Abstract
Backgound
Preformed metal crowns (PMCs) and zirconia crowns (ZCs) are commonly used for the treatment of primary molar caries. However, there have been no reports on factors influencing parental awareness, willingness to use these treatments, and the associated discomfort after crown placement in children.This study is the first to report factors influencing preformed crowns, providing a reference for the prevention and treatment of deciduous carious teeth.
Methods
Parents whose children’s posterior caries were restored with preformed crowns at Shenzhen Children’s Hospital from October 2021 to October 2023 were recruited. A questionnaire gathered data on multiple variables, including basic information about the participants, their oral health behaviors, and their attitudes toward oral health.
Results
Approximately two-thirds of the surveyed parents were aware of preformed metal crowns (PMCs) (67.8%), whereas over half were hardly aware of prefabricated zirconia crowns (ZCs) (59.6%). In terms of discomfort symptoms, 105 (76.7%) and 102 (76.1%) cases were reported after PMC and ZC placement respectively; however, there was no statistically significant difference between the two groups (P > 0.05). Among the surveyed parents, 19 (8.7%) expressed that they could not accept the PMC color, whereas all could accept the ZC color, and the difference was statistically significant (P < 0.05). A total of 217 parents (99.5%) could accept PMCs to protect or repair primary carious teeth; 29.8% of the parents stated that they were reluctant to use ZCs to protect or repair their children’s deciduous teeth, and the difference was significant (P < 0.05). In terms of location selection, the majority of surveyed parents chose comprehensive hospitals (58.7%) and stomatological hospitals (41.3%). In terms of institution selection, priority was given to the doctor’s qualifications (90.4%). Pearson correlation analysis revealed that “acceptance of the PMC color”, “oral health awareness”, and “parental willingness to use PMCs” were positively correlated (P < 0.05) and that “non-nuclear family status” was negatively related to “parental willingness to use PMCs” (P < 0.05). The logistic multiple regression analysis revealed that oral health awareness and restoration awareness significantly affected the duration of discomfort symptoms after PMC placement (P < 0.15). Children with higher annual family incomes, families with fewer children, lower consumption of desserts, better oral health awareness, and teeth brushing under the assistance of their parents showed a dramatic decline in untimely PMC repair (P < 0.15); children who brushed their teeth less and whose parents had a poorer perception of restoration methods showed an increase in untimely PMC repair (P < 0.15).
Conclusions
This discrepancy is reflected in the cognition and willingness to use PMCs and ZCs. PMCs are more accepted due to cost, whereas ZCs are preferred for aesthetics. The factors affecting PMC restoration are oral health awareness, manner of restoration, family income, number of children, consumption of desserts, and toothbrushing frequency.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12903-024-05391-3.
Keywords: Metal preformed crown, Ceramic prefabricated crown, Influencing factors
Introduction
Dental caries is the most common chronic infectious childhood disease and is characterized by a high prevalence and a low consultation rate [1]. According to the Chinese Fourth National Oral Health Epidemiological Survey, the incidence of caries in 5-year-old children was 70.9%, with a rise of 5.8% during the last decade. Approximately 62.68% of primary caries occur in molar teeth [2]. Once treatment management is postponed or delayed, cavitated lesions quickly develop pulpitis or apical periodontitis and even increase the risk of systemic diseases such as Henoch–Schonlein purpura and rheumatic fever [3]. On the one hand, more cavitated lesions or early loss could reduce masticatory function, hinder digestive assimilation, increase the risk of malnutrition and have negative effects on normal growth and development [4]. On the other hand, once the caries involve the proximal surfaces, the natural primary dentition may be broken, and the occlusal height may be sabotaged, which may lead to abnormal maxillofacial growth and development, further affecting children’s aesthetics and psychological health [5]. Therefore, strategic management of caries should be implemented in a timely, persistent and effective manner to promote children’s oral health-related quality of life (OHRQoL).
Drug and restorative treatment are the mainstream methods used in pediatric restorative dentistry [6]. However, the former can provide prevention rather than restore tooth shape, and few dental practitioners use it in clinical practice [7]. Conventional filling materials (such as amalgams, composites, glass ionomers, resin-modified glass ionomers and compomers) are commonly used to restore cavitated teeth. However, filling materials probably fail in a short period. Hence, preformed crowns, as a reliable restorative selection for decayed teeth, are gradually replacing traditional treatments [8].
