Abstract
The present study was aimed to investigate whether Gensini score or SYNTAX score was a valuable tool to predict in-stent restenosis (ISR) in coronary artery disease (CAD) patients with drug-eluting stents (DES) implantation. A retrospective case-control study and a validating retrospective cohort study were designed. All subjects’ information was collected from the First Affiliated Hospital of Xinjiang Medical University. A total of 916 patients were enrolled in the case-control study, and 961 subjects were included in the retrospective-cohort study. In the case-control study, significant differences were observed between the ISR and non-ISR groups regarding baseline characteristics and clinical examinations, including waist circumference, systolic blood pressure, blood glucose levels, ApoA1 levels, left ventricular ejection fraction, lesion vessels, Gensini score, and SYNTAX score (all P < 0.05). All parameters showing significant differences were also associated with ISR (all P < 0.05). However, after adjustment for confounders, both Gensini score [tertile 3 vs. tertile 1 with OR 95%CI: 15.61 (5.37–45.39)] and SYNTAX score [high risk ≥ 33 vs. low risk ≤ 22 with OR 95%CI 12.61 (5.14–30.94)] were still independently associated with ISR. Furthermore, Gensini score [AUC 95%CI: 0.81 (0.78–0.84)] and SYNTAX score [AUC 95%CI: 0.76 (0.72–0.79)] showed a moderate ability to predict ISR. The predictors were further verified in a cohort validation study, which confirmed that the Gensini score was a better predictor for ISR than SYNTAX score, with an AUC and 95%CI of 0.67 (0.60–0.73) and 0.53 (0.46–0.60), respectively. Gensini score showed a higher capability to predict ISR than SYNTAX score in CAD patients with DES implantation. SYNTAX score may also be a useful tool for assessing the risk of ISR in patients with multivessel lesions.
Keywords: Gensini score, SYNTAX score, Coronary artery disease, In-stent restenosis, Drug-eluting stent
Subject terms: Cardiovascular diseases, Cardiology
Introduction
Coronary heart disease (CAD) is still one of the main causes of death worldwide. Its effective treatment including percutaneous coronary intervention (PCI), in which stents are implanted in coronary arteries to restore blood flow to myocardium, has been widely used in patients with CAD. However, the benefits of PCI have been partially offset by the occurrence of in-stent restenosis (ISR), which leads to myocardial infarction (MI) or repeat vessel revascularization. With millions of patients receiving stents each year, ISR has become a significant public health problem. Over the past decades, stents have evolved to address this problem. For example, drug-eluting stents (DES) and biodegradable stents have been developed and have significantly reduced the likelihood of ISR compared to bare-metal stents (BMS)1. Despite the widespread use of DES, ISR still occurs in approximately 5–10% of patients2,3, which remains an unavoidable obstacle to the application of stents and weakens the long-term benefits of PCI.
To date, many ISR-related risk factors have been developed, such as calcified lesions, bifurcation lesions, diabetes mellitus, stent diameter and length in terms of anatomy factors, clinical factors, and stent- and procedure-related factors4. Several novel predictive indicators including laboratory serological parameters or microRNAs, have also been proposed before coronary stenting5–8. Recently, prediction models and novel score systems have also been developed to assess the probability risk of ISR9, and our previous study showed that a prediction model based on platelet, blood pressure, blood cholesterol, and lesion vessel parameters was a feasible model to predict ISR in patients undergoing DES implantation10. However, to date, no widely accepted and efficient predictor has been practiced to assess the risk of ISR. Therefore, we wondered whether some score systems already frequently performed in clinics could also be considered as a score system to assess the likelihood of ISR. However, few score systems have been validated and accepted. One published study tried to use CHA2DS2-VASc score to predict ISR, but the result was not ideal11.
As we know, ISR exists some different mechanisms from the regular progression of coronary atherosclerosis in the pathophysiological process, such as the procedures of stent implantation, stent characters, the response of the platelet aggregation in the circulation and endothelial immunity in the vascular to the stents were part of the mechanisms contributing to adverse arterial remodeling and neointimal hyperplasia. However, most of the mechanisms of ISR were still the same as the mechanisms of atherosclerosis development, including the common risk factors of patient-related factors, anatomical factors, enhanced vascular inflammation, excessive proliferation of vascular smooth muscle cells, and structural remodeling of the vasculature4,12,13. One would naturally think that patients with more severe coronary artery stenosis would be more likely to experience ISR. However, whether the severity of coronary artery stenosis predicts the risk of ISR has not been well defined. Both the Gensini score and SYNTAX score have been widely applied to evaluate the complexity of CAD because they incorporate multiple elements, such as lesion severity, summed scores of each obstruction, and weighting of the roles of their location14,15. In addition, they have also been developed as predictors of adverse cardiovascular disease (CVD)16,17. However, whether Gensini score or SYNTAX score is a valuable tool for predicting ISR is still less evaluated. And investigation of this issue would help to find novel predictors and new functions of these score systems to perform risk stratification for ISR in patients with CAD and stent implantation.
The aim of this study was to determine whether Gensini score or SYNTAX score from the primary angiographic examination is an effective tool for predicting the risk of ISR in CAD patients implanted with DES.
Methods and materials
Ethical approval
This study was approved by the Ethics Committee of the First Affiliated Hospital of Xinjiang Medical University (approval number: K202003-23) and was conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from all participants or their legal guardians.
