Abstract
Background
Triglyceride glucose index(TyG) and a body shape index(ABSI) are both independent predictor of stroke incidence or adverse prognosis but these two indicators seldom were combined to predict. The purpose of this study is to evaluate whether the combination of TyG and ABSI better predict the incidence of stroke.
Methods
Based on the China Health and Retirement Longitudinal Study(CHARLS), 8,257 people aged 45 years and older without stroke were enrolled and followed up to 9 years. Sociodemographic information, health status, physical examination and blood data were collected retrospectively. Cox regressions were to determine the relationship between different groups and stroke incidence, using receiver operating characteristic curves to evaluate the diagnostic value. Meanwhile, subgroup analysis was performed to investigate the prediction performance among different population.
Results
672(8.14%) of 8,257 participants had stroke incidence during 9 years. In the adjusted multivariate cox regression model, both TyG and ABSI were still predictors of stroke. The HR of TyG was 1.25(95%CI: 1.06–1.47) and the HR of ABSI was 1.33(95%CI: 1.06–1.68). Restricted cubic spline regression showed the associations between TyG or ABSI and stroke. The combination of TyG and ABSI had the highest diagnostic efficacy(AUC: 0.579, 95%CI: 0.553–0.597), compared to TyG(AUC:0.566, 95%CI: 0.544–0.587) and ABSI(AUC:0.533, 95%CI: 0.524–0.597). Kaplan-Meier curves showed that the highest cumulative stroke incidence was among people with high TyG and ABSI(TyG ≥ 8.5742, ABSI ≥ 0.0852; P < 0.0001), which had the highest HR of stroke incidence(HR:1.64, 95%CI:1.2–2.24).
Conclusion
The combined prediction of TyG and ABSI had higher clinical value and enabled earlier detection of the stroke in the general population, which could be monitored and intervened to reduce the overall burden of stroke.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12933-024-02569-5.
Keywords: Triglyceride glucose, A body shape index, Stroke, Joint indicator, CHARLS
Introduction
According to the global burden of disease study(GBD) 2021, ischemic stroke remained high global burden with a significant increase in absolute cases and it is necessary to explore the risk factors that could predict the occurrence of stroke to take early intervention [1, 2]. Obesity was a well-known risk factor of stroke incidence and body mass index(BMI) was the most commonly index used to assess obesity status [3, 4]. But single index analysis based on BMI easily resulted in “obesity paradox” [5, 6], because BMI cannot provide information about body composition, fat distribution and body metabolism, which also had influence on the incidence and adverse outcomes of cardio-cerebrovascular diseases [7, 8]. Hence, there was a growing interest in identifying more comprehensive indicators providing more information about stroke. A Body Shape Index(ABSI) is a variant of taper index, which is not affected by “obesity paradox” and provides more information about physical fitness, combining BMI with waist circumference(WC), a visceral fat measurement [8, 9]. As for body metabolism, insulin resistance(IR) is an essential factor of cardio-cerebrovascular diseases including stroke [10, 11]. And triglyceride glucose(TyG) index calculating based on fasting glucose and triglycerides, is a simple and reliable measurement tool for IR [12, 13].
Recently, researchers had found TyG is an independent predictor of the occurrence and adverse outcome of stroke [14–17]. When TyG is combined with obesity indeices, such as BMI, WC and waist-height ratio(WHtR), these joint associations have better predictive effectiveness than single TyG index on cardio-cerebrovascular diseases [18–20]. ABSI, an indicator unaffected by “obesity paradox” with more physical information, is superior to other obesity indices(BMI, WC and WHtR) in terms of representation of physical fitness [8, 9], having proved a valuable predictor of stroke incidence [21–23]. Nevertheless, there are few studies dealing with the combined impact of TyG and ABSI on the stroke incidence. The purpose of this study is to evaluate whether the combination of TyG and ABSI better predict the incidence of stroke based on the data from the China Health and Retirement Longitudinal Study(CHARLS) 2011–2020.
Methods
Study population
This study was a secondary analysis sourced from CHARLS from 2011 to 2020. CHARLS is conducted by the National School of Development at Peking University, which is a nationally representative longitudinal survey among adults aged 45 years or older, approved by the Institutional Review Board of Peking University(IRB00001052-11015). All subjects provided written informed consent prior to participating in the CHARLS study. This study was conducted in accordance with Enhanced Observational Epidemiological Research Reports (STROBE) reporting guidelines [24]. Detailed information of the study population, study design and cohort profile have been described in other publications previously [25]. The first CHARLS survey conducted in 2011–2012 as baseline(Wave 1) and subsequently follow-up surveys had been completed every two years(Wave 2 in 2013, Wave 3 in 2015, Wave 4 in 2018 and Wave 5 in 2020).
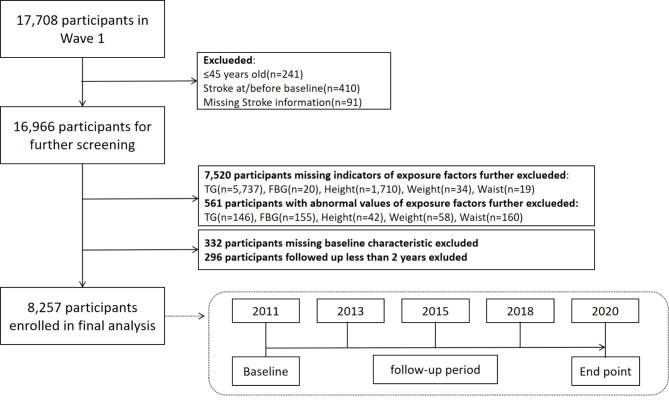
Our study downloaded data(https://charls.pku.edu.cn/) from 5 waves of CHARLS(2011, 2013, 2015, 2018, 2020). The initial survey in 2011 included 17,708 participants. For this study, participants had to be aged 45 years old and older without stroke, so 16,966 participants were eligible for further screening. 7,520 participants were excluded without data on triglycerides(TG), fasting blood glucose(FBG), height, weight and WC. Respondents who had abnormal values for exposure factors were further exclueded(n = 561). People were also excluded if their baseline characteristic was incomplete or they had followed up less than two years. 8,257 respondents met all requirements and were enrolled in final analysis. The comparison between the excluded population with absence or abnormal of exposure factors and the final included population was displayed in Additional File 1: Table S1–S2. The flow chart of population selection in this study is shown in Fig. 1.
Fig. 1.
Flowchart illustrating the selection of the study population. TG triglyceride, FBG fasting blood glucose
Data assessment
Outcome ascertainment
The primary outcome of this study was the incidence of stroke. In follow-up period, participants who had answered “yes” to the question of “Have you been diagnosed with stroke by a doctor?” were considered as occurring stroke events according to previous studies [20, 26, 27].