The American Academy of Pediatric Dentistry (AAPD) guidelines recommend [9] that preformed metal crowns (PMCs) are suitable for all kinds of decayed teeth and have a high survival rate. PMC is a preformed stainless-steel full crown that fits closely to the tooth. In China [10, 11], PMC utilization in Chengdu and Xi’an exceeds 50.0%, with 20% in Wuhan and approximately 5.5% in Shanghai. However, the application rate of PMCs is less than 5% in Shenzhen. Another survey of 3-year-old children in Shenzhen revealed that more than 95% of dental caries were not effectively treated [12], and the low treatment efficacy in children was correlated with a low utilization rate of PMC. The medical resources and number of tertiary hospitals in Shenzhen are far fewer than those in similar large cities such as Beijing, Shanghai, and Guangzhou, and the capability of primary health care services is also limited. In terms of dental medical services, there is a serious shortage of dental institutions and dental staff in Shenzhen. On average, nearly 20,000 people have only one dentist, and the scarcity of pediatric dentists is especially conspicuous, which makes it difficult to guarantee the pediatric need. In Europe and the United States, the incidence of PMCs has increased in recent years, and PMCs have become a routine clinical treatment. In the United States, the use of PMCs can reach 80%. Several studies have confirmed that PMCs are clinically effective in treating primary molars, protecting teeth and prolonging their survival time. In terms of safety, through a randomized clinical trial, Kodaira et al. [13] reported in a randomized clinical trial that the level of the metal element chromium (Cr), an important component of preformed crowns in hair, was greater in the PMC group than in the control group, but there were no significant differences in the Fe or Ni levels. The levels of the trace elements Ni, Cr, and Fe were within allowable ranges, indicating that these minerals are unlikely to be harmful and could be safe to use. PMC is a convenient and economical option to achieve esthetic, healthy, and functional results while restoring primary teeth [14–16]. However, PMCs have a nonaesthetic appearance and have become a point of concern.
Recently, prefabricated zirconia crowns have been gradually used as aesthetic restorative materials for primary teeth. NuSmile® zirconia crowns (ZCs), a type of prefabricated ceramic crown, have been extensively used to restore cativated teeth. Owing to their delicate nature, replicating aesthetics, ultimate durability, and convenient placement, ZCs have become silver bullets. The clinical outcomes of the ZCs were comparable to those of the other crowns. ZCs could be a choice for aesthetic purposes, with the disadvantage of a relatively high cost [17]. The zirconia crown is a new method for restoring primary teeth that may be commonly applied in clinical practice [18, 19]. Gingival health and plaque accumulation were better after ZC repair than after PMC repair. A prospective clinical trial including 136 children with early childhood caries aged 36–71 months who were assigned to the ZC and resin-bonded composite strip crown groups concluded that preschool children with OHRQOL treated with ZC were significantly better than those who received RCSC [20].
PMCs and ZCs are commonly used for the treatment of primary molar caries. The choice of restoration method can ensure reliable efficacy and reduce the impact on periodontal health, which is the focus of pediatric dentists. However, there have been no reports on factors influencing parental awareness, willingness to use these treatments, and the associated discomfort after crown placement in children. Therefore, this study is the first to report factors influencing preformed crowns, providing a reference for the prevention and treatment of deciduous carious teeth.
The null hypothesis was that there would be no significant difference in the relevant factors affecting symptoms of discomfort between PMCs and ZCs.
Objects and methods
Subjects
Parents whose children underwent dental carious restoration via PMCs and ZCs at Shenzhen Children’s Hospital from October 2021 to October 2023 were included as subjects. A total of 233 parents completed the questionnaire, and after collection, the questionnaires were coded and invalidated. The study protocol was reviewed and approved by the Shenzhen Children’s Hospital ethics committee [Project No. 202312] and conformed to the ethical standards for medical research involving human subjects, as laid out in the 1964 Declaration of Helsinki and its later amendments. The participants, including children and their guardians, provided written informed consent prior to taking part in the study.
Questionnaire survey
The questionnaire survey for this study was based on the lifestyle and dietary habits of the children, as well as parental perceptions of preformed crown restorations. The questionnaires were ultimately designed according to the purposes of this study and the suggestions of pediatric dental experts as follows: ① parents’ basic information, such as their date of birth, education level, family income, family member, etc.; ② children’s oral health behaviors, including toothbrushing frequency, consumption of desserts, frequency of receiving oral health education, etc.; and ③ parents’ attitudes toward oral health, including their understanding of oral health knowledge and preformed crowns, and concerns about preformed crown restoration treatment.
Questionnaire quality control
The questionnaire was completed by the child’s primary guardian. Before the electronic questionnaire was distributed, the researcher informed each parent of the requirements and standards and collected the questionnaire within 48 h after allocation. After a questionnaire was returned, the investigators first screened it according to the completion time. According to the calculations of the questionnaire designer, questionnaires that took less than 120 s to complete were considered invalid. If parents completed the questionnaires more than two times, the last questionnaire completed was adopted. After the questionnaire was collected, the original data were checked and verified item by item. Any questionnaire that did not match the original data was removed, and the remaining questionnaires were considered valid and included in this study.
Statistical analysis
The data were analyzed via SPSS version 26.0 for Windows (SPSS Inc., Chicago, IL, USA). Continuous variables with a normal distribution are presented as the means ± standard deviations (SDs); nonnormal variables are reported as medians (interquartile ranges). Count data are represented by n (%). Independent sample t tests or analyses of variance were used for normally distributed variables, chi square tests were used for intergroup comparisons of binary and unordered multiclass variables, and Kruskal‒Wallis tests were applied to intergroup nonparametric rank sum tests for ordered categorical variables and nonnormally distributed continuous variables. Logistic multiple regression analyses were used to identify the relevant factors affecting symptoms of discomfort. Pearson correlation analyses of factors affecting the willingness to use preformed crowns were performed. A value of P < 0.05 was considered significant.
