Abstract
The need to understand subjective health has increased during the COVID-19 pandemic, given its substantial impact on lifestyle habits and perceptions. Thus, this study aimed to investigate the trends and association of subjective health with demographic and behavioral factors, primarily focusing on the change when the COVID-19 pandemic emerged. This study used data from the Korea Youth Risk Behavior Web-based Survey, comprising 1,190,468 adolescents aged 12–18 years (female, 48.49%). We investigated the trends and association of subjective health with demographic and behavioral factors from 2006 to 2023. A weighted linear regression and joinpoint regression were conducted to evaluate the trend in adolescent subjective health, while logistic regression was used to assess associated factors. A stratification analysis was performed for subgroups to determine variations across different demographic and behavioral groups. The prevalence of reporting high subjective health increased throughout the years before the COVID-19 pandemic; however, subjective health exhibited a decreasing trend during the pandemic. Regarding demographic factors, female sex (ratio of odds ratio [ROR], 0.85 [95% CI, 0.83–0.87]), low-income households (ROR, 0.67 [95% CI, 0.64–0.69]), and low academic achievement (ROR, 0.83 [95% CI, 0.81–0.85]) were associated with less likelihood of reporting high subjective health. Healthier behavioral factors (ROR, breakfast consumption, 1.13 [95% CI, 1.10–1.16]; sufficient fruit intake, 1.12 [95% CI, 1.09–1.15]; sufficient physical activity, 2.02 [95% CI, 1.95–2.09]) were associated with higher subjective health, and the disparities increased during the COVID-19 pandemic. To address the observed decline in subjective health among adolescents during the COVID-19 pandemic, targeted interventions aimed at promoting healthy behaviors among particularly vulnerable demographics are crucial.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-83810-9.
Keywords: COVID–19, Subjective health, South Korea
Subject terms: Epidemiology, Paediatric research
Introduction
Subjective health, an individual’s self-assessment of health status, provides valuable insights into self-perception, mental health, and overall well-being, which can often differ significantly from objective health measures1. It encompasses unquantifiable aspects of health that could be often overlooked in conventional assessments of overall well-being. Understanding subjective health became particularly relevant during the COVID-19 pandemic, substantially impacting adolescents’ lifestyles. The pandemic led to decreased physical activity, increased screen time, and heightened social isolation, fundamentally altering adolescents’ daily routines and health behaviors2,3. Subjective health could be influenced by numerous factors, including lifestyle choices, educational experiences, and socio-environmental conditions4. Therefore, it is essential to investigate which factors are associated with high subjective health status and how these associations may have changed during the COVID-19 pandemic. Identifying the key determinants of subjective health before and during the pandemic can provide valuable insights for public health interventions and policies to improve public health5.
A healthy lifestyle includes activities and behaviors that enhance overall physical and mental fitness and reduce the risk of major illnesses6. Such behaviors include regular exercise, a balanced nutritious diet, adequate sleep, and abstaining from smoking. Numerous studies have found that a healthier lifestyle is associated with objective health, including reduced risks of obesity-related diseases, non-alcoholic fatty liver disease, cardiovascular disease risk, and type 2 diabetes7–9.
Adolescence represents a pivotal developmental period during which lifestyle habits are established and often persist into adulthood, making it essential to understand how these habits influence subjective health during this formative stage10. Despite this importance, most previous research has focused on investigating subjective health only in adults11,12. Therefore, this study aimed to identify the trend of subjective health status and its association with lifestyle factors and mental health among adolescents. Additionally, we studied the potential impact of the COVID-19 pandemic on adolescent subjective health to understand the changes associated with the pandemic.
Methods
Sample selection and data collection
This study utilized data collected through the Korea Youth Risk Behavior Web-based Survey (KYRBS) over 18 years, 2006–2023. The KYRBS is an anonymous survey conducted annually by the Korean Disease Control and Prevention Agency to assess various health behaviors, including socioeconomic conditions, physical activity, dietary behaviors, alcohol consumption, smoking status, and mental health, among Korean adolescents13,14.
To ensure representative sampling, all middle and high schools nationwide were stratified based on urban, suburban, and rural classifications. The sample maintained a 1:1 ratio of middle schools to high schools. Sample schools were allocated based on urban/rural locations and sex compositions. In total, 800 sample schools were selected nationwide, and the class information of these sample schools was registered to determine the sample classes. A web-based survey at their schools recruited adolescents. Respondents with missing values or incomplete responses were excluded, resulting in a final dataset of 1,190,468 adolescents for this study. The KYRBS data were collected anonymously, and the study protocol received approval from the Institutional Review Board of the Korean Disease Control and Prevention Agency (2014-06EXP-02-P-A). Additionally, the study complied with the Population Health Promotion Act 19 (117058) as mandated by the Korean government. All participants, or their parents or legal guardians in the case of minors, provided written informed consent, and this study adhered to the tenets of the Declaration of Helsinki.
End points
This study investigated the trends in subjective health and its association with socio-demographic and behavioral factors among South Korean adolescents. Considering that the first confirmed case of COVID-19 in South Korea was reported in January 2020, the years from 2020 onwards were considered the pandemic period15.
Subjective health status was assessed by asking, “How do you think your health status compares to your friends?”. The answer options are as follows: ‘very healthy’; ‘healthy’; ‘average’; ‘unhealthy’; and ‘very unhealthy.’ These answers were recategorized into three groups: ‘very healthy’ and ‘healthy’ as high subjective health, ‘average’ as middle subjective health, and ‘unhealthy’ and ‘very unhealthy’ as low subjective health. We compared the trends and factors associated with high subjective health among Korean adolescents before and during the COVID-19 pandemic.
Definition of covariates
The study variables included both socio-demographic and behavioral factors. Socio-demographic factors included sex, grade (middle school [grades 7th -9th ] and high school [grades 10th -12th ]), body mass index (BMI; underweight (< 18.5 kg/m2), normal weight (18.5–22.9 kg/m2), overweight (23–25 kg/m2), and obese (≥ 25.0 kg/m2), academic achievement (high, middle, and low), and household income (high, middle, and low). Behavioral factors included breakfast consumption (rarely, often, and usually), fruit intake (insufficient and sufficient), physical activity (insufficient, moderate, and sufficient), sedentary behavior on weekdays and weekends (rarely, often, and usually), perceived sleep sufficiency (sufficient, moderate, and insufficient), frequency of brushing teeth (usually and rarely), alcohol consumption (no and yes), current smoking status (no and yes), and stress levels (low, moderate, and high). All variables were based on self-reported data. Additional detailed questionnaires and specific categorizations are provided in Supplementary Table 1.