Assessment of TyG and ABSI
The exposure of this study were TyG index and ABSI index. Blood sample were collected by the staff of the Chinese Center for Disease Control and Prevention(China CDC) and were almost collected after a night of fasting. Enzymatic colormetric tests were used to assess TG and FBG and the coefficient of variations between-assay was 1.80%. The Chinese Ministry of Health organizes regular external quality assessment. This laboratory conducts assay quality control samples on a daily basis and has excellent performance during annual evaluation by External Quality Assurance (EQA) Program organized by the National Center for Clinical Laboratories, Chinese Ministry of Health. The TyG index was calculated by this formula “TyG index = ln[TG(mg/dl) × FBG(mg/dl/2)]” [28]. As for physical examination, height was measured by a vertical altimeter and weight was measured by a weight scale. WC was measured by a soft ruler measuring the length of the navel horizontal circle around the waist when participant stood. The formula of body mass index(BMI) was “BMI = Weight(kg)/Height(m)2” [29]. According to previous studies [30], ABSI was calculated based on “ABSI = WC(m) × Weight(kg)−2/3 ”.
”.
Data collection
Trained investigators collected sociodemographic and health status information through the structured questionnaire during survey in Wave 1. Sociodemographic data included gender, age, education level(elementary school and below, secondary school, college and above), marital status(married, other status) and Hukou(the system of household registration: agriculture, others). Health status data included self-reported smoke and drink status(yes or no) and self-reported doctor-diagnosed diseases(hypertension, diabetes, dyslipidemia and heart-problems). This study also included basic anthropometric measurements(height, weight, WC and BMI) and laboratory examination data, containing TG, FBG, glycated hemoglobin(HbA1c), high density lipoprotein cholesterol(HDL), low density lipoprotein cholesterol(LDL) and total cholesterol(TC).
Statistical analysis
The baseline characteristics were summarized according to the ABSI index quartile groups, the TyG index median value and the combined ABSI and TyG groups. Descriptive statistics(continuous data using means and standard deviation, SD, categorical data using quantity and percentage) were used to report basic characteristics. Differences in baseline features between classes were analyzed through the t-test or Mann-Whitney U test for continuous variables and chi-square test or Fisher’s exact test for categorical variables. Histograms were used to describe the distribution of TyG and ABSI in the study population. A generalized variance inflation factor(GVIF) analysis was used to identify variables with multicollinearity. We also adjusted for variables if their p-values were less than 0.1 for univariate analysis or if they were chosen on the basis of previous findings and clinical constraints. Setting new stroke incidence as the primary outcome events, cox hazard regression models were used to assess hazard ratios (HR) and 95% confidence intervals(95% CIs) for outcomes associated with ABSI (categorized as quartile), TyG (categorized based on mean value) and the combination of ABSI and TyG(categorized as 8 groups). The crude model and three adjusted model were estimated. Model 1 adjusted age and gender, while model 2 were adjusted for age, gender and socio-demographic information(education levels, marital status, smoking and drinking status, and BMI). Model 3 were adjusted for factors in model 2 and disease history(hypertension, dyslipidemia, diabetes and heart problems). Restricted cubic spline(RCS) regression were used to explore the potential non-liner associations between TyG or ABSI and stroke incidence. The cumulative incidence of stroke events based on the combined ABSI and TyG grouping was represented by the Kaplan-Meier curve. Receiver operating characteristic(ROC) curves were used to evaluate the diagnostic value and the area under the curves (AUC) were calculated to quantify the predictive power of ABSI, TyG, and the combination of ABSI and TyG for stroke occurrence.
In addition, subgroup analysis was performed to investigate whether the association between stroke occurrence and the combination of ABSI and TyG varied according to the state of the covariates(age, gender, marital status, education levels, smoke and drinking status, diabetes, dyslipidemia and heart-problems). All Statistical analyses were performed using R version 4.4.0 software(R Foundation for Statistical Computing, http://www.R-project.org/). Bilateral P < 0.05 were considered statistically significant.
Results
Baseline characteristics of study participants
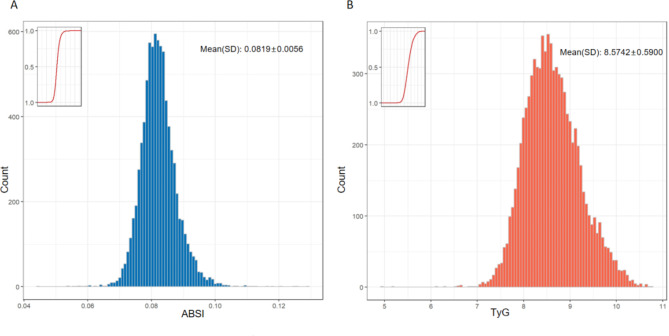
A total of 8726 participants in CHARLS from 2011 to 2020 were included in this study with an average age of 60.88(± 9.36) and 46.0% males. The quartile of ABSI index were 0.0788(Q1), 0.0819(Q2) and 0.0852(Q3). The median of TyG index was 8.5742. Figure 2 showed the distribution of ABSI and TyG. People with higher TyG index also had higher weight, waist circumference, HbA1c, FBG, TC, LDL and TG(Table 1). People were described based on the combined ABSI and TyG showed in Additional File 1: Table S3.
Fig. 2.
Distribution of ABSI index ad TyG index. A distribution of ABSI index, B distribution of TyG index
Table 1.