Results
Basic information
A total of 233 questionnaires were included in this study. After the check, 15 questionnaires were excluded, and 218 were valid, for an effective response rate of 93.56%.
A total of 218 surveyed parents were enrolled, including 37 males (16.9%) and 181 females (83%). The average age was 36.75 ± 4.50 years (males: 38.52 ± 7.47 years; females: 34.84 ± 5.80 years). Among the surveyed population, the majority of the parents had an undergraduate education (70.1%), followed by a high school education (12.8%) and a master’s degree or above (10.5%). The annual income of most surveyed households ranged from 250,000 to 300,000 ¥ (24.7%) and 100,000 to 150,000 ¥ (21.1%), followed by 150,000 to 200,000 ¥ (15.6%) and no more than 100,000 ¥ (14.7%). The sample mainly consisted of nuclear families (88.5%) with 1–2 children (94.9%).
Oral health-related behaviors and attitudes
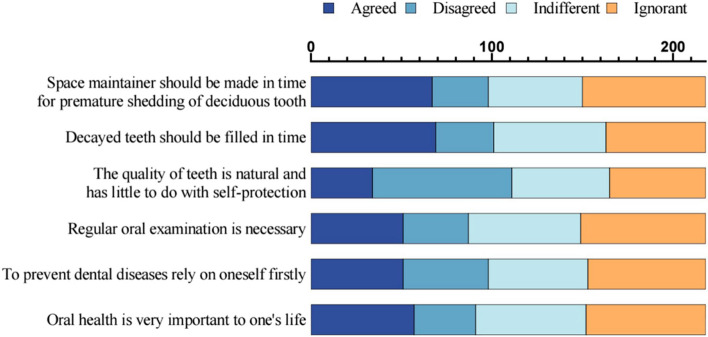
Among the surveyed population, children brushed their teeth twice a day at most. Parents help their children brush their teeth more often. Most children use fluoride toothpaste to brush their teeth. The children ate sweet Dim sum and sweet drinks once per day at most. More than 70% of the children had received oral health education at school. See Table 1 for details. In terms of parents’ attitudes toward oral health, there were 6 items, with 1 point given for each correct answer and a total possible score of 6 points. The higher the score was, the better the knowledge that was mastered. The results revealed that the overall oral health awareness rate among parents was relatively low, as shown in Fig. 1.
Table 1.
Oral health-related behaviors of the surveyed children
| Entry | Number of people | Percentage(%) | Entry | Number of people | Percentage(%) |
|---|---|---|---|---|---|
| Tooth brushing times per day | 1 per week | 42 | 19.2 | ||
| 0 | 0 | 0 | 1 ~ 2 per month | 31 | 14.2 |
| 1 | 58 | 26.6 | Rarely/never | 28 | 12.8 |
| 2 | 160 | 73.3 | How many times do your children drink sweet beverages per day? | ||
| Do you help your children with tooth brushing? | ≥ 2 per day | 23 | 10.6 | ||
| Yes | 112 | 51.3 | 1 times per day | 53 | 24.3 |
| No | 106 | 48.6 | 2 ~ 6 times per week | 45 | 20.6 |
| Do your children use fluoride toothpaste when brushing their teeth? | 1 time per week | 33 | 15.1 | ||
| Yes | 145 | 66.5 | 1 ~ 2 per month | 33 | 15.1 |
| No | 45 | 20.6 | Rarely/never | 31 | 14.2 |
| No Clue | 28 | 12.8 | Last semester, how many times did your children attended classes on oral health at school? | ||
| How many times do your children eat sweets per day? | 1 time | 63 | 28.9 | ||
| ≥ 2 times per day | 23 | 10.6 | 2 times | 57 | 26.1 |
| 1 time per day | 67 | 30.7 | >2 times | 31 | 14.2 |
| 2 ~ 6 times per week | 27 | 12.4 | No Clue | 67 | 30.7 |
Fig. 1.
Parental attitudes toward oral health
Understanding of prefabricated crowns
Most parents had knowledge of PMCs (67.8%), whereas more than half had little knowledge of ZCs (59.6%). The people who had a preliminary understanding of ZCs accounted for 35.8% of the sample. The difference between understanding PMCs and ZCs was statistically significant (χ2 = 13.472, P = 0.009). The respondents heard of PMC restoration through doctors (86.6%) and acquaintances (71.5%), whereas the respondents were aware of ZC restoration from doctors (83.5%), followed by acquaintances (66.5%) and online channels (51.4%). With respect to preformed crown restoration of deciduous carious defects, most parents believed that preformed crowns could restore the tooth shape and chewing function (85.3%), followed by preventing caries, protecting primary teeth (62.8%), serving as a retainer for tooth gaps (52.7%), facilitating the eruption of permanent teeth, and reducing the occurrence of malocclusion (46.8%).