Statistical analysis
This study analyzed KYRBS data to investigate the national trends in subjective health among adolescents during the past 18 years, primarily focusing on the COVID-19 pandemic. The beta coefficients were analyzed using linear regression to the trends of high subjective health before and during the pandemic3. Temporal trends in subjective health were analyzed using joinpoint regression. This method allows for the detection of points where statistically significant changes in trend occur over time. The average annual percentage change (AAPC) for reporting high subjective health was calculated across three time periods: before the pandemic (2016–2019) and during the pandemic (2020–2023), and the overall study period (2006–2023). The joinpoint regression analysis was conducted for the entire sample and stratified by demographical and behavioral variables for a comprehensive exploration of trends across different population subgroups. To compare associations between high subjective health and socio-demographic and behavioral factors before and during the COVID-19 pandemic, adjusted and weighted odds ratios (ORs) were derived using binary logistic regression models. Weighted ORs with 95% confidence intervals (CIs) were calculated after adjusting for the covariates. To assess the magnitude of OR change before and during the pandemic, the ratio of the ORs (ROR) was utilized16. All analyses in this study were performed via R software (version 4.3.2; R Foundation, Vienna, Austria) and Joinpoint Regression Program (version 5.2.0; Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute). Statistical significance was set when a two-sided P-value was less than 0.053,16.
Results
This study consists of 1,190,468 adolescents (female, 48.49%) surveyed by the KYRBS between 2006 and 2023. Table 1 shows the baseline characteristics of the study population.
Table 1.
Crude characteristics of South Korean adolescents, 2006–2023 (N = 1,190,468).
| Variables | Total | Before pandemic | During pandemic |
|---|---|---|---|
| Overall, n | 1,190,468 | 975,950 | 214,518 |
| Subjective health, n (%) | |||
| High | 799,194 (67.13) | 658,319 (67.45) | 140,875 (65.67) |
| Middle | 299,759 (25.18) | 246,011 (25.21) | 53,748 (25.06) |
| Low | 091,515 (7.69) | 071,620 (7.34) | 19,895 (9.27) |
| Sex, n (%) | |||
| Male | 613,153 (51.51) | 503,239 (51.56) | 109,914 (51.24) |
| Female | 577,315 (48.49) | 472,711 (48.44) | 104,604 (48.76) |
| Grade, n (%) | |||
| Middle school (Grades 7–9) | 611,415 (51.36) | 496,026 (50.82) | 115,389 (53.79) |
| High school (Grades 10–12) | 579,053 (48.64) | 479,924 (49.18) | 099,129 (46.21) |
| Breakfast consumption, n (%) | |||
| Rarely (0–2 days per week) | 355,726 (29.88) | 272,084 (27.88) | 83,642 (38.99) |
| Often (3–5 days per week) | 274,314 (23.04) | 217,058 (22.24) | 57,256 (26.69) |
| Usually (6–7 days per week) | 560,428 (47.08) | 486,808 (49.88) | 73,620 (34.32) |
| Fruit intake, n (%) | |||
| Insufficient (not every day) | 754,680 (63.39) | 599,040 (61.38) | 155,640 (72.55) |
| Sufficient (every day) | 435,788 (36.61) | 376,910 (38.62) | 58,878 (27.45) |
| Physical activity, n (%) | |||
| Insufficient (0–2 days per week) | 778,868 (65.43) | 638,932 (65.47) | 139,936 (65.23) |
| Moderate (3–4 days per week) | 243,071 (20.42) | 201,632 (20.66) | 41,439 (19.32) |
| Sufficient (5–7 days per week) | 168,529 (14.16) | 135,386 (13.87) | 33,143 (15.45) |
| Sedentary behavior on weekdays | |||
| Rarely (0–2 h per day) | 469,731 (40.12) | 425,448 (44.32) | 44,283 (21.01) |
| Often (2–4 h per day) | 455,674 (38.92) | 364,536 (37.97) | 91,138 (43.23) |
| Usually (≥ 4 h per day) | 245,409 (20.96) | 170,017 (17.71) | 75,392 (35.76) |
| Sedentary behavior on weekends, n (%) | |||
| Rarely (0–2 h per day) | 244,986 (20.83) | 221,433 (22.93) | 23,553 (11.21) |
| Often (2–4 h per day) | 405,165 (34.46) | 351,352 (36.38) | 53,813 (25.62) |
| Usually (≥ 4 h per day) | 525,706 (44.71) | 393,001 (40.69) | 132,705 (63.17) |
| Perceived sleep sufficiency, n (%) | |||
| Sufficient | 314,119 (26.39) | 258,788 (26.52) | 55,331 (25.79) |
| Moderate | 393,162 (33.03) | 322,149 (33.01) | 71,013 (33.10) |
| Insufficient | 483,187 (40.59) | 395,013 (40.47) | 88,174 (41.10) |
| Frequency of brushing teeth, n (%) | |||
| Usually | 447,446 (37.59) | 391,184 (40.08) | 56,262 (26.23) |
| Rarely | 743,022 (62.41) | 584,766 (59.92) | 158,256 (73.77) |
| Alcohol consumption, n (%) | |||
| No | 973,014 (81.73) | 782,685 (80.20) | 190,329 (88.72) |
| Yes | 217,454 (18.27) | 193,265 (19.80) | 24,189 (11.28) |
| Current smoking status, n (%) | |||
| No | 1,083,058 (90.98) | 877,882 (89.95) | 205,176 (95.65) |
| Yes | 107,410 (9.02) | 98,068 (10.05) | 9,342 (4.35) |
| Academic achievement, n (%) | |||
| High | 437,957 (36.79) | 357,192 (36.60) | 80,765 (37.65) |
| Middle | 334,736 (28.12) | 270,224 (27.69) | 64,512 (30.07) |
| Low | 417,775 (35.09) | 348,534 (35.71) | 69,241 (32.28) |
| Household income, n (%) | |||
| High | 401,802 (33.75) | 314,597 (32.23) | 87,205 (40.65) |
| Middle | 563,062 (47.30) | 461,464 (47.28) | 101,598 (47.36) |
| Low | 225,604 (18.95) | 199,889 (20.48) | 25,715 (11.99) |
| BMI, n (%)* | |||
| Underweight | 284,503 (24.62) | 237,592 (25.10) | 46,911 (22.46) |
| Normal | 605,598 (52.40) | 506,139 (53.46) | 99,459 (47.61) |
| Overweight | 132,655 (11.48) | 105,794 (11.17) | 26,861 (12.86) |
| Obese | 132,882 (11.50) | 097,219 (10.27) | 35,663 (17.07) |
| Stress levels, n (%) | |||
| Low | 34,594 (2.91) | 27,774 (2.85) | 6,820 (3.18) |
| Moderate | 670,794 (56.35) | 544,096 (55.75) | 126,698 (59.06) |
| High | 485,080 (40.75) | 404,080 (41.40) | 81,000 (37.76) |
*According to the Asian–Pacific guidelines, the BMI is divided into four groups: underweight (< 18.5 kg/m2), normal (18.5–22.9 kg/m2), overweight (23.0–24.9 kg/m2), and obese (≥ 25.0 kg/m2).
KYRBS. Korea Youth Risk Behavior Web-based Survey; BMI, body mass index.