Participants
This study firstly enrolled 916 patients in a case-control design, all of these subjects were recruited from the First Affiliated Hospital of Xinjiang Medical University from September 2014 to September 2018, and were diagnosed with CAD, implanted with DES, and had angiographic follow-up for more than 6 months. In addition, these recruited patients need to meet the inclusion and exclusion criteria. The inclusion criteria were that all subjects were over 18 years old, diagnosed with CAD, underwent the DES implantation, and accepted angiographic follow-up after stent implantation for more than 6 months. The exclusion criteria were that subjects had autoimmune diseases, coronary artery bypass surgery, malignant tumors, and heart failure. And the included patients were divided into ISR group and non-ISR group according to their angiographic diagnosis.
The distributions of the case and control groups were according to whether the participants had ISR. We then matched the case groups to the control group according to the age and sex of the control group.
Then we used our previously established retrospective cohort study of 961 CAD subjects10 to verify the results of the case-control study. The inclusion and exclusion criteria were similar. Subjects in this cohort study were recruited between September 2010 and September 2013. (Fig. 1)
Fig. 1.
The study flow diagram. CAD coronary artery disease, ISR in-stent restenosis, DES drug-eluting stents.
Data collection
Demographic information, medical history, clinical data, biochemical results, and angiographic results of primary PCI were collected. Specifically, the information collected included sex, age, body mass index (BMI), history of hypertension, diabetes, smoking, echocardiographic data, angiographic results, procedural information of PCI, stent information, blood glucose, blood cholesterol, and angiographic follow-up results. Missing quantitative data were imputed by using the mean value of the variable close to the missing data in the statistics.
Diagnostic criteria
The ISR is defined as the follow-up angiography results indicating that the degree of restenosis in the inner stents or 5 mm distance to the edge of the stent is more than 50%, if not were defined as non-IS18.
The diagnosis of hypertension was made according to the guideline of hypertension, briefly was repeated measurement of systolic pressure ≥ 140 mmHg and/or diastolic pressure ≥ 90 mmHg in resting state, or taking antihypertensive medication19. The definition of diabetes mellitus (DM) was according to previously published guidelines20.
Calculation and classification of Gensini score and SYNTAX score
We calculated the Gensini score according to its formula14 and the SYNTAX I score by software (https://syntaxscore.org/). The calculation of Gensini score is depends on the location of the stenosis in the coronary arteries and the degree of stenosis. Specifically, stenosis degrees of 25%, 50%, 75%, 90%, 99%, and total occlusion were given scores of 1, 2, 4, 8, 16, and 32, respectively, and then multiplied by the scores in the location of proximal, middle, and distal parts of each artery, and finally summed the scores in each artery for each subject21. SYNTAX scores were obtained by clicking on the appropriate choices in the SYNTAX I score software for each patient to obtain their calculated score. The Gensini score was classified according to the statistical methods of tertile in order to facilitate a more profound comprehension of the characteristics and trends exhibited by the data. The SYNTAX score was categorized as low risk (≤ 22), moderate risk (23–32), and high risk (≥ 33)22,23.
Statistical analyses
All results were analyzed according to their value categories. The continuous variables had normal distributions, tested by the Kolmogorov–Smirnov test, expressed as means ± SD and tested by the independent T-test or one-way ANOVA test. Categorical variables were presented as frequencies and percentages, and compared using the χ2 test. Continuous variables that were not normally distributed were expressed as medians (first quartile, third quartile), and analyzed by the Wilcoxon signed-rank test. Univariate and forward stepwise multivariable logistic regression analyses were performed to identify independent risk factors. Receiver operating characteristic (ROC) curves were used to determine the capability to predict ISR. In addition, the Youden Index was applied to figure out the optimal cut-off values for potential variables. Statistical tests of P value were two-sided. When a P < 0.05 was considered as statistically significant. All statistical procedures were conducted by SPSS 23.0 (SPSS Inc., Chicago, IL, USA).
Results
Characteristics of subjects in the ISR and non-ISR group
There were 916 patients recruited, of 315 patients in the ISR group and 601 patients in the non-ISR group. The mean age (60.09 ± 9.85 years vs. 60.30 ± 10.88 years, P > 0.05) and male proportion (80.32% vs. 79.13%, P > 0.05) were comparable between the ISR and non-ISR groups. The comparisons between the ISR and non-ISR groups in aspects of baseline characteristics, medical history, and clinical results are displayed (Table 1). And angiographic results and stent information were presented in Table 2. The frequencies of smoking, drinking, history of hypertension, diabetes, arrhythmia, atrial fibrillation, the levels of BMI, lipoprotein (a), total cholesterol (TC), triglyceride (TG), low-density lipoprotein (LDL), high-density lipoprotein (HDL), creatinine, and uric acid were showed no differences between groups (all P > 0.05, Table 1). However, the parameters of waist circumference, systolic blood pressure (SBP), diastolic blood pressure (DBP), blood glucose, frequencies of myocardial infarction (MI), ApoA1, and left ventricular ejection fraction (LVEF) were significantly different between groups (all P < 0.05, Table 1).
Table 1.