Baseline Characteristic according to ABSI and TyG
| Characteristics | Total | ABSI Index | P-value | TyG Index | P-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| ABSI<0.0788 | 0.0788 ≤ ABSI<0.0819 | 0.0819 ≤ ABSI<0.0852 | 0.0852 ≤ ABSI | TyG<8.5742 | TyG ≥ 8.5742 | ||||
| n | 8257 | 2074 | 2059 | 2046 | 2078 | 4130 | 4127 | ||
| Gender (%) | < 0.001 | < 0.001 | |||||||
| Male | 3797 (46.0) | 1008 (48.6) | 1071 (52.0) | 998 (48.8) | 720 (34.6) | 2096 (50.8) | 1701 (41.2) | ||
| Female | 4460 (54.0) | 1066 (51.4) | 988 (48.0) | 1048 (51.2) | 1358 (65.4) | 2034 (49.2) | 2426 (58.8) | ||
| Age. years (mean (SD)) | 60.88 (9.36) | 57.26 (8.19) | 59.19 (8.46) | 61.09 (8.83) | 65.96 (9.58) | < 0.001 | 60.79 (9.55) | 60.97 (9.17) | 0.37 |
| Education.level (%) | < 0.001 | 0.545 | |||||||
| Elementary school and below | 3797 (46.0) | 1305 (62.9) | 1374 (66.7) | 1436 (70.2) | 1693 (81.5) | 2916 (70.6) | 2892 (70.1) | ||
| Secondary school | 4460 (54.0) | 723 (34.9) | 658 (32.0) | 583 (28.5) | 374 (18.0) | 1154 (27.9) | 1184 (28.7) | ||
| College and above | 60.88 (9.36) | 46 ( 2.2) | 27 ( 1.3) | 27 ( 1.3) | 11 ( 0.5) | 60 ( 1.5) | 51 ( 1.2) | ||
| Marital.status (%) | < 0.001 | 0.603 | |||||||
| Married | 7265 (88.0) | 1883 (90.8) | 1854 (90.0) | 1822 (89.1) | 1706 (82.1) | 3642 (88.2) | 3623 (87.8) | ||
| Others | 992 (12.0) | 191 ( 9.2) | 205 (10.0) | 224 (10.9) | 372 (17.9) | 488 (11.8) | 504 (12.2) | ||
| Hukou (%) | 0.0614 | < 0.001 | |||||||
| Agriculture | 6867 (83.2) | 1724 (83.1) | 1726 (83.8) | 1684 (82.3) | 1733 (83.4) | 3525 (85.4) | 3342 (81.0) | ||
| Others | 1390 (16.8) | 350 (16.9) | 333 (16.2) | 362 (17.7) | 345 (16.6) | 605 (14.6) | 785 (19.0) | ||
| Smoke (%) | < 0.001 | < 0.001 | |||||||
| Yes | 3179 (38.5) | 816 (39.3) | 875 (42.5) | 812 (39.7) | 676 (32.5) | 1722 (41.7) | 1457 (35.3) | ||
| No | 5078 (61.5) | 1258 (60.7) | 1184 (57.5) | 1234 (60.3) | 1402 (67.5) | 2408 (58.3) | 2670 (64.7) | ||
| Drink (%) | < 0.001 | < 0.001 | |||||||
| Yes | 2668 (32.3) | 696 (33.6) | 752 (36.5) | 670 (32.7) | 550 (26.5) | 1473 (35.7) | 1195 (29.0) | ||
| No | 5589 (67.7) | 1378 (66.4) | 1307 (63.5) | 1376 (67.3) | 1528 (73.5) | 2657 (64.3) | 2932 (71.0) | ||
| Hypertension (%) | < 0.001 | < 0.001 | |||||||
| Yes | 1903 (23.0) | 392 (18.9) | 453 (22.0) | 495 (24.2) | 563 (27.1) | 723 (17.5) | 1180 (28.6) | ||
| No | 6354 (77.0) | 1682 (81.1) | 1606 (78.0) | 1551 (75.8) | 1515 (72.9) | 3407 (82.5) | 2947 (71.4) | ||
| Diabetes (%) | < 0.001 | < 0.001 | |||||||
| Yes | 376 ( 4.6) | 69 ( 3.3) | 74 ( 3.6) | 108 ( 5.3) | 125 ( 6.0) | 109 ( 2.6) | 267 ( 6.5) | ||
| No | 7881 (95.4) | 2005 (96.7) | 1985 (96.4) | 1938 (94.7) | 1953 (94.0) | 4021 (97.4) | 3860 (93.5) | ||
| Dyslipidemia (%) | 0.038 | < 0.001 | |||||||
| Yes | 687 ( 8.3) | 151 ( 7.3) | 166 ( 8.1) | 199 ( 9.7) | 171 ( 8.2) | 229 ( 5.5) | 458 (11.1) | ||
| No | 7570 (91.7) | 1923 (92.7) | 1893 (91.9) | 1847 (90.3) | 1907 (91.8) | 3901 (94.5) | 3669 (88.9) | ||
| Heart.problems (%) | 0.002 | < 0.001 | |||||||
| Yes | 934 (11.3) | 218 (10.5) | 209 (10.2) | 226 (11.0) | 281 (13.5) | 404 ( 9.8) | 530 (12.8) | ||
| No | 7323 (88.7) | 1856 (89.5) | 1850 (89.8) | 1820 (89.0) | 1797 (86.5) | 3726 (90.2) | 3597 (87.2) | ||
| Height, cm (mean (SD)) | 157.86 (8.41) | 158.45 (7.78) | 158.94 (8.15) | 158.49 (8.38) | 155.59 (8.87) | < 0.001 | 158.16 (8.45) | 157.56 (8.36) | 0.001 |
| Weight, kg (mean (SD)) | 58.36 (10.71) | 58.68 (9.99) | 59.93 (10.68) | 59.63 (10.80) | 55.24 (10.70) | < 0.001 | 56.32 (10.07) | 60.40 (10.94) | < 0.001 |
| Waist, cm (mean (SD)) | 84.99 (9.83) | 78.53 (8.31) | 84.17 (8.73) | 87.28 (9.02) | 90.00 (9.33) | < 0.001 | 82.44 (9.12) | 87.55 (9.86) | < 0.001 |
| BMI, kg/m2 (mean (SD)) | 23.36 (3.57) | 23.35 (3.50) | 23.67 (3.55) | 23.68 (3.56) | 22.75 (3.57) | < 0.001 | 22.46 (3.30) | 24.26 (3.60) | < 0.001 |
| HbA1c, mg/dl (mean (SD)) | 5.19 (0.58) | 5.13 (0.53) | 5.17 (0.54) | 5.20 (0.59) | 5.26 (0.63) | < 0.001 | 5.10 (0.46) | 5.28 (0.66) | < 0.001 |
| FBG, mg/dl (mean (SD)) | 105.71 (21.21) | 102.65 (19.19) | 105.66 (20.50) | 107.22 (21.86) | 107.33 (22.79) | < 0.001 | 98.01 (14.55) | 113.41 (23.87) | < 0.001 |
| TC, mg/dl (mean (SD)) | 192.73 (37.47) | 187.58 (36.38) | 192.21 (36.37) | 194.95 (38.25) | 196.20 (38.26) | < 0.001 | 184.25 (34.05) | 201.21 (38.79) | < 0.001 |
| HDL, mg/dl (mean (SD)) | 51.84 (15.06) | 53.16 (14.94) | 52.09 (15.21) | 50.69 (15.03) | 51.39 (14.97) | < 0.001 | 57.85 (14.81) | 45.82 (12.74) | < 0.001 |
| LDL, mg/dl (mean (SD)) | 117.15 (33.97) | 113.44 (32.32) | 116.99 (33.66) | 118.85 (34.69) | 119.35 (34.88) | < 0.001 | 113.44 (30.22) | 120.87 (36.99) | < 0.001 |
| TG, mg/dl (mean (SD)) | 123.18 (71.24) | 115.04 (69.56) | 120.19 (67.67) | 128.71 (73.96) | 128.81 (72.69) | < 0.001 | 75.00 (20.38) | 171.38 (71.36) | < 0.001 |
BMIbody mass index, HbA1cglycated hemoglobin, FBGfasting blood glucose, TCtotal cholesterol, HDLhigh density lipoprotein cholesterol, LDLlow density lipoprotein cholesterol, TGtriglyceride, TyGtriglyceride glucose, ABSIa body shape index;Hukouthe system of household registration
Analyses of TyG or ABSI with incident stroke
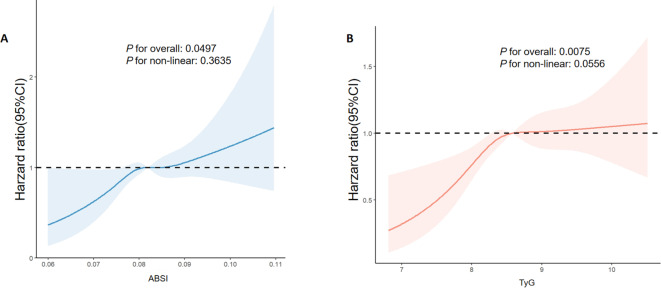
During a maximum follow-up period of 9 years, 672(8.14%) participants had occurred strokes. Table 2 showed the incidence risk of stroke stratified by ABSI and TyG. The incidence of stroke was 9.62% in the high TyG group and 10.11% in the highest ABSI group. High TyG index was a risk factor for stroke incidence and remained significance in the adjusted Model 3 with an HR of 1.25(95%CI: 1.06–1.47). HRs of 0.0852 ≤ ABSI in four models were significant statistically(P < 0.05), and the HR was 1.33(95%CI: 1.06–1.68) in the final adjusted Model 3, which indicated the risk of stroke was increased by 33%(Table 2). Based on Model 3, RCS regression analysis found that both ABSI index and TyG index had a linear relationship with stroke occurrence (ABSI: P for non-linear = 0.3635; TyG: P for non-linear = 0.0556; Fig. 3).
