Abstract
Background
While the striking impact of the COVID-19 pandemic on mental health, heath care access and lifestyle behaviors, including perceived health, diet, physical activity, and sleep has been reported, few studies have examined these domains jointly among pregnant and postpartum people in the early stages of the COVID-19 pandemic.
Methods
This mixed methods study was conducted among a subset of participants (n = 22) in a cohort study in Austin, Texas, who were pregnant or had recently delivered when the outbreak occurred. Measures were from the early second trimester up to 6 months postpartum. Findings from questionnaires were complemented by qualitative interviews during Spring/Summer 2020 regarding experiences during the early pandemic.
Results
From our quantitative data (n = 22), most participants reported that the pandemic generally had a negative impact on their lives (81%), that they shifted to eating more at home (71%), and that they were less physically active (62%). Five major themes emerged in our qualitative interviews (n = 22): (1) adaptation to pandemic restrictions; (2) psychosocial experiences, such as feelings of anxiety, guilt, sadness, isolation, and frustration; (3) health behavior changes; (4) health care experiences; and (5) where they obtained general and perinatal related pandemic information. Of those who completed both pregnancy and postpartum interviews (n = 8), all reported anxiety during both periods; however, those who delivered in Spring 2020 experienced more anxiety surrounding delivery and less social support than those who delivered in Summer 2020, who reported less anxiety surrounding hospital birth and greater social support, particularly after delivery.
Conclusions
Overall, our findings confirm prior evidence that the COVID-19 pandemic had a marked impact on stress, anxiety, and worries, as well as lifestyle behaviors among pregnant and postpartum people. Our work provides lessons for health care practitioners about support need for pregnant and postpartum persons amid societal disruption.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12884-024-07011-y.
Keywords: COVID-19, Pregnancy, Postpartum, Health behavior, Mental health
Introduction
Pregnancy is a period of marked changes in both physical and mental health and is a time where some people may adopt more or less healthful behaviors [1–3]. Stressful experiences during pregnancy are associated with adverse pregnancy and perinatal outcomes. The impact of these stressful experiences during pregnancy can extend to longer-term behavioral and mental health outcomes, and also affect health-related behaviors during and after pregnancy [4–7]. The SARS-CoV-2 virus and the disease caused by the virus, COVID-19, was identified in the United States in January 2020 and was declared a pandemic by the World Health Organization (WHO) on March 11, 2020. In the early stages of the pandemic, several states, including Texas, issued state-wide disaster proclamations and local stay-at-home orders to attempt to limit the spread of disease [8]. These were coupled with changes in policies and practices among health care providers and systems that influenced prenatal and postpartum care, including a pivot to virtual health care, limiting in-person interaction, and reducing the number of people allowed as visitors during delivery and confinement. Persons who were pregnant or delivered in the early stages of the pandemic experienced dramatic shifts in their lives and health care, and experienced fear about the unknown [8]. As pregnant people were labeled “high-risk” due to the severe threat other coronavirus diseases had exhibited in this group, such as changes in acute immune and cardiorespiratory functions [9], these individuals were particularly vulnerable to the repercussions of the pandemic.
The COVID-19 pandemic had a major impact on mental well-being among pregnant and postpartum people [10]. Beyond the typical anxieties related to pregnancy, pregnant people were also placed in unprecedented situations during the pandemic that directly and indirectly affected their ability to adapt to challenges related to their increased risk for disease, pandemic-related restrictions, mental well-being, health behaviors, and health care experiences [11–13]. These additional COVID-19 stressors were concerning for this vulnerable group, as depression and poor mental health have been shown to be leading underlying causes of pregnancy-related death [14]. Prior to the pandemic, Texas mothers were at risk for mental health challenges with 14% reporting postpartum depression within six months of delivery [15], which is slightly higher than other reports from across the US with an average prevalence of 13.2% across 31 sites [16]. Texas PRAMS data from 2020 show that during depression prevalence during pregnancy is around 12% and postpartum depression prevalence ranges from 12 to 15% [17]. During the pandemic, many individuals experienced extreme anxiety that they or their loved ones might contract the disease, as well as an overwhelming fear of an uncertain future [18]. Pregnant people also experienced stress related to prenatal care, deliveries, transition to parenthood, and fear of infection for themselves, their family members, and their newborn infants [19–22].
Today, the implications of the pandemic on pregnant and postpartum people remain to be understood broadly or incorporated into systems-level support structures for this group [23]. While there have been qualitative and quantitative studies examining the experiences of those who experienced pregnancy and birth during the COVID-19 pandemic globally [12, 13, 19–22, 24–30]. Only two other mixed-methods investigations were found in the literature during preparation of this paper. These papers did not focus on lifestyle behaviors and further, were only conducted among postpartum persons. One of these papers focused specifically among Asian American women and assessed pregnancy and birth experiences, the early postpartum period, and seeking mental health resources [31]. Mothers reported a unique perinatal journey and the emotional and psychological consequences of COIVD-19 [31]. The other paper conducted interviews assessing experiences during pregnancy, labor, birth and postpartum among postpartum women, and reported effects of COVID-19 on birth plans, and mental health [32]. To date, there has been no mixed methods study that has assessed how the early COVID-19 pandemic impacted lifestyle behaviors, mental health, and health care access among both pregnant and postpartum persons.
This study aims to identify and explore the impact of the early stages of the COVID-19 pandemic in pregnant and postpartum people on lifestyle behaviors, mental health, and health care access using both quantitative and qualitative methods to yield a more rich understanding of experiences.The goal of this paper was to apply a mixed methods approach to examine the impact of the COVID-19 pandemic on the lifestyle behaviors, including perceived health, physical activity, sleep, as well as health care access and mental health of pregnant and postpartum people. Participants were enrolled prior to the pandemic and were followed prior to and during the early stages of the COVID-19 pandemic. We hypothesized that the spread of the virus and associated pandemic restrictions had significant negative impacts on participants’ lives, health behaviors, mental health, and access to health care.
Methods
We applied a concurrent mixed methods research design by collecting both quantitative and qualitative data in a subset of a prospective cohort of pregnant and postpartum people. Data collection and analysis of quantitative and qualitative data were conducted independently.
Study participants were a subset of pregnant and postpartum participants (n = 22) from the Mother and Infant NutriTion (MINT) Study enrolled from 08/01/2019 and through 03/13/2020. MINT is a complex longitudinal pregnancy observational cohort study with intensive data collection and nutritional phenotyping (n = 61) that was designed to examine adipose tissue changes during pregnancy and postpartum among mothers and their infants. Due to the pandemic, a subset of participants were recruited prior to late March 2020, and then the next batch of participants were not recruited until 2022. This secondary analysis focuses on the participants who experienced pregnancy or postpartum during the early stages of the COVID-19 pandemic. Participants were recruited into the cohort through flyers and provider referrals at federally qualified health centers and local Ob/Gyn clinics, newsletter announcements, and local social media advertisements. Eligibility criteria included age ≥ 18 years, nonsmoking, no diagnoses of diabetes prior to pregnancy, pre-pregnancy BMI ≤ 35 kg/m2, no history of significant weight change or weight-loss surgery prior to pregnancy, singleton pregnancy, and living within 50 miles of Austin, Texas. The exclusion criteria were gestational age > 14 weeks, MRI contraindications, history of bariatric surgery, delivery outside of partnered hospitals, regularly breastfeeding, and recent significant weight change. These criteria were designed to ensure participants would fit within the MRI during late pregnancy and to ensure that breastfeeding was not impacting prenatal adipose tissue changes. Pregnant participants were enrolled at approximately 14–15 weeks gestation and were prospectively followed, with study visits scheduled at 25- and 35-weeks gestation, at birth, and at 10 days and 6 weeks postpartum. Study visits were conducted in person prior to the pandemic and virtually after the pandemic. Demographic characteristics were collected prior to the pandemic and included age, race and ethnicity, income, education, and parity.