The willingness to use preformed crowns among the respondents
The results revealed that 74 parents (54%) reported that their children experienced symptoms of discomfort that persisted for less than 1 week, 31 (22.6%) reported that their children experienced symptoms of discomfort that persisted for more than 1 week, and 32 (23.3%) reported that their children experienced no symptoms of discomfort. A total of 72 (53.6%) parents reported that their children experienced symptoms of discomfort that persisted for less than 1 week, 30 (22.4%) reported that their children experienced symptoms of discomfort that persisted for more than 1 week, and 32 (23.9%) reported that their children experienced no symptoms of discomfort. There was no statistically significant difference between the two groups (P > 0.05) (Table 2), and the symptoms of discomfort disappeared within 2 weeks. Most parents believed that after preformed crown restoration, it was necessary to brush their teeth twice a day (100%), visit the hospital regularly (84.8%), and avoid eating too sticky or hard food (65.6%) to maintain their children’s oral hygiene. Second, the parents believed that the habits of using dental floss for cleaning teeth (57.8%) and regularly brushing teeth (36.2%) should be developed. Among the surveyed parents, 19 (8.7%) expressed that they could not accept the PMC color, and the parents were more willing to consider the ZC color (P < 0.05). A total of 217 parents (99.5%) were able to “accept the use of PMCs to protect or repair deciduous teeth”; 29.8% of the parents expressed a reluctance to use ZCs to protect or repair primary teeth, and their willingness to use PMCs was greater than that of ZCs, with a statistically significant difference (P < 0.05). However, all the respondents reached a consensus on the willingness to recommend PMCs and ZCs to others.
Table 2.
The acceptance of preformed crowns by surveyed parents
| Entry | PMCs(%) | ZCs(%) | χ2 | P |
|---|---|---|---|---|
| How did does your child experience discomfort symptoms after wearing a preformed crown? | ||||
| 1 ~ 3 Days | 40(29.2) | 43(32.0) | 0.989 | 0.804 |
| 4 ~ 7 Days | 34(24.8) | 29(21.6) | ||
| 1 ~ 2 Weeks | 31(22.6) | 30(22.4) | ||
| >2 Weeks | 0(0) | 0(0) | ||
| No discomfort | 32(23.3 | 32(23.9) | ||
| Can you accept the color of the preformed crown? | ||||
| Yes | 105(48.2) | 128(58.7) | 7.443 | 0.024 |
| Reluctantly yes | 94(43.1) | 90(41.3) | ||
| No | 19(8.7) | 0(0) | ||
| Do you accept the use of preformed crowns for the protection or restoration of deciduous teeth? | ||||
| Absolutely yes | 81(37.1) | 7(3.2) | 17.142 | 0.047 |
| Willingly yes | 59(27.0) | 59(27.0) | ||
| Yes | 77(35.2) | 87(39.9) | ||
| Not very much | 1(0.5) | 65(29.8) | ||
| No | 0(0) | 0(0) | ||
| Would you be willing to recommend preformed crowns for deciduous tooth repair to others? | ||||
| Very much | 137(62.8) | 93(42.6) | 0.168 | 0.682 |
| Yes | 81(37.1) | 125(57.3) | ||
| No | 0(0) | 0(0) | ||
After the PMCs were restored, parents were accustomed to focusing on aesthetics (81.2%), pain and discomfort (89.4%), safety of the materials (77.5%) and tooth development (72.9%). However, after wearing ZC restorations, parents usually emphasized expensive prices (38.1%), tooth development (63.7%), pain and discomfort (61.9%), and material security (56.8%).
In terms of the choice of treatment institution, the respondents preferred comprehensive hospitals (58.7%) and stomatological hospitals (41.3%). In terms of choosing medical qualifications, the priority selection was doctor titles (90.4%), followed by the success rate of treatment (68.4%), registration difficulties and consultation time with doctors (67.0%), hospital/clinic reputation (62.8%), and hospital/clinic comfort (61.4%).
Analysis of factors related to the duration of discomfort after preformed crown repair
The duration of discomfort after PMC repair was used as the dependent variable, and a forward stepwise regression analysis method was used to regress the data. First, reasonable values were assigned to each influencing factor based on the different types of data, as shown in Table 3. The significance level was set to 0.15 to improve the level of fit, and logistic multiple regression analysis was conducted. The results are shown in Table 4. In the model comparison of discomfort symptom durations of “4 ~ 7 days”, “1 ~ 2 weeks” and “1 ~ 3 days”, family income, number of children in the family, toothbrush frequency, parental assistance in tooth brushing, sweet dim sum consumption, oral health awareness, and awareness of repair methods had significant effects on the duration of discomfort symptoms after PMC repair (P < 0.15). Children with higher annual family incomes, fewer children, lower consumption of desserts, better oral health awareness, and teeth brushing under the assistance of their parents showed a dramatic decline in untimely PMC repair (P < 0.15); children who brushed their teeth less and whose parents had a poorer perception of restoration methods showed an increase in untimely PMC repair (P < 0.15). When the same analysis method was used to analyze the duration of discomfort after ZC repair, the abovementioned variables had no significant impact (P > 0.15).