Table 2.
Incidence risk of stroke stratified by ABSI and TyG in baseline
| Case | Crude | Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P-value | HR(95%CI) | P-value | HR(95%CI) | P-value | HR(95%CI) | P-value | ||
| Total | 672(8.14%) | ||||||||
| TyG | |||||||||
| TyG<8.5742 | 275(6.66%) | Ref | Ref | Ref | Ref | ||||
| TyG ≥ 8.5742 | 397(9.62%) | 1.49(1.28–1.74) | < 0.0001 | 1.51(1.30–1.77) | < 0.0001 | 1.32(1.12–1.55) | 0.0007 | 1.25(1.06–1.47) | 0.0071 |
| ABSI | |||||||||
| ABSI<0.0788 | 133(6.41%) | Ref | Ref | Ref | Ref | ||||
| 0.0786 ≤ ABSI<0.0819 | 174(8.45%) | 1.36(1.06–1.67) | 0.0129 | 1.26(1.01–1.58) | 0.0445 | 1.21(0.97–1.52) | 0.0962 | 1.21(0.96–1.52) | 0.1001 |
| 0.0819 ≤ ABSI<0.0852 | 155(7.58%) | 1.20(0.95–1.52) | 0.1187 | 1.08(0.86–1.37) | 0.5035 | 1.04(0.82–1.31) | 0.7529 | 1.00(0.79–1.27) | 0.9726 |
| 0.0852 ≤ ABSI | 210(10.11%) | 1.71(1.38–2.13) | < 0.0001 | 1.36(1.08–1.71) | 0.0096 | 1.38(1.09–1.74) | 0.0065 | 1.33(1.06–1.68) | 0.0148 |
Model 1adjusted for age and gender;Model 2adjusted for age, gender, education levels, marital status, smoking status, drinking status, and BMI;Model 3adjusted for factors in model 2 and history of hypertension, dyslipidemia, diabetes and heart problems.
Fig. 3.
Nonlinear associations of ABSI and TyG with stroke incidence. A, B Graphs show HRs for stroke incidence based on Cox hazaeds regression model 3(adjusted for gender, age, marital status, education, level, smoking and drinking status, BMI, and history of hypertension, diabetes, dyslipidemia and heart problems). Solid lines indicate HRs. Shadow shapes indicate 95% CIs.
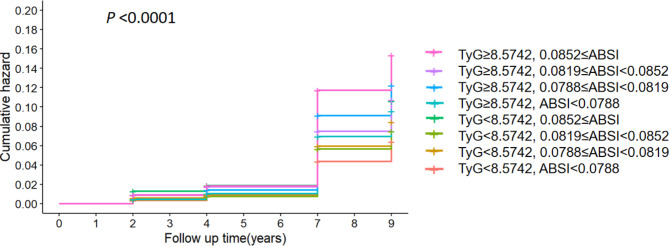
Joint analyses of TyG and ABSI with incident stroke
Combining ABSI and TyG, the study population were divided into eight groups and Fig. 4 displayed the Kaplan-Meier curves of the cumulative incidence of stroke among the overall study participants(P < 0.01). People with high TyG and the highest ABSI had the highest cumulative stroke incidence(Fig. 4). TyG < 8.5742 and ABSI < 0.0788 setting as reference group, Table 3 showed the stroke incidence risk of the other combined group. Regardless of TyG level, ABSI ≥ 0.0852 group had the highest incidence of stroke(TyG < 8.5742, ABSI ≥ 0.0852: 8.35%; TyG ≥ 8.5742, ABSI ≥ 0.0852: 11.57%). The risk of stroke incidence all increased significantly in four groups within high TyG index. These four groups’ HRs were 1.50(95%CI: 1.07–2.1; TyG ≥ 8.5742, ABSI < 0.0788), 1.92(95%CI: 1.4–2.63; TyG ≥ 8.5742, 0.0788 ≤ ABSI < 0.0819), 1.69(95%CI: 1.23–2.32; TyG ≥ 8.5742, 0.0819 ≤ ABSI < 0.0852) and 2.42(95%CI: 1.79–3.26;TyG ≥ 8.5997, ABSI ≥ 0.0852). In the final adjusted Model 3, the risk of stroke were still statistically significant in one group(TyG ≥ 8.5997, ABSI ≥ 0.0852, P = 0.0020). The group with TyG ≥ 8.5997 and ABSI ≥ 0.0852 had 64% increased risk compared to the reference group(Table 3).
Fig. 4.
K-M plot of stroke incidence by ABSI and TyG
Table 3.
Incidence risk of stroke stratified by the joint of ABSI and TyG
| Case | Crude | Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|---|---|
| HR(95%CI) | P-value | HR(95%CI) | P-value | HR(95%CI) | P-value | HR(95%CI) | P-value | ||
| TyG<8.5742 | |||||||||
| ABSI<0.0788 | 64(5.37%) | ref | ref | ref | ref | ||||
| 0.0788 ≤ ABSI<0.0819 | 74(6.99%) | 1.32(0.94–1.84) | 0.1039 | 1.22(0.87–1.70) | 0.2493 | 1.17(0.84–1.63) | 0.3624 | 1.19(0.85–1.67) | 0.3032 |
| 0.0819 ≤ ABSI<0.0852 | 58(6.21%) | 1.17(0.82–1.68) | 0.3748 | 1.05(0.73–1.49) | 0.8057 | 1.00(0.70–1.43) | 0.9883 | 1.02(0.71–1.46) | 0.9092 |
| 0.0852 ≤ ABSI | 79(8.35%) | 1.67(1.20–2.32) | 0.0023 | 1.31(0.94–1.85) | 0.1152 | 1.33(0.95–1.87) | 0.0976 | 1.29(0.92–1.82) | 0.1389 |
| TyG ≥ 8.5742 | |||||||||
| ABSI<0.0788 | 69(7.81%) | 1.50(1.07–2.10) | 0.0200 | 1.51(1.08–2.13) | 0.0175 | 1.28(0.91–1.81) | 0.1591 | 1.25(0.89–1.77) | 0.2015 |
| 0.0788 ≤ ABSI<0.0819 | 100(10.00%) | 1.92(1.40–2.63) | < 0.0001 | 1.88(1.37–2.57) | 0.0001 | 1.57(1.14–2.16) | 0.0056 | 1.50(1.09–2.07) | 0.0123 |
| 0.0819 ≤ ABSI<0.0852 | 97(8.72%) | 1.69(1.23–2.32) | 0.0011 | 1.55(1.13–2.67) | 0.0071 | 1.31(0.95–1.81) | 0.1006 | 1.20(0.87–1.66) | 0.2686 |
| 0.0852 ≤ ABSI | 131(11.57%) | 2.42(1.79–3.26) | < 0.0001 | 1.96(1.43–2.67) | < 0.0001 | 1.72(1.26–2.35) | 0.0007 | 1.64(1.2–2.24) | 0.0020 |
Model 1adjusted for age and gender;Model 2adjusted for age, gender, education levels, marital status, smoking status, drinking status, and BMI;Model 3adjusted for factors in model 2 and history of hypertension, dyslipidemia, diabetes and heart problems.