After the onset of the pandemic, the research team added a qualitative interview and an additional questionnaire about COVID-19 to be delivered in the late second trimester or during the third trimester of pregnancy, or within the first two months after delivery for postpartum participants. Interviews were completed by female research staff members who had built relationships with the participants prior to the pandemic. The questionnaire included the 4-item Perceived Stress Scale (PSS-4) [33]; Brief Resilience Scale [34]; several items that were adapted from other stress scales (e.g., Stanford Acute Stress Reaction Questionnaire) or diagnostic criteria (e.g., DSM-5 criteria for acute stress disorder) [35–39]; and instruments that were developed for this study to assess pandemic-specific worries and concerns, and impacts on health and other areas of life (e.g., childcare, employment, health behaviors). Pandemic-specific worry and concern items covered fear of exposure to or infection with the coronavirus, access to health care or social support, and enactment of behavioral restrictions such as quarantining and social distancing. The 5-point Likert scales ranged from Not at all worried to Extremely worried and from Not at all concerned to Extremely concerned. Statistical analyses were conducted using Stata SE 15 (College Station, TX). The questionnaire was sent to enrolled participants in May 2020 via the secure web platform Research Electronic Data Capture (REDCap). A two-tailed t-test p value of < 0.05 was considered statistically significant when assessing differences between groups (e.g., pregnant vs. postpartum mothers; first-time mothers vs. mothers with older children). Descriptive statistics, such as frequencies, percentages, and means, were reported in this paper.
For qualitative interviews, a semi-structured interview guide (S1 Table) was developed by the authors by reviewing relevant literature and seeking input of the interdisciplinary team. The major themes included the COVID-19 pandemic’s impact on participants’ daily lives, health behaviors (e.g., diet, physical activity, sleep), emotional and mental health, and health care. Two researchers trained in qualitative methods (SD and GD) conducted interviews. Interviews were audio-recorded and lasted approximately one hour. Participants were invited to complete interviews during pregnancy and/or postpartum. Ten women participated in a pregnancy interview and 15 participated in a postpartum interview, which were held on or after 6 weeks postpartum. Eight women completed both a pregnancy and a postpartum interview. Pregnancy interviews were conducted from 06/24/2020 to 07/10/2020, while postpartum interviews were conducted from 6/10/2020 to 10/21/2020.
Among the 22 participants enrolled in the observational study, 25 semi-structured interviews were conducted via phone (n = 23) and Zoom (n = 2). Audio files were transcribed, reviewed, and checked against interviewer field notes for quality, accuracy, and to de-identify transcripts. All interviews were conducted in English. The data were analyzed through inductive methods, specifically grounded theory [40, 41]. The data were analyzed through grounded theory analysis. Four data coders independently did open coding by reading 10% of the transcripts line by line to capture emerging concepts. At the second stage, axial coding involves connecting initial concepts to exploring the relationship and patterns among these concepts. At the third stage, the selective coding process was conducted focusing on identifying central themes from the data. Through this process, a codebook was finalized comprised of sub-themes and themes along with the conceptual definitions. Once we finalized the codebook, three trained data coders (SD, GD, and JG) then independently conducted line-by-line coding with the remaining transcripts using NVivo software to organize quotes and summarize themes, and used group consensus to facilitate agreement between coders to reconcile discrepancies.
Ethical consideration
This study was approved by The University of Texas at Austin’s Office of Research Support and Compliance Institutional Review Board. Informed consent was obtained through DocuSign and verbal informed consent was confirmed prior to the collection of qualitative data. Participants were provided with electronic gift cards immediately after individual questionnaires and interviews were completed.
Results
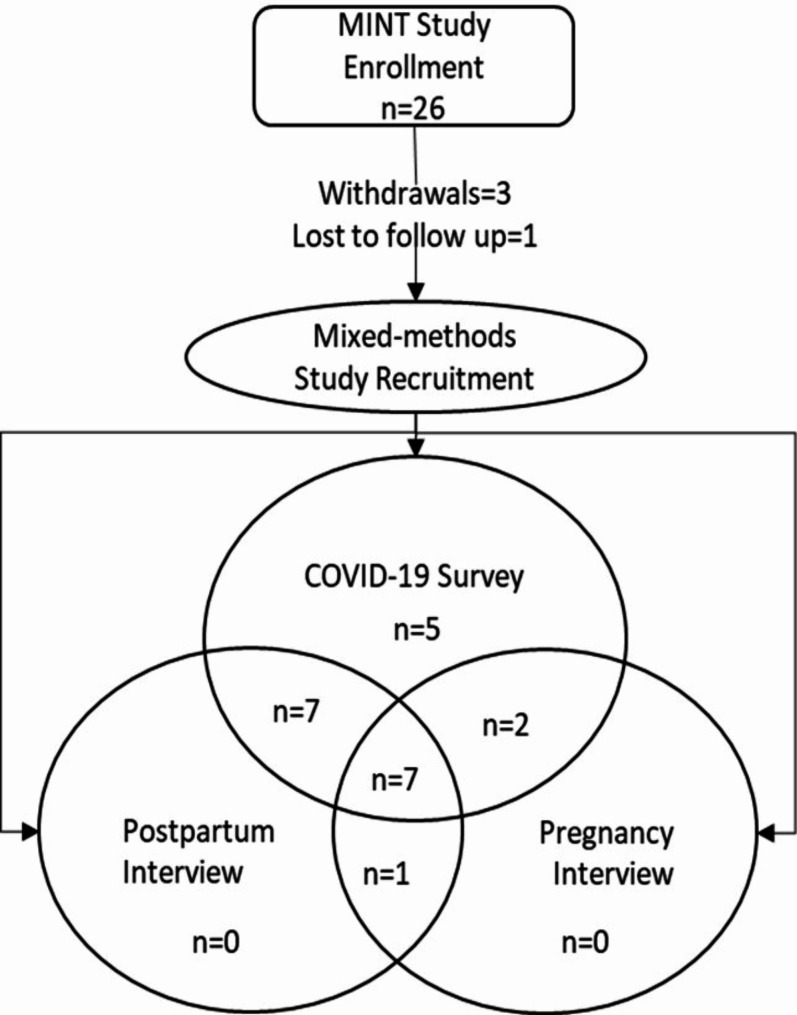
Of the 26 participants enrolled into MINT prior to 03/13/2020, three participants withdrew, and one participant was lost to follow up, resulting in 22 participants eligible for this study. Twenty-one participants (95% of those eligible) completed the questionnaire were included in the quantitative and 17 (77% of those eligible) participated in the qualitative components of this study (Fig. 1). Based on the timing of enrollment into the cohort relative to the onset of the pandemic and when the infants were born, some participants had prenatal and/or postpartum interviews. Questionnaires completed during pregnancy (71%) were conducted at mean 32.3 (± 4.6) weeks gestation, while postpartum questionnaires (29%) were conducted on average at 7.0 (± 4.3) weeks postpartum. Of those who participated in the qualitative interview, 10 were pregnant and were on average 33.9 (± 2.5) weeks gestation, while the 15 postpartum interviews were conducted on average 8.7 (± 3.1) weeks since birth. 7 participants completed the questionnaire as well as two interviews, one during pregnancy and one postpartum.