Table 3.
Multiple regression variables and assignment
| Variables | Assignment |
|---|---|
| Annual revenue for family (thousands) | 1 = < 50; =2 = 50 ~ 100; 3 = 100 ~ 150; 4=150 ~ 200; 5=200 ~ 250; 6=250 ~ 300; 7=300 ~ 350; 8=350 ~ 400; 9=400 ~ 450; 10=450 ~ 500; 11=> 500 |
| Number of children | 1=1; 2=2; 3=3 |
| Number of tooth brushing sessions | 1=0; 2=1; 3=2 |
| Parents helping children with tooth brushing | 1=Yes; 0=No ; |
| Children’s consumption of sweets | 0=Rarely/never; 1=1 ~ 2 times per month; 2=1 time per week; 3=2 ~ 6 times per week; 4=1 time per day; 5=≥ 2 times per day; |
| Understanding of oral health | 1 ~ 6, The higher the score, the better they understand |
| Understanding of methods of restoration | 1=No understanding; 2=Basic understanding; 3=Understand a lot |
Table 4.
Logistic multiple regression analysis of the factors influencing the duration of discomfort after the use of metal prefabricated crowns
| Time for discomforta | 4 ~ 7 Days | 1 ~ 2 Weeks | No discomfort | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| B | Sig. | Exp(B) | B | Sig. | Exp(B) | B | Sig. | Exp(B) | ||
| Annual revenue for family (thousands) | < 10 | 50.728 | 0.997 | 1.074E + 22 | −18.127 | . | 1.341E-8 | 53.783 | . | 2.279E + 23 |
| 10–15 | −6.897 | 1.000 | 0.001 | −81.019 | 0.065* | 6.512E-36 | −4.545 | 1.000 | 0.011 | |
| 15–20 | −27.662 | 0.998 | 9.694E-13 | −98.853 | 0.055* | 1.171E-43 | −20.958 | 0.998 | 7.907E-10 | |
| 20–25 | 18.390 | 0.999 | 97009140.006 | −43.262 | 0.985 | 1.627E-19 | 25.074 | 0.998 | 7.756E + 10 | |
| 25 ~ 30 | −5.328 | 1.000 | 0.005 | −61.042 | 0.060* | 3.087E-27 | −2.477 | 1.000 | 0.084 | |
| > 30 | 0 | . | . | 0 | . | . | 0 | . | . | |
| Number of children in the family | 1 | −16.696 | 0.040* | 5.610E-8 | −10.819 | 0.061* | 2.002E-5 | −34.035 | 0.995 | 1.654E-15 |
| 2 | −36.638 | 0.050* | 1.225E-16 | −3.796 | 0.577 | 0.022 | −47.479 | 0.992 | 2.400E-21 | |
| 3 | 0 | . | . | 0 | . | . | 0 | . | . | |
| Number of tooth brushing sessions per day | 1 | 24.512 | 0.033* | 4.422E + 10 | 38.378 | 0.046* | 4.649E + 16 | −25.488 | 0.036* | 1.173E + 11 |
| 2 | 0 | . | . | 0 | . | . | 0 | . | . | |
| Parents helping children with tooth brushing | Yes | −13.576 | 0.051* | 1.270E-6 | −2.795 | 0.336 | 0.061 | −1.446 | 0.461 | 0.235 |
| No | 0 | . | . | 0 | . | . | 0 | . | . | |
| Frequency of sweet consumption | Rarely/never | 5.474 | 0.200 | 238.472 | −24.485 | 0.074* | 2.323E-11 | −35.840 | 0.991 | 2.722E-16 |
| 1 ~ 2 times per month | −58.213 | 0.980 | 5.231E-26 | −18.038 | 0.097* | 1.466E-8 | −56.251 | 0.983 | 3.719E-25 | |
| 1 time per week | −10.934 | 0.057* | 1.783E-5 | 7.050 | 0.282 | 1152.510 | −0.970 | 0.751 | 0.379 | |
| 2 ~ 6 times per week | −46.134 | 0.057* | 9.207E-21 | −15.942 | 0.083* | 1.193E-7 | −55.624 | 0.982 | 6.960E-25 | |
| 1 time per day | −5.410 | 0.319 | 0.004 | 11.346 | 0.258 | 84629.555 | 10.993 | 0.273 | 59464.900 | |
| ≥ 2 times per day | 0 | . | . | 0 | . | . | 0 | . | . | |
| Understanding of oral health | 0 | −2.547 | 0.643 | 0.078 | −15.675 | 0.145* | 1.557E-7 | 18.999 | 0.995 | 178241676.577 |
| 1 | 7.719 | 0.070* | 2251.334 | −16.775 | 0.127* | 5.187E-8 | 34.855 | 0.991 | 1.372E + 15 | |
| 2 | 19.988 | 0.079* | 479191658.591 | −71.858 | 0.060* | 6.204E-32 | 30.136 | 0.992 | 1.225E + 13 | |
| 3 | −5.170 | 0.401 | 0.006 | −56.411 | 0.055* | 3.171E-25 | 8.647 | 0.998 | 5695.225 | |
| 4 | 56.495 | 0.993 | 3.430E + 24 | −37.110 | 0.996 | 7.642E-17 | 47.444 | 0.996 | 4.023E + 20 | |
| 5 | −15.806 | 0.998 | 1.366E-7 | −53.561 | 0.065* | 5.477E-24 | 11.179 | 0.999 | 71612.957 | |
| 6 | 0 | . | . | 0 | . | . | 0 | . | . | |
| Understanding of methods of restoration | No understanding | 7.156 | 0.170 | 1281.326 | 26.346 | 0.047* | 2.765E + 11 | 13.598 | 0.089* | 804708.324 |
| Basic understanding | 14.438 | 0.065* | 1862984.236 | −10.989 | 0.138* | 1.689E-5 | 3.530 | 0.270 | 34.128 | |
| Understand a lot | 0 | . | . | 0 | . | . | 0 | . | . | |
| ① * Indicating a significance level of 0.15; ② a. Reference category: 1~3 days | ||||||||||
