Abstract
BACKGROUND
Kyphotic spinal deformity is a complication of ankylosing spondylitis (AS). In rare cases, particularly in obese patients, the deformity might extend to the cervicothoracic spine, resulting in a severe “chin-on-abdomen” deformity. This condition severely impairs quality of life by affecting gaze, swallowing, and causing chronic pain. While corrective surgery is often performed for lumbar and thoracic kyphosis, cases involving global kyphotic deformities are less common.
OBSERVATIONS
The authors present the case of a 66-year-old obese man with AS and a chin-on-abdomen deformity. Prone positioning for surgery was not feasible due to his body habitus. A three-stage corrective surgery was performed: a C7 extension osteotomy in a semisitting position, an L3 pedicle subtraction osteotomy in the lateral decubitus position, and a T11 vertebral column resection in the prone position. The first stage utilized a seldom-used, earlier osteotomy technique with modern instrumentation and neuromonitoring. Obesity again precluded prone positioning in the second stage, necessitating surgery in the lateral position. Postoperatively, the patient exhibited significant postural improvement, maintained over a 5-year follow-up period.
LESSONS
This case underscores the importance of adaptable techniques and positioning strategies in correcting complex spinal deformities in obese patients with AS. Integrating traditional methods with modern technology is crucial for achieving successful outcomes.
Keywords: ankylosing spondylitis, osteoclastic osteotomy, pedicle subtraction osteotomy, global kyphotic deformity
ABBREVIATIONS: AS = ankylosing spondylitis, CBVA = chin-brow vertical angle, CT = computed tomography, PSO = pedicle subtraction osteotomy, VCR = vertebral column resection.
Kyphotic spinal deformity is one of the classic manifestations of ankylosing spondylitis (AS). It has been suggested that the vertebral wedging observed in patients with AS who have hyperkyphosis is caused not only by the loss of disc height but also by periarticular bone loss due to osteoporosis, which can be global or restricted to the spine.1 This condition is more common among older men with a longer duration of disease. Typically, hyperkyphosis is distributed along the lumbar, thoracolumbar, and thoracic spine, as ossification of the spinal column is classically said to start at the sacroiliac joint and progress cranially.2 This is now known to not always be true, and in some cases the kyphotic deformity can affect the cervicothoracic spine, leading to a distinctive “chin-on-chest” deformity. This condition can significantly compromise a patient’s quality of life by causing an inability to maintain horizontal gaze, dysphagia, and chronic neck pain.2, 3 Numerous reports document favorable clinical outcomes following corrective osteotomies in the lumbar and thoracic spine, despite the associated risk of neurological complications.4, 5 Surgical reports that deal with global kyphotic deformities with simultaneous lumbar and cervicothoracic spine kyphosis that necessitate multiple three-column osteotomies are far less common, and these global kyphotic deformities have been described as “chin-on-pubis.” However, these successful reports for chin-on-pubis deformities describe predominantly posterior approaches that are best performed with the patient in a prone position. We present a case with the rare combination of obesity and a global, fixed kyphotic deformity, which made it impossible to place the patient prone, and describe alternative osteotomies and positioning strategies to correct this challenging case, which we describe as a “chin-on-abdomen” deformity. We also review the literature and discuss the precautions, potential risks, perils, and pitfalls of this kind of surgery.
Illustrative Case
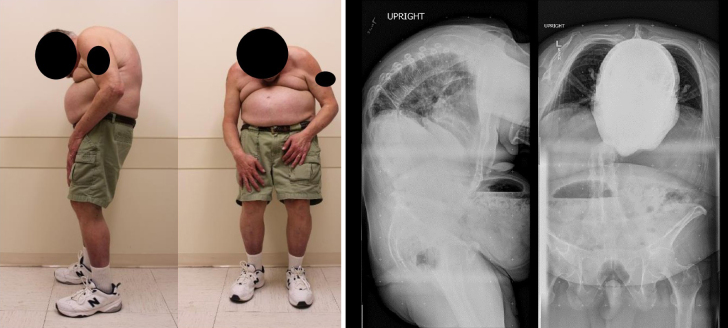
A 66-year-old obese man with AS diagnosed in his late 20s presented to our clinic with a long-standing chin-on-abdomen deformity, leading to marked dysphagia to solid foods, neck and back pain, difficulty maintaining horizontal gaze, and a consequent inability to perform activities of daily living and self-care. The kyphosis had acutely worsened 5 years prior to presentation following a T11 fracture that was managed nonoperatively elsewhere. On physical examination, a global kyphotic deformity with a chin-on-abdomen deformity was obvious, though the patient was neurologically intact. His chin-brow vertical angle (CBVA) was 103°. Full-spine radiography and computed tomography (CT) demonstrated a completely ankylosed spine with a global kyphotic deformity (Fig. 1). As with most global fixed deformities, nonoperative management was not effective, and a multidisciplinary, comprehensive surgical plan was devised, discussed with the patient, and accepted. Preoperative bone quality was assessed with dual-energy x-ray absorptiometry. Because of AS, the radius was the only suitable site for assessment, revealing a normal T-score of 0.4. Preoperative evaluations by the anesthesia, cardiology, and pulmonology teams were completed, including an assessment for difficult airway management, and the patient was cleared for surgery.