Fig. 1.
Participant Enrollment (n = 22)
Demographic characteristics of participants in this sub-study are shown in Table 1. The majority of participants were Non-Hispanic White, married or living with their partner, educated at a college level, and had a household income above $100,000. Slightly more than half of participants were primiparous; demographics did not differ by parity status.
Table 1.
Participant characteristics (n = 22)
| n (%) or Mean (± SD) | |
|---|---|
| Age | 32.2 (± 3.9) |
| Hispanic Ethnicity | 1 (5) |
| Race | |
| White/Caucasian | 18 (81) |
| Black/African American | 1 (5) |
| Asian | 1 (5) |
| More than one race | 2 (9) |
| Married or cohabitating with significant other | 21 (95) |
| College Degree or Postgraduate Work | 21 (95) |
| Household Income of $100,000 or more | 15 (68) |
| First pregnancy/birth | 13 (59) |
Quantitative results
Questionnaire results are shown in Table 2. Most participants reported no changes in employment, but did shift to working from home as almost all were under local stay-at-home orders. Nine participants had older children, and almost all of those participants reported closure of their childcare facility. The format of antenatal care (ANC) or postnatal care (PNC) changed from in-person appointments to telemedicine or video conference for over half of participants.
Table 2.
Quantitative results of COVID-19 impacts on participant circumstances, behaviors, intentions, and well-being
| Variable | n (%) or Mean (± SD) |
|---|---|
| Changes in circumstances | |
| Under local stay-at-home orders or employer encouraged | 17 (81) |
| No changes to employment | 13 (62) |
| Moved to remote work/work from home | 12 (57) |
| Child’s daycare/preschool/school closed | 8 (89) |
| The format of ANC/PNC changed | 13 (62) |
| Changes in behaviors | |
| Eating more home cooked meals | 15 (71) |
| Eating same amount (quantity) | 12 (57) |
| Doing less physical activity | 13 (62) |
| Doing more screen-time activities (e.g., TV, social media) | 14 (67) |
| Sleeping same amount | 14 (67) |
| Talking with friends/family by phone/text/video same amount | 9 (43) |
| Talking with medical health care provider same amount | 12 (63) |
| Talking with mental health care provider same amount | 4 (67) |
| COVID-19 pandemic had a general negative impact | 17 (81) |
|
Perceived stress sum score (range 0–16) Change in stress level (scale 1–10) |
9.1 (± 3.0) 1.1 (± 1.8) |
|
Responses on likert scale of 1–5 with higher scores indicating greater stress, concerns, worries or resiliency General stress related to perinatal experiences |
2.3 (± 1.0) |
| Acute stress | 2.3 (± 0.6) |
| Concerns overall | 2.3 (± 0.5) |
| Impact on your community | 3.5 (± 1.1) |
| Other | 3.5 (± 1.9) |
| An elderly relative or close family friend will get COVID-19 | 3.2 (± 1.1) |
| Worries overall | 3.3 (± 0.7) |
| Being separated from my baby after delivery | 3.9 (± 1.1) |
| Contracting the coronavirus after my baby’s birth and not being able to care for my baby | 3.8 (± 1.2) |
| Changing my plans to breastfeed due to COVID-19 | 2.2 (± 0.3) |
| Resilience | 3.9 (± 0.7) |
Overall, participants shifted their behaviors during the pandemic to eating more home-cooked meals, and doing less physical activity and more screen-time activities compared with their pre-pandemic levels. Some behaviors were maintained, with most participants reporting that they were eating the same quantity of food, and sleeping and talking with their friends, family, and health care providers at similar levels as they had before the pandemic. S2 Table compares questionnaire responses between prenatal vs. postpartum participants and between first-time mothers vs. mothers with older children. A majority of postpartum participants reported eating more and sleeping less during the pandemic compared with before the pandemic, while a majority of prenatal participants reported no change in these behaviors. Mothers with children were less likely to report decreases in their physical activity but more likely to report increased screen-time activities than first-time mothers. Though most participants reported talking to health care providers at the same amount as pre-pandemic levels, pregnant participants were more likely to report talking with health care providers less during the pandemic than postpartum participants. Participants with older children were more likely to report talking more with a mental health care provider compared to pre-pandemic, than the first-time mothers, but parents with older children reported that they spoke less with their medical health care provider.
Regarding emotional and mental well-being, most participants indicated the pandemic had a generally negative impact. Participants reported higher stress levels, with moderate general stress and a mean 1.1-point increase from their recalled pre-pandemic stress levels on a scale of 1 to 10. Mean perceived stress scale sum score also indicated elevated stress levels among participants, as higher scores indicate more perceived stress. Participants reported that they were worried or concerned about a variety of factors, including impact on the community, concern over a loved one contracting COVID-19, and being separated from or not being able to care for their baby due to COVID-19. The only significant difference between groups was the worry that participants would have to change their plans to breastfeed their baby due to COVID-19, with first-time mothers and postpartum mothers being significantly more worried than mothers with older children and pregnant mothers, respectively. While not significantly different, first-time mothers were more likely to report higher scores for most measures of stress, worries, and concerns compared with mothers with older children. Similarly, postpartum mothers were more likely to report higher scores on these measures compared to pregnant mothers.
The mean resilience score of participants indicated that they had normal resilience (reference ranges being 1.00-2.99 for low resilience, 3.00-4.30 for normal, and 4.31-5.00 for high) [34]. Mothers with older children were more likely to report nonsignificant higher resiliency scores compared with first-time mothers. Pregnant mothers were also more likely than postpartum mothers to report higher resiliency, also not significant. Participants who scored normal and high for resiliency did not show any significant differences in their stress scores or health behavior scores compared with other participants. Participants with low resiliency scores, however, showed significantly higher acute stress (3.3 ± 0.1 vs. 2.3 ± 0.3) and overall concern (3.0 ± 0.1 vs. 2.2 ± 0.1) scores compared with other participants. Low resilience participants were also significantly more concerned about their ability to access baby supplies (3.0 ± 1.0 vs. 1.6 ± 0.1) and personal or household supplies (3.0 ± 1.0 vs. 1.5 ± 0.2), not being able to access medical (4.0 ± 0.0 vs. 1.8 ± 0.2) or mental (3.5 ± 1.5 vs. 1.7 ± 0.2) health care, and were significantly more likely to indicate they felt their quality of health care had worsened during the pandemic (0.5 ± 0.5 vs. 0.1 ± 0.1) compared with other participants.
Qualitative results
The qualitative analysis yielded five major themes, as described below. Within these major themes, 13 sub-themes emerged and are listed in Table 3.
Table 3.