Analysis of relevant factors influencing the willingness to use preformed crowns
Pearson correlation analysis (see Table 5) revealed that the correlation coefficients between “parental willingness to use PMCs” and “parental acceptance of the PMC color”, “non-nuclear family”, and “oral health awareness” were 0.139, −0.149, and 0.143, respectively. “Parental acceptance of PMC color”, “oral health awareness”, and “parental willingness to use PMCs” were positively correlated (P < 0.05), and “non-nuclear family” was negatively correlated with “parental acceptance of PMC color” (P < 0.05), indicating that parents with high acceptance of PMC color, good oral health awareness, and a nuclear family have a stronger willingness to use PMCs.
Table 5.
Analysis of the willingness and factors influencing the use of preformed crowns
| Group | PMCs | ZCs | ||
|---|---|---|---|---|
| r | P | r | P | |
| Age | −0.118 | 0.082 | −0.70 | 0.303 |
| Education level | −0.011 | 0.872 | −0.55 | 0.423 |
| Annual family revenue | 0.042 | 0.542 | 0.024 | 0.730 |
| Acceptance of the color of preformed crowns | 0.139 | 0.041 | 0.027 | 0.697 |
| Number of children in the family | 0.002 | 0.976 | 0.089 | −0.189 |
| Family status(nonnuclear family) | −0.149 | 0.028 | −0.042 | 0.540 |
| Understanding of oral health | 0.143 | 0.034 | 0.038 | 0.572 |
Discussion
This study is the first to report factors influencing preformed metal crowns and prefabricated Zcrconia crowns, and 218 respondents completed the questionnaire survey. According to the findings, children with higher annual family income, fewer children in the family, lower consumption of desserts, better oral health awareness and tooth brushing with the assistance of parents experienced a shorter duration of discomfort symptoms after PMC restoration, whereas children who brushed their teeth less and whose parents had a poorer understanding of restoration manners lasted for a longer duration of discomfort symptoms after PMC repair.
In this study, there was no significant difference in symptoms of discomfort after treatment between PMCs and ZCs, which was inconsistent with the findings of other studies. Innes NP et al. and Duggal M et al. reported that discomfort was related to the restoration technique; that is, crowns fitted via the Hall technique may reduce discomfort at the time of treatment compared with filling [9, 21]. The majority of discomfort symptoms presumably came from local gum damage or slight compression of the crown margin, and exotic sensations and swelling discomfort resolved spontaneously within one week. The parents’ willingness seems to be an indispensable factor in choosing repair restoration materials. In this study, the respondents showed a stronger willingness to use PMCs than ZCs did; over 90% of them stated that they were reluctant to use ZCs owing to the high price in Shenzhen, which was also different from other countries or states. Researchers have reported that, compared with PMCs, parents are more satisfied with ZCs because of their aesthetic appearance and only minor color differences with adjacent teeth [22].
In addition, this study revealed that factors such as non-nuclear families and the level of oral health awareness also affected parental willingness to use PMCs. Oral health knowledge is the cornerstone for maintaining children’s oral health. Parents who had more oral health awareness were more willing to select PMCs. This was probably because these people were aware of the importance of their teeth and tended to accept appropriate treatment strategies when oral health problems occurred, which was similar to the findings of other studies [23, 24]. Compared with those in non-nuclear families, parents in nuclear families have higher education levels, better oral health awareness, greater willingness to use preformed crowns, and better maintenance behavior after treatment, increasing parents’ knowledge, attitudes, and behaviors [25], thereby promoting the application of preformed crowns in posterior-cativated defects.
