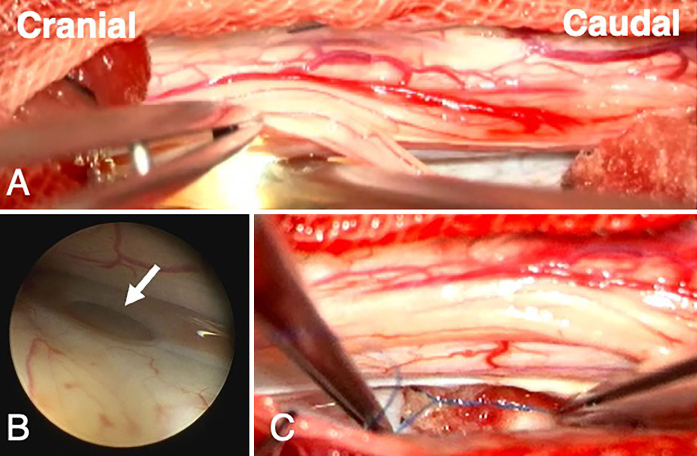
FIG. 4.
Intraoperative findings after T10 and T11 laminectomy. A: Microscopic view showing the application of an angled endoscope next to the spinal cord at the T10 level to provide the view ventral to the spinal cord. B: Endoscopic view demonstrating a dural defect (arrow), as indicated by preoperative MRI. The outer dural membrane was confirmed through the defect, which confirmed the diagnosis of the interdural cyst. C: Microscopic view demonstrating that the dural defect is sutured and closed.
Postoperative Course
One week after the surgery, postoperative MRI confirmed that the epidural enlargement had disappeared and that the size of the fluid-filled interdural cavity had decreased. Physical examination confirmed that deltoid muscle weakness had significantly improved. During the follow-up period, the patient showed a gradual improvement in his symptoms. Recurrence of the interdural spinal cyst or epidural venous enlargement was not observed on MRI performed 22 months after the surgery (Fig. 5).
FIG. 5.
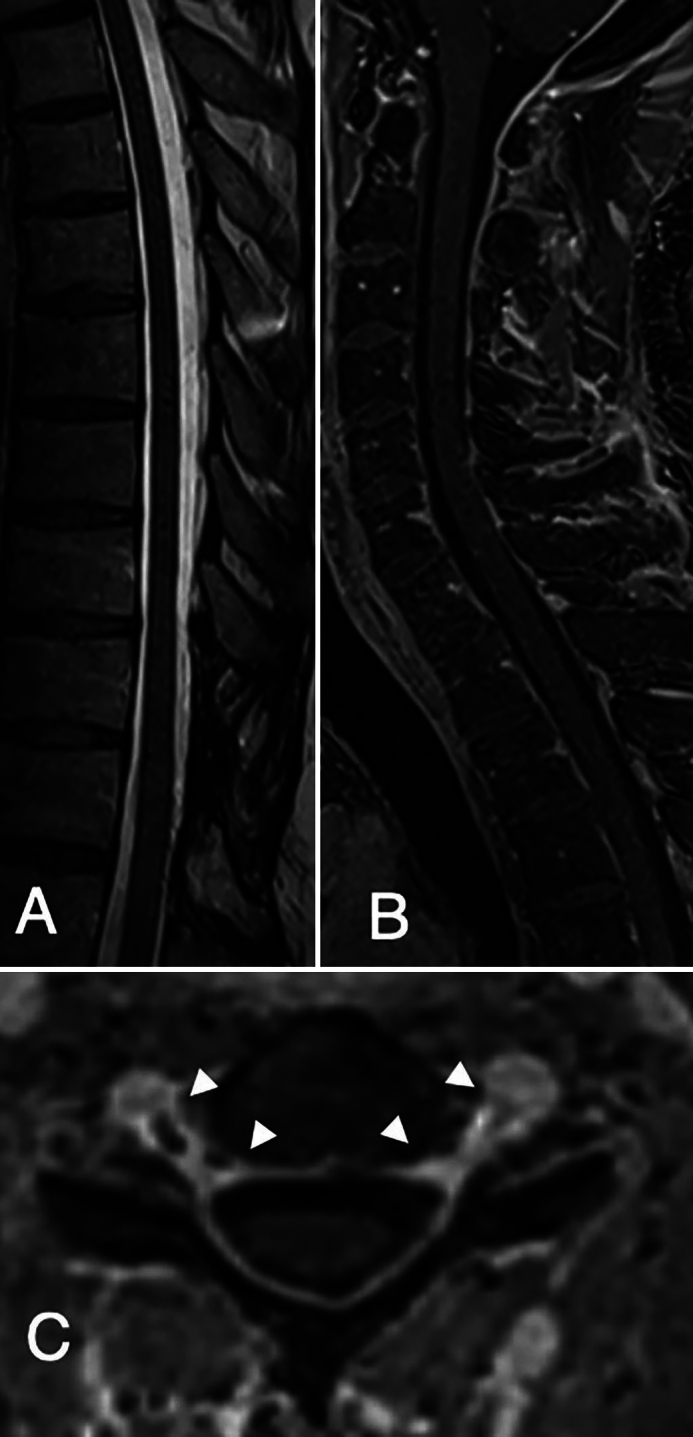
MRI 22 months after the operation. Sagittal T2-weighted MRI (A) showing no fluid accumulation ventral to the thoracic spinal cord. Postcontrast T1-weighted sagittal (B) and axial (C) MRI demonstrating the disappearance of venous enlargement in the cervical spine. Compression of the cervical nerve roots was completely resolved (arrowheads).