Qualitative results
| Major themes | Sub-themes | Brief summary |
|---|---|---|
| Adapting to pandemic restrictions | Work life transformed | Offices closures lead to remote work and lack of in-person interaction with colleagues. Social life shifted to online platforms. |
| Changes in socialization | Participants were spending more time with friends and relatives through social media. | |
| Difficulty adapting to pandemic restrictions | Participants expressed difficulty accepting or dealing with the consequences of virus transmission and pandemic closures. | |
| Psychosocial experiences in pregnancy and postpartum | Anxiety, guilt, sadness and frustration | The pandemic brought forth a range of emotions, from frustration over mask-wearing and political divides, to heightened anxiety and a sense of loneliness. |
| Coping mechanisms and social support | Participants coped with disappointment and sadness through activities (e.g., walking and home projects) and social support. Support from friends, neighbors, and relatives through group texts and doorstep drop-offs played a significant role in providing connection and solidarity during the pandemic. | |
| Other feelings during the pandemic | The pandemic offered participants opportunities to find and express other emotions, such as shame, gratitude, and resiliency. | |
| Changes in health behaviors | Changes in physical activity | Participants had to adjust their physical activities according to closures, the weather, and their pregnancy or postpartum symptoms. |
| Changing in diet | Pandemic prompted a shift in grocery shopping habits, which resulted in a change in diet towards longer-lasting food choices, such as frozen, canned, and processed foods over fresh foods that don’t last as long. | |
| Changes in sleep patterns | Reduced or changed workloads led to shifts in sleep patterns for participants. | |
| Health care experiences | Changes to ANC and PNC | Almost all participants reported their ANC/PNC changed from in-person to telehealth or video appointments. |
| Other changes made to health care | Participants reported changes (e.g., change to telehealth, canceled appointments) in health care appointments beyond ANC/PNC for themselves and their family members. | |
| Information Sources | Trust deficit on COVID-related information | Participants relied on various sources for pandemic information but expressed skepticism due to limited reliability. |
Adapting to pandemic restrictions
From changes in work responsibilities and format, changes in socialization practices, and difficulty adjusting to pandemic restrictions, pregnant and postpartum participants experienced significant changes to their daily lives. Most participants reported that they were working from home and experienced limited face-to-face interaction with colleagues. This perception was echoed by a pregnant participant:
My office closed on March 16th. So, I started working from home then and I haven’t been in the office since. I think it’s gonna be closed to the end of the year. No more face-time with work colleagues. No more, I guess, that sort of routine of getting up and going to the office. – 31 weeks gestation, age 30, Asian.
Most participants spent substantial time using social media to connect with other people due to the pandemic restrictions. Social and religious gatherings switched to online meetings. According to one participant:
We socialize differently. We do a lot of Facebook, video chat… some people we’ve been talking to more than we would’ve before…We stopped going, obviously, and we still haven’t picked it back up because I don’t feel comfortable yet, to [OLDER CHILD’S] extra-curricular stuff. Religiously, our services have switched to Zoom. – 33 weeks gestation, age 33, White/American-Indian.
All participants described the general nature of the changes they had to make to adjust and adapt to the pandemic and pandemic-related restrictions. In addition, several participants explained the negative or long-lasting implications those changes might have. A postpartum participant reported:
We had been planning to send [BABY] to daycare, we didn’t know when and as of right now we’re trying to keep [BABY] home as long as possible, just to avoid exposure and we also want to make sure [BABY] gets vaccines and builds up an immune system before we send [BABY] out into the world. We’re kind of waiting until we have no other choice. – 8 weeks postpartum, age 33, Hispanic White.
Another participant reported how the pandemic was compounding her difficulties:
I know that COVID is making it so much worse, because what I would do to cope, I can’t do. I can’t go to a coffee shop and take her and just feel like I have a life again. I just feel I am isolated. I don’t get to see people and it sucks. It has been super sucky. – 9 weeks postpartum, age 33, White.
Psychosocial experiences in pregnancy and postpartum
Sub-themes of anxiety, frustration, coping mechanisms, social support, and other experiences emerged. Participants repeatedly described feelings of anxiety, sadness, guilt, frustration, anger, loss of control, and loneliness due to the fear of rapid transmission of COVID-19 virus and politicization of the pandemic. As described by one pregnant participant:
There’s been some frustration and anger at people not wanting to wear a mask and things like that…I kinda felt like when the orders got lifted that it was gonna come back and spike right around the time, I was due. So, when I would have to go grocery shopping or something and I would wear a mask and I would see so many people out in public not, it would definitely make me upset… that was very frustrating as far as knowing it was going to come back to impact me. – 38 weeks gestation, age 25, White.
Feelings of anxiety and isolation were particularly acute in postpartum interviews, with participants expressing concern about their newborns and lacking the social support they may have been originally planning for as part of their postpartum care plan.
My anxiety was higher [as] more of a side effect of the things not happening the way that they should happened. Not being able to have a regular baby shower, not being able to have a normal birth experience, not being able to have my normal support system afterward. I mean all of that. Not being able to go and see – I couldn’t get visits from any of my work friends when I was in the hospital or after. Or, ya know, I couldn’t get any of my friends to come see me after the baby was born like they normally would have. – 11 weeks postpartum, age 35, White.
Despite these feelings, most participants also exhibited resiliency by describing ways they were coping with the increased stressors of the pandemic. One pregnant woman reported that:
I think for me, the way I dealt with it was I just gave myself some time to be disappointed and sad. And said, ‘Ya know what, there’s bigger things in the world going on, but this still impacts me.’ I gave myself a couple of days…And I just kind of focused on the fact that I’m still really blessed to be where I’m at. – 38 weeks gestation, age 25, White.
Additionally, participants expressed feelings of pride in their abilities to parent their child(ren) and adapt during such difficult times.
If you had told me that this was coming and this was gonna be my postpartum experience, I probably wouldn’t have had this baby. Which would’ve been sad, of course. And, as it turns out, we did all the things that needed to be done, so far. And we survived, and I didn’t have mental or mood issues so severe that it caused irreparable harm. So, I would say that we succeeded through this, and I wouldn’t have guessed … now we have our daughter, and we realized that we’re stronger than we thought. And it’s changing the way I’m thinking about being a parent in the future … so that has really been nice. – 12 weeks postpartum, age 36, White/American Indian.
Changes in health behaviors
Three sub-themes emerged relating to changes in health behaviors among pregnant and postpartum women: changes in diet, changes in physical activity, and changes in sleeping patterns.
In interviews, most participants described changes in their eating patterns and food sources as pandemic restrictions and supply chain issues limited their access to grocery stores and fresh vegetable and fruits. This led some participants to consume more frozen and processed food items relative to their pre-pandemic intakes. One participant highlighted:
A lot less fruits and vegetables because you can only have those in the beginning of the grocery run. Since they go faster than anything else. All the frozen stuff. We’re doing a lot more canned and powdered stuff, like milk. Evaporated milk and powdered milk; usually we get a lot of fresh milk. So, I think we tried to find alternatives. Protein’s a problem, so we started stocking up on protein powder for example. We have a lot of canned beans, which we normally didn’t used to consume. I freeze a lot of my vegetables now. I guess in that way it has changed. I guess we adapted to having more longevity in foods. – 31 weeks gestation, age 30, Asian.