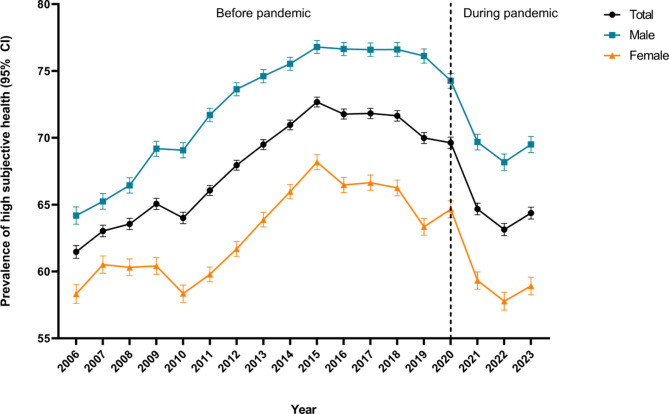
Figure 1; Table 2 present the prevalence and trend of Korean adolescents who reported themselves as healthy, mainly focusing on the COVID-19 pandemic. Before the COVID-19 pandemic, the prevalence of adolescents reporting high subjective health increased from 61.46% (95% CI, 60.98 to 61.93) in 2006 to 69.98% (95% CI, 69.57 to 70.39) in 2019. This trend reversed with the outbreak of the COVID-19 pandemic; it showed a gradual decrease from 69.63% (95% CI, 69.21 to 70.05) in 2020 to 63.13% (95% CI, 62.68 to 63.59) in 2022. However, in 2023, near the end of the pandemic, the prevalence slightly increased to 64.37% (95% CI, 63.92 to 64.81). Additionally, sex-specific trends indicate that male adolescents consistently reported higher subjective health than females throughout the study period.
Fig. 1.
The trend of high subjective health among South Korean adolescents by sex, 2006–2023. Abbreviations: CI, confidence interval.
Table 2.
National trends for reporting high subjective health among South Korean adolescents, 2016–2023.
| Variables | High subjective health trend, β (95% CI) | High subjective health differences, β difference (95% CI)a | |
|---|---|---|---|
| Before the pandemic (2016–2019) | During the pandemic (2020–2023) | ||
| Total | 0.850 (0.645 to 1.055) | -1.732 (-3.654 to 0.189) | -2.582 (-4.514 to -0.649) |
| Sex | |||
| Male | 1.043 (0.835 to 1.252) | -1.579 (-3.409 to 0.250) | -2.623 (-4.465 to -0.781) |
| Female | 0.655 (0.388 to 0.922) | -1.874 (-3.886 to 0.139) | -2.529 (-4.559 to -0.499) |
| Grade | |||
| Middle school (Grades 7–9) | 1.055 (0.794 to 1.316) | -1.381 (-3.341 to 0.579) | -2.436 (-4.413 to -0.458) |
| High school (Grades 10–12) | 0.733 (0.548 to 0.917) | -2.138 (-4.120 to -0.156) | -2.871 (-4.862 to -0.881) |
| Breakfast consumption | |||
| Rarely (0–2 days per week) | 0.876 (0.664 to 1.088) | -1.647 (-3.881 to 0.587) | -2.523 (-4.767 to -0.279) |
| Often (3–5 days per week) | 0.778 (0.590 to 0.965) | -1.663 (-3.719 to 0.393) | -2.441 (-4.505 to -0.377) |
| Usually (6–7 days per week) | 1.021 (0.814 to 1.228) | -1.647 (-3.136 to -0.157) | -2.668 (-4.172 to -1.164) |
| Fruit intake | |||
| Insufficient (not every day) | 0.977 (0.721 to 1.233) | -1.830 (-3.883 to 0.224) | -2.807 (-4.876 to -0.738) |
| Sufficient (every day) | 1.049 (0.845 to 1.252) | -1.291 (-2.978 to 0.395) | -2.340 (-4.039 to -0.641) |
| Physical activity | |||
| Insufficient (0–2 days per week) | 0.760 (0.551 to 0.969) | -2.584 (-4.446 to -0.723) | -3.344 (-5.218 to -1.471) |
| Moderate (3–4 days per week) | 0.885 (0.755 to 1.014) | -2.462 (-4.562 to -0.361) | -3.346 (-5.451 to -1.242) |
| Sufficient (5–7 days per week) | 0.731 (0.587 to 0.875) | -1.955 (-3.248 to -0.662) | -2.686 (-3.987 to -1.385) |
| Sedentary behavior on weekdays | |||
| Rarely (0–2 h per day) | 0.796 (0.592 to 1.000) | -1.618 (-3.069 to -0.167) | -2.414 (-3.880 to -0.949) |
| Often (2–4 h per day) | 0.958 (0.751 to 1.165) | -1.736 (-3.625 to 0.153) | -2.694 (-4.594 to -0.794) |
| Usually (≥ 4 h per day) | 1.192 (0.886 to 1.497) | -1.980 (-4.660 to 0.700) | -3.172 (-5.869 to -0.474) |
| Sedentary behavior on weekends | |||
| Rarely (0–2 h per day) | 0.645 (0.393 to 0.897) | -1.305 (-3.182 to 0.572) | -1.950 (-3.844 to -0.057) |
| Often (2–4 h per day) | 1.029 (0.789 to 1.269) | -1.689 (-3.001 to -0.378) | -2.719 (-4.052 to -1.385) |
| Usually (≥ 4 h per day) | 0.850 (0.645 to 1.055) | -1.732 (-3.654 to 0.189) | -2.582 (-4.514 to -0.649) |
| Perceived sleep sufficiency | |||
| Sufficient | 0.900 (0.687 to 1.113) | -1.684 (-3.644 to 0.276) | -2.584 (-4.556 to -0.613) |
| Moderate | 0.575 (0.395 to 0.755) | -2.035 (-3.523 to -0.548) | -2.610 (-4.109 to -1.112) |
| Insufficient | 1.304 (1.018 to 1.591) | -1.455 (-3.382 to 0.472) | -2.759 (-4.707 to -0.812) |
| Frequency of brushing teeth | |||
| Usually | 0.712 (0.477 to 0.947) | -1.864 (-4.268 to 0.540) | -2.576 (-4.991 to -0.160) |
| Rarely | 0.450 (0.223 to 0.677) | -1.912 (-3.966 to 0.142) | -2.362 (-4.429 to -0.295) |
| Alcohol consumption | |||
| No | 0.900 (0.687 to 1.113) | -1.684 (-3.644 to 0.276) | -2.584 (-4.556 to -0.613) |
| Yes | 0.575 (0.395 to 0.755) | -2.035 (-3.523 to -0.548) | -2.610 (-4.109 to -1.112) |
| Current smoking status | |||
| No | 0.831 (0.651 to 1.012) | -1.316 (-3.046 to 0.415) | -2.147 (-3.887 to -0.407) |
| Yes | 0.623 (0.398 to 0.848) | -2.216 (-3.906 to -0.525) | -2.839 (-4.544 to -1.133) |
| Academic achievement | |||
| High | 1.033 (0.790 to 1.276) | -1.767 (-3.098 to -0.436) | -2.800 (-4.153 to -1.447) |
| Middle | 0.772 (0.554 to 0.989) | -1.591 (-3.866 to 0.684) | -2.363 (-4.648 to -0.077) |
| Low | 0.627 (0.428 to 0.826) | -1.928 (-4.412 to 0.556) | -2.555 (-5.047 to -0.063) |
| Household income | |||
| High | 0.745 (0.532 to 0.958) | -1.907 (-3.441 to -0.374) | -2.652 (-4.201 to -1.104) |
| Middle | 0.712 (0.477 to 0.947) | -1.864 (-4.268 to 0.540) | -2.576 (-4.991 to -0.160) |
| Low | 0.450 (0.223 to 0.677) | -1.912 (-3.966 to 0.142) | -2.362 (-4.429 to -0.295) |
| BMIb | |||
| Underweight | 1.304 (1.018 to 1.591) | -1.455 (-3.382 to 0.472) | -2.759 (-4.707 to -0.812) |
| Normal | 0.831 (0.651 to 1.012) | -1.316 (-3.046 to 0.415) | -2.147 (-3.887 to -0.407) |
| Overweight | 0.623 (0.398 to 0.848) | -2.216 (-3.906 to -0.525) | -2.839 (-4.544 to -1.133) |
| Obese | 0.536 (0.341 to 0.730) | -2.848 (-5.121 to -0.575) | -3.384 (-5.665 to -1.103) |
| Stress levels | |||
| Low | 0.536 (0.341 to 0.730) | -2.848 (-5.121 to -0.575) | -3.384 (-5.665 to -1.103) |
| Moderate | 0.876 (0.664 to 1.088) | -1.647 (-3.881 to 0.587) | -2.523 (-4.767 to -0.279) |
| High | 0.778 (0.590 to 0.965) | -1.663 (-3.719 to 0.393) | -2.441 (-4.505 to -0.377) |
aEstimated β was calculated using weighted linear regression and the difference of β (βdiff) was conducted to analyze the trend changes between before (reference) and during the COVID-19 pandemic.
