Abstract
Background
Voice barriers among frontline healthcare workers hinder safety related to work and patients. Understanding these barriers and practices is crucial to improve voice behavior in healthcare settings. Therefore, this study aims to identify the voice barriers and practices among healthcare workers in Pakistan.
Research method
The study has adopted a mixed-method research design. Data was collected from 15 frontline healthcare workers through semi-structured interviews to achieve study objectives. Descriptives and content analysis were conducted to explore voice barriers and alternative practices to solve their concerns. After that, a quantitative study was conducted to determine the statistical significance of the identified voice barriers and the magnitude of their effect. For this purpose, data was collected from 480 frontline healthcare workers in the primary, secondary, and territory healthcare units. A questionnaire survey was used for data collection. Then, multistage hierarchical regression analysis was employed for data analysis.
Results
Study findings highlight the determinants of two key factors: withholding patient safety concerns and withholding worker safety concerns. First, the study identifies several factors that increase the likelihood of healthcare workers withholding concerns about patient safety. These factors include professional designation, work experience, blackmailing, overconfidence, longer work tenure, feelings of insult, early career stage, fear of patient reactions, bad past experiences, job insecurity, and uncooperative management. Fear of increased workload also plays a significant role. Second, when it comes to work-related safety concerns, factors such as gender, shyness, lack of confidence, fear of duty changes, management issues, interpersonal conflicts, and resource shortages contribute to the withholding of concerns. To navigate these challenges, healthcare workers often resort to strategies such as seeking political connections, personal settlements, transfers, union protests, quitting, using social media, engaging in private practice, or referring patients to other hospitals.
Conclusion
Findings demonstrates that healthcare workers in Pakistan often withhold safety concerns due to hierarchical pressures, personal insecurities, and fear of repercussions. Their reliance on external mechanisms, such as political influence or social media, underscores the need for significant reforms to improve safety culture and management support. Addressing these issues is crucial for ensuring both patient and worker safety.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-024-11782-7.
Keywords: Voice barriers, Prohibitive voice, Patient safety, Worker safety, Healthcare workers
Contribution to the literature review
This study provides an in-depth qualitative examination of the voice barriers encountered by healthcare workers, including doctors, nurses, and midwives, in Pakistani public hospitals
It explores the practices adopted by healthcare workers when facing these voice barriers, offering insights into their coping mechanisms and the impact on their professional behavior.
Using hierarchical regression analysis, the study quantitatively assesses the magnitude of the effect of each voice barrier on prohibitive voice related to patient safety and healthcare worker safety. It contributes valuable figures to the understanding of communication challenges in healthcare settings.
Introduction
Healthcare sector is the most fragile, with no room for errors. Upon fulfilling all the safety standards in healthcare system, finally the diagnosis, procedures and treatments depends on health practitioners. One small error can jeopardise a patient’s life. There are several psychosocial factors and consequent outcomes which can adversely affect employee’s ability to proceed with successful work operations. Such as job demand control imbalance, effort reward imbalance, interpersonal conflicts [1], bullying etc., and their consequences as stress, mental health issues, burnout, and voice suppressions etc. Basically, voice plays a moderating role in the relationship between psychosocial factors and employee outcomes. If voice raised, it reduces the negative effect of psychosocial factors on employee outcome. If voice supressed, it increases the negative effect of psychosocial factors on employee outcome and increase the chances of error in healthcare practices. Prohibitive voice describes “employees ‘expressions of concern about work practices, incidents, or employee behavior that are harmful to their organization” [2]. Prohibitive voice plays an important role for organizational health, mainly since such frightening communications place beforehand unobserved glitches on the shared agenda to be determined or avoid tricky initiatives. Similarly, withholding voice related to patient safety is defined as “an intentional behaviour not to verbalise ideas, information and opinions for the improvement of patient safety and is thus more than the absence of speaking up” [3]. While, voice barriers are the obstacles to raise voice for safety concerns. When employees cannot directly raise their safety concerns, they resort to indirect methods to address their issues to some extent. These indirect methods, termed as consequent voice practices, can be harmful to the organization.
Medication and medical errors cause adverse events and serious threat to the lives of the patients. Every year 134 million adverse events occur in lower- and middle-income countries, which results in 2.6 million deaths. However, medical errors are avoided to disclose, report and record in the hospitals [4, 5]. Whereas, medication errors cannot be hide due to prescription and manual records. Statistics shows that annually 500,000 people die in Pakistan due to medication errors [6, 7]. Medication errors accounts for 18.3% of adverse events occur in Pakistani hospitals [8]. There are several reasons, which leads to medical and medication errors. Such as organizational fear, workload, pay problems, concentration issues (among nurses, USA) [9], inadequacy of physical examination [10], burnout [11–13]. Consequently, all these factors along with realization of medical errors leads to adverse mental health [14, 15] and suicidal behaviour among healthcare workers [16–18]. Therefore, medical errors endanger both the health and safety of patients and healthcare workers. However, health and safety of both the stakeholders can improve through healthcare worker’s voice behaviour [19, 20]. Speaking up behaviour can prevent harms [21], and can increase patient safety culture [22]. Nonetheless, there are several voice barriers in the healthcare sector.
So far, several studies were conducted to investigate workers voice barriers, worldwide. In this regard, Morrow, et al. [23] conducted meta-analysis of 11 qualitative articles published during 2005 to 2015. It was identified that safety voice among healthcare workers is (1) perceived as unsafe and ineffective, (2) delayed because of power dynamic and hierarchies, and (3) can be increased by open communication and manager’s support. Further it was identified that all the studies were conducted in context of Australia, Bulgaria, Canada, Hong Kong, East Africa, Ireland, Korea, New Zealand, Sweden, Switzerland, and the United States.
Fisher and Kiernan [24] examined the factors which effect nurses’ voice behaviour for patient safety through qualitative study in context of the UK. They found that nurses do not speak for patient safety because of fear of punitive action, context of exposure, hierarchy, and team culture.
Lee and Dahinten [25] investigated voice behaviour of nurses in South Korea and found that inclusive leadership and psychological safety reduce withholding voice and increase the behaviour of speaking up and intention to report error. Similarly, another study was conducted in the Netherlands found psychological safety can increase speaking up behaviour [26]. Mihdawi, et al. [27] identified that patient safety can be enhance through nursing working environment. In context of Pakistan, Nawaz, et al. [28] concluded that idiosyncratic deals can improve healthcare workers voice behaviour.
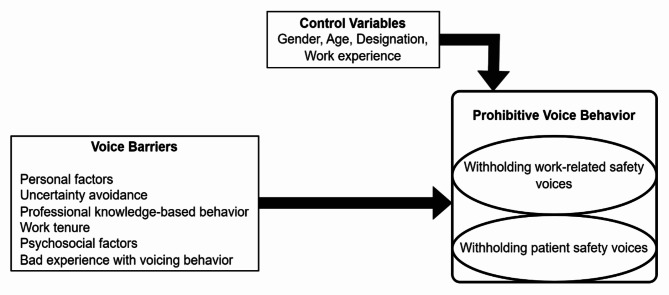
Thus, previous literature review on voice behaviour suggests six research gaps. First, previous studies largely focused on nurse’s voice behaviour. Whereas the behaviour of doctors and midwives was overlooked. Second, voice behaviour related to patient safety is densely investigated, whereas, voice behaviour related to workers safety was ignored. Though workers safety leads to patient safety [27]. Third, almost all the studies were conducted in the developed countries and developing countries such as Pakistan were ignored greatly. Fifth, previous study found voice barriers through qualitative method but the identified barriers were not empirically validated. Sixth, previous studies ignored to identify the alternative practices in presence of voice barriers. Thus, we propose to address these gaps by uncovering voice barrier among healthcare workers in developing country, Pakistan, by identifying voice barriers to both patient safety and workers safety, by extending study sample to other healthcare workers as doctors and midwives, by validating identified voice barriers through empirical analysis as the research model proposed (as depicted in Fig. 1), and by identifying healthcare worker’s alternative voice practices in presence of voice barriers. We raised three main questions based on the above discussion.
What are the prohibitive voice barriers (patient safety and worker safety), among frontline healthcare workers (doctors, nurses, and midwives) in Pakistan?