Informed Consent
The necessary informed consent was obtained in this study.
Discussion
Observations
Herein, we report the case of an interdural spinal cyst in a patient who exhibited atrophy of the bilateral deltoid muscles. Imaging confirmed a dural fistula at the T10 level, which was the primary pathology. Our case exemplified CSF overdrainage via a fistula into an interdural cyst, which caused radiculopathy attributed to epidural venous plexus enlargement.
Classification of the Spinal Cyst
The interdural spinal cyst can be classified as a novel type of spinal meningeal cyst. The conventional classifications were as follows: type I, extradural cyst without spinal nerve root fibers; type II, extradural cyst with spinal nerve root fibers; and type III, intradural cyst.2 According to the classification described by Kawasaki et al., the cyst in the current case was consistent with interdural meningeal cysts communicating with the arachnoid space via a fistula (type IIA).1 In addition to this case report, other studies have reported interdural cysts accompanied by a hole in the dura mater, which allows communication with the arachnoid space and cyst.1, 3, 4, 7, 9
Pathogenesis and Etiology
Dural defects typically arise spontaneously. The defects can be associated with trauma, degenerative disc disease, osteophytes, or connective tissue disorders.11–14 However, in most cases, the cause of the dural tear remains unknown.
If CSF drains into an interdural cyst, the thin-walled venous system initiates the first compensatory response, resulting in engorgement of the spinal epidural venous plexuses.15 This mechanism resembles the pathophysiology of Miyazaki syndrome, which is associated with overdrainage caused by the valveless ventriculoperitoneal shunt.15 In Miyazaki syndrome, the cervical epidural venous enlargement can potentially compress the spinal cord and/or nerve roots, causing myelopathy and/or radiculopathy, respectively.15–17
Patients with interdural cysts of the spinal cord, characterized by dural defects, can develop CSF leakage and can typically present with acute and chronic symptoms. This condition can initially result in a persistently decreased intracranial pressure, leading to symptoms of low cranial pressure such as postural headache.10 Importantly, our patient also recalled remote episodes of postural headache that had occurred several years earlier. Thereafter, a mild degree of dural collapse in response to the depletion of CSF volume can occur, compensated for by engorgement of the epidural venous plexus.16 Ultimately, based on the spinal region involved, engorgement of the epidural venous plexus will lead to further complications such as compressive myelopathy.
Although this pathophysiology has been widely accepted, not all patients will exhibit this clinical course. In cases involving a dural tear and interdural cysts, the predisposing factors causing epidural venous enlargement remain to be elucidated.
Diagnosis
In this case, the cause of radiculopathy was challenging to identify. Epidural venous dilation is a rare etiology of radiculopathy, and vascular lesions within the epidural space are frequently overlooked or misdiagnosed.18 Intervertebral disc herniation is the most common cause of radiculopathy, followed by hematoma, tumor, and abscess.18 Based on this case report, although rare, epidural venous dilation can be a different etiology that should be considered in the differential diagnosis.
The initial clinical symptoms can appear in the cervical region. However, imaging of the whole spinal region is essential. Furthermore, it is important to detect any fistulas causing CSF leakage in the lower regions.
After detecting the interdural cyst and fluid accumulation consistent with CSF overdrainage on spinal MRI, the next challenge was locating the dural tear.12 T2-weighted MRI, which provides high-resolution soft tissue images, is excellent for visualizing various cranial and spinal cord lesions and is useful for detecting spinal lesions that might be missed on routine spin-echo sequences.19 This method facilitated the detection of CSF dural defects. Hence, it played an essential role in detecting dural defects in the current case.