bAccording to the Asian–Pacific guidelines, the BMI is divided into four groups: underweight (< 18.5 kg/m2), normal (18.5–22.9 kg/m2), overweight (23.0–24.9 kg/m2), and obese (≥ 25.0 kg/m2).
BMI, body mass index; CI, confidence interval.
Significant values are in [bold].
Table 3 presents the AAPC for high subjective health reporting analyzed through joinpoint regression analysis. Before the COVID-19 pandemic, the total AAPC was 0.96 (95% CI, 0.75 to 1.24), indicating a steady increase in subjective health. However, during the pandemic, the AAPC shifted to -2.51 (95% CI, -3.73 to -1.69), signifying a decline. Stratified analysis by sex showed that males had an AAPC of 0.47 (95% CI, 0.14 to 0.87) before the pandemic and − 2.47 (95% CI, -3.61 to -1.72) during the pandemic. Females experienced a greater decrease during the pandemic with an AAPC of -1.96 (95% CI, -2.80 to -1.30).
Table 3.
Average annual percentage change for reporting high subjective health among South Korean adolescents, 2006–2023.
| Variables | AAPC before the pandemic, (95% CI) (2006–2019) | AAPC during the pandemic, (95% CI) (2020–2023) |
AAPC, (95% CI) (2006–2023) |
|---|---|---|---|
| Total | 0.96 (0.75 to 1.24) | -2.51 (-3.73 to -1.69) | 0.13 (-0.15 to 0.38) |
| Sex | |||
| Male | 0.47 (0.14 to 0.87) | -2.47 (-3.61 to -1.72) | 0.35 (0.10 to 0.60) |
| Female | 0.90 (0.72 to 1.08) | -1.96 (-2.80 to -1.30) | -0.11 (-0.44 to 0.23) |
| Grade | |||
| Middle school (Grades 7–9) | 1.00 (0.77 to 1.31) | -3.01 (-4.21 to -2.10) | 0.13 (-0.14 to 0.40) |
| High school (Grades 10–12) | 1.05 (0.83 to 1.37) | -2.75 (-3.95 to -1.72) | 0.10 (-0.18 to 0.38) |
| Breakfast consumption | |||
| Rarely (0–2 days per week) | 1.06 (0.83 to 1.38) | -2.56 (-3.71 to -1.70) | 0.19 (-0.07 to 0.48) |
| Often (3–5 days per week) | 0.99 (0.75 to 1.34) | -2.04 (-3.44 to -1.14) | 0.26 (-0.04 to 0.57) |
| Usually (6–7 days per week) | 1.23 (1.00 to 1.50) | -2.10 (-3.29 to -1.25) | 0.44 (0.17 to 0.68) |
| Fruit intake | |||
| Insufficient (not every day) | 1.13 (0.91 to 1.44) | -2.11 (-2.92 to -1.45) | 0.36 (0.11 to 0.64) |
| Sufficient (every day) | 1.23 (1.03 to 1.44) | -2.20 (-3.24 to -1.44) | 0.41 (0.18 to 0.59) |
| Physical activity | |||
| Insufficient (0–2 days per week) | 1.05 (0.83 to 1.37) | -3.64 (-4.90 to -2.68) | -0.07 (-0.38 to 0.20) |
| Moderate (3–4 days per week) | 1.11 (0.87 to 1.35) | -3.20 (-4.02 to -2.34) | 0.08 (-0.13 to 0.28) |
| Sufficient (5–7 days per week) | 0.80 (0.67 to 1.01) | -2.03 (-2.77 to -1.49) | 0.13 (-0.05 to 0.29) |
| Sedentary behavior on weekdays | |||
| Rarely (0–2 h per day) | 0.90 (0.72 to 1.08) | -2.64 (-3.69 to -1.90) | 0.06 (-0.18 to 0.22) |
| Often (2–4 h per day) | 1.16 (0.95 to 1.46) | -2.15 (-3.29 to -1.36) | 0.37 (0.11 to 0.63) |
| Usually (≥ 4 h per day) | 1.64 (1.21 to 2.58) | -2.34 (-5.66 to -0.71) | 0.69 (0.02 to 1.48) |
| Sedentary behavior on weekends | |||
| Rarely (0–2 h per day) | 0.63 (0.36 to 0.87) | -3.21 (-4.80 to -2.14) | -0.29 (-0.66 to -0.06) |
| Often (2–4 h per day) | 1.07 (0.79 to 1.46) | -2.66 (-4.42 to -1.72) | 0.18 (-0.24 to 0.51) |
| Usually (≥ 4 h per day) | 1.67 (1.37 to 2.09) | -1.75 (-2.71 to -0.98) | 0.85 (0.56 to 1.23) |
| Perceived sleep sufficiency | |||
| Sufficient | 1.25 (1.11 to 1.44) | -2.03 (-2.75 to -1.50) | 0.47 (0.32 to 0.63) |
| Moderate | 1.16 (0.96 to 1.41) | -2.32 (-3.39 to -1.51) | 0.33 (0.08 to 0.57) |
| Insufficient | 0.67 (0.53 to 0.84) | -3.16 (-3.80 to -2.77) | -0.24 (-0.40 to -0.12) |
| Frequency of brushing teeth | |||
| Usually | 0.91 (0.70 to 1.17) | -2.04 (-3.40 to -1.20) | 0.21 (-0.12 to 0.46) |
| Rarely | 0.98 (0.81 to 1.20) | -2.17 (-2.87 to -1.57) | 0.23 (0.04 to 0.44) |
| Alcohol consumption | |||
| No | 1.01 (0.79 to 1.33) | -2.59 (-3.94 to -1.71) | 0.15 (-0.15 to 0.43) |
| Yes | 0.61 (0.41 to 0.84) | -2.42 (-3.81 to -1.53) | -0.11 (-0.43 to 0.12) |
| Current smoking status | |||
| No | 0.94 (0.76 to 1.18) | -1.96 (-2.73 to -1.37) | 0.25 (0.03 to 0.48) |
| Yes | 0.68 (0.46 to 0.89) | -4.09 (-5.54 to -3.27) | -0.46 (-0.84 to -0.27) |
| Academic achievement | |||
| High | 1.26 (1.10 to 1.49) | -2.47 (-3.40 to -1.90) | 0.37 (0.17 to 0.55) |
| Middle | 0.83 (0.61 to 1.19) | -1.89 (-3.12 to -1.12) | 0.19 (-0.15 to 0.50) |
| Low | 0.72 (0.47 to 1.04) | -2.79 (-4.33 to -1.75) | -0.12 (-0.45 to 0.18) |
| Household income | |||
| High | 0.86 (0.65 to 1.07) | -2.73 (-3.49 to -1.90) | 0.01 (-0.18 to 0.19) |
| Middle | 0.72 (0.52 to 0.98) | -2.39 (-3.33 to -1.69) | -0.02 (-0.29 to 0.23) |
| Low | 0.48 (0.23 to 0.76) | -1.97 (-3.07 to -1.26) | -0.10 (-0.46 to 0.18) |
| BMI* | |||
| Underweight | 1.67 (1.44 to 1.95) | -2.71 (-3.95 to -1.94) | 0.62 (0.29 to 0.84) |
| Normal | 0.96 (0.78 to 1.19) | -1.86 (-2.93 to -1.17) | 0.29 (0.04 to 0.49) |
| Overweight | 0.59 (0.37 to 0.85) | -2.44 (-3.46 to -1.76) | -0.13 (-0.41 to 0.08) |