What are the consequent practices frontline healthcare workers follow within the presence of voice barriers?
What is the magnitude of the effect of voice barriers on withholding voice (patient safety and worker safety)?
Fig. 1.
Conceptual model
Conservation of resources theory (COR) [29] severs as basis to support this study. Which indicates employee’s behaviour of resource conservation by shaping voice behaviours. Such as healthcare workers withhold voices to avoid resource depletion. The study has several practical and theoretical implications. The study finding compels strategists to make policies to improve working conditions leading to worker and patient safety in the hospitals. It helps healthcare management to develop a safe working culture, which motivate workers to bring their concerns to management. Further, this study supports management to remove voice barriers in the hospitals with larger magnitude of effect on withholding voice. The study also adds in literature related to healthcare safety.
Methodology
Following the research questions of the study, Mixed-method research design was adopted to conduct it. As the study aims to identify voice barriers among healthcare workers in Pakistan and then validate them through empirical analysis. Therefore, initially, semi structured interviews were conducted with the healthcare workers. The study sample encompassed participants employed in public hospitals at primary, secondary, and tertiary levels in the Lahore district, Pakistan. Interviewees were selected using the convenience sampling technique. No explicit criteria were applied for interviewee selection, as all medical and paramedical staff working in public hospitals met the necessary job requirements. Consequently, in line with the study objectives, participants were comprised in this study without age and experience limits. All methods were conducted in accordance with the Helsinki guidelines. Informed written consent was taken before interview session. Interviewees were ensured about confidentiality of the data and its removal after utilization for research purpose. Each interview lasted about 35 min. Data collection continued until saturation was achieved, which occurred after 15 interviews were completed. To ensure data saturation, an additional 3 interviews were conducted, confirming that saturation has achieved. However, data collection on 15th interview was completed due to reiteration of the responses.
Interviews were conducted in Urdu language. All the interview sessions were digitally recorded, transcribed, contents were derived and translated into English language for reporting and analysis purpose.
Based on the identified contents a questionnaire was developed and distributed for data collection among 700 healthcare frontline workers. A total of 511 filled in questionnaires were returned. Thirty-one questionnaires were discarded due to improper filled in responses and rest 480 were used for data analysis. Data was tested for common method bias. According to [30] common method bias can occur if data of dependent and independent variable is collected from the same respondent. To ensure data is free from common method bias, Herman’s single factor analysis was conducted [31]. Then diagnostic tests as multicollinearity, normality, and reliability were employed before main statistical analysis. Finally, we proceeded for Hierarchical Multilevel Regression analysis to analyse data using statistical software SPSS [32–34].
Measures
Withholding prohibitive voice behaviour for worker was measured with five items, on 5-point Likert scale adapted from the study Liang, et al. [2] ranging from “1” strongly disagree to “5” strongly agree. Whereas withholding voice behaviour related to patient safety was adapted from the study of Schwappach and Richard [35] and measured with four items, on 5-point Likert scale ranging from “1” rarely to “5” very often.
Voice barriers identified through interview were measured on categorical scale coded with 1 “Yes” and 0 “No” (See appendices: Questionnaire). The study controlled the effect of four variables such as gender, age, designation and work experience. Else, they can influence main results of the study.
Results
Results qualitative study
Demographic details
Demographic results show percentage of interviewees based on gender, age, designation, and work experience. 8 males and 7 females participated in this study. Based on age 46.7% of participants were from age group 31 to 40 followed by 33.3% were from age group 22 to 30, and 20% of the participants were related to age group 41 to 50 years old. Designation wise, doctors, nurses, dispensers, and midwives participated in the study with the percentage of 26.7, 33.3, 20, and 20 respectively. Based on work experience 20% of the participants were less than one year of work experience, 33.3% of the participants experienced ranged from 1 to 5 years, experience of 26.7% and 20% of the participants was ranged from 5 to 10 years, and greater than ten years, respectively.
Prohibitive voice barriers and consequent practices
Voice barriers
-
i.
Personal traits
First, voice barriers were distinguished based on individual and contextual characteristics as personal or internal factors, such as self-efficacy, which is the basic concept introduced by Bandura and Cervone [36]. Which determines the degree of resistance and amount of pressure to change. Self-efficacy is defined in terms of hard work, deliberate effort, choosing tough projects, progress towards mastery of work, goal achievement, and perseverance in the face of challenges. As a result, particularly in high-risk situations, a high level of self-efficacy reinforces the notion that an individual can influence events to get the desired results. According to Amos and Klimoski [37] self-confidence is a personality trait, therefore, it affects voice behaviour [38, 39]. Similarly, shyness is one of the personality components [40], individuals those shy avoids speaking behaviour. Related to personality traits, this study evidenced, shyness, lack of confidence, and feeling insult are the potential voice barriers.
-
ii.
Uncertainty avoidance
According to Ebrahimi, et al. [41] workers reluctant to speak due to fear of job loss, demotion, and job pressure. Similarly, this study demonstrated healthcare workers have several fears if they speak, they would be transferred to health facilities at longer distance. Which can loss them in terms of money, time and effort. Another type is the fear of rotation change, in which duty could be changed in different unsuited rotation as from morning to night shift. Fear of inquiries, in which workers get involved into unnecessary inquiries, which costs them mental stress and wastage of time. Another fear is related to pay stop, through which workers being pushed into departmental processes to resume their salaries. Fear of job lost also restrict individuals to raise their voices. In short, to avoid all these problems, workers withhold their voices and adjust themselves according to working environment.
Align with previous research findings, we have found pressure of external and internal stakeholders as an important factor of voice behaviour qualitative and quantitative data analysis. In this study, external stakeholders were described as patient and their attendants, and internal stakeholder were peers and hospital management personnel. We have identified that frontline healthcare workers do not raise their voices of patient to avoid negative reactions of internal and external stakeholders. healthcare workers familiar with stakeholders’ negative reactions by their past experiences and ongoing incidents occurring with other colleagues or at other health facilities. Negative reactions by external stakeholders includes protests by patients and attendants with the perceptions of faulty medical treatment, against frontline healthcare workers. Which creates further problems for the healthcare worker in terms of investigations and reputation. Therefore, withholding voice perceived as safe behaviour. Secondly, internal stakeholders as hospital management and peers consider worker’s raised voice regarding patient safety, as a weakness or voice raiser’s fault towards patient, therefore, they put all the blame on the voice raiser and blackmail them in future. To avoid this fear healthcare workers less likely, raise voice related to patient safety, particularly.
-
iii.
Psychosocial factors
Relationship between psychosocial factors and voice behaviour is evidenced in previous research. According to Detert and Edmondson [42] and Subhakaran and Dyaram [43] explained that psychosocial voice barriers effect the employees’ inclination to speak up [43] and consequently team’s performance [44].
Interpersonal conflicts, lack of support by management, bullying, perceived injustice, and conflicts based on job cadre (power distance), are the psychosocial factors identified among healthcare workers as the voice barriers in context of Pakistan.
-
iv.
Previous voice experience
Previous experience related to voice raising and its outcomes plays important role to determine voice behaviour. Employees are reluctant to raise voices if less likely regarded with their voices in the past or they got worse consequences due to their voice behaviour and vice versa. Several studies evidenced the role of experience in changing behaviour [45]. Other studies identified that the experience of psychological contract breach (not fulfilling promise by management / boss) effect voice behaviour [46]. Similar concept is supported by social cognitive theory of self-regulation by Bandura [47]. Albarracín and Wyer [48] provided empirical evidence of the positive relationship between past behaviour and future behaviour. In the same way, this study identified that employees past voice behaviours and its effects, shape individuals’ voice behaviours. In this study, we found that majority of the respondents demonstrated that they do not raise their voice because they are cannot bear its consequences, as in the past they did.
-
xxii.
Professional knowledge rivalries
Professional knowledge rivalry is another factor of voice behaviour among healthcare individuals identified in this study. Individuals with higher self-efficacy in their field, less likely raise their voices to seek help. Similarly, healthcare workers, those have professional knowledge conflicts with others do not speak out to get guidance on the issues related to patient safety. Differ of opinion halt them to consult with each other in patient safety matters.