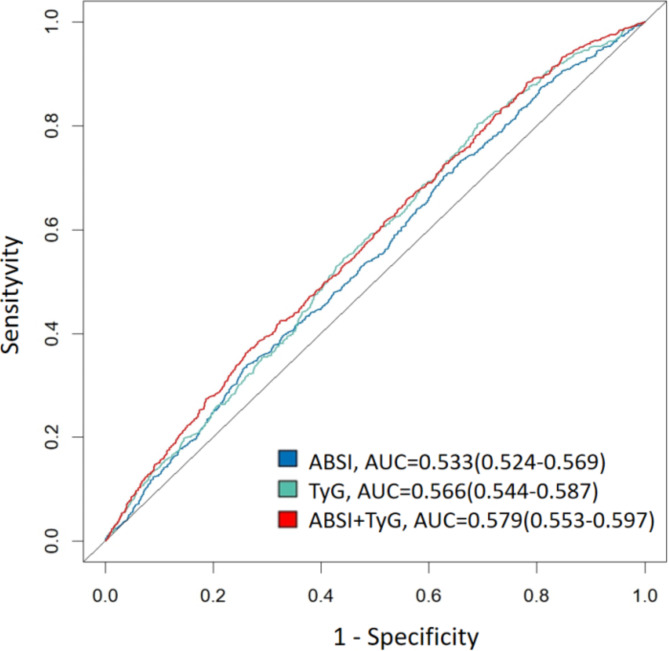
Predictive value of TyG and ABSI in incident stroke
Based on Model 3, the ROC curves indicated that combined with TyG and ABSI had the highest diagnostic efficacy of stroke incidence(AUC 0.579, 95% CI 0.533–0.597), followed by TyG(AUC:0.566, 95% CI: 0.544–0.587), and ABSI(AUC:0.533, 95% CI: 0.524–0.569; Fig. 5).
Fig. 5.
Receiver operating characteristic curves for ABSI, TyG and ABSI + TyG predicting stroke incidence based on Model 3
Subgroup analyses
Subgroup analyses were performed to stratify the relationship between stroke incidence and the combined ABSI and TyG group in Additional File 1: Table S4 A, B. Two groups of the combined ABSI and TyG(TyG ≥ 8.5742, 0.0788 ≤ ABSI < 0.0819; TyG ≥ 8.5742, ABSI ≥ 0.0852) with statically significance in model 3 were shown in Table 4. The joint indicator groups had interaction with gender(p for interaction: 0.021), age(p for interaction: 0.004) and smoking status(p for interaction:0.035). The risk of stroke was fairly equally pronounced in high and low educational level subgroups. Both in high and low BMI subgroups, the association was significant. High TyG and high ABSI pronounced stroke risk regardless of the presence of diabetes, dyslipidemia and heart problems. This association still significant in people with or without drinking.
Table 4.
Subgroups analysis of the joint association of ABSI and TyG with stroke incidence
| Case/total | TyG<8.5742 ABSI<0.0788 | TyG ≥ 8.5742 0.0788 ≤ ABSI<0.0819 | TyG ≥ 8.5742 0.0852 ≤ ABSI | P for interaction | |
|---|---|---|---|---|---|
| Gender | 0.021 | ||||
| Male | 319/3797 | Ref | 2.76(1.81–4.21) | 2.42(1.52–3.85) | |
| Female | 353/4459 | Ref | 1.27(0.79–2.04) | 2.40(1.60–3.60) | |
| Age | 0.004 | ||||
| ≥ 60 | 433/4324 | Ref | 2.76(1.73–4.42) | 2.32(1.48–3.62) | |
| < 60 | 239/3933 | Ref | 1.24(0.79–1.94) | 2.11(1.32–3.88) | |
| BMI | 0.763 | ||||
| ≥ 24 | 333/3281 | Ref | 1.42(0.88–2.28) | 1.99(1.25–3.16) | |
| < 24 | 339/4976 | Ref | 2.12(1.37–3.27) | 2.45(1.65–3.65) | |
| Education level | 0.457 | ||||
| Elementary school and below | 494/5808 | Ref | 1.83(1.25–2.68) | 2.27(1.59–3.23) | |
| Secondary school and above | 178/2449 | Ref | 2.10(1.22–3.62) | 2.68(1.50–4.79) | |
| Marital status | 0.758 | ||||
| Married | 575/7265 | Ref | 1.92(1.37–2.70) | 2.52(1.82–3.49) | |
| Others | 97/992 | Ref | 2(0.85–4.67) | 1.56(0.73–3.36) | |
| Smoke | 0.035 | ||||
| Yes | 283/3179 | Ref | 2.62(1.69–4.08) | 2.01(1.24–3.27) | |
| No | 389/6078 | Ref | 1.44(0.92–2.26) | 2.73(1.85–4.04) | |
| Drink | 0.453 | ||||
| Yes | 221/2668 | Ref | 2.69(1.60–4.53) | 2.27(1.31–3.93) | |
| No | 451/5589 | Ref | 1.59(1.07–2.36) | 2.41(1.68–3.46) | |
| Diabetes | 0.193 | ||||
| Yes | 54/376 | Ref | 1.87(0.40–8.81) | 2.12(0.47–9.47) | |
| No | 618/7881 | Ref | 1.89(1.37–1.97) | 2.38(1.75–3.23) | |
| Dyslipidemia | 0.700 | ||||
| Yes | 105/687 | Ref | 1.30(0.50–3.38) | 2.28(0.93–5.61) | |
| No | 567/7570 | Ref | 1.94(1.39–2.71) | 2.32(1.68–3.19) | |
| Heart problems | 0.641 | ||||
| Yes | 132/934 | Ref | 1.18(0.56–2.47) | 2.02(1.06–3.86) | |
| No | 540/7323 | Ref | 2.09(1.48–2.96) | 2.41(1.72–3.38) |
Discussion
Among 8726 Chinese adults aged 45 years old and above from CHARLS followed up to nine years, the incidence of first stroke in our sample population was 8.14%, which is in the normal range based on CHARLS database according to previous studies [14, 26, 31]. Both TyG index and ABSI index were independent factors in predicting stroke occurrence.