FIG. 1.
Lateral and frontal photographs (left) and whole-spine radiographs (right) of the patient before the operations.
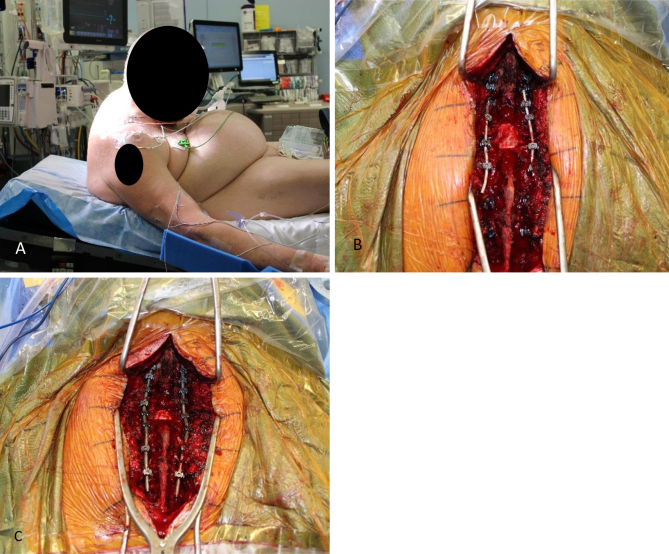
It was obvious that prone positioning was not an initial option. On the CT topogram, the distance between the chin and sternum was 58 mm, not accounting for soft tissue, and no support could be placed there. The first corrective surgery was then performed with the patient under general anesthesia and in a sitting position, with multimodal neurophysiological monitoring of somatosensory evoked potentials and motor evoked potentials during a C7 extension osteotomy (Smith-Petersen) and C3–T4 instrumented fusion (Fig. 2). The patient recovered well with only mild, transient C8 radiculopathy, which resolved within 3 months. The original plan for the second stage was to perform an L3 pedicle subtraction osteotomy (PSO) in the prone position; however, even under general anesthesia and neuromuscular blockade, prone positioning was still not possible because the patient could not be ventilated due to elevated airway pressure. Thus, the second stage in the prone position was aborted, and we created an alternate plan with a left lateral decubitus posterior approach for an L3 PSO and T12–S1 posterior instrumented fusion (Fig. 3). Initially planned under neuronavigation, screw positioning was performed under anatomical guidance due to the inability to close the O-arm around the patient. The third and final stage was performed with the patient in the prone position without any difficulty and involved a T11 vertebral column resection (VCR) and completion of the fusion by extension and connection, C3–S1 (Fig. 4). Alignment parameters before surgery and after each surgical stage are listed in Table 1. The total time between the first and third surgical stages was 13 months. His only perioperative complication was a right upper-extremity deep venous thrombosis between stages 1 and 2, which was treated with anticoagulation for 6 months. He is now 5 years out from surgery, with a dramatically increased quality of life, the ability to perform all activities of self-care except for clipping his toenails, and no neck or back pain. He has declined any further corrections of sagittal imbalance or coronal offset, stating that he is not bothered by the coronal offset and that he feels he is at the limit of being able to go down a flight of stairs without difficulty with the current CBVA.
FIG. 2.
A: Semisitting positioning of the patient during the first stage of surgery. B: Temporary rods have been placed between the C5 and C6 lateral mass and T1–2 pedicular screws, and a wide laminectomy of C7 is shown. C: After finishing extension of the osteotomy, the final rods were placed between C3 and T4 bilaterally.
FIG. 3.
Left lateral decubitus position, from two perspectives, for the second stage of surgery, an L3 PSO and T12–S1 fusion.
FIG. 4.
Lateral whole-spine radiographs of the patient after the first (A), second (B), and third (C) stages of surgery. The procedures included C7 Smith-Petersen osteotomy, L3 PSO, and T11 VCR, respectively. Lateral photograph of the patient after the final surgery (D).
TABLE 1.