Characteristics of study subjects.
| Parameters | Non-ISR group (n = 601) | ISR group (n = 315) | P values |
|---|---|---|---|
| Demographic information | |||
| Age (years) | 60.3 ± 10.9 | 60.1 ± 9.9 | 0.778 |
| Male, n (%) | 474 (79.1) | 253 (80.3) | 0.559 |
| Current smoking, n (%) | 351 (80.3) | 175 (78.8) | 0.682 |
| Alcohol intake, n (%) | 73 (17.1) | 42 (19.4) | 0.455 |
| Waist circumference (cm) | 91.9 ± 13.0 | 95.2 ± 13.2 | 0.002 |
| BMI (kg/m2) | 26.4 ± 3.4 | 26.6 ± 3.4 | 0.348 |
| SBP (mmHg) | 144.0 ± 32.9 | 150.5 ± 31.2 | 0.019 |
| DBP (mmHg) | 88.6 ± 22.2 | 93.7 ± 21.6 | 0.007 |
| Medical history | |||
| Hypertension, n(%) | 343 (57.2) | 191 (60.6) | 0.324 |
| Diabetes, n(%) | 137 (22.8) | 80 (25.4) | 0.414 |
| MI, n(%) | 56 (9.3) | 46 (14.6) | 0.019 |
| Arrhythmia (%) | 38 (6.3) | 17 (5.4) | 0.661 |
| Atrial fibrillation, n(%) | 8 (1.3) | 6 (1.9) | 0.573 |
| Laboratory data | |||
| TC (mmol/L) | 4.0 ± 2.1 | 4.2 ± 2.3 | 0.212 |
| TG (mmol/L) | 2.9 ± 5.2 | 2.8 ± 4.7 | 0.728 |
| HDL (mmol/L) | 3.6 ± 15.5 | 3.5 ± 14.7 | 0.922 |
| LDL (mmol/L) | 3.9 ± 16.5 | 2.9 ± 7.8 | 0.356 |
| Blood glucose (mmol/L) | 6.1 ± 3.0 | 6.8 ± 3.9 | 0.007 |
| Glycated serum protein (mmol/L) | 4.6 ± 11.9 | 4.2 ± 10.9 | 0.628 |
| Creatine (µmol/L) | 79.6 ± 37.8 | 79.3 ± 31.1 | 0.915 |
| ApoA1 (g/L) | 1.2 ± 0.3 | 1.1 ± 0.2 | 0.006 |
| Uric acid (µmol/L) | 310.6 ± 112.5 | 320.2 ± 110.5 | 0.227 |
| LVEF (%) | 61.1 ± 8.9 | 59.4 ± 8.3 | 0.024 |
| Gensini score | 18.3 ± 24.4 | 50.7 ± 38.4 | < 0.001 |
Data are expressed as means ± SD, median with IQR, and numbers with percentages depending on their data categories and distributions.
ISR in-stent restenosis, BMI body mass index, SBP systolic blood pressure, DBP diastolic blood pressure, MI myocardial infarction, PDW platelet distribution width, LDL-C low-density lipoprotein cholesterol, HDL high density lipoprotein, TC total cholesterol, TG triglyceride, LVEF left ventricular ejection fraction.
Table 2.
Comparisons of characteristics of angiography and stents.
| Parameters | Non-ISR group (n = 601) | ISR group (n = 315) | t/χ2 | P values |
|---|---|---|---|---|
| Stenosis of coronary artery | ||||
| LM, n (%) | 19 (3.2) | 18 (5.7) | 3.46 | 0.077 |
| LAD, n (%) | 201 (33.5) | 253 (80.3) | 181.11 | < 0.001 |
| LCX, n (%) | 171 (28.5) | 169 (53.6) | 55.95 | < 0.001 |
| RCA, n (%) | 173 (28.8) | 179 (56.8) | 68.37 | < 0.001 |
| Lesion vessels | 1.3 ± 1.2 | 2.5 ± 1.2 | – 14.39 | < 0.001 |
| Number of stents | 1.1 ± 0.3 | 1.1 ± 0.3 | 0.03 | 0.980 |
| Total of stents length (mm) | 38.7 ± 23.9 | 35.0 ± 18.7 | – 1.09 | 0.276 |
| Gensini Score, M (Q1, Q3) | 8.0 (2.0,25.0) | 44.0 (18.5,72.0) | – 15.17 | < 0.001 |
| SYNTAX score, M (Q1, Q3) | 6.0 (0.0,13.0) | 16.5 (9.0,25.0) | – 12.30 | < 0.001 |
Data are expressed as means ± SD, median with IQR, and numbers with percentages depending on their data categories and distributions.
LM left main coronary artery, LCX left circumflex coronary artery, RCA right coronary artery, LAD left anterior descending coronary artery.
Comparisons of characteristics of angiography and stents
The characteristics of angiographic results in Table 2 indicated that the distributions of stenosis in left anterior descending coronary artery (LAD), left circumflex coronary artery (LCX), right coronary artery (RCA), and the average number of lesion vessels were significantly higher in the ISR group than the non-ISR groups (all P < 0.05). But the average numbers of implanted stent and total stent length were similar between the two groups (P > 0.05). Furthermore, the results demonstrated that both the Gensini score and SYNTAX score were significantly higher in the ISR group than the non-ISR group (p < 0.05). (Table 2)
Logistic regression analysis was conducted to explore whether Gensini score and SYNTAX score were independently associated with ISR
The parameters existed differences in baseline characteristics and clinical results were proceed the further analysis of univariate and multivariate logistic regression analysis. Variables such as waist circumference, SBP, blood glucose, ApoA1, LVEF, number of lesion vessels, Gensini Score, and SYNTAX score were found to be associated with ISR (all P < 0.05). When regarding the first tertile of Gensini score and low risk (≤ 22) of SYNTAX score as references, respectively, and after adjusting confounding factors of waist circumference, SBP, blood glucose, ApoA1, LVEF, number of lesion vessels, the second and third tertiles of Gensini score and moderate (23–32) and high risk (≥ 33) of SYNTAX score were still independently associated with ISR. Furthermore, their odds ratios (OR) of the second tertile and the third tertile of Gensini score and the moderate and high risk of SYNTAX score were gradually increased. (Table 3)
Table 3.