Interviews also revealed that participants were generally less physically active due to barriers related to pandemic restrictions, pregnancy discomfort, and summer heat. Several participants described alternative ways they were able to stay active during the pandemic, such as working out at home or walking in their neighborhoods.
Luckily, one of things that has saved us having the boys at home is a lot of outside time. So, going on lots of walks and doing lots of things outside. So, we try and do at least two long walks or two outside times a day to just kind of help with the boys and give us a break from work when we’re home. – 30 weeks gestation, age 31, White.
Due to the pandemic restrictions, most participants spent more time at home and reported that their work burden had slowed or changed, and that this lifestyle adjustment influenced their sleep patterns. A pregnant participant alluded:
Because my work has really slowed down tremendously, I was in an adjustment period of not having to get up super early. So, my sleep – I don’t know if erratic is the word, but I stay up later, I sleep in later, I take naps. – 34 weeks gestation, age 39, White.
Health care experiences
Changes to ANC and PNC and other health care changes were the sub-themes of health care experiences of the pregnant and postpartum people in this study. Interviews revealed that almost all participants received telehealth or video consultations for their ANC during the pandemic, and several reported that their health care providers also canceled all in-person consultations. These changes sometimes resulted in delayed or confusing ANC, as evidenced by one postpartum mother:
I stopped having in-person appointments for most of my appointments. I think I had one appointment after the pandemic started in my third trimester. So, I had my 36-week appointment, and I went to the hospital when I was 39 weeks in labor. Those were the times that I’ve actually seen a health care provider … I think they canceled a third of [my appointments] and then moved the rest to telehealth. – 6 weeks postpartum, age 30, White.
I would say I got definitely less in-person postpartum checks, which had no, no visible effect, except it could have, you know. I don’t think that it did, but it could have. My midwife came to check on us for the postpartum like day 2, but then she didn’t come for the 2-week, that was virtual. I had a few therapy, psychotherapy sessions and I’ve had a few psychiatrist, many psychiatrist appointments, and they’re all virtual. I did have enough anxiety and trouble sleeping and that I did seek medication therapy, and I think that, um, I wouldn’t have needed those medications if I hadn’t had the excess worry and decreased rest and self-care that came up because of COVID. – 12 weeks postpartum, age 36, White/American-Indian.
When the health care system shifted to accommodate pandemic restrictions, patient preference was also highly compromised. The same participant reported her experience of receiving care from a new physician in each consultation:
It was typically a different Ob/Gyn each time, because they had moved a lot of the schedule around. So, for the first part of my pregnancy, before the pandemic, I saw the same OB each time. For that third trimester, I saw a different person each time, and I often wouldn’t find out who it was going to be until the week of the appointment. – 6 weeks postpartum, age 30, White.
Participants also reported an absence of in-person support, with infection control policies prohibiting partners from attending ANC and pediatric appointments and restricting mothers from bringing their babies with them to PNC appointments.
The biggest change to my health care would just be that my husband hasn’t been able to be as involved. I know that that’s been really hard on both of us. – 38 weeks gestation, age 25, White.
My 6-week [appointment], when I was supposed to go back to be seen, I was turned away at the door because I didn’t have anyone to watch [BABY and had to bring him with me]. I ended up having to make a special call because I work in the hospital to basically get around it in order to do my 6-week postpartum visit. – 11 weeks postpartum, age 35, White.
Apart from the regular ANC and pediatric care, participants also described canceling or delaying appointments they deemed non-essential in order to reduce their risk of exposure to the virus.
I ended up canceling [OLDER CHILD’S] dentist appointment. I canceled a follow-up for [OLDER CHILD’S] ENT. My husband canceled his dentist appointment. We just haven’t really been doing any appointments, unless we thought they were really vital. – 33 weeks gestation, age 33, White/American Indian.
Sources of pandemic information
Participants reported the sources they used to learn more about the pandemic, local and national responses, and what they should do personally. While many reported looking to the Centers for Disease Control and Prevention (CDC) and the WHO for guidance, they reported also getting information from their personal health care providers, friends and family, employers, school districts, and stories from the internet or social media. Participants commented on the limits of all information sources, including the CDC, WHO, and health care providers, in terms of reliability and trustworthiness.
I remember my doctor at one point mentioning that based on the research that had come out, pregnant women were actually doing well with COVID. And I just took that with a grain of salt because that was back in late March [2020], and I’m like, ‘Thank you for telling me that.’ But I know that the research at that point, the timeline was just small and the sample size was so small, so how could you really make a definitive claim to that? It was more of a ‘Thank you, I’m still going to be cautious.’ – 32 weeks gestation, age 28, White.
Crosscutting trends experienced during and after pregnancy
Across pregnancy interviews, participants mostly discussed how they were adapting to the pandemic and associated restrictions, and the specific behaviors they were engaging in to reduce their risk of infection. Pregnant participants also expressed their anxiety as it related to being exposed to the coronavirus, the unknowns related to the pandemic, and other concerns they had. Postpartum participants expressed increased anxiety related to coronavirus exposure and other worries. They also spoke more about behaviors they were taking to reduce their and their baby’s risk. Postpartum participants were also more likely to describe how their access to health care was less interrupted, as they were more able to maintain their baby’s pediatric appointments than their own prenatal appointments. Postpartum participants were more likely than pregnant participants to express that they lacked social support and were also more likely to discuss all the ways they were coping with the stresses presented by the pandemic.
[I used] a lot of the techniques that I learned to deal with the anxiety. So, negative, catastrophic thinking. Stopping those things, recognizing those things as being transient. Buddhist nonattachment-type thoughts, and …I’ve been journaling, which I don’t think I would’ve done quite as religiously. – 12 weeks postpartum, age 36, White/American Indian.
Among the eight participants who completed both interviews, in pregnancy these participants discussed their anxieties generally and how their anxiety related to delivering their babies in the hospital, and how they felt as they balanced getting essential health care with the risk of exposing themselves to the coronavirus. Postpartum, these participants shared much of the same sentiments as the overall postpartum sample but also described some instances where they were able to access social support from their family members by creating a “pandemic pod” or “pandemic bubble.”
We were basically seeing my mom and that was the extent of doing things throughout the pandemic. In the lead up to [BABY’S] due date, my mom, she quarantined completely from seeing my nephews and my brother and sister-in-law. So, she came down to help with the baby when she was born. – 34 weeks gestation, age 32, White.
Discussion
This study highlights the experiences of women before and after childbirth, and how significantly their lives and health behaviors changed in the midst of the COVID-19 pandemic and lockdown in 2020, using both quantitative and qualitative methods. Quantitative results provided general insights into how the pandemic impacted participants’ daily lives, well-being and feelings, and how they had changed their health behaviors. Survey responses indicate near universal changes in the format of their work, health care, and socialization. Participants did report changes in their diet, physical activity, and screen-time behaviors. They also reported increased stress and were concerned or worried about many topics. Qualitative results provided a richer understanding of how exactly pandemic policies and events specifically impacted pregnant and postpartum individuals. Participants shared their feelings about these adjustments, mostly expressing anxiety, guilt, sadness, and frustration. Participants also shared how they were coping with these feelings and disruptions, and how they were managing social support during times of social distancing. Qualitative themes and subthemes also shed more light on how participants experienced changes made to the medical and mental health care they and their families received during the pandemic, and where participants looked for reliable information regarding the pandemic, their personal risk, and recommendations for their personal behaviors.