Knowledge based conflicts occurs when individuals being disregarded based on their knowledge and practices. Conflicts can occur for a wide variety of reasons, from incompatible behaviour (Deutsch 1973) to a misunderstanding of one another’s interests (Rubin et al. 1994). Another study identified conflicts negatively effects operational functioning, reduce satisfaction and effect future decisions through endangering cohesiveness of a team (Schweiger et al. 1986). Similarly, this study identified conflicts related to professional knowledge affect individuals’ decision to ask for help and guidance. This finding is specifically evident in context of voice raising regarding patient safety.
-
vi.
Work tenure
Work tenure is also identified as a potential determinant of voice behaviour. Previously many studies highlighted the importance of work tenure or job tenure as a significant factor of voice behaviour such as Ngo, et al. [49] identified it among Hong Kong workers for voice behaviour of discrimination at work. Similarly, Zhang, et al. [50] found work tenure as a covariate factor to shape voice behaviour among teachers. Whereas several other researchers considered work tenure as a potential control variable, while assessing the effect of other independent factors on voice behaviour [51–53]. Likewise, we have identified work tenure as a critical factor in shaping voice behaviour among frontline healthcare workers in Pakistan, into two domains as work safety and patient safety. We have further validated the point (greater or lesser) of work tenure effects voice behaviour through quantitative study.
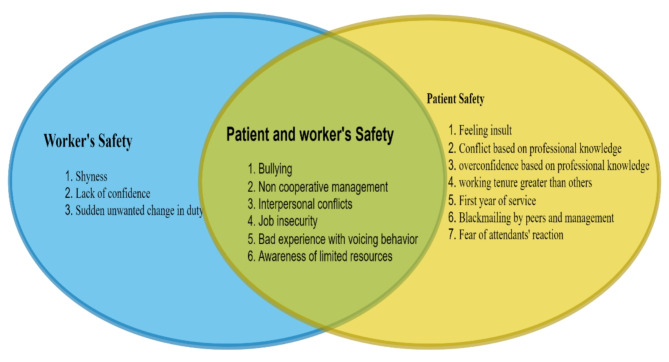
Figure 2 elaborate and distinguishes the voice barriers related to patient safety and worker’s safety among healthcare workers in Pakistan. Voice barriers with the domains and factors, and consequent practices is presented below (Table 1).
Fig. 2.
Distinguished voice barriers to patient and worker safety
Table 1.
Classification of voice barriers and consequent practices
| Domains | Factors | Consequences of withholding prohibitive voice behavior | ||
|---|---|---|---|---|
| Patient safety | Safety at work | |||
| Voice barriers | Personal | Lack of confidence |
1. Motivate patient to move to a private healthcare facility 2. Part time practices on private clinics 3. Union protests |
1. Political approaches 2. Change workstations 3. Burnout 4. Quit 5. Adjust accordingly 6. Union protests 7. Social media sharing from fake ids 8. Individually matter settlement |
| Shyness | ||||
| Feeling insult | ||||
| Uncertainty | Fear of job lost | |||
| Fear of inquiries | ||||
| Fear of change in duties | ||||
| Fear of patient and attendants’ reaction | ||||
| Fear of blackmailing by management and peers | ||||
| Professional knowledge | Professional knowledge-based conflict | |||
| Over confidence based on professional knowledge | ||||
| Psychosocial factors | Interpersonal conflicts | |||
| Bullying | ||||
| Unsupportive management | ||||
| Perceived injustice | ||||
| Conflict based on cadre (power distance) | ||||
| Work tenure | Greater than others | |||
| First year of service | ||||
| Voice experience | Bad experience with voicing behavior | |||
Consequent practices
However, voice barriers at workplace impel workers to adopt over the counter approaches to fix their workplace problems. Such as political references, relocations, and social media sharing. To resolve work related problems, workers put political pressure on hospital management through political pubic representative figures. Some workers effort to change their workstations, whereas, most of the young workers highlight problematic issues on social media to get public support. Most of the workers resolve their problems individually and secretly, which is the biggest hinderance in forming safety culture at the workplace. However, if same problem experienced frequently by all the workers within the same cadre than it is tackled through union protests. Such as undervalue someone’s role and workload issues. However, some of the workers with well-off background prefer to quit their jobs.
Whereas, to solve the matters related to patient safety, healthcare workers refer patients to other hospitals, beware them about lack of medical equipment and facilities in the hospital, suggest them private hospitals. In this way, they ruin reputation of public hospitals and promote private practices.
Results quantitative study
Sample characteristics
Demographics statistics presented in Table 2, demonstrates dominant participation of female respondents in this study with 55%. Based on age, 35% of the respondents were of age 31 to 40 followed by 32.5% from age group 22 to 30, 22.5% from age group 41 to 50, and 10% respondents were greater than 50 years in age. Designation wise respondents categorized into four categories, among them participation rate of disperser was 40%, followed by doctor’s participation rate 30%, nurses 22.5%, and midwife’s participation rate was 7.5%. Most of the respondents (38.2) were with 5 to 10 years work experience followed by 35.4% with more than 10 years, 19.6% with 1 to 5 years, and 6.8% were with less than 1 year of work experience.
Table 2.
Sample characteristics
| Gender | Frequency (%) | Age (Years) | Frequency (%) | Designation | Frequency (%) | Work experience (year) | Frequency (%) |
|---|---|---|---|---|---|---|---|
| Male | 45.0 | 22–30 | 32.5 | Doctor | 30.0 | < 1 | 6.8 |
| Female | 55.0 | 31–40 | 35.0 | Nurse | 22.5 | 1–5 | 19.6 |
| - | - | 41–50 | 22.5 | Dispenser | 40.0 | 5–10 | 38.2 |
| - | - | > 50 | 10.0 | Midwife | 7.5 | > 10 | 35.4 |
Diagnostic tests
Before proceeding for hierarchical multilevel regression analysis, first, the independent variables were tested for multicollinearity through correlation analysis. Table 3 presents the results of correlation analysis, which shows that none of the independent variables is highly correlated (Correlation coefficient > 0.50) [54], hence, the problem of multicollinearity not detected. Second, normality of the data was ensured through skewness (within ± 1) and kurtosis (within ± 3) values [55, 56]. Third, internal consistency of the constructs verified through the value of Cronbach’s alpha not less than 0.70 for each construct [57]. Fourth, data is tested for common method bias through Harman’s single factor analysis and principal component analysis [30, 58]. The first factor accounted for 30% variance, which indicates data is free from common method bias.
Table 3.