We found that higher levels of the TyG index at baseline were associated with an increased risk of future stroke, which was similar to the result of Anxin Wang’s research based on the other database named the Kailuan Study [17]. In 2023, Ying Yang conducted a meta-analysis of eight studies within 554,334 population and found that the general population with a higher TyG index had a 37.10% increased risk of ischemic stroke [32], which our study also revealed[HR:1.25, (95%CI: 1.06–1.47)]. TyG is a simple and reliable measurement tool for IR [12, 13], whose mechanism leading to stroke may based on the following possibilities: Firstly, endothelial dysfunction caused by IR leads to atherosclerosis [33–35]; Secondly, arterial stenosis would result from platelet adhesion, activation and aggregation effected by IR [36–39]; Thirdly, IR would increase sympathetic nervous system activity and impair cardiac autonomic function [40–42].
Recently, more and more studies had found that TyG could influence on cardiovascular events including stroke and the research directions tended to the change trend or cumulative effect of TyG [14, 43–44] and the prediction of joint indicators [18, 19, 20, 26, 42–43]. As for the prediction of joint indicators, most researchers combined TyG and obesity markers including BMI, WC and waist-to-height ratio(WHtR) [18–20, 26, 46] to get better diagnostic efficacy on cardiovascular diseases(CVDs). TyG combined with WHtR [19] or BMI [20] had higher diagnostic efficacy than TyG single index analysis, while Cancan Cui had came to inconsistent conclusions, which was TyG single index had the highest C-index of CVDs compared to TyG + BMI, TyG + WC and TyG + WHtR [18]. “Obesity paradox”, more observably in people with IR [26], was the possible reason for this discrepancy [5, 6] because these indicators could not provide a comprehensive picture of physical fitness. BMI was unable to distinguish between fat and lean mass, whose diagnostic ability of CVDs would also decreased with age and easily effected by the cardiovascular complications [47, 48]. WC and WHtR could represent fat to a certain extent but were unavailable to provide weight information and unable to distinguish visceral fat from subcutaneous fat [8, 9, 49]. These two types of fat had different impacts on the risks of CVDs and only visceral fat was significant [26, 30, 41–53].
ABSI, first proposed by Nir Y. Krakauer in 2012 [30], is a body shape indicator which is not affected by “obesity paradox”, providing more comprehensive information including visceral fat [9, 30]. Our study had found that high ABSI(ABSI ≥ 0.0852) was the independent predictor of stroke incidence(HR:1.33, 95%CI: 1.06–1.68), which was similar to Guang Li Wang’s[23] and Masato Kajikawa’s [21] findings. Some researchers also found that ABSI had higher predictive value on CVDs comparing to other obesity index including BMI, WC and WHtR [21, 54, 55]. After RCS regression analysis based on Model 3 in our study, it was found that ABSI index had linear association with stroke incidence(P for nonlinear: 0.3635), which filled the gap of previous research.
To the best of our knowledge, this is the first study to combine ABSI and TyG and we found that the combination of ABSI and TyG may better predict the incidence of stroke(AUC: 0.679, 95% CI: 0.533–0.597). The mechanisms of this joint analysis having better predictive performance as following: firstly, this joint index analysis provided more comprehensive information including IR and physical condition; secondly, joint index analysis was able to capture the differences of multiple indicators to predict stroke earlier; thirdly, everyone had differences in different biomarker levels and joint index analysis could be comprehensively analyzed according to the specific individuals. In model 3 of cox regression analysis, only one groups(TyG ≥ 8.5742, ABSI ≥ 0.0852) had the significant relationship with stroke, but the lower limit of the confidence interval in other groups was closely to 1, which might because of the sample size. The change of ABSI was more predictive in the group with high TyG value because ABSI was not effected by “obesity paradox” caused by IR [9, 26, 30]. The group with high TyG and ABSI, having higher probability of IR and visceral fat obesity [30, 38], had the most cumulative hazard ratio of stroke incidence. ABSI had better predictive performance than BMI [21, 54, 55] and our subgroup analysis also found that low-BMI population with high ABSI and TyG also were high risk group having stroke occurrence(HR:2.45, 95%CI:1.65–3.65). In subgroup analysis, the combination of ABSI and TyG was a still a predictor of stroke occurrence among those we consider to be low-risk populations(without drinking, diabetes, dyslipidemia or heart problems).
However, out study had several limitations to be considered. Firstly, we did not compare the predictive performance of ABSI with other obesity indicators including BMI, WC and WHtR. Secondly, we excluded individuals who have abnormal values of or lacking of exposurre factors, which might have some selection bias. Thirdly, the detailed development of joint indicators cannot be obtained without studying the dynamic changes of ABSI and TyG indicators. Fourthly, drug intervention was not considered because it was impossible to tracke specific drug usage situation and respondents’ compliance during 9-year follow-up. Fifthly, the target population of CHARLS was all from China and the extrapolation of results to other countries might have limitations. In addition, CHARLS is a database using questionnaire to collect information of health status, so the diagnosis of stroke is only based on participants’ self-reports lacking imaging examination, which might had some limitations.
Conclusion
Our study observed that both TyG and ABSI were valuable tools for predicting stroke occurrence, and the combined prediction of these two indicators had higher clinical value. The combined prediction of TyG and ABSI enabled earlier detection of the stroke in the general population, which could be monitored and intervened to reduce the overall burden of stroke.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to express our appreciation to all the members of the CHARLS for their contributions and all the participants who contributed the data.
Abbreviations
- CHARLS
China Health and Retirement Longitudinal Study
- CDC
Center for Disease Control and Prevention
- CVDs
Cardiovascular diseases
- WC
waist circumference
- IR
Insulin resistance
- BMI
Body mass index
- HbA1c
Glycated hemoglobin
- FBG
Fasting blood glucose
- TC
Total cholesterol
- HDL
High density lipoprotein cholesterol
- LDL
Low density lipoprotein cholesterol
- TG
Triglyceride
- TyG
Triglyceride glucose
- ABSI
A body shape index
- HR
Hazard ratio
- CI
Confidence interval
- RCS
Restricted cubic spline
- K-M
Kaplan-Meier curve
- ROC
Receiver operating characteristic
- AUC
Area under the curve
- WHtR
Waist-to-height ratio
Author contributions
R.Z. and J.H. wrote the main manuscript text and designed the study. R.Z., J.H. and Y. W. analyzed the data. L.L. and S.C. carried out literature search. Y.X. performed the manuscript review. All authors reviewed the manuscript.
Funding
None.
Data availability
Online repositories(https://charls.pku.edu.cn/) contain the datasets used in this investigation. Registration as a user on the website would be needed to obtain the data. After registration is reviewed and approved, the data set could be downloaded following the provided instructions.