Participants adopted behaviors to reduce their risk for exposure and disease, such as social distancing, wearing masks, and working and caring for their children at home. As participants worked more from home, they reported being able to sleep and wake on their own schedule in interviews despite reporting getting the same amount of sleep as their pre-pandemic levels in the questionnaire. Unsurprisingly, participants who delivered their babies by the time they completed the questionnaire were the only group that reported getting less sleep than they did before the pandemic, likely reflecting the realities of taking care of a newborn. Within the family, roles were adjusted to suit their new needs. Partners were prevented from attending prenatal or pediatrician appointments, consistent with other studies globally [12, 13, 22, 29–31], thereby putting more responsibility on participants to retain and relay medical information to the other caregiver(s). Similar to other research [42], in-person interaction decreased substantially, and many participants turned to social media and technology to connect with their family and friends while practicing social distancing. Access to health care also changed significantly due to the pandemic, with most participants reporting a shift to virtual appointments and altered hospital experiences when delivering their babies. These findings are consistent with prior research that has also highlighted that prenatal telehealth consultation was common and generally viewed positively [29, 32, 43, 44]. However, women also expressed various concerns about receiving prenatal telehealth care including monitoring the pregnancy at home, connectivity issues, and perceived insufficient patient-provider discussion via teleheath appointments [43–45]. This was exemplified by one participant explaining that she only saw a health care provider once in person during her third trimester.
The burden of the pandemic also indirectly affected participants’ health behaviors. Participants adjusted their behaviors to accommodate pandemic restrictions and supply chain interruptions. As reported nationally, there were shortages of household and food items available, which led families to change their shopping habits [46]. The focus changed from fresh produce to foods that were more readily available or had a longer shelf-life (such as canned foods, frozen items, and other nonperishable foods) since families elected to stretch the time between grocery trips. Similar findings were also reported from a study conducted in Denmark, Slovenia, and Germany: people shopped less frequently during lockdown and there was an overall reduction in the consumption of fresh foods, but an increase in the consumption of food with a longer shelf-life [47]. While most of our participants reported in the survey that they cooked more meals at home than before the pandemic, in interviews some described eating more meals from fast-food chains as a way to cope. Compared with pregnant mothers, postpartum mothers who completed the survey were less likely to report eating more home cooked meals than they did before the pandemic; this may reflect using take-out food as a coping mechanism or how busy mothers felt as they juggled caring for a newborn during a global pandemic. Both changes in food availability and changes in the nutritional needs of mothers who are breastfeeding may have also contributed to postpartum participants’ increased likelihood of eating more in quantity during the pandemic compared with pregnant mothers.
Consistent with other findings [26], more than half of participants reported less physical activity. As most participants began working from home, they no longer benefited from the daily activity they engaged in while working. This trend was seen across participants regardless of how active their jobs were prior to the pandemic; from participants who had more active jobs (e.g., nurse, university-level athletic trainer) to participants who had office-based positions (e.g., bank teller, software developer). Group differences were more likely to be seen comparing first-time mothers with mothers with older children. First-time mothers were more likely to report a decrease in physical activity during the pandemic, which may be due to mothers with older children using physical activity as way to pass the time with their children while everyone was home. Throughout interviews, participants also reported changes in the types of activities they could engage in and the frequency. Participants’ usual activity locations were either closed or perceived to be too crowded, making it difficult for them to be active and continue their preferred activities. Although not reflected in questionnaire results, in interviews pregnant participants also described feeling increasingly uncomfortable in their bodies and the Texas heat as their pregnancies progressed, making it more difficult for them to be active. Despite the barriers and consistent with other research [26, 42], several participants stated that they began to walk around their neighborhoods more than they had prior to the pandemic, and even turned to walking as a way to cope with the stress of the pandemic.
In addition to the changes to participants’ daily lives and health behaviors, the authors were particularly struck with the impact of the pandemic on participants’ mental health and well-being. Consistent with other research [11–13, 20–22, 24–28, 31, 32, 42], participants’ initial responses to the rapidly evolving pandemic included anxiety and fear of coronavirus exposure and the repercussions. Beyond this, in interviews, participants also expressed anxiety about a variety of topics, from the unknowns related to delivering their child in a hospital with COVID restrictions to concern about how to parent their older children during uncertain times. They mourned not being able to celebrate their pregnancies with their families and friends, and once home with their newborns they expressed continued sadness as many of their loved ones could not provide needed postpartum support due to fear of coronavirus exposure. Consistent with other international qualitative research [11, 13, 20, 22, 29–32, 42, 43], forced changes in socialization negatively affected participants’ psychosocial well-being. Participants expressed feelings of loneliness, isolation, sadness, and guilt in interviews. They also reported that the rapidly changing COVID protocols implemented at their prenatal clinics and hospitals contributed to feelings of unease and made them more concerned about the quality of care they were receiving. These qualitative findings were reflected in questionnaire results and are consistent with other surveys [19, 25]. Although only one participant reported clinically depressive symptoms (and was thus provided with resources and referrals), several reported increased stress, a general negative impact of pandemic, worries about getting COVID and not being able to care for their infant, and negative impacts specific to their community, the economy, and childcare. These qualitative findings are supported by quantitative results and are consistent with a systematic review indicating a rise in anxiety and depressive symptoms among mothers with young children in the pandemic [10].
While some anxiety may occur naturally during pregnancy as parents prepare to welcome a baby, the COVID-19 pandemic compounded participants’ feelings and added feelings of frustration as they observed others’ actions or inactions during the pandemic. On one end of the spectrum, consistent with other studies, the health care system’s implementation of conservative risk-reduction protocols seemed to have decreased participants’ access to physical care and contributed to their feelings of frustration, fear, anxiety, and increased responsibility for their own and their baby’s well-being [22, 30, 43, 48]. If participants did have in-person care, visitors were unable to accompany them, as evidenced by our participant who was prohibited from bringing her baby to her postpartum check-up despite being a single mother and unable to access childcare support due to social distancing closures and precautions. On the other end of the spectrum, several participants explained that when they observed the numbers of infected individuals increasing in their area, they were angry and frustrated that others were not participating in preventive measures, such as mask-wearing and social distancing. When the state of Texas adjusted its policies regarding pandemic precautions toward greater leniency, participants felt a heightened sense of fear, rather than the relief that others may have felt. Participants perceived the relaxation of precautionary policies as an action that increased their personal risk. This added to their feelings of frustration and anger toward policymakers and the general public for making pandemic precautions a polarizing political issue.
While they experienced a myriad of stressors and feelings during the pandemic, consistent with other studies [21, 29, 42], participants were still able to demonstrate their resiliency and develop coping mechanisms to help them during such difficult times. Although quantitative results did not elucidate protective factors for resiliency, through interviews participants shared how they found alternative means to receive support as they participated in meal trains, group texts, backyard and driveway get-togethers, and video calls. As the pandemic continued, participants who delivered their babies later in the study expressed being able to create a “pandemic pod” with family members to access much needed social support. Several participants also explained the joy they felt in being able to spend more time with their families and children, and the pride they felt at being able to take care of themselves and their families through everything. Although only a few participants reported seeking out additional mental health support in the survey, most reported talking with their medical health care providers as a way to gain more information, which gave them peace of mind.