Preoperative and final alignment parameters
| Parameter | Preop | After 1st Stage | After 2nd Stage | After 3rd Stage |
|---|---|---|---|---|
| CBVA (˚) | 103 | 50 | 35 | 25 |
| C7–SVA (mm) | +216 | +216 | +129 | +69 |
| PI (˚) | 56 | 56 | 56 | 56 |
| PT (˚) | 50 | 24 | 37 | 31 |
| SS (˚) | 5 | 32 | 21 | 24 |
| LL (°) | 22 | 26 | 47 | 44 |
| TK T5–12 (˚) | 101 | 96 | 70 | 58 |
| CL C2–T1 (˚) | 10 | 26 | 28 | 28 |
| C7–CSVL (mm) | 54 to rt | 45 to rt | 50 to rt | 59 to rt |
CL = cervical lordosis; CSVL = central sacral vertical line; LL = lumbar lordosis; PI = pelvic incidence; PT = pelvic tilt; SS = sacral slope; SVA = sacral vertical axis; TK = thoracic kyphosis.
Informed Consent
The necessary informed consent was obtained in this study.
Discussion
Observations
A global fixed kyphotic deformity is one of the most debilitating consequences of AS and a markedly difficult surgical challenge. Numerous reports have described single or double three-column osteotomies in the thoracolumbar spine for the correction of these deformities;6 few studies have described the occurrence of a triple three-column osteotomy in the same patient and, most importantly, the utilization of unorthodox osteotomies, as in our case.7, 8 Although PSOs and VCRs are part of the deformity surgeon’s armamentarium, the classic Smith-Petersen–type cervical extension osteotomy, a technique historically developed by Simmons9 and Urist10 and later refined by numerous spine surgeons,11, 12 has largely been abandoned in recent years due to several factors: the increased utilization of disease-modifying drugs for AS, which have led to improved clinical outcomes; the unpredictability of the osteoclastic maneuver; reports of elevated rates of neurological morbidity and pseudarthrosis; and, finally, the increased popularity of more conventional and controllable upper thoracic three-column osteotomies such as the PSO or VCR. The inability to place our patient prone and the limited thoracic visualization in the sitting position (exposure was limited to T4) led us to choose this osteotomy, and we present one of the few modern reports of its utilization, i.e., with efficient posterior instrumentation and modern neuromonitoring techniques.
After placing the patient in a semisitting position and applying the Mayfield head holder, instrumentation was placed from C3 to T4 by utilizing lateral mass screws from C3 to C6 and pedicle screws from T1 to T4. The osteotomy procedure began with a wide C6 to T1 laminectomy and bilateral decompression of the C8 nerve roots. Using 5-mm-wide osteotomes, stress risers were symmetrically created on both sides of the C7 vertebral body, while carefully retracting the C8 nerve roots medially to avoid injury. Before performing the sharp osteotomy on each side, a temporary rod was inserted between the C5, C6, T1, and T2 screws on the contralateral side to prevent translation and potential spinal cord injury. After loosening the bilateral screw nuts below the osteotomy level (T1 and T2), the assistant surgeon gently extended the patient’s head to achieve osteoclasis or an open wedge fracture of the anterior spinal column. Further correction was accomplished with mild compression between the C6 lateral mass screws and the T1 pedicle screws. Finally, the rods were securely fixed bilaterally. Throughout the procedure, strict control of the patient’s head and trunk was maintained to prevent inadvertent translation of the opened segment before the osteotomy was stabilized.
Despite the good outcome of the first osteotomy, we were still unable to position the patient prone for the second stage after multiple attempts. A lateral lumbar PSO has been reported in only three patients,13, 14 all of them with AS and an inability to be positioned prone due to severe hip contractures. Song et al.14 reported two cases of AS treated with a lateral-position PSO due to hip flexion contracture and spine rigidity, with comparable surgical timing and blood loss to the prone procedure. Ma et al.13 also demonstrated that double-level spinal osteotomy in a lateral position could be an alternative for patients with AS who cannot be placed prone. We followed the recommendations of Ma et al. to tilt the patient away from the surgical team 10°–20° and encountered the same reported challenge in performing the osteotomy on the side facing the floor. Our findings during this case allow us to suggest a wide soft tissue dissection, comprehensive dissection of the posterior elements, performing most of the work from the side closer to the ceiling of the room, and placing the PSO at L3 (as opposed to L4 or L5) as useful techniques to mitigate the difficulties intrinsic to operating in this nonergonomic position. Compared to the unorthodox procedures utilized in the initial steps of our case, the conventional thoracic VCR, performed with the patient finally in the prone position, was relatively lacking in novelty but resulted in a very functional outcome in terms of alignment and function.
Lessons
Correction of chin-on-chest deformities is complex. The risks along each step of the process are substantial, and patients must be aware that the risk of permanent deficits or mortality is high before embarking on this multistage endeavor. Only subspecialized deformity groups should undertake these corrections, given the risks and technical demands associated with certain osteotomies. Even with extensive planning, surgeons must be ready to adapt and deploy unorthodox surgical approaches to achieve adequate surgical correction, all while maintaining patient safety at the forefront. If successful, patients can benefit by regaining the independence that they once lost to these debilitating deformities.