| Obese | 0.65 (0.32 to 1.12) | -3.88 (-6.15 to -2.51) | -0.44 (-0.85 to -0.05) |
| Stress levels | |||
| Low | 1.12 (0.90 to 1.49) | -2.07 (-2.88 to -1.34) | 0.36 (0.14 to 0.64) |
| Moderate | 0.98 (0.77 to 1.32) | -2.38 (-3.44 to -1.68) | 0.18 (-0.06 to 0.44) |
| High | 0.44 (0.21 to 0.73) | -2.50 (-3.69 to -1.71) | -0.26 (-0.59 to 0.01) |
*According to the Asian–Pacific guidelines, the BMI is divided into four groups: underweight (< 18.5 kg/m2), normal (18.5–22.9 kg/m2), overweight (23.0–24.9 kg/m2), and obese (≥ 25.0 kg/m2).
AAPC, Average annual percentage change; BMI, body mass index; CI, confidence interval.
Significant values are in [bold].
The association between socio-demographic and behavioral factors and high subjective health is depicted in Table 4. Among socio-demographic factors, female sex (OR, 0.96 [95% CI, 0.96 to 0.96]; reference, male), low academic achievement (OR, 0.96 [95% CI, 0.96 to 0.97]; reference, high), low household income (OR, 0.90 [95% CI, 0.89 to 0.90]; reference, high), and obesity (OR, 0.96 [95% CI, 0.95 to 0.96]; reference, underweight) were associated with a lower likelihood of reporting high subjective health before the COVID-19 pandemic. The pandemic contributes to a further decrease in subjective health among individuals with the following socio-demographic factors: female sex (ROR, 0.85 [95% CI, 0.83 to 0.87]), low academic achievement (ROR, 0.83 [95% CI, 0.81 to 0.85]), low household income (ROR, 0.67 [95% CI, 0.64 to 0.69]), and obesity (ROR, 0.78 [95% CI, 0.75 to 0.81]).
Table 4.
Adjusted and weighted odds ratios and ratio of odds ratios for the association between behavioral and sociodemographic factors and high subjective health.
| Variables | Before the pandemic (2016–2019) | During the pandemic (2020–2023) | Ratio of ORs (95% CI) during the pandemic compared to before the pandemic (reference) | |||
|---|---|---|---|---|---|---|
| Weighted OR (95% CI) | p-value | Weighted OR (95% CI) | p-value | Weighted ratio of ORs (95% CI) | p-value | |
| Sex | ||||||
| Male | 1 (ref) | 1 (ref) | 1 (ref) | |||
| Female | 0.96 (0.96 to 0.96) | < 0.001 | 0.81 (0.79 to 0.83) | < 0.001 | 0.85 (0.83 to 0.87) | < 0.001 |
| Grade | ||||||
| Middle school (Grades 7–9) | 1 (ref) | 1 (ref) | 1 (ref) | |||
| High school (Grades 10–12) | 0.97 (0.96 to 0.97) | < 0.001 | 0.98 (0.96 to 1.00) | 0.067 | 1.01 (0.99 to 1.04) | 0.295 |
| Breakfast consumption | ||||||
| Rarely (0–2 days per week) | 1 (ref) | 1 (ref) | 1 (ref) | |||
| Often (3–5 days per week) | 1.00 (1.00 to 1.01) | 0.784 | 1.02 (0.99 to 1.05) | 0.171 | 1.02 (0.99 to 1.05) | 0.197 |
| Usually (6–7 days per week) | 1.02 (1.02 to 1.03) | < 0.001 | 1.16 (1.13 to 1.19) | < 0.001 | 1.13 (1.10 to 1.16) | < 0.001 |
| Fruit intake | ||||||
| Insufficient (not every day) | 1 (ref) | 1 (ref) | 1 (ref) | |||
| Sufficient (every day) | 1.02 (1.02 to 1.03) | < 0.001 | 1.14 (1.11 to 1.17) | < 0.001 | 1.12 (1.09 to 1.15) | < 0.001 |
| Physical activity | ||||||
| Insufficient (0–2 days per week) | 1 (ref) | 1 (ref) | 1 (ref) | |||
| Moderate (3–4 days per week) | 1.09 (1.08 to 1.09) | < 0.001 | 1.56 (1.52 to 1.61) | < 0.001 | 1.44 (1.39 to 1.48) | < 0.001 |
| Sufficient (5–7 days per week) | 1.14 (1.13 to 1.14) | < 0.001 | 2.30 (2.22 to 2.38) | < 0.001 | 2.02 (1.95 to 2.09) | < 0.001 |
| Sedentary behavior on weekdays | ||||||
| Rarely (0–2 h per day) | 1 (ref) | 1 (ref) | 1 (ref) | |||
| Often (2–4 h per day) | 1.00 (1.00 to 1.01) | 0.232 | 1.04 (1.00 to 1.07) | 0.030 | 1.03 (1.00 to 1.07) | 0.048 |
| Usually (≥ 4 h per day) | 0.99 (0.98 to 0.99) | < 0.001 | 0.99 (0.95 to 1.02) | 0.450 | 1.00 (0.96 to 1.04) | 0.956 |
| Sedentary behavior on weekends | ||||||
| Rarely (0–2 h per day) | 1 (ref) | 1 (ref) | 1 (ref) | |||
| Often (2–4 h per day) | 1.01 (1.00 to 1.02) | 0.001 | 1.07 (1.03 to 1.12) | < 0.001 | 1.06 (1.02 to 1.11) | 0.005 |
| Usually (≥ 4 h per day) | 0.99 (0.98 to 0.99) | < 0.001 | 0.98 (0.94 to 1.02) | 0.421 | 1.00 (0.96 to 1.04) | 0.831 |
| Perceived sleep sufficiency | ||||||
| Sufficient | 1 (ref) | 1 (ref) | 1 (ref) | |||
| Moderate | 0.95 (0.95 to 0.96) | < 0.001 | 0.68 (0.66 to 0.70) | < 0.001 | 0.71 (0.69 to 0.74) | < 0.001 |
| Insufficient | 0.90 (0.89 to 0.90) | < 0.001 | 0.49 (0.48 to 0.51) | < 0.001 | 0.55 (0.53 to 0.56) | < 0.001 |
| Frequency of brushing teeth | ||||||
| Usually | 1 (ref) | 1 (ref) | 1 (ref) | |||
| Rarely | 0.98 (0.98 to 0.98) | < 0.001 | 0.87 (0.85 to 0.90) | < 0.001 | 0.89 (0.87 to 0.91) | < 0.001 |
| Alcohol consumption | ||||||
| No | 1 (ref) | 1 (ref) | 1 (ref) | |||
| Yes | 1.01 (1.01 to 1.02) | < 0.001 | 1.06 (1.02 to 1.10) | 0.002 | 1.05 (1.01 to 1.09) | 0.014 |
| Current smoking status | ||||||
| No | 1 (ref) | 1 (ref) | 1 (ref) | |||
| Yes | 1.00 (1.00 to 1.01) | 0.293 | 1.04 (0.98 to 1.11) | 0.147 | 1.04 (0.98 to 1.10) | 0.204 |
| Academic achievement | ||||||
| High | 1 (ref) | 1 (ref) | 1 (ref) | |||