Management
To close the fistula,20–22 single-stage repair is the preferred treatment option, as it is associated with optimal long-term clinical outcomes.23, 24 However, the failure rate of direct suture is high at 5%–9%.25 Endoscopy has evolved as a useful adjunct in spinal surgery.26, 27 Based on previous studies, endoscopic techniques are helpful in identifying dural defects, with three patients showing a dural hole ventral to the spinal cord.3, 4 Overall, endoscopy is minimally invasive, and it prevents complications. Thus, it is associated with a lower level of postoperative pain and a shorter hospital stay.28
In the current case, MRI successfully confirmed the resolution of the fluid-filled cavity after endoscope-assisted micro-neurosurgery. Postoperative decrease in the size of the epidural venous plexus and improved neurological symptoms associated with cervical radiculopathy indicated the disappearance of the interdural cyst. The patient had positive outcomes after comprehensive preoperative examination and well-planned surgery.
Lessons
This case report highlights the importance of recognizing interdural spinal cysts, which are a rare cause of cervical epidural venous enlargement and radiculopathy. Advanced imaging, particularly T2-weighted MRI, is essential for obtaining an accurate diagnosis and facilitating surgical planning. The successful resolution of symptoms after endoscope-assisted surgery emphasizes the efficacy of surgical intervention. Increased knowledge about this condition can lead to an appropriate diagnosis and management, thereby resulting in improved patient outcomes.
Acknowledgments
We thank Enago for the English-language review.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Endo, Irwan, Takahashi, Faried. Acquisition of data: Endo, Irwan, Takahashi, Saito, Ito, Nishizawa. Analysis and interpretation of data: Endo, Irwan, Takahashi. Drafting the article: Endo, Irwan, Takahashi, Sasaki, Faried. Critically revising the article: Endo, Irwan, Takahashi, Faried. Reviewed submitted version of manuscript: Endo, Irwan, Takahashi, Ito, Faried. Approved the final version of the manuscript on behalf of all authors: Endo. Administrative/technical/material support: Endo. Study supervision: Endo, Irwan, Nishizawa, Faried.
Correspondence
Toshiki Endo: Tohoku Medical and Pharmaceutical University, Sendai, Japan. toshendo@tohoku-mpu.ac.jp.
References
- 1.Kawasaki T, Takayama M, Maki Y, Nakajima K, Ioroi Y, Kobayashi T. An interdural spinal cyst in the cervicothoracic spine: a review and proposal for a revised classification of spinal meningeal cysts. Illustrative case. J Neurosurg Case Lessons. 2022;4(19):CASE22198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nabors MW, Pait TG, Byrd EB, et al. Updated assessment and current classification of spinal meningeal cysts. J Neurosurg. 1988;68(3):366-377. [DOI] [PubMed] [Google Scholar]
- 3.Sato Y, Endo T, Inoue T, Fujimura M, Tominaga T. Successful endoscopic identification of the bleeding source in the ventral dura of the cervical spine in a case of superficial siderosis. J Neurosurg Spine. 2020;33(1):73-76. [DOI] [PubMed] [Google Scholar]
- 4.Arishima H, Higashino Y, Yamada S, et al. Spinal endoscopy combined with selective CT myelography for dural closure of the spinal dural defect with superficial siderosis: technical note. J Neurosurg Spine. 2018;28(1):96-102. [DOI] [PubMed] [Google Scholar]
- 5.Aoun SG, Plitt AR, El Ahmadieh TY, Al Tamimi M, Whitworth T. Traumatic lumbar interdural cyst with intradural expansion and compression of the cauda equina: case report and surgical video. Cureus. 2019;11(6):e4824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen HJ, Chen L. Traumatic interdural arachnoid cyst in the upper cervical spine: case report. J Neurosurg. 1996;85(2):351-353. [DOI] [PubMed] [Google Scholar]
- 7.Done SL, Hayman LA, New PFJ, Davis KR, Chapman PH. Interdural cyst of the lumbosacral region. Neurosurgery. 1984;14(3):287-294. [DOI] [PubMed] [Google Scholar]
- 8.Lee JH, Jung TG, Kim HS, Jang JS, Lee SH. Symptomatic isolated lumbar interdural arachnoid cyst. Neurol Med Chir (Tokyo). 2010;50(11):1035-1038. [DOI] [PubMed] [Google Scholar]