One of the limitations to this study was lack of diversity among the participants’ self-identified race and ethnicity, education, and income level. Additionally, since we recruited participants from a larger study, we only approached those originally enrolled in the MINT study rather than recruiting with the goal of saturation or phenomenological discovery. Further, the small sample size of this study limits the statistical analyses appropriate for our quantitative data, and although more participants were subsequently enrolled in MINT after the pandemic, they were not pregnant or early postpartum during the early stages of the pandemic so they could not be included in this mixed-methods report. Despite these limitations, this is the first mixed-methods report of the general impacts the COVID-19 pandemic had on pregnant and postpartum individuals’ daily lives and health behaviors in addition to their mental health. Follow-up interviews with some participants also provided insights into how participants adapted to the pandemic over time and as they transitioned from pregnancy to postpartum; yet, longer-term follow up about these experiences was not feasible once in person research activities were resumed.
Conclusions
The COVID-19 pandemic had an evolving impact on pregnant people before and after delivery. While participants reported predictable changes to their daily lives and health behaviors due to pandemic-related restrictions and global supply chain shortages, the breadth and depth of pandemic impacts on their mental health and daily lives were significant. Almost all participants reported decreased access to care and support during their pregnancies and postpartum. These findings suggest that while pandemic precautions are vital to fight disease spread and sustain the public’s health, efforts must also be made to assure that the most vulnerable groups maintain their access to health care systems that provide, at minimum, the standard of care, but ideally an increased support structure that helps them address additional stressors presented by pandemic, or other emergency situations.
Our results highlight specific areas for improvement or future intervention by medical and mental health care providers working to care for pregnant and postpartum people and expand access to care, particularly during pandemic and other emergency situations. For example, medical and mental health care professionals offering supplemental resources and care, in addition to standard-of-care practices, represent an ideal intervention to boost patient resiliency before mental health declines. Additionally, and consistent with other researchers [49], the authors recommend providers share individualized, evidence-based information, resources, and support in a clear and transparent way. However, to avoid provider burnout, appropriate resources need to be made available in terms of staffing and funding to assure mothers and babies receive the above and beyond support they need during times of hardship to achieve positive health outcomes. Recently, postpartum Medicaid coverage was expanded to 12-months in Texas, indicating that policy is moving in the right direction to support postpartum health and well-being [50].
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to thank our participants, and our community partners who supported recruiting, including CommUnityCare, People’s Community Clinic, St. David’s Healthcare and Ascension Seton and UT Health Austin. We also would like to thank Lauren DeMasie, Haley Etzler, and Inaara Aly for their assistance with transcribing.
Author contributions
SD and EW conceptualized this study. EW obtained funding and is PI of the observational study. SD, JG, GD collected data. SD, MA, JG, EW analyzed data and wrote the paper. MLW, MJG, LGK and DJ provided input on data interpretation and provided major input on the manuscript. All authors read and approved the final manuscript.
Data availability
Data cannot be shared publicly because of the agreement to which the participants consented. The quantitative data described in the manuscript will be made available upon reasonable request to Dr. Widen or Dr. Wright. Excerpts of our transcripts from the qualitative interviews relevant to the study have been included in the manuscript.
Declarations
Ethical approval and consent to participate
This study was approved by The University of Texas at Austin’s Office of Research Support and Compliance Institutional Review Board. Informed consent was obtained through DocuSign and verbal informed consent was confirmed prior to the collection of qualitative data.
Consent for publication
n/a.
Competing interests
The authors declare no competing interests.
Sources of support
Research activities were supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development (K99/R00 HD086304 and P2CHD042849). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Crozier SR, Robinson SM, Borland SE, Godfrey KM, Cooper C, Inskip HM. Do women change their health behaviours in pregnancy? Findings from the Southampton women’s Survey. Paediatr Perinat Epidemiol. 2009;23(5):446–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Versele V, Stas L, Aerenhouts D, Deliens T, Matthys C, Gucciardo L, et al. Dietary intake, physical activity and sedentary behavior and association with BMI during the transition to parenthood: a prospective dyadic study. Front Public Health. 2023;11:1092843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Corder K, Winpenny EM, Foubister C, Guagliano JM, Hartwig XM, Love R, et al. Becoming a parent: a systematic review and meta-analysis of changes in BMI, diet, and physical activity. Obes Rev. 2020;21(4):e12959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van den Bergh BRH, van den Heuvel MI, Lahti M, Braeken M, de Rooij SR, Entringer S, et al. Prenatal developmental origins of behavior and mental health: the influence of maternal stress in pregnancy. Neurosci Biobehavioral Reviews. 2020;117:26–64. [DOI] [PubMed] [Google Scholar]
- 5.Raphael-Leff J. The psychological processes of childbearing. Routledge; 2018.
- 6.Walder DJ, Laplante DP, Sousa-Pires A, Veru F, Brunet A, King S. Prenatal maternal stress predicts autism traits in 6½ year-old children: Project Ice Storm. Psychiatry Res. 2014;219(2):353–60. [DOI] [PubMed] [Google Scholar]
- 7.Lederman SA, Rauh V, Weiss L, Stein JL, Hoepner LA, Becker M, Perera FP. The effects of the World Trade Center event on birth outcomes among term deliveries at Three Lower Manhattan Hospitals. Environ Health Perspect. 2004;112(17):1772–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prevention CfDCa. CDC Museum COVID-19 Timeline: David J, Sencer CDC. Museum; 2022 [ https://www.cdc.gov/museum/timeline/covid19.html
- 9.Wang CL, Liu YY, Wu CH, Wang CY, Wang CH, Long CY. Impact of COVID-19 on pregnancy. Int J Med Sci. 2021;18(3):763–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Racine N, Eirich R, Cooke J, Zhu J, Pador P, Dunnewold N, Madigan S. When the Bough breaks: a systematic review and meta-analysis of mental health symptoms in mothers of young children during the COVID-19 pandemic. Infant Ment Health J. 2022;43(1):36–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Altman MR, Gavin AR, Eagen-Torkko MK, Kantrowitz-Gordon I, Khosa RM, Mohammed SA. Where the System failed: the COVID-19 Pandemic’s impact on pregnancy and birth care. Glob Qual Nurs Res. 2021;8:23333936211006397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Linden K, Domgren N, Zaigham M, Sengpiel V, Andersson ME, Wessberg A. Being in the shadow of the unknown - Swedish women’s lived experiences of pregnancy during the COVID-19 pandemic, a phenomenological study. Women Birth. 2022;35(5):440–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keating NE, Dempsey B, Corcoran S, McAuliffe FM, Lalor J, Higgins MF. Women’s experience of pregnancy and birth during the COVID-19 pandemic: a qualitative study. Ir J Med Sci. 2022;191(5):2177–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davis NL, Smoots AN, Goodman DA. Pregnancy-Related Deaths: Data from 14 U.S. Maternal Mortality Review Committees, 2008–2017. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2019.