| Middle | 0.99 (0.98 to 0.99) | < 0.001 | 0.93 (0.91 to 0.96) | < 0.001 | 0.94 (0.92 to 0.97) | < 0.001 |
| Low | 0.96 (0.96 to 0.97) | < 0.001 | 0.80 (0.78 to 0.82) | < 0.001 | 0.83 (0.81 to 0.85) | < 0.001 |
| Household income | ||||||
| High | 1 (ref) | 1 (ref) | 1 (ref) | |||
| Middle | 0.95 (0.94 to 0.95) | < 0.001 | 0.73 (0.71 to 0.75) | < 0.001 | 0.77 (0.75 to 0.79) | < 0.001 |
| Low | 0.90 (0.89 to 0.90) | < 0.001 | 0.60 (0.58 to 0.62) | < 0.001 | 0.67 (0.64 to 0.69) | < 0.001 |
| BMI* | ||||||
| Underweight | 1 (ref) | 1 (ref) | 1 (ref) | |||
| Normal | 1.04 (1.04 to 1.05) | < 0.001 | 1.33 (1.29 to 1.37) | < 0.001 | 1.27 (1.24 to 1.31) | < 0.001 |
| Overweight | 1.03 (1.02 to 1.03) | < 0.001 | 1.19 (1.14 to 1.23) | < 0.001 | 1.16 (1.11 to 1.20) | < 0.001 |
| Obese | 0.96 (0.95 to 0.96) | < 0.001 | 0.75 (0.72 to 0.77) | < 0.001 | 0.78 (0.75 to 0.81) | < 0.001 |
| Stress levels | ||||||
| Low | 1 (ref) | 1 (ref) | 1 (ref) | |||
| Moderate | 0.95 (0.94 to 0.95) | < 0.001 | 0.53 (0.49 to 0.58) | < 0.001 | 0.56 (0.52 to 0.61) | < 0.001 |
| High | 0.83 (0.82 to 0.83) | < 0.001 | 0.28 (0.25 to 0.30) | < 0.001 | 0.33 (0.31 to 0.36) | < 0.001 |
*According to the Asian–Pacific guidelines, the BMI is divided into four groups: underweight (< 18.5 kg/m2), normal (18.5–22.9 kg/m2), overweight (23.0–24.9 kg/m2), and obese (≥ 25.0 kg/m2).
BMI, body mass index; CI, confidence interval; OR, odds ratio; ROR, ratio of odds ratio.
Significant values are in [bold].
Regarding behavioral factors, regular breakfast consumption (usually; OR, 1.16 [95% CI, 1.13 to 1.19]; reference, rarely), sufficient fruit intake (sufficient; OR, 1.14 [95% CI, 1.11 to 1.17]; reference, insufficient), and sufficient vigorous physical activity (sufficient; OR, 2.30 [95% CI, 2.22 to 2.38]; reference, insufficient) were positively associated with high subjective health. During the pandemic, individuals with these behaviors exhibited a stronger positive association with subjective health: breakfast consumption (ROR, 1.13 [95% CI, 1.10 to 1.16]), sufficient fruit intake (ROR, 1.12 [95% CI, 1.09 to 1.15]), sufficient vigorous physical activity (ROR, 2.02; [95% CI, 1.95 to 2.09]), and alcohol consumption (ROR, 1.05; [95% CI, 1.01 to 1.09]). Conversely, insufficient sleep (OR, 0.49 [95% CI, 0.48 to 0.51]; reference, insufficient), rarely brushing teeth (OR, 0.87 [95% CI, 0.85 to 0.90]; reference, usually), and high-stress levels (OR, 0.28 [95% CI, 0.25 to 0.30]; reference, low) were associated with a decreased likelihood of high subjective health, with this negative impact being more pronounced during the pandemic: insufficient sleep (ROR, 0.55 [95% CI, 0.53 to 0.56]), rarely brushing teeth (ROR, 0.89 [95% CI, 0.87 to 0.91]), and high-stress levels (ROR, 0.33 [95% CI, 0.31 to 0.36]).
Discussion
Key findings
This study analyzed 18-year trends in subjective health and its association with demographic and behavioral factors using a nationally representative cohort of South Korean adolescents, including the COVID-19 pandemic era, and yielded several key findings. The prevalence of adolescents reporting high subjective health increased before the COVID-19 pandemic; however, this trend reversed during the early and mid-pandemic (2020–2022). Subsequently, in the late-pandemic period (2023), it slightly increased. AAPC before the COVID-19 pandemic showed consistent improvement in subjective health status, however, the decline observed during the COVID-19 pandemic in all demographic groups highlights the widespread impact of the global health crisis on perceived health. Socio-demographic factors such as female sex, low academic achievement, low household income, and obese BMI were consistently associated with a lower likelihood of reporting high subjective health. Conversely, positive behavioral factors, such as regular breakfast consumption, sufficient fruit intake, sufficient physical activity, sufficient sleep, usually brushing teeth, and low stress levels, were associated with higher subjective health. These associations became more pronounced during the pandemic, suggesting that healthy lifestyle choices may have offered resilience against its challenges.
Comparison with previous studies
Previous studies have documented the importance of a healthy lifestyle for improving and maintaining physical and mental health. However, many of these studies have been limited by relatively small sample sizes, such as those conducted in Belgium (n = 6,054)17, South Korea (n = 7,700)18, and China (n = 161,744)19, leading at times to inconclusive evidence and controversial findings. In contrast, our study utilized large, population-based national data to examine trends and associated factors in self-rated health, offering more robust and generalizable results. This approach provides a clearer understanding of the determinants of adolescent subjective health.