Descriptives and correlation analysis
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | 1.000 | ||||||||||||||||||||
| Age | − 0.062 | 1.000 | |||||||||||||||||||
| Designation | 0.026 | − 0.027 | 1.000 | ||||||||||||||||||
| Work Exp. | − 0.002 | 0.002 | 0.002 | 1.000 | |||||||||||||||||
| BPS1(Feeling Insult) | 0.201* | 0.258* | 0.000 | − 0.055 | 1.000 | ||||||||||||||||
| BPS2(Knowledge based Conflict) | − 0.212* | 0.301* | 0.078* | 0.029 | 0.101* | 1.000 | |||||||||||||||
| BPS3(Knowledge based overconfidence) | − 0.212* | 0.041 | 0.078* | 0.053 | − 0.201* | 0.293* | 1.000 | ||||||||||||||
| BPS4(Work tenure greater than others) | 0.000 | 0.155* | − 0.310* | − 0.032 | 0.200* | 0.101* | 0.000 | 1.000 | |||||||||||||
| BPS5(1st year of service) | 0.341* | − 0.068 | 0.013 | − 0.004 | − 0.051 | − 0.168* | 0.036 | − 0.152* | 1.000 | ||||||||||||
| BPS6(Blackmailing) | 0.257* | 0.057 | − 0.194* | 0.001 | 0.150* | 0.357* | 0.156* | 0.150* | 0.413* | 1.000 | |||||||||||
| BPS7(Fear of reaction by patient and attendants) | 0.055 | − 0.253* | − 0.246* | 0.049 | − 0.150* | − 0.247* | 0.156* | 0.050 | 0.210* | 0.298* | 1.000 | ||||||||||
| BWS1 (Shyness) | 0.448* | − 0.057 | − 0.116* | − 0.017 | 0.050 | − 0.055 | − 0.257* | 0.250* | 0.195* | 0.103* | 0.203* | 1.000 | |||||||||
| BWS2 (Lack of Confidence) | 0.179* | − 0.195* | − 0.135* | − 0.049 | 0.000 | − 0.032 | 0.074 | − 0.105* | 0.535* | 0.278* | 0.173* | − 0.068 | 1.000 | ||||||||
| BWS (Fear of duty change) | 0.285* | 0.293* | − 0.113* | − 0.071 | 0.000 | 0.175* | − 0.044 | − 0.109* | 0.099* | 0.186* | − 0.142* | 0.142* | 0.320* | 1.000 | |||||||
| BBS1(Bullying) | − 0.263* | 0.011 | − 0.113* | − 0.105* | − 0.109* | − 0.263* | − 0.044 | − 0.327* | − 0.121* | − 0.251* | 0.076 | − 0.186* | − 0.023 | 0.048 | 1.000 | ||||||
| BBS2(Non cop. management) | 0.373* | − 0.068 | − 0.169* | 0.096* | 0.000 | 0.044 | 0.154* | 0.218* | 0.121* | 0.142* | 0.033 | 0.295* | 0.137* | 0.071 | − 0.524* | 1.000 | |||||
| BBS3(Interpersonal Conflict) | 0.075 | 0.077* | 0.194* | − 0.002 | 0.000 | 0.201* | − 0.050 | 0.000 | − 0.329* | 0.025 | − 0.350* | 0.100* | − 0.157* | 0.055 | − 0.082* | − 0.191* | 1.000 | ||||
| BBS4(Job Insecurity) | 0.371* | − 0.037 | − 0.222* | − 0.012 | 0.253* | 0.066 | − 0.239* | 0.152* | 0.125* | 0.195* | − 0.109* | 0.008 | 0.207* | 0.011 | − 0.320* | 0.320* | − 0.051 | 1.000 | |||
| BBS5(Workload Increase) | 0.055 | 0.057 | − 0.142* | − 0.101* | 0.150* | 0.055 | − 0.146* | 0.250* | − 0.195* | − 0.103* | − 0.003 | 0.203* | − 0.247* | − 0.033 | 0.076 | − 0.076 | − 0.100* | 0.195* | 1.000 | ||
| BBS6(Bad Voice Exp) | 0.406* | 0.119* | − 0.030* | − 0.105* | 0.346* | − 0.174* | 0.058 | 0.000 | 0.263* | 0.145* | 0.029 | 0.202* | 0.061 | 0.126* | 0.126* | 0.126* | 0.000 | − 0.029 | 0.145* | 1.000 | |
| BBS7(Shortage of Resources) | 0.091* | − 0.166* | 0.285* | 0.021 | − 0.302* | − 0.010 | 0.091* | − 0.302* | 0.239* | − 0.045 | 0.156* | 0.146* | 0.179* | 0.285* | − 0.154* | − 0.066 | − 0.050 | − 0.442* | − 0.146* | − 0.174* | 1.000 |
| Mean | 0.55 | 2.10 | 2.25 | 3.02 | 0.50 | 0.55 | 0.55 | 0.50 | 0.58 | 0.48 | 0.48 | 0.53 | 0.65 | 0.70 | 0.70 | 0.30 | 0.20 | 0.43 | 0.48 | 0.25 | 0.55 |
| SD | 0.50 | 0.97 | 0.97 | 0.91 | 0.50 | 0.50 | 0.50 | 0.50 | 0.50 | 0.50 | 0.50 | 0.50 | 0.48 | 0.46 | 0.46 | 0.46 | 0.40 | 0.50 | 0.50 | 0.43 | 0.50 |
* indicates a 1% significance level
Hierarchical multilevel regression analysis
Hierarchical multilevel regression analysis was conducted to determine the direct effect of voice barriers to prohibitive voice behaviour related to patient safety and safety at work. Table 4 presents the direct effect of voice barriers on withholding prohibitive voice behaviour related to patients’ (WPVPS) safety. Stepwise hierarchical regression analysis consists on different steps. The first step includes control variable. Second step includes independent variable. Regression was run with stepwise method, which produce results based on magnitude of effect and significance of the model. Following the standard practice, we selected model 13 for this study.
Table 4.
Voice barriers effecting withholding patient safety voice
| Variables | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | Model 9 | Model 10 | Model 11 | Model 12 | Model13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Constant) | 3.884*** | 2.357*** | 1.972*** | 1.276*** | 1.234*** | 1.176*** | 1.227*** | 1.076*** | 0.720*** | 0.727*** | 0.526*** | 0.521*** | 0.443*** |
| Gender | 0.866*** | 0.020 | 0.347*** | 0.352*** | 0.280*** | 0.304*** | 0.466*** | 0.369*** | 0.380*** | 0.278*** | 0.140** | 0.042 | 0.018 |
| Age | 0.139 | 0.028 | 0.020 | − 0.053 | − 0.119*** | − 0.097*** | − 0.158*** | − 0.177*** | − 0.145*** | − 0.165*** | − 0.144*** | − 0.133*** | − 0.130*** |
| Designation | − 0.308*** | 0.017 | − 0.064 | 0.086** | 0.060 | 0.112*** | 0.075** | 0.040 | 0.055* | 0.071** | 0.114*** | 0.125*** | 0.127*** |
| Work Exp. | 0.055 | 0.051 | 0.018 | 0.035 | 0.047 | 0.047 | 0.039 | 0.042 | 0.031 | 0.048* | 0.051** | 0.040 | 0.043* |
| Blackmailing | 3.169*** | 2.874*** | 2.787*** | 2.720*** | 2.749*** | 2.533*** | 2.294*** | 2.051*** | 2.063*** | 2.053*** | 2.059*** | 2.090*** | |
| Knowledge based Overconfidence | 1.170*** | 1.167*** | 1.276*** | 1.238*** | 1.145*** | 1.139*** | 1.063*** | 0.969*** | 0.997*** | 0.943*** | 0.957*** | ||
| Work tenure greater than others | 1.002*** | 0.912*** | 0.939*** | 0.921*** | 0.986*** | 0.980*** | 1.002*** | 0.985*** | 0.943*** | 0.907*** | |||
| Feeling insult | 0.523*** | 0.490*** | 0.450*** | 0.512*** | 0.572*** | 0.449*** | 0.379*** | 0.410*** | 0.426*** | ||||
| Interpersonal Conflicts | − 0.540*** | − 0.662*** | − 0.466*** | − 0.283*** | − 0.328*** | − 0.288*** | − 0.213*** | − 0.167** | |||||
| Knowledge based conflict | 0.544*** | 0.660*** | 0.847*** | 0.925*** | 0.879*** | 0.856*** | 0.816*** | ||||||
| 1st year of service | 0.462*** | 0.549*** | 0.485*** | 0.456*** | 0.477*** | 0.514*** | |||||||
| Fear of reaction by patient and attend. | 0.472*** | 0.475*** | 0.540*** | 0.571*** | 0.559*** | ||||||||
| Bad voice Exp. | 0.399*** | 0.497*** | 0.484*** | 0.433*** | |||||||||
| Job insecurity | 0.326*** | 0.287*** | 0.252*** | ||||||||||
| Non-cop. management | 0.235*** | 0.282*** | |||||||||||
| Fear of workload increase | 0.140*** | ||||||||||||
| R2 | 0.288 | 0.858 | 0.908 | 0.943 | 0.951 | 0.958 | 0.965 | 0.969 | 0.974 | 0.977 | 0.979 | 0.980 | 0.981 |
| ∆R2 | 0.070 | 0.731 | 0.821 | 0.886 | 0.902 | 0.915 | 0.929 | 0.937 | 0.947 | 0.952 | 0.957 | 0.959 | 0.960 |
| F |
(4-275) 6.229 |
(5-274) 152.899 |
(6-273) 213.627 |
(7-272) 310.369 |
(8-271) 322.740 |
(9-270) 335.083 |
(10–269) 363.975 |
(11–268) 377.223 |
(12–267) 412.586 |
(13–266) 427.989 |
(14–265) 444.975 |
(15–264) 437.074 |
(16–263) 419.402 |
| Durbin-Watson | 1.524 | ||||||||||||
* indicates a 10% significance level, ** indicates a 5% significance level, *** indicates a 1% significance level
The direct effect of control variables on withholding prohibitive voice behaviour related to patient safety revealed the positive effect of gender (β = 0.866, p < 0.01) and negative effect of designation (β= − 0.308, p < 0.01) towards withholding prohibitive voice behaviour related to patient safety. However, the result of age and work experience did not demonstrated significance at this stage. Then, hierarchical regression analysis automatically selected the factor of blackmailing among all other independent variables for model 2. Which indicates blackmailing by peers and management (β = 0.3.169, p < 0.001) contributes greatest effect towards WPVPS as compare to all other factors. The third model added knowledge-based overconfidence with 2nd major effect (β = 0.1.170, p < 0.001). Fourth model included the factor of work tenure greater than others at work (β = 1.002, p < 0.001) as a third major factor. Fifth model added another factor feeling insult (β = 0.523, p < 0.001) as fourth major voice barrier. Model 6 added interpersonal conflict with significant negative effect (β=-0.540, p < 0.001). Which demonstrates frontline healthcare workers do not compromise for patient safety due to interpersonal conflicts. Model 7 added knowledge-based conflict (β = 0.544) as a fourth major fifth substantial factor contributes toward voice WPVPS. Then, model 9,10,11, 12 and 13 added 1st year of service (β = 0.462, p < 0.001), fear of reaction by patients and attendants (β = 0.472, p < 0.001), bad voice experience (β = 0.399, p < 0.001), job insecurity (β = 0.326, p < 0.001), non-cooperative management (β = 0.235, p < 0.001), and fear of increase in workload (β = 0.140, p < 0.001), respectively, as a potential positive contributor towards WPVPS.