Baldani [26] reported that children from high-income families had to seek dental treatment five times more often than those from low-income families did; however, this survey revealed that there was no significant difference in household income among respondents who selected preformed crowns. Family income may affect discomfort after crown restoration rather than parental willingness. The reason is likely that China is in the development stage, and there are no correlations among family income, education level or social level. Moreover, the parents in this study had higher education and economic status and paid more attention to investing in the oral health industry.
Promoting oriented prevention strategies such as oral health awareness can enhance correct oral health behaviors and reduce the incidence of dental caries in children [27]. This study revealed that the main means for parents to acquire oral health knowledge were through dentists, acquaintances, the internet and transportation billboards. Therefore, a series of methods should spare no efforts to conduct propaganda on preformed crowns, including the Dental Association website, official accounts, online television, public welfare courses and hospital bulletin boards, thereby heightening the public’s awareness of children’s oral health, oral health habits and correct use of preformed crowns.
Conclusions
The study revealed that PMCs are more accepted due to cost, whereas ZCs are preferred for aesthetics, highlighting important trade-offs in clinical decision-making. Parents are prone to select PMCs for primary decayed teeth in Shenzhen city, which is more cost-effective and more widely recognized than zirconia crowns, which are relatively expensive and have a low reputation. Cognitive factors such as oral health, type of restoration, family income, number of family children, frequency of desserts, tooth-brushing frequency and tooth-brushing under the survival of parents significantly influence the clinical effectiveness of preformed crown restorations. The results may help practitioners choose better therapeutic options and explain to parents the pros and cons of these two therapies.
Limitations
The clinical use of preformed crowns is not very popular in Shenzhen city, and restorative techniques differ among dental practitioners. Shenzhen Children’s Hospital is a specialized hospital for children, and dental staff often conduct uniform training and perform many preformed crown restorations; hence, the data are relatively reliable. However, the sample size in this study was relatively small, and the research focused only on a single hospital in Shenzhen and could not be generalized to other regions or populations, which probably limits its applicability. Multicenter institutions will be included in future studies. Moreover, the factors affecting the clinical data of preformed crowns will be studied, which will be beneficial for enhancing their utilization and effectively promoting OHRQoL.
Supplementary Information
Acknowledgements
The authors deny any conflicts of interest related to this study.
Abbreviations
- PMCs
preformed metal crowns
- OHRQoL
oral health-related quality of life
- Zirconia Crowns
ZCs
Authors’ contributions
Li Zhang and Shuman Deng conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted. Zhixiao Chen and Ying Chen conceptualized and designed the study, conducted the data analysis, and drafted the initial manuscript. Weiwei Dou and Jing Xie participated in data collection and sorting and reviewed and revised the manuscript. Qi Gao and Ning Song prepared the data and initial analysis, critically reviewed the manuscript and approved the final manuscript as submitted. All the authors have read and approved the manuscript.
Funding
This study was funded by the Shenzhen Science and Technology Program (No. JCYJ20230807093811023).
Data availability
All the data used in this study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The study protocol was reviewed and approved by the Shenzhen Children’s Hospital ethics committee [Project No. 202312] and conformed to the ethical standards for medical research involving human subjects, as laid out in the 1964 Declaration of Helsinki and its later amendments. The participants, including children and their guardians, provided written informed consent prior to taking part in the study.
Consent for publication
The results/data/figures in this manuscript have not been published elsewhere, nor are they under consideration by another publisher.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shuman Deng and Weiwei Dou are co-first authors.
Li Zhang and Qi Gao contributed equally as Corresponding authors.
Contributor Information
Qi Gao, Email: gorky986661@163.com.
Li Zhang, Email: adazhangl@126.com.
References
- 1.Seow WK. Early childhood caries. Pediatr Clin North Am. 2018;65(5):941–54. [DOI] [PubMed] [Google Scholar]
- 2.Feng XP. Oral health status of Chinese residents—the fourth epidemiological survey of oral health in China. Professional Committee of Oral Preventive Medicine, Chinese Stomatological Association. Compilation of papers on the 18th annual conference of oral preventive medicine of Chinese Stomatological Association in 2018. Xi’an: Chinese Stomatological Association; 2018. p. 13.