- 9.Sajjad J, Yousaf I, Bermingham N, Kaar G. Interdural spinal cyst: a rare clinical entity. World Neurosurg. 2016;88:688.e9-688.e12. [DOI] [PubMed] [Google Scholar]
- 10.Dong RP, Zhang Q, Yang LL, Cheng XL, Zhao JW. Clinical management of dural defects: a review. World J Clin Cases. 2023;11(13):2903-2915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DeLuca GC, Boes CJ, Krueger BR, Mokri B, Kumar N. Ventral intraspinal fluid-filled collection secondary to CSF leak presenting as bibrachial amyotrophy. Neurology. 2011;76(16):1439-1440. [DOI] [PubMed] [Google Scholar]
- 12.Kumar N. Beyond superficial siderosis: introducing “duropathies.” Neurology. 2012;78(24):1992-1999. [DOI] [PubMed] [Google Scholar]
- 13.Payer M, Sottas C, Bonvin C. Superficial siderosis of the central nervous system: secondary progression despite successful surgical treatment, mimicking amyotrophic lateral sclerosis. Case report and review. Acta Neurochir (Wien). 2010;152(8):1411-1416. [DOI] [PubMed] [Google Scholar]
- 14.Shih P, Yang BP, Batjer HH, Liu JC. Surgical management of superficial siderosis. Spine J. 2009;9(8):e16-e19. [DOI] [PubMed] [Google Scholar]
- 15.Várallyay P, Nagy Z, Szűcs A, et al. Miyazaki syndrome: cervical myelo/radiculopathy caused by overshunting. A systematic review. Clin Neurol Neurosurg. 2019;186:105531. [DOI] [PubMed] [Google Scholar]
- 16.Mokri B. The Monro–Kellie hypothesis: applications in CSF volume depletion. Neurology. 2001;56(12):1746-1748. [DOI] [PubMed] [Google Scholar]
- 17.Fujimori J, Kikuchi H, Kameyama M, et al. A case of overshunting-associated myelopathy that developed 27 years after placement of a ventriculoperitoneal shunt. Neurol Clin Neurosci. 2021;9(3):230-232. [Google Scholar]
- 18.Wnuk E, Maj E, Dziedzic T, Podlecka Piętowska A. Spinal epidural venous plexus enlargement as a cause of neurologic symptoms: vascular anatomy and MRI findings. Neurol India. 2020;68(5):1238-1241. [DOI] [PubMed] [Google Scholar]
- 19.Hingwala D, Chatterjee S, Kesavadas C, Thomas B, Kapilamoorthy TR. Applications of 3D CISS sequence for problem solving in neuroimaging. Indian J Radiol Imaging. 2011;21(2):90-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hosokawa M, Murata KY, Hironishi M, et al. Superficial siderosis associated with duplicated dura mater detected by CISS reverse MRI. J Neurol Sci. 2018;392:38-43. [DOI] [PubMed] [Google Scholar]
- 21.Egawa S, Yoshii T, Sakaki K, et al. Dural closure for the treatment of superficial siderosis: report of 2 cases. J Neurosurg Spine. 2013;18(4):388-393. [DOI] [PubMed] [Google Scholar]
- 22.Kumar N, Lane JI, Piepgras DG. Superficial siderosis: sealing the defect. Neurology. 2009;72(7):671-673. [DOI] [PubMed] [Google Scholar]
- 23.Desai A, Ball PA, Bekelis K, et al. SPORT: does incidental durotomy affect long-term outcomes in cases of spinal stenosis? Neurosurgery. 2011;69(1):38-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Desai A, Ball PA, Bekelis K, et al. Surgery for lumbar degenerative spondylolisthesis in spine patient outcomes research trial: does incidental durotomy affect outcome? Spine. 2012;37(5):406-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fang Z, Tian R, Jia YT, Xu TT, Liu Y. Treatment of cerebrospinal fluid leak after spine surgery. Chin J Traumatol. 2017;20(2):81-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Endo T, Takahashi T, Jokura H, Tominaga T. Surgical treatment of spinal intradural arachnoid cysts using endoscopy: clinical article. J Neurosurg Spine. 2010;12(6):641-646. [DOI] [PubMed] [Google Scholar]
- 27.Ito A, Endo T, Inoue T, Endo H, Sato K, Tominaga T. Use of indocyanine green fluorescence endoscopy to treat concurrent perimedullary and dural arteriovenous fistulas in the cervical spine. World Neurosurg. 2017;101:814.e1-814.e6. [DOI] [PubMed] [Google Scholar]
- 28.Baron EM, Levene HB, Heller JE, Jallo JI, Loftus CM, Dominique DA. Neuroendoscopy for spinal disorders: a brief review. Neurosurg Focus. 2005;19(6):E5. [DOI] [PubMed] [Google Scholar]