The 13th model considered the final model of the study, which indicates significance of three control variables age (β=-0.130, p < 0.001), designation (β = 0.127, p < 0.001), and work experience (β = 0.043, p < 0.10), which indicates significant positive effect of designation and work experience, and negative significant effect of age towards withholding patients’ safety voice. Whereas the model did not demonstrate significant effect of gender. Among voice barriers, blackmailing by peers and management establish largest positive effect (β = 0.2.090, p < 0.001), followed by knowledge based over confidence (β = 0.957, p < 0.001), work tenure greater than others at work (β = 0.907, p < 0.001), knowledge-based conflict (β = 0.816, p < 0.001), fears of reaction by patient and attendants (β = 0.559, p < 0.001), first year of service (β = 0.514, p < 0.001), bad voice experience (β = 0.433, p < 0.001), feeling insult (β = 0.426, p < 0.001), no cooperation by management (β = 0.282, p < 0.001), job insecurity (β = 0.252, p < 0.001), and fear of workload increase (β = 0.140, p < 0.001). Whereas, interpersonal conflict has significant negative effect towards withholding voice behaviour related to patient safety. The R2 value 0.96 shows, identified voice barriers accounts for 96% variation in the dependent variable, withholding voice behaviour related to patient safety. The value of F statistics is 419.402, which is significant at 1% level and evidence significance of overall model. 1.524 the value of Durbin-Watson is less than 2, which indicate there is no problem of autocorrelation.
To measure the direct effect of voice barriers on withholding voice behaviour related to safety at work through multilevel hierarchical regression, at the first step control variables were entered, then, all the voice barriers related to work safety were added at step two, and stepwise method was employed. The results provided three models (See Table 5). First model included gender, which demonstrate significant positive effect towards withholding prohibitive voice related to safety at work (WPVSW). Model 2 included the significant negative effect of shyness (β = 0.303, p < 0.001). Finally, model 3 demonstrated 10 factors with significant effects. Regarding control variables, gender established positive effect (β = 0.471, p < 0.001) and designation evidenced significant negative effect (β=-0.202, p < 0.001). Fear of change in duties identified as substantial factor with largest positive effect (β = 0.731, p < 0.001) on WPVSW. 2nd substantial factor lack of confidence demonstrated significant positive effect (β = 0.730, p < 0.001) on WPVSW. Shyness (β = 0.657, p < 0.001) identified as third largest barrier towards WPVSW. Familiarity with shortage of resources found as fourth dominant factor towards withholding voice related to safety at work. Followed by non-cooperative management (β = 0.179, p < 0.05), workload increase (β = 0.142, p < 0.05), bad voice experience (β = 0.136, p < 0.10), and interpersonal conflicts (β = 0.142, p < 0.10). Whereas, bullying (β=-0.383, p < 0.001) demonstrated negative significant effect toward withholding voice related to safety at work. Job insecurity did not find as significant voice barrier related to work safety. The value of R2 = 0.832, evidenced 83.2% variation in the dependent variable withholding voice behaviour related to work safety, due to independent variables. The value of F = 115.815 is significant at 1% level, which evidence overall acceptability of the model is substantial. Value of Durbin-Watson is less than 2, that indicates model is free from the problem of autocorrelation.
Table 5.
Voice barriers effecting prohibitive behaviour of withholding work-related safety concerns
| Variables | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| (Constant) | 2.287*** | 2.960*** | 1.772*** |
| Gender | 1.357*** | 1.372*** | 0.471*** |
| Designation | − 0.303*** | − 0.202*** | |
| BWS1(Shyness) | 0.657*** | ||
| BWS2(Lack of confidence) | 0.730*** | ||
| BWS3 (Fear of change in duty) | 0.731*** | ||
| BBS1(Bullying) | − 0.383*** | ||
| BBS2(Non cop. management) | 0.179** | ||
| BBS3(Interpersonal conflict) | 0.142* | ||
| BBS4(Job insecurity) | 0.102 | ||
| BBS5(Fear of workload increase) | 0.142** | ||
| BBS6(Bad voice exp.) | 0.136* | ||
| BBS7(Familiarity with shortage of resources) | 0.305*** | ||
| R2 | 0.625 | 0.681 | 0.916 |
| ∆R2 | 0.388 | 0.460 | 0.832 |
| F |
(1-278) 178.043*** |
(2-277) 119.874*** |
(12–267) 115.815*** |
| Durbin-Watson | 1.525 | ||
* indicates a 10% significance level, ** indicates a 5% significance level, *** indicates a 1% significance level
Discussion
This study was conducted to identify voice barriers in the healthcare industry among frontline healthcare workers in Pakistan. Voice behaviors were discerned based on patients’ safety and workers safety. Voice behavior can be categorized into two ways: promotional voice behavior and problem resolving voice behavior. Promotional voice behavior is necessary for innovation and development purposes. Whereas problem-solving voice behavior is essential to overcome challenges. Absence of problem-solving voice behavior tends to decrease health and well-being. We cannot proceed for innovation and development through promotional voice behavior without prohibitive voice behavior. Therefore, in this study, we focused on prohibitive voice behavior among healthcare workers, as it is essential to address workplace challenges.
Healthcare is a sensitive sector, where employees’ prohibitive voice behavior plays a critical role in safe work operations. Worker’s behavior of withholding prohibitive voices affects their mental and physical health destructively. This further affects their behavior towards patients’ safety and increases the rate of medical errors. Healthcare worker’s minor mistake can take life of the patient under treatment or cause long term disability or injury. Thus, to ensure safe working conditions and patients’ safety it is essential to assess prohibitive voice behavior of healthcare workers and underlying factors. In this regard this study answers three questions proposed in the beginning.
First question was “what are the prohibitive voice barriers (patient safety and worker safety), among frontline healthcare workers in Pakistan?” To answer this question the study adopted a qualitative method. Seventeen voice barriers were explored through interviews. Content analysis further categorized these barriers into six main factors: (1) personal traits, (2) uncertainty avoidance, (3) psychosocial factors in the workplace, (4) work tenure, (5) professional knowledge rivalries, and (6) unpleasant experiences of voice raising. In the domain of personal traits, it was explored that individuals do not raise patient safety voices because of lack of confidence and feeling insult in asking for help in diagnosis and treatment. According to them, asking questions shows their inability to work in the hospital. Whereas shyness is another cause due to which healthcare workers are reluctant to raise voices for their own safety. Empirical analysis demonstrated statistical significance of all three factors in affecting prohibitive voice of patient and workers safety. Further, the results are in line with previous studies [40, 41].