In comparison with previous studies, several investigations corroborate our main findings regarding the detrimental impact of the COVID-19 pandemic on subjective health across diverse populations. Specifically, a Polish study found that COVID-19 convalescents who experienced symptomatic manifestations exhibited a higher propensity for developing nervousness, tension, and anxiety compared to those with milder symptomatology, with female and younger participants demonstrating particular vulnerability to post-recovery psychological distress20 Furthermore, a longitudinal cohort investigation of older individuals in England documented a systematic deterioration in mental health and well-being, characterized by persistent socioeconomic inequities, predominantly affecting women and non-partnered people21. Moreover, research conducted in the Netherlands established that lockdown measures exerted differential impacts on individuals with chronic conditions and urban residents, resulting in diminished self-reported health status22. These investigations collectively substantiate our findings by elucidating how sociodemographic variables influenced the varying degrees of subjective health deterioration across distinct population segments during the pandemic period.
Plausible mechanisms
Before the COVID-19 pandemic, there was an increase in the percentage of adolescents reporting high subjective health, potentially due to South Korea’s economic growth. Economic growth has been associated with better nutrition, enhanced public health infrastructure, and more effective medical technology, leading to improved public health23,24. The steady increase in South Korea’s gross domestic product before the pandemic likely contributed to the rising trend in subjective health. However, the COVID-19 pandemic led to a decline in subjective health, likely due to reduced socialization opportunities from lockdowns and stay-at-home orders25. Increased consumption of substances like alcohol and tobacco during the pandemic exacerbated this decline26,27. Remote learning and increased time at home disrupted regular routines, leading to more sedentary behavior and a preference for quick, unhealthy foods over balanced meals28.
The mechanisms underlying the decline in subjective health during the pandemic can be linked to the interruption of positive health behaviors and routines. School closures and social distancing measures limited access to healthy meals and physical activity opportunities provided by schools29. Increased screen time and lack of structured schedules contributed to poor sleep hygiene and higher stress levels. The pandemic’s economic impact disproportionately affected low-income families, exacerbating existing health disparities. Additionally, the social isolation resulting from lockdowns had a profound effect on mental health, particularly among adolescents who rely heavily on peer interactions for emotional support30.
According to previous research, significant gender differences have been observed in physical activity, with males more frequently meeting the World Health Organization’s guidelines, which recommend engaging in at least 60 min of moderate-to-vigorous physical activity daily31. Adequate physical activity is strongly associated with lower stress levels and a healthier BMI, which may help explain the consistently lower subjective health reported among adolescent females compared to males32,33.
Understanding these mechanisms is crucial for developing comprehensive policies that address both immediate and long-term health challenges adolescents face. School-based nutritional programs, mental health services, physical activity promotion, and economic policies supporting low-income families are necessary to mitigate the adverse effects of such crises34. Furthermore, the lower odds of females reporting high subjective health, further reduced by the pandemic, suggest a need for sex-specific health interventions to address the unique challenges faced by female adolescents.
Policy implications
Adolescence is a critical stage marked by significant physical and psychological changes, necessitating efforts to promote mental health and well-being35. The decline in subjective health among adolescents during the COVID-19 pandemic is alarming, requiring targeted policies to restore previous levels of subjective health, particularly for those with vulnerable demographics36. Key recommendations include implementing school-based nutritional programs that provide healthy meals, promoting oral hygiene, encouraging physical activity through school and community initiatives, enhancing access to mental health services and stress management programs, promoting good sleep hygiene, and providing additional educational support such as tutoring and mentoring to improve academic performance and health perceptions16,37.
Strengths and limitations
This study has multiple strengths. First, we used large-scale, population-based, nationwide data on adolescents to examine trends in subjective health before and during the COVID-19 pandemic. Second, despite the challenges of collecting individual data during the COVID-19 pandemic, our analysis was based on data gathered through non-face-to-face methods unaffected by the COVID-19 pandemic. Third, unlike objective health, subjective health encompasses unquantified aspects of well-being, thereby broadening the scope of research.
However, this study has several limitations. First, the data were collected only from the South Korean adolescent population, so the findings may not apply to other regions of the world due to cultural differences and variations in countries’ responses to the COVID-19 pandemic. Large-scale international research is required to find global associations between adolescents’ subjective health and the COVID-19 pandemic. Second, because only adolescents attending school were allowed to participate, the sample might not represent all Korean youth between the ages of 12 and 18 years. However, only approximately 1.8% of those between the ages of 12 and 18 do not attend school in Korea. Third, a self-report questionnaire was used to collect information about adolescents’ subjective health, which may underestimate the prevalence of these issues due to reporting bias38.
Conclusion
We examined 18-year trends in subjective health among South Korean adolescents by various socio-demographic and behavioral factors using a large nationally representative dataset. Our study found that before the pandemic, subjective health was steadily improving. However, during the pandemic, we observed a decline in subjective health. In particular, adolescents who were female, from low-income households, and had low academic achievement had lower subjective health, with disparities worsening during the pandemic. Conversely, adolescents with healthy behavioral factors, such as regular breakfast consumption and sufficient physical activity, had higher subjective health status before and during the COVID-19 pandemic. Our findings clearly display the association between socio-demographic and behavioral factors on adolescent health disparities and highlight the importance of developing policies to address health inequalities.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
DKY had full access to all data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. All authors have approved the final version of the manuscript before submission. Study concept and design: Jaehyun Kong, SH, Seunghwan Lee, SW, and DKY; Acquisition, analysis, or interpretation of data: Jaehyun Kong, SH, Seunghwan Lee, SW, and DKY; Drafting of the manuscript: Jaehyun Kong, SH, Seunghwan Lee, SW, and DKY; Critical revision of the manuscript for important intellectual content: all authors; Statistical analysis: Jaehyun Kong, SH, Seunghwan Lee, SW, and DKY; Study supervision: DKY. DKY supervised the study and served as the guarantor. Jaehyun Kong, SH, and Seunghwan Lee contributed equally as the first authors. DKY and SW contributed equally as corresponding authors. The corresponding author attests that all listed authors meet the authorship criteria, and others not meeting the criteria have been omitted.
Funding
This research was supported by the National Research Foundation of Korea (NRF) grants funded by the Korean Government (MSIT; RS-2023-00248157) and the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Education (RS-2024-00460379). The funders had no role in the study design, data collection, data analysis, data interpretation, or manuscript writing.
Data availability
The data are available upon request. Study protocol and statistical code: Available from DKY (yonkkang@gmail.com). Dataset: Available from the Korea Disease Control and Prevention Agency through a data use agreement. Data from the Korea Youth Risk Behavior Web-based Survey can be accessed via the following link: https://www.kdca.go.kr/yhs/.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Selin Woo and Dong KeonYon jointly supervised this work.
Jaehyun Kong, Seohyun Hong, and Seunghwan Lee contributed equally to this work.
Contributor Information
Selin Woo, Email: dntpfls@naver.com.
Dong Keon Yon, Email: yonkkang@gmail.com.