- 15.Commission THaHS. State efforts to address Postpartum Depression, maternal mortality and morbidity in Texas. Austin, TX: Texas Health and Human Services; 2020. [Google Scholar]
- 16.Bauman BL, Ko JY, Cox S, D’Angelo Mph DV, Warner L, Folger S, et al. Vital signs: Postpartum depressive symptoms and provider discussions about Perinatal Depression - United States, 2018. MMWR Morb Mortal Wkly Rep. 2020;69(19):575–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Services TDSH. Texas Health Data Austin, Texas: Texas Department of State Health Services; 2024 [Available from: healthdata.dshs.texas.gov/dashboard/maternal-and-child-health/maternal-health/maternal-health
- 18.Coelho CM, Suttiwan P, Arato N, Zsido AN. On the nature of fear and anxiety triggered by COVID-19. Front Psychol. 2020;11:581314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moyer CA, Compton SD, Kaselitz E, Muzik M. Pregnancy-related anxiety during COVID-19: a nationwide survey of 2740 pregnant women. Arch Womens Ment Health. 2020;23(6):757–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Güner Ö, Öztürk R. Psychological and social impact and lifestyle changes among pregnant women of COVID-19 pandemic: a qualitative study. Arch Psychiatr Nurs. 2022;36:70–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aydin R, Aktaş S. An investigation of women’s pregnancy experiences during the COVID-19 pandemic: a qualitative study. Int J Clin Pract. 2021;75(9):e14418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moltrecht B, Dalton LJ, Hanna JR, Law C, Rapa E. Young parents’ experiences of pregnancy and parenting during the COVID-19 pandemic: a qualitative study in the United Kingdom. BMC Public Health. 2022;22(1):523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Services THaH. Maternal Depression Strategic Plan Update for Fiscal Years 2021–2025. Austin, TX: Texas Health and Human Services; 2021. [Google Scholar]
- 24.Thayer ZM, Gildner TE. COVID-19-related financial stress associated with higher likelihood of depression among pregnant women living in the United States. Am J Hum Biol. 2021;33(3):e23508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lebel C, MacKinnon A, Bagshawe M, Tomfohr-Madsen L, Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord. 2020;277:5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davenport MH, Meyer S, Meah VL, Strynadka MC, Khurana R. Moms are not OK: COVID-19 and maternal Mental Health. Front Glob Womens Health. 2020;1:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Preis H, Mahaffey B, Lobel M. The role of pandemic-related pregnancy stress in preference for community birth during the beginning of the COVID-19 pandemic in the United States. Birth. 2021;48(2):242–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Preis H, Mahaffey B, Heiselman C, Lobel M. Vulnerability and resilience to pandemic-related stress among U.S. women pregnant at the start of the COVID-19 pandemic. Soc Sci Med. 2020;266:113348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Atmuri K, Sarkar M, Obudu E, Kumar A. Perspectives of pregnant women during the COVID-19 pandemic: a qualitative study. Women Birth. 2022;35(3):280–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McKinlay AR, Fancourt D, Burton A. Factors affecting the mental health of pregnant women using UK maternity services during the COVID-19 pandemic: a qualitative interview study. BMC Pregnancy Childbirth. 2022;22(1):313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goyal D, Han M, Feldman-Schwartz T, Le HN. Perinatal experiences of Asian American women during COVID-19. MCN Am J Matern Child Nurs. 2022;47(2):71–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saleh L, Canclini S, Greer K, Mathison C, Combs SM, Dickerson B, Collins K. Mothers’ experiences of pregnancy, Labor and Birth, and Postpartum during COVID-19 in the United States: preliminary results of a mixed-methods study. J Perinat Neonatal Nurs. 2022;36(1):55–67. [DOI] [PubMed] [Google Scholar]
- 33.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983:385–96. [PubMed]
- 34.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194–200. [DOI] [PubMed] [Google Scholar]
- 35.Association AP. APA Stress in America survey. 2019.
- 36.Bryant RA, Friedman MJ, Spiegel D, Ursano R, Strain J. A review of acute stress disorder in DSM-5. Focus. 2011;9(3):335–50. [DOI] [PubMed] [Google Scholar]
- 37.Cardeña E, Koopman C, Classen C, Waelde LC, Spiegel D. Psychometric properties of the Stanford Acute stress reaction questionnaire (SASRQ): a valid and reliable measure of acute stress. J Trauma Stress. 2000;13(4):719–34. [DOI] [PubMed] [Google Scholar]
- 38.Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. J Health Soc Behav. 1981:337–56. [PubMed]
- 39.Okechukwu CA, El Ayadi AM, Tamers SL, Sabbath EL, Berkman L. Household food insufficiency, financial strain, work–family spillover, and depressive symptoms in the working class: the work, family, and health network study. Am J Public Health. 2012;102(1):126–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grounded theory in practice. Strauss AL, Corbin JM, editors. Thousand Oaks, CA, US: Sage Publications, Inc. 1997. viii, 280-viii, p.
- 41.Chun Tie Y, Birks M, Francis K. Grounded theory research: a design framework for novice researchers. SAGE Open Med. 2019;7:2050312118822927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kinser P, Jallo N, Moyer S, Weinstock M, Barrett D, Mughal N, et al. It’s always hard being a mom, but the pandemic has made everything harder: a qualitative exploration of the experiences of perinatal women during the COVID-19 pandemic. Midwifery. 2022;109:103313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Farrell R, Collart C, Craighead C, Pierce M, Chien E, Frankel R, et al. The successes and challenges of implementing Telehealth for Diverse patient populations requiring prenatal care during COVID-19: qualitative study. JMIR Form Res. 2022;6(3):e32791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Morgan A, Goodman D, Vinagolu-Baur J, Cass I. Prenatal telemedicine during COVID-19: patterns of use and barriers to access. JAMIA Open. 2022;5(1). [DOI] [PMC free article] [PubMed]
- 45.Craighead CG, Collart C, Frankel R, Rose S, Misra-Hebert AD, Tucker Edmonds B, et al. Impact of Telehealth on the delivery of prenatal care during the COVID-19 pandemic: mixed methods study of the Barriers and Opportunities To Improve Health Care Communication in discussions about pregnancy and prenatal genetic testing. JMIR Form Res. 2022;6(12):e38821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chenarides L, Grebitus C, Lusk JL, Printezis I. Food consumption behavior during the COVID-19 pandemic. Agribusiness (N Y N Y). 2021;37(1):44–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Janssen M, Chang BPI, Hristov H, Pravst I, Profeta A, Millard J. Changes in Food Consumption during the COVID-19 pandemic: analysis of consumer Survey Data from the First Lockdown Period in Denmark, Germany, and Slovenia. Front Nutr. 2021;8:635859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mirzakhani K, Shoorab NJ, Akbari A, Khadivzadeh T. High-risk pregnant women’s experiences of the receiving prenatal care in COVID-19 pandemic: a qualitative study. BMC Pregnancy Childbirth. 2022;22(1):363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cole C, Tsakiroglou M, Waitt C. Communication is crucial: lessons from COVID-19 vaccination and pregnancy. Br J Clin Pharmacol. 2023;89(2):582–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Texas Extends Postpartum Coverage For Medicaid. CHIP recipients [press release]. Volume 28. Austin, Texas; 2024. p. 2024.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data cannot be shared publicly because of the agreement to which the participants consented. The quantitative data described in the manuscript will be made available upon reasonable request to Dr. Widen or Dr. Wright. Excerpts of our transcripts from the qualitative interviews relevant to the study have been included in the manuscript.