Univariate and multivariate logistic regression analysis for Gensini score and SYNTAX score in subjects with ISR.
| Parameters | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P values | OR | 95% CI | P values | |
| SBP | 1.01 | (1.01–1.01) | 0.008 | |||
| Waist circumference | 1.02 | (1.01–1.03) | 0.002 | |||
| LVEF | 1.66 | (1.10–2.52) | 0.017 | |||
| Blood glucose | 1.06 | (1.02–1.11) | 0.006 | |||
| ApoA1 | 0.43 | (0.23–0.79) | 0.007 | |||
| Lesion vessels | 1.50 | (1.12–2.00) | < 0.001 | |||
| Gensini score | ||||||
| T1, Gensini score < 8.00, n (%) | 1 (Reference) | 1 (Reference) | ||||
| T2, 8 ≤ Gensini score < 32, n (%) | 3.13 | (2.25–4.34) | < 0.001 | 2.44 | (1.53–3.89) | < 0.001 |
| T3, Gensini score ≥ 32.00, n (%) | 23.80 | (14.05–40.30) | < 0.001 | 15.61 | (5.37–45.39) | < 0.001 |
| SYNTAX score | ||||||
| Low SYNTAX score (≤ 22) | 1 (Reference) | 1 (Reference) | ||||
| Intermediate SYNTAX score (22–33) | 2.75 | (1.82–4.17) | < 0.001 | 2.72 | (1.69–4.36) | < 0.001 |
| High SYNTAX score (≥ 33) | 13.12 | (5.74–29.97) | < 0.001 | 12.61 | (5.14–30.94) | < 0.001 |
Adjusted variables: SBP, Waist circumference, LVEF, blood glucose, APOA1, number of lesion vessels.
ISR in-stent restenosis, OR odds ratio, SBP systolic blood pressure, LVEF left ventricular ejection fraction.
ROC analysis to ascertain the predictability of the Gensini score and SYNTAX score for ISR in subjects with varying numbers of lesion vessels
In the study, the subjects who exhibited one or more lesion vessels demonstrated superior predictability when assessed using the Gensini score in comparison to the SYNTAX score (Fig. 2a-b). The area under the curve (AUC) values were 0.81 (95% CI 0.78–0.84) for the Gensini score and 0.76 (95% CI 0.72–0.79) for the SYNTAX score, respectively (Fig. 2a). The optimal Gensini score cut-off value was determined to be 21.50, with a sensitivity of 73% and a specificity of 72%. Subjects with a SYNTAX score greater than 8.75 were found to be at a significantly elevated risk of ISR, with a sensitivity and specificity of 77% and 62%, respectively. A subsequent subgroup analysis was conducted on subjects with lesion vessels comprising more than two or three vessels. The SYNTAX score demonstrated superior predictability compared to the Gensini score. The AUC values were 0.69 (95% CI 0.64–0.74) for the Gensini score and 0.70 (95% CI 0.65–0.75) for the SYNTAX score in cases with more than two lesion vessels (Fig. 2c). The optimal SYNTAX score cut-off value was determined to be 14.75, with a sensitivity of 69% and a specificity of 61%. In cases involving three or more lesion vessels, the AUC was 0.69 (95% CI 0.62–0.77) for the Gensini score and 0.73 (95% CI 0.66–0.79) for the SYNTAX score (Fig. 2d).
Fig. 2.
ROC analysis results of Gensini score and SYNTAX score for ISR in the case-control study.
The baseline characteristics of the validating cohort study
As we observed that the Gensini score indicated a more efficient capability to predict ISR in the case-control designed study. To validate the findings observed in the case-control study, we analyzed the relationship between Gensini score and ISR in the validating cohort study. We firstly equally distributed subjects into three groups according to the first and third tertiles of Gensini score. The parameters of age, sex, smoking, BMI, waist circumference, TC, and LDL showed comparable results. However, the variables of DBP, blood glucose, ApoA1, LVEF, and lesion vessels showed significant differences among groups (all P < 0.05). Meanwhile, the incidences of ISR were gradually raised from the first tertile to the third tertile of Gensini score (P < 0.05). In addition, we observed that the SYNTAX scores were also gradually increased from the first-tertile group to the third tertile group of Gensini score (P < 0.05). (Table 4)
Table 4.