Declarations
Ethics approval and consent to participate
The studies involving human participants were reviewed and approved by the Ethics Review Committee of Peking University. The patients/participants provided their written informed consent to participate in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ruiying Zhang and Jianan Hong contributed equally to this work
References
- 1.Li XY, Kong XM, Yang CH, et al. Global, regional, and national burden of ischemic stroke, 1990–2021: an analysis of data from the global burden of disease study 2021. EClinicalMedicine. 2024;75:102758. 10.1016/j.eclinm.2024.102758. Published 2024 Jul 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martin SS, Aday AW, Almarzooq ZI et al. 2024 Heart disease and stroke statistics: a report of US and Global Data From the American Heart Association [published correction appears in Circulation. 2024;149(19):e1164. 10.1161/CIR.0000000000001247]. Circulation. 2024;149(8):e347–e913. 10.1161/CIR.0000000000001209 IF: 35.5 Q1 B1 [DOI] [PubMed]
- 3.Wang X, Huang Y, Chen Y, et al. The relationship between body mass index and stroke: a systemic review and meta-analysis. J Neurol. 2022;269(12):6279–89. 10.1007/s00415-022-11318-1. [DOI] [PubMed] [Google Scholar]
- 4.Ohlsson C, Bygdell M, Sondén A, Jern C, Rosengren A, Kindblom JM. BMI increase through puberty and adolescence is associated with risk of adult stroke. Neurology. 2017;89(4):363–9. 10.1212/WNL.0000000000004158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Forlivesi S, Cappellari M, Bonetti B. Obesity paradox and stroke: a narrative review. Eat Weight Disord. 2021;26(2):417–23. 10.1007/s40519-020-00876-w. [DOI] [PubMed] [Google Scholar]
- 6.Liu X, Zhang D, Liu Y, et al. A J-shaped relation of BMI and stroke: systematic review and dose-response meta-analysis of 4.43 million participants. Nutr Metab Cardiovasc Dis. 2018;28(11):1092–9. 10.1016/j.numecd.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 7.Piché ME, Poirier P, Lemieux I, Després JP. Overview of epidemiology and contribution of obesity and body fat distribution to cardiovascular disease: an update. Prog Cardiovasc Dis. 2018;61(2):103–13. 10.1016/j.pcad.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 8.Pillay P, Lewington S, Taylor H, Lacey B, Carter J, Adiposity, body fat distribution, and risk of major stroke types among adults in the United Kingdom. JAMA Netw Open. 2022;5(12):e2246613. 10.1001/jamanetworkopen.2022.46613. [DOI] [PMC free article] [PubMed]
- 9.Nagayama D, Fujishiro K, Watanabe Y, et al. A body shape index (ABSI) as a variant of conicity index not affected by the obesity paradox: a cross-sectional study using arterial stiffness parameter. J Pers Med. 2022;12(12):2014. 10.3390/jpm12122014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hill MA, Yang Y, Zhang L, et al. Insulin resistance, cardiovascular stiffening and cardiovascular disease. Metabolism. 2021;119:154766. 10.1016/j.metabol.2021.154766. [DOI] [PubMed] [Google Scholar]
- 11.Zhou X, Kang C, Hu Y, Wang X. Study on insulin resistance and ischemic cerebrovascular disease: a bibliometric analysis via CiteSpace. Front Public Health. 2023;11:1021378. 10.3389/fpubh.2023.1021378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pan Y, Jing J, Chen W et al. Post-glucose load measures of insulin resistance and prognosis of nondiabetic patients with ischemic stroke. J Am Heart Assoc. 2017;6(1):e004990. 10.1161/JAHA.116.004990 [DOI] [PMC free article] [PubMed]
- 13.Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M, et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metab. 2010;95(7):3347–51. 10.1210/jc.2010-0288. [DOI] [PubMed] [Google Scholar]
- 14.Wu Y, Yang Y, Zhang J, Liu S, Zhuang W. The change of triglyceride-glucose index may predict incidence of stroke in the general population over 45 years old. Cardiovasc Diabetol. 2023;22(1):132. 10.1186/s12933-023-01870-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang Y, Liu T, Li Y et al. Triglyceride-glucose index, symptomatic intracranial artery stenosis and recurrence risk in minor stroke patients with hypertension. Cardiovasc Diabetol. 2023;22(1):90. 10.1186/s12933-023-01823-6 [DOI] [PMC free article] [PubMed]
- 16.Chen T, Qian Y, Deng X. Triglyceride glucose index is a significant predictor of severe disturbance of consciousness and all-cause mortality in critical cerebrovascular disease patients. Cardiovasc Diabetol. 2023;22(1):156. 10.1186/s12933-023-01893-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang A, Wang G, Liu Q, et al. Triglyceride-glucose index and the risk of stroke and its subtypes in the general population: an 11-year follow-up. Cardiovasc Diabetol. 2021;20(1):46. 10.1186/s12933-021-01238-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cui C, Qi Y, Song J, et al. Comparison of triglyceride glucose index and modified triglyceride glucose indices in prediction of cardiovascular diseases in middle aged and older Chinese adults. Cardiovasc Diabetol. 2024;23(1):185. 10.1186/s12933-024-02278-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ren Q, Huang Y, Liu Q, Chu T, Li G, Wu Z. Association between triglyceride glucose-waist height ratio index and cardiovascular disease in middle-aged and older Chinese individuals: a nationwide cohort study. Cardiovasc Diabetol. 2024;23(1):247. 10.1186/s12933-024-02336-6. Published 2024 Jul 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shao Y, Hu H, Li Q, Cao C, Liu D, Han Y. Link between triglyceride-glucose-body mass index and future stroke risk in middle-aged and elderly Chinese: a nationwide prospective cohort study. Cardiovasc Diabetol. 2024;23(1):81. 10.1186/s12933-024-02165-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kajikawa M, Maruhashi T, Kishimoto S, et al. A body shape index as a simple anthropometric marker of abdominal obesity and risk of Cardiovascular events. J Clin Endocrinol Metab. 2024;25. 10.1210/clinem/dgae282. [DOI] [PubMed]
- 22.Yang N, Zhuo J, Xie S, et al. A body shape index and its changes in relation to all-cause mortality among the Chinese Elderly: a retrospective cohort study. Nutrients. 2023;15(13):2943. 10.3390/nu15132943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang GL, Zhang R, Zhou YT, et al. Combined effects of a body shape index and serum C-reactive protein on ischemic stroke incidence among mongolians in China. Biomed Environ Sci. 2019;32(3):169–76. 10.3967/bes2019.024. [DOI] [PubMed] [Google Scholar]
- 24.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9. 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 25.Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. 2014;43(1):61–8. 10.1093/ije/dys203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huo RR, Liao Q, Zhai L, You XM, Zuo YL. Interacting and joint effects of triglyceride-glucose index (TyG) and body mass index on stroke risk and the mediating role of TyG in middle-aged and older Chinese adults: a nationwide prospective cohort study. Cardiovasc Diabetol. 2024;23(1):30. 10.1186/s12933-024-02122-4 [DOI] [PMC free article] [PubMed]