The second major domain is uncertainty avoidance. Which suggests that healthcare workers avoid uncertainties by withholding their voices. They do not speak up due to fear of job loss, unnecessary inquiries, changes in duties, salary freezes, and negative reaction of patient attendants. Fear of job loss, fear of blackmailing by peers and management, and negative reaction by patient attendants were identified as significant causes of withholding patient safety voices. Whereas fear of job loss and unwanted change in duty demonstrated significance in withholding workers’ safety voices. The results are supported by previous studies [42].
The third major domain is professional knowledge rivalries. Which demonstrates that healthcare workers have knowledge and technique-based conflicts. Which tends them to disagree on peers’ diagnosis and treatment methods. Thus, their overconfidence of professional knowledge does not let them get others’ opinions. Empirical analysis indicates statistical significance of knowledge-based conflicts affecting patient safety voices. Findings are supported by previous literature [59, 60].
The fourth major reason is the psychosocial factors at the workplace. Interpersonal conflicts, bullying, unsupportive management, perceived injustice, and designation/cadre-based conflicts were explored as voice barriers and grouped in psychosocial factors through content analysis. Empirical findings confirmed the effect of bullying, interpersonal conflicts, awareness of shortage of resources, and unsupportive management on prohibitive voices related to patient safety. Unsupportive management, bullying, awareness of shortage of resources, and interpersonal conflicts were also identified as significant determinants of withholding prohibitive voice related to workers safety. The results are in line with previous studies [43, 44].
The fifth major voice barrier is work tenure. Qualitative results demonstrate that healthcare workers avoid raising voices if their work tenure is shortest or longest at the workplace. Empirical findings demonstrated Work tenure is the significant determinant of withholding voice related to patient safety. Previous studies [50–54] support these findings.
The sixth major voice barrier explored through qualitative findings is voice experience. Healthcare workers those got negative consequence of raising voice in the past, they reluctant to speak up on patient safety and workers safety concerns. Empirical analysis demonstrated statistical significance in this regard. The results are supported by previous studies [46–49].
Secondly, the study answers the question “What are the consequent practices frontline healthcare workers follow within the presence of voice barriers”? Following qualitative methods and using content analysis this study identified several practices healthcare workers adopt in consequence of suppressing voice. For patients’ safety, firstly, they refer them to other health facilities which have all the resources to treat the patients. Secondly, limited resources and threats to voice raising motivate them to open their private clinics and serve the patients part-time. Thirdly, voice barriers cause union protest, but if majority of the healthcare workers face same issue.
The consequence of suppressing voice related to workers safety arise in terms of leave the workstation and accelerating the efforts to transfer to other health facility, using political references to solve their problems at the workplaces, union protests, sharing the problems on social media using fake IDs, quitting the jobs, or working until finding out new jobs. The findings are in line with previous studies [61, 62]. Previous studies suggest that employees leave their job due to workplace problems. However, this study indicates employees leave their jobs if they cannot raise their voices to solve these problems.
The third question, this study answers is “What is the magnitude of effect of voice barriers on withholding prohibitive voice (patient safety and worker safety)”? The study answers this question using hierarchical regression analysis. Related to withholding patent safety voice 15 factors were identified. Based on magnitude of effect these factors were listed in descending order as fear of blackmailing (2.090), knowledge-based overconfidence (0.957), longest work tenure (0.907), knowledge based conflict (0.816), fear of reaction by patient and attendants (0.559), shortest work tenure (0.514), bad experience in raising voice (0.433), feeling insult (0.426), uncooperative management (0.282), job insecurity (0.252), fear of increase in workload (0.140), designation (0.127), and work experience (0.043). The result of the study is in line with previous research in terms of climate of fear [63], bullying [64], organizational tenure [1], unsafe working conditions [64].
However, in this study we have extended previous research related to voice barriers to patient safety as Liang, et al. [2] identified work tenure effect voice behavior, but it was not identified which point of work tenure effect voice behavior. This study extended previous research by evidencing first year of service and work tenure greater than others at work significantly contributes to withholding patient safety voice. Related to unsafe working conditions [23] and safety climate [60], this study evidenced the factors and their effect on withholding patient safety voice, such as non-cooperative management, blackmailing, and job insecurity. Workers personal concerns such as lack of confidence, bad voice experience in the past, and fear of reaction by patient and attendants. Further, voice barriers related to knowledge-based conflict and overconfidence were not identified in previous research related to healthcare.
Regarding withholding voice related to workers safety, it was found that fear of change in duty (0.731), lack of confidence (0.730), shyness (0.657), awareness of lack of resources (0.305) non-cooperative management (0.179), fear of upsurge workload (0.142), interpersonal conflict (0.142), bad experience of raising voice (0.136), and job insecurity (0.102) significantly contributes to withholding voice related to safety at work. None of the previous studies identified the magnitude of effect of these factors on withholding prohibitive voice related to safety at work in healthcare settings. Overall, the results are in line with previous studies in terms of personal (lack of confidence and shyness) and managerial factors (unsupportive management, change in duty, job insecurity, increase in workload), previous experience, and anticipated fears [23, 64].
This study identifies barriers to voicing concerns in healthcare settings, impacting patient safety, work safety, and outcomes. Implications for healthcare management include ensuring resources, transparent procedures, and periodic surveys to assess worker satisfaction, along with safety training and discouraging political favoritism. Policymakers should create protective policies for those raising concerns and discourage political interference. Organizational management needs to address issues like job insecurity and resource shortages, ensuring a safe environment and encouraging workers to speak up. For healthcare workers, safety and resiliency training can enhance confidence and reduce fear, promoting a culture of open communication.
Limitations and future research directions
This study has several future directions to enhance understanding of voice barriers in healthcare sector and in general.
Although this study has identified potential barriers to prohibitive voice behavior related to patient and workers safety among frontline healthcare workers in context of developing country, Pakistan. However, there are certain limitations. First, this study is conducted in context of Pakistan. Thus, the results may vary based on socio demographic characteristics. Future researchers may explore voice barriers in the context of different countries. Second, this study focused on the healthcare sector and frontline healthcare workers. Future researchers may focus on other sectors and healthcare workers other than frontline. Third, this study’s sample consists of public sector hospitals, which are different from private hospitals in terms of resources and management. Therefore, upcoming studies may enhance the understanding of voice barriers in context of private hospitals. Fourth, this study identified the effect of voice barriers on prohibitive voice, the results are controlled based on gender, age, designation, and work experience. Future studies may extend the current study model by investigating moderating effect of gender, age, designation, and work experience on the effect of voice barriers on prohibitive voice. Fifth, this study further suggests examining the effect of prohibitive voice related to work safety on prohibitive voice related to patient safety.
Sixth, there are other factors such as personality traits, cognition, peer support, and other social and environmental factors, which may be helpful to study prohibitive voice behavior. Seventh, this study focused on determinants of prohibitive voice behavior. Future studies can extend the study model employing mediating and moderating techniques by incorporating social and environmental factors. Eighth, the second phase of the study is cross-sectional, and future researchers can adopt a longitudinal research design to further validate the results.
Conclusion
The study concludes that healthcare workers in Pakistan often withhold safety concerns to avoid administrative retaliation, such as salary stoppages, blackmail, and duty reassignments. The lack of a safety culture and power gaps lead to bullying and reduced communication about safety issues. Consequently, many turn to private practices, citing insufficient resources in public hospitals, which increases costs for patients. Other methods include incognito sharing concerns on social media and seeking political support to address problems. This situation highlights significant challenges for both patient and worker safety in public hospitals, underscoring the need for major administrative reorganizations.
Supplementary Information
Authors’ contributions
Dr. Noreen Kanwal designed this study, conducted empirical analysis, prepared the initial draft and refined it based on co-authors’ comments.Dr Ahmad Sharul Nizam and Dr Albaraa reviewed and supervised the study.Dr. Rao Irfan Ali Haider helped in this study’s literature review and data collection.
Funding
This research project's Article Processing Charge (APC) is funded by the YUTP project titled "Assessing the Impact of Energy Transition and Its Speed on Economic Disruption for PETRONAS" (Cost Centre: 015LC0-531). We sincerely extend our gratitude to the management of Universiti Teknologi PETRONAS for their invaluable support in facilitating this research.
Data availability
Data is preserved under the custody of corresponding author and will be available at potential request.