The baseline characteristics of validating cohort study.
| Parameters | Gensini score ≤ 10 (n = 298) | Gensini score 10–34 (n = 330) | Gensini score ≥ 34 (n = 333) | t/χ2 | P value |
|---|---|---|---|---|---|
| Age (year) | 58.3 ± 10.7 | 58.9 ± 10.9 | 59.8 ± 10.9 | 1.53 | 0.218 |
| Male, n (%) | 236 (79.2) | 256 (77.6) | 261 (78.4) | 0.24 | 0.886 |
| Smoking, n (%) | 150 (50.3) | 175 (53.0) | 169 (50.8) | 0.54 | 0.762 |
| BMI (kg/m2) | 26.4 ± 3.6 | 26.0 ± 3.7 | 26.1 ± 3.5 | 0.68 | 0.504 |
| Waist circumference (cm) | 92.2 ± 13.4 | 91.4 ± 13.3 | 93.1 ± 13.9 | 0.87 | 0.418 |
| SBP (mmHg) | 135.1 ± 34.7 | 138.0 ± 30.8 | 140.3 ± 33.2 | 1.92 | 0.147 |
| DBP (mmHg) | 93.4 ± 23.7 | 98.9 ± 26.0 | 96.0 ± 24.7 | 3.82 | 0.022 |
| Blood glucose (mmol/L) | 6.3 ± 2.7 | 6.3 ± 2.7 | 6.8 ± 3.3 | 3.66 | 0.026 |
| TC (mmol/L) | 4.2 ± 1.5 | 4.1 ± 1.3 | 4.3 ± 1.9 | 2.2 | 0.111 |
| LDL (mmol/L) | 2.5 ± 0.9 | 2.5 ± 0.9 | 2.4 ± 0.9 | 1.02 | 0.359 |
| ApoA1 (g/L) | 1.2 (1.0,1.3) | 1.2 (0.9,1.3) | 1.1(0.9,1.3) | 10.01 | 0.007 |
| LVEF (%) | 61.9 ± 7.2 | 62.0 ± 6.1 | 60.6 ± 7.8 | 3.19 | 0.042 |
| Lesion vessels | 0.8 ± 1.0 | 2.3 ± 1.1 | 3.1 ± 1.2 | 347.77 | < 0.001 |
| ISR, n (%) | 7 (12.9) | 17 (31.5) | 30 (55.6) | 13.36 | < 0.001 |
| SYNTAX score | 9.0 (4.0,19.0) | 12.0 (8.0,19.0) | 22.0 (14.0,31.0) | 180.45 | < 0.001 |
Data are expressed as means ± SD, median with IQR, and numbers with percentages depending on their data categories and distributions.
ISR in-stent restenosis, BMI body mass index, SBP systolic blood pressure, DBP diastolic blood pressure, LDL-C low-density lipoprotein cholesterol, TC total cholesterol, LVEF left ventricular ejection fraction.
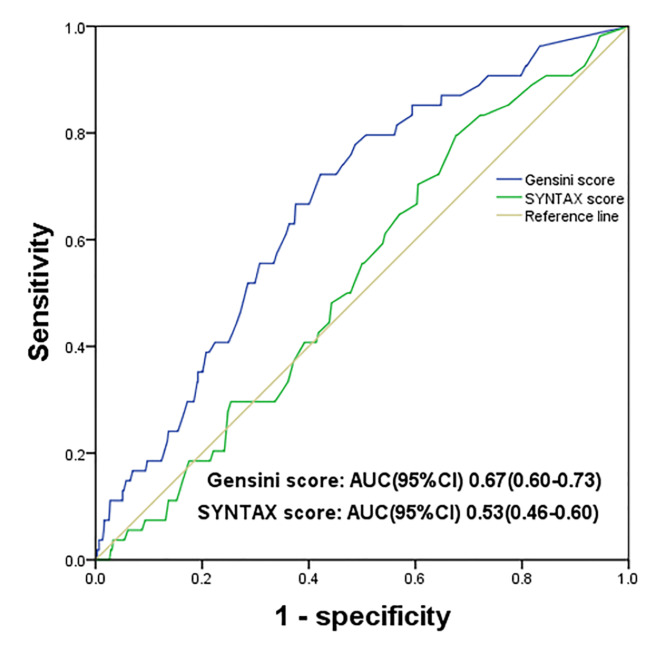
Logistic regression and ROC analysis demonstrated that the Gensini score was a practical, independent predictor of ISR in the validating cohort study
Further analysis confirmed that the Gensini score was also independently associated with ISR in the validating study, after adjusting for the confounding risk factors of DBP, LVEF, APOA1, blood glucose, and lesion vessels (Table 5). However, the SYNTAX score did not indicate significant associations with ISR in univariate and multivariate analysis. Furthermore, the ROC analysis was conducted to assess the predictive capacity of the Gensini score and the SYNTAX score for ISR. Ultimately, our findings demonstrated that the Gensini score exhibited superior predictive efficacy for ISR compared to the SYNTAX score. The respective AUCs (95% CI) were 0.67 (0.60–0.73) and 0.53 (0.46–0.60) (Fig. 3). A Gensini score of 25.50 was identified as the optimal cut-off point for predicting ISR, with a sensitivity and specificity of 72% and 57%, respectively.
Table 5.
Logistic regression analysis for ISR in validation cohort study.
| Parameters | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| RR | 95% CI | P values | RR | 95% CI | P values | |
| Gensini score | ||||||
| T1, Gensini score < 8.00 | 1 (Reference) | 1 (Reference) | ||||
| T2, 8 ≤ Gensini score < 32 | 2.26 | (0.92–5.52) | 0.074 | 1.55 | (0.51–4.73) | 0.443 |
| T3, Gensini score ≥ 32.00 | 4.12 | (1.78–9.52) | < 0.001 | 3.93 | (1.43–10.75 | 0.008 |
| SYNTAX score | ||||||
| Low SYNTAX score (≤ 22) | 1 (Reference) | 1 (Reference) | ||||
| Intermediate SYNTAX score (22–33) | 1.23 | (0.43–3.52) | 0.705 | 0.97 | (0.33–2.85) | 0.951 |
| High SYNTAX score (≥ 33) | 1.67 | (0.53–5.23) | 0.378 | 1.48 | (0.47–4.73) | 0.505 |
Adjusted variables: DBP, LVEF, APOA1, blood glucose, number of lesion vessels.