- 27.He Y, Gao M, Hu M, et al. The nonlinear relationship between triglyceride glucose-waist circumference and stroke risk in middle-aged and elderly people: a nationwide prospective cohort study of the CHARLS. Lipids Health Dis. 2024;23(1):264. 10.1186/s12944-024-02259-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tao LC, Xu JN, Wang TT, Hua F, Li JJ. Triglyceride-glucose index as a marker in cardiovascular diseases: landscape and limitations. Cardiovasc Diabetol. 2022;21(1):68. 10.1186/s12933-022-01511-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Flegal KM. Body-mass index and all-cause mortality. Lancet. 2017;389(10086):2284–5. 10.1016/S0140-6736(17)31437-X. [DOI] [PubMed] [Google Scholar]
- 30.Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE. 2012;7(7):e39504. 10.1371/journal.pone.0039504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Qu L, Fang S, Lan Z et al. Association between atherogenic index of plasma and new-onset stroke in individuals with different glucose metabolism status: insights from CHARLS. Cardiovasc Diabetol. 2024;23(1):215. 10.1186/s12933-024-02314-y [DOI] [PMC free article] [PubMed]
- 32.Yang Y, Huang X, Wang Y, et al. The impact of triglyceride-glucose index on ischemic stroke: a systematic review and meta-analysis. Cardiovasc Diabetol. 2023;22(1):2. 10.1186/s12933-022-01732-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee SB, Ahn CW, Lee BK et al. Association between triglyceride glucose index and arterial stiffness in Korean adults. Cardiovasc Diabetol. 2018;17(1):41. 10.1186/s12933-018-0692-1 [DOI] [PMC free article] [PubMed]
- 34.Wu S, Xu L, Wu M, Chen S, Wang Y, Tian Y. Association between triglyceride-glucose index and risk of arterial stiffness: a cohort study. Cardiovasc Diabetol. 2021;20(1):146. 10.1186/s12933-021-01342-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bornfeldt KE, Tabas I. Insulin resistance, hyperglycemia, and atherosclerosis. Cell Metab. 2011;14(5):575–85. 10.1016/j.cmet.2011.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Santilli F, Vazzana N, Liani R, Guagnano MT, Davì G. Platelet activation in obesity and metabolic syndrome. Obes Rev. 2012;13(1):27–42. 10.1111/j.1467-789X.2011.00930.x. [DOI] [PubMed] [Google Scholar]
- 37.Moore SF, Williams CM, Brown E, et al. Loss of the insulin receptor in murine megakaryocytes/platelets causes thrombocytosis and alterations in IGF signalling. Cardiovasc Res. 2015;107(1):9–19. 10.1093/cvr/cvv132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Du T, Yuan G, Zhang M, Zhou X, Sun X, Yu X. Clinical usefulness of lipid ratios, visceral adiposity indicators, and the triglycerides and glucose index as risk markers of insulin resistance. Cardiovasc Diabetol. 2014;13:146. 10.1186/s12933-014-0146-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ferreiro JL, Gómez-Hospital JA, Angiolillo DJ. Platelet abnormalities in diabetes mellitus. Diab Vasc Dis Res. 2010;7(4):251–9. 10.1177/1479164110383994. [DOI] [PubMed] [Google Scholar]
- 40.Shi W, Xing L, Jing L, et al. Value of triglyceride-glucose index for the estimation of ischemic stroke risk: insights from a general population. Nutr Metab Cardiovasc Dis. 2020;30(2):245–53. 10.1016/j.numecd.2019.09.015. [DOI] [PubMed] [Google Scholar]
- 41.Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord. 2008;6(4):299–304. 10.1089/met.2008.0034. [DOI] [PubMed] [Google Scholar]
- 42.Liu Y, Zhu B, Zhou W, et al. Triglyceride-glucose index as a marker of adverse cardiovascular prognosis in patients with coronary heart disease and hypertension. Cardiovasc Diabetol. 2023;22(1):133. 10.1186/s12933-023-01866-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yan Y, Wang D, Sun Y, et al. Triglyceride-glucose index trajectory and arterial stiffness: results from Hanzhong adolescent hypertension cohort study. Cardiovasc Diabetol. 2022;21(1):33. 10.1186/s12933-022-01453-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cheng L, Zhang F, Xue W, et al. Association of dynamic change of triglyceride-glucose index during hospital stay with all-cause mortality in critically ill patients: a retrospective cohort study from MIMIC IV2.0. Cardiovasc Diabetol. 2023;22(1):142. 10.1186/s12933-023-01874-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cui C, Liu L, Qi Y, et al. Joint association of TyG index and high sensitivity C-reactive protein with cardiovascular disease: a national cohort study. Cardiovasc Diabetol. 2024;23(1):156. 10.1186/s12933-024-02244-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li F, Wang Y, Shi B, et al. Association between the cumulative average triglyceride glucose-body mass index and cardiovascular disease incidence among the middle-aged and older population: a prospective nationwide cohort study in China. Cardiovasc Diabetol. 2024;23(1):16. 10.1186/s12933-023-02114-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Xu J, Wang A, Meng X, Jing J, Wang Y, Wang Y. Obesity-stroke paradox exists in insulin-resistant patients but not insulin sensitive patients. Stroke. 2019;50(6):1423–9. 10.1161/STROKEAHA.118.023817. [DOI] [PubMed] [Google Scholar]
- 48.Romero-Corral A, Somers VK, Sierra-Johnson J, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond). 2008;32(6):959–66. 10.1038/ijo.2008.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Iliodromiti S, Celis-Morales CA, Lyall DM, et al. The impact of confounding on the associations of different adiposity measures with the incidence of cardiovascular disease: a cohort study of 296 535 adults of white European descent. Eur Heart J. 2018;39(17):1514–20. 10.1093/eurheartj/ehy057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Oesch L, Tatlisumak T, Arnold M, Sarikaya H. Obesity paradox in stroke—myth or reality? A systematic review. PLoS ONE. 2017;12(3):e0171334. 10.1371/journal.pone.0171334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Neeland IJ, Poirier P, Després JP. Cardiovascular and metabolic heterogeneity of obesity: clinical challenges and implications for management. Circulation. 2018;137(13):1391–406. 10.1161/CIRCULATIONAHA.117.029617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bigaard J, Frederiksen K, Tjønneland A, et al. Body fat and fat-free mass and all-cause mortality. Obes Res. 2004;12(7):1042–9. 10.1038/oby.2004.131. [DOI] [PubMed] [Google Scholar]
- 53.Heitmann BL, Frederiksen P. Thigh circumference and risk of heart disease and premature death: prospective cohort study. BMJ. 2009;339:b3292. 10.1136/bmj.b3292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dhana K, Ikram MA, Hofman A, Franco OH, Kavousi M. Anthropometric measures in cardiovascular disease prediction: comparison of laboratory-based versus non-laboratory-based model. Heart. 2015;101(5):377–83. 10.1136/heartjnl-2014-306704. [DOI] [PubMed] [Google Scholar]
- 55.Abete I, Arriola L, Etxezarreta N, et al. Association between different obesity measures and the risk of stroke in the EPIC Spanish cohort. Eur J Nutr. 2015;54(3):365–75. 10.1007/s00394-014-0716-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Online repositories(https://charls.pku.edu.cn/) contain the datasets used in this investigation. Registration as a user on the website would be needed to obtain the data. After registration is reviewed and approved, the data set could be downloaded following the provided instructions.