- 3.Yin CF, Zhang RZ, Yang XM. Study on linear regression prediction model of childhood Henoch-Schonlein purpura based on quantitative analysis of caries related factors. J Clin Stomatol. 2023;39(1):33–7. [Google Scholar]
- 4.Kirthiga M, Muthu MS, Kayalvizhi G, et al. Variations in primary molar contact and approximal caries in children: a three-year prospective cohort study. Pediatr Dent. 2023;45(5):434–42. [PMC free article] [PubMed] [Google Scholar]
- 5.Ekstrand KR, Gimenez T, Ferreira FR, et al. The International Caries Detection and Assessment System - ICDAS: a systematic review. Caries Res. 2018;52(5):406–19. [DOI] [PubMed] [Google Scholar]
- 6.American Academy on Pediatric Dentistry Clinical Affairs Committee-Restorative Dentistry Subcommittee, American Academy on Pediatric Dentistry Council on Clinical Affairs. Guideline on pediatric restorative dentistry. Pediatr Dent. 2008;30(7 Suppl):163–9.19216416 [Google Scholar]
- 7.Whelton HP, Spencer AJ, Do LG, et al. Fluoride revolution and dental caries: evolution of policies for global use. J Dent Res. 2019;98(8):837–46. [DOI] [PubMed] [Google Scholar]
- 8.Deng S, Gao Q, Zhang L, et al. Prefabricated zirconia crowns and preformed metal crowns in the treatment of severely childhood caries and anterior crossbite in a child with autistic spectrum disorder. Case Rep Dent. 2024;2024:5556502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Innes NP, Ricketts D, Chong LY, et al. Preformed crowns for decayed primary molar teeth. Cochrane Database Syst Rev. 2015;2015(12):CD005512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koleventi A, Sakellari D, Arapostathis KN, et al. Periodontal impact of preformed metal crowns on permanent molars of children and adolescents: a pilot study. Pediatr Dent. 2018;40(2):117–21. [PubMed] [Google Scholar]
- 11.Yun Liu G, Hao Q, Zhang, et al. Survey and analysis of the application of metal pre crown for deciduous molars in children aged 3–5 in Shenzhen. China J Aesthetic Med. 2022;31(11):142–5. [Google Scholar]
- 12.Yun Liu G, Hao J. A sampling survey on the caries status of deciduous teeth in 3-year-old children in Shenzhen. J Clin Stomatol. 2020;36(11):669–72. [Google Scholar]
- 13.Kodaira H, Ohno K, Fukase N, et al. Release and systemic accumulation of heavy metals from preformed crowns used in restoration of primary teeth. J Oral Sci. 2013;55(2):161–5. [DOI] [PubMed] [Google Scholar]
- 14.Chen Y, Chen K, Liu ZL. Evaluation of occlusal function of young permanent molars with serious dental defects repaired by different ways. China J Conserv Dent. 2017;27(7):407–9. [Google Scholar]
- 15.Randall RC, Vrijhoef MM, Wilson NH. Efficacy of preformed metal crowns vs. amalgam restorations in primary molars: a systematic review. J Am Dent Assoc. 2000;131(3):337–43. [DOI] [PubMed] [Google Scholar]
- 16.Hanafi L, Altinawi M, Comisi JC. Evaluation and comparison two types of prefabricated zirconia crowns in mixed and primary dentition: a randomized clinical trial. Heliyon. 2021;7(2):e06240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Güçlü ZA, Çalışkan S, Efe Z, Doğan S. Can Zirconia crowns be the first restorative choice after endodontic treatment of primary teeth? Int J Clin Pract. 2021;75(12):e14888. [DOI] [PubMed] [Google Scholar]
- 18.Wang J, Zhang B, Chen Y, et al. A comparison of the mechanical proprieties of different types of primary tooth restorations: an in vitro study. Clin Oral Investig. 2022;26(6):4419–26. [DOI] [PubMed] [Google Scholar]
- 19.Taran PK, Kaya MS. A Comparison of Periodontal Health in primary molars restored with Prefabricated Stainless Steel and Zirconia crowns. Pediatr Dent. 2018;40(5):334–9. [PubMed] [Google Scholar]
- 20.Elheeny AAH, Abdelmotelb MA. Oral health-related quality of life (OHRQOL) of preschool children’s anterior teeth restored with zirconia crowns versus resin-bonded composite strip crowns: a 12-month prospective clinical trial. Clin Oral Investig. 2022;26(5):3923–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duggal M, Gizani S, Albadri S, et al. Best clinical practice guidance for treating deep carious lesions in primary teeth: an EAPD policy document. Eur Arch Paediatr Dent. 2022;23(5):659–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Almaghrabi MA, Albadawi EA, Dahlan MA, et al. Exploring parent’s satisfaction and the effectiveness of Preformed Metal crowns Fitting by Hall technique for Carious Primary molars in Jeddah Region, Saudi Arabia: findings of a prospective cohort study. Patient Prefer Adherence. 2022;16:2497–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zou J, Du Q, Ge L, Wang J, et al. Expert consensus on early childhood caries management. Int J Oral Sci. 2022;14(1):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ludovichetti FS, Zuccon A, Lucchi P, et al. Mothers’ awareness of the correlation between their own and their children’s oral health. Int J Environ Res Public Health. 2022;19(22):14967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Naidu RS, Nunn JH. Oral health knowledge, attitudes and behaviour of parents and caregivers of preschool children: implications for oral Health Promotion. Oral Health Prev Dent. 2020;18(2):245–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baldani MH, Mendes YBE, Lawder JADC, et al. Inequalities in dental services utilization among Brazilian low-income children: the role of individual determinants. J Public Health Dent. 2011;71(1):46–53 Win. [DOI] [PubMed] [Google Scholar]
- 27.George A, Sousa MS, Kong AC, et al. Effectiveness of preventive dental programs offered to mother s by non-dental professionals to control early childhood dental caries: a review. BMC Oral Health. 2019;19(1):172. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All the data used in this study are available from the corresponding author upon reasonable request.