ISR in-stent restenosis, DBP systolic blood pressure, LVEF left ventricular ejection fraction.
Fig. 3.
ROC analysis results of Gensini score and SYNTAX score for ISR in the validating cohort study.
Discussion
In this study, we demonstrated that the Gensini score and SYNTAX score were independent predictors of ISR in patients with CAD who had undergone implantation of DES. Furthermore, our findings indicated that the Gensini score exhibited superior accuracy in predicting ISR compared to the SYNTAX score, as evidenced by the results of a case-control study and a validating cohort study. The optimal cut-off value for the Gensini score in predicting ISR was determined to be 21.50, exhibiting good sensitivity and specificity. The present study serves to verify and expand the application of the Gensini score as a reliable and practical tool for the prediction of ISR.
PCI represents one of the most efficacious methods for alleviating CAD disease and reducing mortality rates. A drug-eluting stent (DES) was identified as the optimal first-line treatment for PCI, given its superior efficacy24. Given that millions of people receive implanted DES every year, the 2-10% of incidence of ISR still means a large number of patients need to undergo coronary artery revascularization25,26. Except for some stent and implantation procedure factors that promote ISR, most mechanisms of ISR development, such as chronic inflammation and/or endothelial dysfunction-induced neo-atherosclerosis27, are similar to the generation of atherosclerosis. Studies have attempted to develop novel prediction models to provide prevention and stratification strategies for clinics5–8,26, but most of them have not been widely accepted by clinicians. Therefore, a widely accepted and convenient tool to predict ISR is necessary. Some people showed that the CHA2DS2-VASc score was a useful predictor for ISR in patients implanted with bare-metal stents28. It is established that the development of atherosclerosis and ISR share some of the same underlying mechanisms. It is well known that the Gensini score and SYNTAX score are commonly employed to assess the extent of stenosis and plaque burden in coronary arteries. However, there is a paucity of studies that have investigated their efficacy in evaluating the risk of ISR, and there is currently a lack of evidence to determine which score system is more appropriate for predicting ISR.
In this study, we demonstrated that both the Gensini score and the SYNTAX score were independent predictors of ISR in the case-control study. Our findings indicated that the Gensini score was more predictive of ISR than the SYNTAX score in patients with one or more lesions who had undergone DES in both case-control study and also validating cohort study. It is a widely accepted clinical practice to use the Gensini score or the SYNTAX score as a means for comprehensively evaluating the degree of stenosis and plaque burden in coronary arteries. Several published studies mentioned that the Gensini score and the SYNTAX score are involved in the development of ISR. Jiao Wang et al. proposed that the Gensini score and ApoB level would serve as predictors for ISR in Chinese Uygur CAD patients29. Jian-Long Wang et al. proposed that a higher SYNTAX score in conjunction with elevated serum levels of very-low-density lipoprotein cholesterol (VLDL-C) and uric acid (UA) may serve as predictors for ISR in patients with diabetes mellitus (DM) and with DES implantation30. The aforementioned published studies provided partial support for our conclusion that the Gensini score and SYNTAX score are independent predictors of ISR. However, our study, which had a larger sample size and was further validated in another study. In addition, we demonstrated that the Gensini score is more advanced than the SYNTAX score in predicting ISR in patients with DES implantation.
In the present study, the Gensini score indicated its advancement to predict ISR. The Gensini score is calculated based on the importance and corresponding area of blood supply of the coronary arteries where lesions occurred, as well as the percentage of stenosis in each coronary artery14. This assessment may be more adherent to the strategies of PCI and more specifically to the characteristic of culprit vessel. Nevertheless, the SYNTAX score incorporates a more intricate set of parameters. These characteristics are more indicative of the anatomic complexity of the coronary arteries than they are of the lesion burdens31,32. The anatomical characteristics of coronary artery dominance, bifurcation, and tortuosity were included in the SYNTAX score32, which may not closely related to the stent implantation or ISR, but potentially increase the confounding factors for ISR evaluation. Furthermore, in comparison to the intricate anatomical structures, the factors that facilitate the overall development of coronary artery lesions demonstrate a greater propensity for more severe inflammation or endothelial dysfunction in arteries that contribute to lesion formation, as opposed to limited complex artery anatomy. Similarly, Anil Avci and colleagues proposed that the Gensini score, rather than the SYNTAX score, was an independent predictor of carotid stenosis31. It is therefore proposed that the Gensini score is a more suitable predictor of ISR in clinical practice for patients with DES implantation. When subjects have a Gensini score above 21.50, they are more likely to experience ISR.
A subgroup analysis of the present study revealed that the SYNTAX score is an effective method for predicting ISR in patients with more than two or three lesion vessels. This implied that the SYNTAX score might be a valuable predictor for assessing multivessel coronary disease when patients with complex multivessel coronary arteries disease. Cavalcante et al. demonstrated that the SYNTAX score is an effective tool for assessing long-term outcomes and anatomic complexity in patients with multivessel disease who have undergone recanalization intervention33. In light of these findings, it seems reasonable to suggest that the SYNTAX score may also be a useful tool for assessing the risk of ISR in patients with multivessel lesions, particularly when the SYNTAX score is higher than 14.75. However, further validation in more complex circumstances and a prospective study with larger sample size is required to determine whether the Gensini score or the SYNTAX score is more suitable for evaluating the risk of ISR.