Disclosures
Dr. Fontes reported personal fees from Globus Medical outside the submitted work.
Author Contributions
Conception and design: Fontes, Rostami, Varela, Kerolus. Acquisition of data: Fontes, Varela. Analysis and interpretation of data: Fontes, Kerolus. Drafting the article: Fontes, Rostami, Varela, Kerolus. Critically revising the article: Fontes, Varela, Kerolus, DeWald. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Fontes. Study supervision: Fontes.
Correspondence
Ricardo B. V. Fontes: Rush University Medical Center, Chicago, IL. ricardo_fontes@rush.edu.
References
- 1.What causes hyperkyphosis in patients with ankylosing spondylitis? Nat Clin Pract Rheumatol. 2006;2(9):463-463. [DOI] [PubMed] [Google Scholar]
- 2.Belanger TA, Milam RA, Roh JS, Bohlman HH. Cervicothoracic extension osteotomy for chin-on-chest deformity in ankylosing spondylitis. J Bone Joint Surg Am. 2005;87(8):1732-1738. [DOI] [PubMed] [Google Scholar]
- 3.Guo XH, Ji HQ. Surgical treatment of a cervical spine fracture in an ankylosing spondylitis patient with severe global spine kyphosis and chin-on-chest deformity. Chin Med J (Engl). 2019;132(21):2644-2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Shaughnessy BA, Kuklo TR, Hsieh PC, Yang BP, Koski TR, Ondra SL. Thoracic pedicle subtraction osteotomy for fixed sagittal spinal deformity. Spine (Phila Pa 1976). 2009;34(26):2893-2899. [DOI] [PubMed] [Google Scholar]
- 5.Willems KF, Slot GH, Anderson PG, Pavlov PW, de Kleuver M. Spinal osteotomy in patients with ankylosing spondylitis: complications during first postoperative year. Spine (Phila Pa 1976). 2005;30(1):101-107. [DOI] [PubMed] [Google Scholar]
- 6.Li S, Chen L, Ye F, et al. Comparison of one-level osteotomy and two-level osteotomy for thoracolumbar kyphotic deformity in ankylosing spondylitis: a systematic review and meta-analysis. World Neurosurg. 2023;173:176-187.e1. [DOI] [PubMed] [Google Scholar]
- 7.Mugge L, Gorka P, Brewer C, McHugh B. Multiple three-column osteotomies successfully correcting cervicothoracic kyphosis in the setting of ankylosing spondylitis: illustrative case. J Neurosurg Case Lessons. 2024;7(11):CASE23708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim KT, Lee SH, Son ES, Kwack YH, Chun YS, Lee JH. Surgical treatment of “chin-on-pubis” deformity in a patient with ankylosing spondylitis: a case report of consecutive cervical, thoracic, and lumbar corrective osteotomies. Spine (Phila Pa 1976). 2012;37(16):E1017-E1021. [DOI] [PubMed] [Google Scholar]
- 9.Simmons EH. The surgical correction of flexion deformity of the cervical spine in ankylosing spondylitis. Clin Orthop Relat Res. 1972;86:132-143. [DOI] [PubMed] [Google Scholar]
- 10.Urist MR. Osteotomy of the cervical spine: report of a case of ankylosing rheumatoid spondylitis. J Bone Joint Surg Am. 1958;40-A(4):833-843. [PubMed] [Google Scholar]
- 11.Wollowick AL, Kelly MP, Riew KD. Osteotomies for the treatment of cervical kyphosis caused by ankylosing spondylitis: indications and techniques. Semin Spine Surg. 2011;23(3):188-198. [Google Scholar]
- 12.Sengupta DK, Khazim R, Grevitt MP, Webb JK. Flexion osteotomy of the cervical spine: a new technique for correction of iatrogenic extension deformity in ankylosing spondylitis. Spine (Phila Pa 1976). 2001;26(9):1068-1072. [DOI] [PubMed] [Google Scholar]
- 13.Ma S, Zhou Z, Yu H, Wu C, Deng W, Cao K. Two-level pedicle subtraction osteotomy in lateral position for an ankylosing spondylitis patient with severe thoracolumbar kyphosis and hip flexion contracture: a case report. Oper Neurosurg (Hagerstown). 2022;23(1):e72-e76. [DOI] [PubMed] [Google Scholar]
- 14.Song DY, Zhang ZF, Wang TH, Qi DB, Wang Y, Zheng GQ. Pedicle subtraction osteotomy in lateral position: a new strategy for correcting severe thoracolumbar kyphosis combined with hip flexion contracture in ankylosing spondylitis. Orthop Surg. 2021;13(8):2396-2404. [DOI] [PMC free article] [PubMed] [Google Scholar]