Declarations
Ethics approval and consent to participate
The study obtained approval from the Research Ethics Committee of the Department of Management and Humanities at the University of Technology PETRONAS in Malaysia. The study has followed all the research ethics. All methods were conducted in accordance with the Helsinki guidelines. Respondents were informed about their voluntary participation in the study and purpose of this study. Further, they were ensured that their identity will not be disclosed at any stage and the collected data will be discarded after certain time period. Informed written consent was taken from all respondents prior to data collection.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kanwal N. Nizam Bin Isha AS, Salleh RB, Kanwal N, Al-Mekhlafi A-BA. Paradoxical effects of social media use on workplace interpersonal conflicts, Cogent Bus Manag. 2023;10(1):2200892. 10.1080/23311975.2023.2200892. 2023/12/31 2023. [Google Scholar]
- 2.Liang J, Farh CIC, Farh J-L. Psychological antecedents of promotive and prohibitive Voice: a two-Wave examination. Acad Manag J. 2012;55(1):71–92. 10.5465/amj.2010.0176. /02/01 2012. [Google Scholar]
- 3.David, Aline R. Speak up-related climate and its association with healthcare workers’ speaking up and withholding voice behaviours: a cross-sectional survey in Switzerland. BMJ Qual Saf. 2018;27(10):827. 10.1136/bmjqs-2017-007388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh H, Thomas EJ, Petersen LA, Studdert DM. Medical errors involving trainees: a study of closed malpractice claims from 5 insurers. Arch Intern Med. 2007;167(19):2030–6. [DOI] [PubMed] [Google Scholar]
- 5.Bari A, Khan RA, Rathore AW. Medical errors; causes, consequences, emotional response and resulting behavioral change. Pakistan J Med Sci. 2016;32(3):523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iftikhar S, Sarwar MR, Saqib A, Sarfraz M, Shoaib Q-u-a. Antibiotic prescribing practices and errors among hospitalized pediatric patients suffering from acute respiratory tract infections: a multicenter, cross-sectional study in Pakistan. Medicina. 2019;55(2):44. 10.3390/medicina55020044. [DOI] [PMC free article] [PubMed]
- 7.Ali M, Abbasi BH, Ahmad N, Fazal H, Khan J, Ali SS. Over-the-counter medicines in Pakistan: misuse and overuse. Lancet. 2020;395(10218):116. [DOI] [PubMed] [Google Scholar]
- 8.Dawn. 0.5m die of wrong medication every year, Dawn News; 2022. [Online]. Available: https://www.dawn.com/news/1711142.
- 9.Culbreth R, Spratling R. Drivers of medical errors in the neonatal intensive care unit (NICU): a qualitative analysis. J Neonatal Nurs. 2023;29(1):179–82. 10.1016/j.jnn.2022.05.004. 2023/02/01/. [Google Scholar]
- 10.Verghese A, Charlton B, Kassirer JP, Ramsey M, Ioannidis JPA. Inadequacies of physical examination as a cause of medical errors and adverse events: a Collection of vignettes. Am J Med. 2015;128(12):1322–4.e3. 10.1016/j.amjmed.2015.06.004. 2015/12/01/. [DOI] [PubMed] [Google Scholar]
- 11.Motluk A. Do doctors experiencing burnout make more errors? (in eng). Cmaj. 2018;190(40):E1216-e1217. 10.1503/cmaj.109-5663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shanafelt TD, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251(6):995–1000. [DOI] [PubMed] [Google Scholar]
- 13.Tsiga E, Panagopoulou E, Montgomery A. Examining the link between burnout and medical error: a checklist approach. Burnout Res. 2017;6:1–8. [Google Scholar]
- 14.Nieuwenhuijsen K. Prevention of mental health problems in healthcare workers, from a randomized controlled trial to the implementation in workplaces. Saf Health Work. 2022; 13:S63. 10.1016/j.shaw.2021.12.926. 2022/01/01/. [Google Scholar]
- 15.Sangrà PS et al. Mental health assessment of Spanish frontline healthcare workers during the SARS-CoV-2 pandemic. Med Clínica (English Edition). 2022;159(6): 268–77. 10.1016/j.medcle.2021.11.010. 2022/09/23/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Menon NK, et al. Association of physician burnout with suicidal ideation and medical errors. JAMA Netw open. 2020;3(12):e2028780–2028780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Irigoyen-Otiñano M et al. Suicide among physicians: major risk for women physicians. Psychiatry Res. 2022;310:114441. 10.1016/j.psychres.2022.114441. 2022/04/01/. [DOI] [PubMed] [Google Scholar]
- 18.Harvey SB, et al. Mental illness and suicide among physicians. Lancet. 2021;398(10303):920–30. 10.1016/S0140-6736(21)01596-8. 09/04/ 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Milliken FJ, Morrison EW. Shades of silence: emerging themes and future directions for research on silence in organizations. J Manage Stud. 2003;40(6):1563–8. [Google Scholar]
- 20.Wu F et al. The role of the informal and formal organisation in voice about concerns in healthcare: a qualitative interview study. Soc Sci Med. 2021;280:114050. 10.1016/j.socscimed.2021.114050. 2021/07/01/. [DOI] [PubMed] [Google Scholar]
- 21.Noort MC, Reader TW, Gillespie A. Speaking up to prevent harm: a systematic review of the safety voice literature. Saf Sci. 2019;117:375–87. 10.1016/j.ssci.2019.04.039. 2019/08/01/. [Google Scholar]
- 22.Lee SE, Dahinten VS, Seo J-K, Park I, Lee MY, Han HS. Patient Safety Culture and speaking up among Health Care workers. Asian Nurs Res. 2023;17(1):30–6. 10.1016/j.anr.2023.01.001. 02/01/2023. [DOI] [PubMed] [Google Scholar]
- 23.Morrow KJ, Gustavson AM, Jones J. Speaking up behaviours (safety voices) of healthcare workers: A metasynthesis of qualitative research studies, (in eng). Int J Nurs Stud. 2016;64:42–51. 10.1016/j.ijnurstu.2016.09.014. [DOI] [PubMed] [Google Scholar]
- 24.Fisher M, Kiernan M. Student nurses’ lived experience of patient safety and raising concerns. Nurse Educ Today. 2019;77:1–5. 10.1016/j.nedt.2019.02.015. 2019/06/01/. [DOI] [PubMed] [Google Scholar]
- 25.Lee SE, Dahinten VS. Psychological safety as a mediator of the Relationship between Inclusive Leadership and Nurse Voice behaviors and Error Reporting. J Nurs Scholarsh. 2021;53(6):737–45. 10.1111/jnu.12689. /11/01 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alingh CW, van Wijngaarden JDH, van de Voorde K, Paauwe J, Huijsman R. Speaking up about patient safety concerns: the influence of safety management approaches and climate on nurses’ willingness to speak up. BMJ Qual Saf. 2019;28(1):39–48. [DOI] [PubMed] [Google Scholar]
- 27.Mihdawi M, Al-Amer R, Darwish R, Randall S, Afaneh T. The influence of nursing work environment on patient safety. Workplace Health Saf. 2020;68(8):384–90. [DOI] [PubMed] [Google Scholar]
- 28.Nawaz M, Abid G, Islam T, Hwang J, Lassi Z. Providing Solution in an Emergency: COVID-19 and Voice Behavior of Healthcare Professionals. SAGE Open. 2022;12(4):215824402211417002undefined. 10.1177/21582440221141700. 2022/10/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hobfoll SE. “Conservation of resources. A new attempt at conceptualizing stress.,” (in eng). Am Psychol. 1989;44:513–24. 10.1037//0003-066x.44.3.513. [DOI] [PubMed] [Google Scholar]
- 30.Kock N. Harman’s single factor test in PLS-SEM: checking for common method bias. Data Anal Perspect J. 2020;2(2):1–6. [Google Scholar]
- 31.Kanwal N, Isha ASN. Identifying the Moderating Effect of Hyperconnectivity on the Relationship between Job Demand Control Imbalance, Work-to-Family Conflict, and Health and Well-Being of Office Employees Working in the Oil and Gas Industry, Malaysia. Hum Behav Emerg Technol. 2022;2022(1):5260866. 10.1155/2022/5260866. 2022/01/01. [Google Scholar]