It should be noted that the present study is subject to a number of limitations. Firstly, the study was retrospective and single-center designed, which may have resulted in the inclusion of confounding factors. Secondly, the optimal examination methods were not employed to assess the characteristics of ISR in greater detail. Thirdly, although the subjects were implanted with an equivalent number of stents in different groups, the locations of the stents were not distinguished, which may potentially influence the accuracy of the results.
Conclusion
The Gensini score and SYNTAX score were found to be independent predictors of ISR in patients with CAD who had undergone DES implantation. The Gensini score exhibited a greater predictive capacity for ISR than the SYNTAX score. In clinical practice, patients with a Gensini score exceeding 21.50 are likely to be at a high risk of ISR. While, SYNTAX score may also be a useful tool for assessing the risk of ISR in patients with multivessel lesions, with an optimal cut-off of 14.75.
Author contributions
The study was designed and conceived by XM.G and MT.G. MT.G and SQ.Y drafted the manuscript, A.R, L.Z, QL.L, BH.Z, AX.D, and S.H performed data collection; MY.W and SQ.Y conducted Gensini score and SYNTAX score calculation; XM.G revised the manuscript. All authors reviewed the manuscript.
Funding
This work was supported by open projects of State Key Laboratory of Pathogenesis, Prevention and Treatment of High Incidence Diseases in Central Asia (SKL-HIDCA-2022-7, SKL-HIDCA-2023-27), Natural Science Foundation of Xinjiang Uygur Autonomous Region (2022D01C768), the Key Program of the Natural Science Foundation of Xinjiang Science and Technology Department (2024D01D24), the National Natural Science Foundation of China (82060073), and the Youth Science and Technology Elite Talent Program of the Xinjiang Medical University (XYD2024Q03).
Data availability
Data is available from the corresponding author upon reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Joner, M. et al. Pathology of Drug-Eluting stents in humans. J. Am. Coll. Cardiol.48, 193–202. 10.1016/j.jacc.2006.03.042 (2006). [DOI] [PubMed] [Google Scholar]
- 2.Moussa, I. D. et al. Trends and outcomes of Restenosis after Coronary Stent Implantation in the United States. J. Am. Coll. Cardiol.76, 1521–1531. 10.1016/j.jacc.2020.08.002 (2020). [DOI] [PubMed] [Google Scholar]
- 3.Ertas, G. & Van Beusekom, H. Drug eluting stents: current status and new developments. Anadolu Kardiyol Derg. 12, 676–683. 10.5152/akd.2012.220 (2012). [DOI] [PubMed] [Google Scholar]
- 4.Giustino, G. et al. Coronary In-Stent restenosis: JACC state-of-the-art review. J. Am. Coll. Cardiol.80, 348–372. 10.1016/j.jacc.2022.05.017 (2022). [DOI] [PubMed] [Google Scholar]
- 5.Norgaz, T. et al. The relationship between preprocedural platelet size and subsequent in-stent restenosis. Acta Cardiol.59, 391–395. 10.2143/ac.59.4.2005204 (2004). [DOI] [PubMed] [Google Scholar]
- 6.Nan, J. et al. The predictive value of Monocyte Count to high-density lipoprotein cholesterol ratio in Restenosis after Drug-Eluting Stent Implantation. Int. J. Gen. Med.13, 1255–1263. 10.2147/IJGM.S275202 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang, Z., Liu, C. & Fang, H. Blood Cell parameters and Predicting Coronary In-Stent restenosis. Angiology70, 711–718. 10.1177/0003319719830495 (2019). [DOI] [PubMed] [Google Scholar]
- 8.Yuan, Y., Liu, X., Hao, S., He, Q. & Shen, Z. Plasma levels of miR-143 and miR-145 are associated with coronary in-stent restenosis within 1 year of follow-up after drug-eluting stent implantation. Ann. Transl Med.8, 756. 10.21037/atm-20-4227 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coughlan, J. J. et al. Derivation and validation of the ISAR score to predict the risk of repeat percutaneous coronary intervention for recurrent drug-eluting stent restenosis. EuroIntervention: J. EuroPCR Collab. Working Group. Interventional Cardiol. Eur. Soc. Cardiol.18, e1328–e1338. 10.4244/eij-d-22-00860 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gai, M. T. et al. A prediction model based on platelet parameters, lipid levels, and angiographic characteristics to predict in-stent restenosis in coronary artery disease patients implanted with drug-eluting stents. Lipids Health Dis.20, 118. 10.1186/s12944-021-01553-2 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yilmaz, S., Akboga, M. K., Aras, D. & Topaloglu, S. Evaluation of the predictive value of CHA(2)DS(2)-VASc score for In-Stent restenosis. Angiology69, 38–42. 10.1177/0003319717700746 (2018). [DOI] [PubMed] [Google Scholar]
- 12.Lee, M. & Banka, G. In-stent restenosis. Interventional Cardiol. Clin.5, 211–220. 10.1016/j.iccl.2015.12.006 (2016). [DOI] [PubMed] [Google Scholar]
- 13.Inoue, T. et al. Vascular inflammation and repair: implications for re-endothelialization, restenosis, and stent thrombosis. JACC Cardiovasc. Interv. 4, 1057–1066. 10.1016/j.jcin.2011.05.025 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gensini, G. G. A more meaningful scoring system for determining the severity of coronary heart disease. Am. J. Cardiol.51 (606). 10.1016/s0002-9149(83)80105-2 (1983). [DOI] [PubMed]
- 15.Farooq, V., Head, S. J., Kappetein, A. P. & Serruys, P. W. Widening clinical applications of the SYNTAX score. Heart (British Cardiac Society). 100, 276–287. 10.1136/heartjnl-2013-304273 (2014). [DOI] [PubMed] [Google Scholar]
- 16.Girasis, C. et al. SYNTAX score and clinical SYNTAX score as predictors of very long-term clinical outcomes in patients undergoing percutaneous coronary interventions: a substudy of SIRolimus-eluting stent compared with pacliTAXel-eluting stent for coronary revascularization (SIRTAX) trial. Eur. Heart J.32, 3115–3127. 10.1093/eurheartj/ehr369 (2011). [DOI] [PubMed] [Google Scholar]
- 17.Wang, K. Y., Zheng, Y. Y., Wu, T. T., Ma, Y. T. & Xie, X. Predictive value of Gensini score in the long-term outcomes of patients with coronary artery Disease who underwent PCI. Front. Cardiovasc. Med.8, 778615. 10.3389/fcvm.2021.778615 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mehran, R. et al. Angiographic patterns of in-stent restenosis: classification and implications for long-term outcome. Circulation100, 1872–1878. 10.1161/01.cir.100.18.1872 (1999). [DOI] [PubMed] [Google Scholar]
- 19.Volpe, M. & Tocci, G. ESH/ESC Guidelines for the management of hypertension, from theory to practice: global cardiovascular risk concept. Journal of hypertension. Supplement: official journal of the International Society of Hypertension. 27, S3-11. (2007). 10.1097/01.hjh.0000356766.86388.e5 (2009). [DOI] [PubMed]
- 20.Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes care. S5-20. (2003). 10.2337/diacare.26.2007.s5 [DOI] [PubMed]
- 21.He, L. Y., Zhao, J. F., Han, J. L., Shen, S. S. & Chen, X. J. Correlation between serum free fatty acids levels and Gensini score in elderly patients with coronary heart disease. J. Geriatr. Cardiol.11, 57–62. 10.3969/j.issn.1671-5411.2014.01.003 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang, X. et al. Association of the triglyceride glucose-body mass index with the extent of coronary artery disease in patients with acute coronary syndromes. Cardiovasc. Diabetol.23, 24. 10.1186/s12933-024-02124-2 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yoon, Y. H. et al. Impact of SYNTAX score on 10-Year outcomes after revascularization for Left Main Coronary Artery Disease. JACC Cardiovasc. Intervent.13, 361–371. 10.1016/j.jcin.2019.10.020 (2020). [DOI] [PubMed] [Google Scholar]
- 24.Costa, F. et al. Does large vessel size justify Use of Bare-Metal stents in primary percutaneous coronary intervention? Circ. Cardiovasc. Interv.12, e007705. 10.1161/circinterventions.118.007705 (2019). [DOI] [PubMed] [Google Scholar]
- 25.Kastrati, A. & Cassese, S. In-Stent restenosis in the United States: time to enrich its treatment armamentarium. J. Am. Coll. Cardiol.76, 1532–1535. 10.1016/j.jacc.2020.08.035 (2020). [DOI] [PubMed] [Google Scholar]
- 26.Ullrich, H., Olschewski, M., Münzel, T. & Gori, T. Coronary In-Stent restenosis: predictors and treatment. Deutsches Arzteblatt Int.118, 637–644. 10.3238/arztebl.m2021.0254 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brancati, M. et al. Coronary stents and vascular response to implantation: literature review. Pragmatic Observational Res.8, 137–148. 10.2147/por.S132439 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kurtul, A. Usefulness of the CHA2DS2-VASc score in Predicting In-Stent restenosis among patients undergoing revascularization with Bare-Metal stents. Clin. Appl. Thromb. Hemost.24, 589–595. 10.1177/1076029617716769 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang, J., Yang, Y., Zhang, L., He, P. & Mu, H. Predictors of Stent Restenosis in Han and Uygur patients with Coronary Heart Disease after PCI in the Xinjiang Region. Cardiol. Res. Pract.2022 (7845108). 10.1155/2022/7845108 (2022). [DOI] [PMC free article] [PubMed]
- 30.Wang, J. L. et al. New predictors of in-stent restenosis in patients with diabetes mellitus undergoing percutaneous coronary intervention with drug-eluting stent. J. Geriatric Cardiology: JGC. 15, 137–145. 10.11909/j.issn.1671-5411.2018.02.011 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Avci, A. et al. Association between the Gensini score and carotid artery stenosis. Korean Circulation J.46, 639–645. 10.4070/kcj.2016.46.5.639 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sianos, G. et al. The SYNTAX score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention: J. EuroPCR Collab. Working Group. Interventional Cardiol. Eur. Soc. Cardiol.1, 219–227 (2005). [PubMed] [Google Scholar]
- 33.Cavalcante, R. et al. Impact of the SYNTAX scores I and II in patients with diabetes and multivessel coronary disease: a pooled analysis of patient level data from the SYNTAX, PRECOMBAT, and BEST trials. European heart journal. 38, 1969– (1977). 10.1093/eurheartj/ehx138 (2017). [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available from the corresponding author upon reasonable request.