- 32.Akbar MA, Sang J, Nasrullah AA, Khan M, Shafiq, Fazal EA. Towards the guidelines for requirements Change Management in Global Software Development: client-vendor perspective. IEEE Access. 2019;7:76985–7007. 10.1109/ACCESS.2019.2918552. [Google Scholar]
- 33.Akbar MA, et al. Requirements Change Management challenges of Global Software Development: an empirical investigation. IEEE Access. 2020;8:203070–85. 10.1109/ACCESS.2020.3035829. [Google Scholar]
- 34.Kamal T, Zhang Q, Akbar MA, Shafiq M, Gumaei A, Alsanad A. Identification and prioritization of agile requirements Change Management Success factors in the Domain of Global Software Development. IEEE Access. 2020;8:44714–26. 10.1109/ACCESS.2020.2976723. [Google Scholar]
- 35.Schwappach D, Richard A. Speak up-related climate and its association with healthcare workers’ speaking up and withholding voice behaviours: a cross-sectional survey in Switzerland. BMJ Qual Saf. 2018;27(10):827–35. 10.1136/bmjqs-2017-007388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bandura A, Cervone D. Differential engagement of self-reactive influences in cognitive motivation. Organ Behav Hum Decis Process. 1986;38(1):92–113. [Google Scholar]
- 37.Amos B, Klimoski RJ. Courage: making Teamwork Work well. Group Organ Manage. 2014;39(1):110–28. 10.1177/1059601113520407. 2014/02/01. [Google Scholar]
- 38.Shafiq M, et al. Smart E-Health System for Heart Disease Detection Using Artificial Intelligence and Internet of Things Integrated Next-Generation Sensor Networks. J Sens. 2023;2023:6383099. 10.1155/2023/6383099. 2023/04/20. [Google Scholar]
- 39.Shafiq M, et al. Effect of project management in requirements engineering and requirements change management processes for global software development. IEEE Access. 2018;6:25747–63. [Google Scholar]
- 40.Erol M, [Adolescent Life Satisfaction Before Young Adulthood. The role of shyness and Self-Efficacy], (in tur). Turk Psikiyatri Derg. 2017;28(2):95–103. Genç Yetişkinliğin Öncesinde Olan Ergenlerin Yaşam Doyumu: Utangaçlık ve Öz Yeterlik Algısının Rolü. [PubMed] [Google Scholar]
- 41.Ebrahimi A, Safari Gerayli M, Valiyan H. Effects of external and internal drivers of individual behavior voice on the moral courage and internal auditors’ effectiveness. J Acc Organizational Change. 2022;ahead–of–print(no ahead–of–print). 10.1108/JAOC-08-2021-0099.
- 42.Detert JR, Edmondson AC. Implicit voice theories: taken-for-granted rules of self-censorship at work. Acad Manag J. 2011;54(3):461–88. [Google Scholar]
- 43.Subhakaran SE, Dyaram L. Interpersonal antecedents to employee upward voice: mediating role of psychological safety. Int J Product Perform Manag. 2018;67(9):1510–25.
- 44.Van Dyne L, Kamdar D, Joireman J. In-role perceptions buffer the negative impact of low LMX on helping and enhance the positive impact of high LMX on voice. J Appl Psychol. 2008;93(6):1195. [DOI] [PubMed] [Google Scholar]
- 45.Sheeran P, Godin G, Conner M, Germain M. Paradoxical effects of experience: past Behavior both strengthens and weakens the intention-behavior relationship. J Association Consumer Res. 2017;2(3)309–18. 10.1086/691216. 2017/07/01. [Google Scholar]
- 46.Ng TWH, Feldman DC, Butts MM. Psychological contract breaches and employee voice behaviour: the moderating effects of changes in social relationships. Eur J work Organizational Psychol. 2014;23(4):537–53. [Google Scholar]
- 47.Bandura A. Social cognitive theory of self-regulation. Organizational Behavior and Human Decision Processes. 2018;50(2):248–87. 10.1016/0749-5978(91)90022-L. 1991/12/01/. [Google Scholar]
- 48.Albarracín D, Wyer RS Jr. The cognitive impact of past behavior: influences on beliefs, attitudes, and future behavioral decisions, (in eng). J Pers Soc Psychol. 2000;79(1):5–22. 10.1037//0022-3514.79.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ngo H-Y, Tang CS-K, Au WW-T. Behavioural responses to employment discrimination: a study of Hong Kong workers. Int J Hum Resource Manage. 2002;13(8):1206–23. 10.1080/09585190210149484. 2002/01/01. [Google Scholar]
- 50.Zhang S, Bowers AJ, Mao Y. Authentic leadership and teachers’ voice behaviour: the mediating role of psychological empowerment and moderating role of interpersonal trust. Educational Manage Adm Leadersh. 2021;49(5):768–85. [Google Scholar]
- 51.Jena LK, Bhattacharyya P, Pradhan S. Employee engagement and affective organizational commitment: Mediating role of employee voice among Indian service sector employees. Vision. 2017;21(4):356–66. [Google Scholar]
- 52.Starzyk A, Sonnentag S, Albrecht AG. The affective relevance of suggestion-focused and problem‐focused voice: a diary study on voice in meetings. J Occup Organizational Psychol. 2018;91(2):340–61. [Google Scholar]
- 53.Arain GA, Hameed I, Crawshaw JR. Servant leadership and follower voice: the roles of follower felt responsibility for constructive change and avoidance-approach motivation. Eur J Work Organizational Psychol. 2019;28(4):555–65. [Google Scholar]
- 54.Vatcheva KP, Lee M, McCormick JB, Rahbar MH. Multicollinearity in Regression Analyses Conducted in Epidemiologic Studies, (in eng). Epidemiology (Sunnyvale). 2016;6(2). 10.4172/2161-1165.1000227. [DOI] [PMC free article] [PubMed]
- 55.Tharu R. Multiple regression model fitted for job satisfaction of employees working in saving and cooperative organization. 2019:43–9. 10.22271/maths. 07/21.
- 56.Blanca MJ, Arnau J, López-Montiel D, Bono R, Bendayan R. Skewness and kurtosis in real data samples. Methodology: European Journal of Research Methods for the Behavioral and Social Sciences. 2013:9(2):78–84. 10.1027/1614-2241/a000057.
- 57.Hair JF, Hult GTM, Ringle CM, Sarstedt M, Danks NP, Ray S. Evaluation of Reflective Measurement Models, in Partial Least Squares Structural Equation Modeling (PLS-SEM) Using R: A Workbook. J. F. Hair Jr, G. T. M. Hult, C. M. Ringle, M. Sarstedt, N. P. Danks, and S. Ray Eds. Cham: Springer International Publishing; 2021, pp. 75–90.
- 58.Kanwal N, bin Isha ASN, Ali K. New ways of working: a comparative empirical analysis appertaining to health and well-being and psychosocial hazards. Technol Anal Strateg Manag. 2024:1–14.
- 59.Schweiger DM, Sandberg WR, Ragan JW. Group approaches for improving strategic decision making: a comparative analysis of dialectical inquiry, Devil’s advocacy, and consensus. Acad Manag J. 1986;29(1):51–71. [Google Scholar]
- 60.Rubin JZ. Models of conflict management. J Soc Issues. 1994;50(1):33–45. [Google Scholar]
- 61.Ananda-Rajah MR, Veness BG, Berkovic D, Parker C, Kelly G, Ayton D. Hearing the voices of Australian healthcare workers during the COVID-19 pandemic. medRxiv. 2021;5:31–35.
- 62.Rauwolf P, Jones A. Exploring the utility of internal whistleblowing in healthcare via agent-based models. BMJ open. 2019;9(1):e021705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Joseph S, Shetty N. An empirical study on the impact of employee voice and silence on destructive leadership and organizational culture. Asian J Bus Ethics. 2022;11(Suppl 1):85–109. 10.1007/s13520-022-00155-0
- 64.Grabbe L, Higgins MK, Baird M, Pfeiffer KM. Impact of a resiliency training to support the Mental Well-being of front-line workers: brief report of a quasi-experimental study of the Community Resiliency Model, (in eng). Med Care. 2021;59(7):616–21. 10.1097/mlr.0000000000001535. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data is preserved under the custody of corresponding author and will be available at potential request.