References
- 1.Schulz, P. J., Pessina, A., Hartung, U. & Petrocchi, S. Effects of objective and subjective health literacy on patients’ accurate judgment of health information and decision-making ability: Survey study. J. Med. Internet Res.23, e20457. 10.2196/20457 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.LaCaille, L. J., Hooker, S. A., Marshall, E., LaCaille, R. A. & Owens, R. Change in perceived stress and health behaviors of emerging adults in the midst of the COVID-19 pandemic. Ann. Behav. Med.55, 1080–1088. 10.1093/abm/kaab074 (2021). [DOI] [PubMed] [Google Scholar]
- 3.Oh, J. et al. National trends in the prevalence of screen time and its association with biopsychosocial risk factors among Korean adolescents, 2008–2021. J. Adolesc. Health74, 504–513. 10.1016/j.jadohealth.2023.10.021 (2024). [DOI] [PubMed] [Google Scholar]
- 4.Tanaka, S., Muraki, S., Inoue, Y., Miura, K. & Imai, E. The association between subjective health perception and lifestyle factors in Shiga prefecture, Japan: A cross-sectional study. BMC Public Health20, 1786. 10.1186/s12889-020-09911-y (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Inoue, S., Watanabe, J. & Wada, Y. Subjective health awareness and sensory ability of taste and olfaction: A case study of a health promotion class for older people. PLoS One17, e0275093. 10.1371/journal.pone.0275093 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li, Y. et al. Impact of healthy lifestyle factors on life expectancies in the US population. Circulation138, 345–355. 10.1161/circulationaha.117.032047 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jahromi, M. K. et al. The association of healthy lifestyle score and risk of non-alcoholic fatty liver disease. BMC Public. Health23, 973. 10.1186/s12889-023-15816-3 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li, Y. et al. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: Prospective cohort study. Bmj368, l6669. 10.1136/bmj.l6669 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rassy, N. et al. Association of healthy lifestyle factors and obesity-related diseases in adults in the UK. JAMA Netw. Open6, e2314741. 10.1001/jamanetworkopen.2023.14741 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baird, S. et al. Realising transformative change in adolescent health and wellbeing: A second Lancet Commission. Lancet400, 545–547. 10.1016/s0140-6736(22)01529-x (2022). [DOI] [PubMed] [Google Scholar]
- 11.Viljanen, A. et al. Subjective and objective health predicting mortality and institutionalization: An 18-year population-based follow-up study among community-dwelling Finnish older adults. BMC Geriatr.21, 358. 10.1186/s12877-021-02311-w (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bishwajit, G. et al. Subjective health, and quality of life among Chinese men living with type 2 diabetes. Am. J. Mens Health11, 357–364. 10.1177/1557988316681128 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim, Y. et al. Data resource profile: The Korea youth risk behavior web-based survey (KYRBS). Int. J. Epidemiol.45, 1076–1076. 10.1093/ije/dyw070 (2016). [DOI] [PubMed] [Google Scholar]
- 14.Hong, S. et al. National prevalence of smoking among adolescents at tobacco tax increase and COVID-19 pandemic in South Korea, 2005–2022. Sci. Rep.14, 7823. 10.1038/s41598-024-58446-4 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park, S. et al. National trends in physical activity among adults in South Korea before and during the COVID-19 pandemic, 2009–2021. JAMA Netw. Open.6, e2316930. 10.1001/jamanetworkopen.2023.16930 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oh, J. et al. Hand and oral hygiene practices of south Korean adolescents before and during the COVID-19 pandemic. JAMA Netw. Open6, e2349249. 10.1001/jamanetworkopen.2023.49249 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hautekiet, P. et al. A healthy lifestyle is positively associated with mental health and well-being and core markers in ageing. BMC Med.20, 328. 10.1186/s12916-022-02524-9 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nari, F., Jeong, W., Jang, B. N., Lee, H. J. & Park, E. C. Association between healthy lifestyle score changes and quality of life and health-related quality of life: A longitudinal analysis of South Korean panel data. BMJ Open11, e047933. 10.1136/bmjopen-2020-047933 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Qin, N. et al. Associations between healthy lifestyle behavioral patterns and mental health problems: A latent class analysis of 161,744 Chinese young adults. J. Affect. Disord.347, 414–421. 10.1016/j.jad.2023.11.087 (2024). [DOI] [PubMed] [Google Scholar]
- 20.Moniuszko-Malinowska, A. et al. COVID-19 pandemic influence on self-reported health status and well-being in a society. Sci. Rep.12, 8767. 10.1038/s41598-022-12586-7 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zaninotto, P., Iob, E., Demakakos, P. & Steptoe, A. Immediate and longer-term changes in the Mental Health and Well-being of older adults in England during the COVID-19 pandemic. JAMA Psychiatry79, 151–159. 10.1001/jamapsychiatry.2021.3749 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Kersen, W. et al. Impact of COVID-19 containment measures on perceived health and health-protective behavior: A longitudinal study. Sci. Rep.14, 419. 10.1038/s41598-023-50542-1 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frakt, A. B. How the economy affects health. Jama319, 1187–1188. 10.1001/jama.2018.1739 (2018). [DOI] [PubMed] [Google Scholar]
- 24.Chen, S. et al. The global economic burden of chronic obstructive pulmonary disease for 204 countries and territories in 2020-50: A health-augmented macroeconomic modelling study. Lancet Glob. Health11, e1183–e1193. 10.1016/s2214-109x(23)00217-6 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rubio-Tomás, T., Skouroliakou, M. & Ntountaniotis, D. Lockdown due to COVID-19 and its consequences on diet, physical activity, lifestyle, and other aspects of daily life worldwide: A narrative review. Int. J. Environ. Res. Public. Health1910.3390/ijerph19116832 (2022). [DOI] [PMC free article] [PubMed]
- 26.van Zyl-Smit, R. N., Richards, G. & Leone, F. T. Tobacco smoking and COVID-19 infection. Lancet Respir. Med.8, 664–665. 10.1016/s2213-2600(20)30239-3 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim, S. et al. Short- and long-term neuropsychiatric outcomes in long COVID in South Korea and Japan. Nat. Hum. Behav.10.1038/s41562-024-01895-8 (2024). [DOI] [PubMed] [Google Scholar]
- 28.Weingart, R. et al. Adolescent sleep duration and timing during early COVID-19 school closures. Sleep Health7, 543–547. 10.1016/j.sleh.2021.07.003 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ludwig-Walz, H. et al. How the COVID-19 pandemic and related school closures reduce physical activity among children and adolescents in the WHO European Region: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act.20, 149. 10.1186/s12966-023-01542-x (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Magson, N. R. et al. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J. Youth Adolesc.50, 44–57. 10.1007/s10964-020-01332-9 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kretschmer, L. et al. Gender differences in the distribution of children’s physical activity: Evidence from nine countries. Int. J. Behav. Nutr. Phys. Act.20, 103. 10.1186/s12966-023-01496-0 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bendau, A., Petzold, M. B., Kaminski, J., Plag, J. & Ströhle, A. Exercise as treatment for stress-related mental disorders. Curr. Neuropharmacol.22, 420–436. 10.2174/1570159x22666230927103308 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu, F., Wang, W., Ma, J., Sa, R. & Zhuang, G. Different associations of sufficient and vigorous physical activity with BMI in Northwest China. Sci. Rep.8, 13120. 10.1038/s41598-018-31227-6 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barnes, C. et al. Improving implementation of school-based healthy eating and physical activity policies, practices, and programs: A systematic review. Transl. Behav. Med.11, 1365–1410. 10.1093/tbm/ibab037 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim, H. et al. Machine learning-based prediction of suicidal thinking in adolescents by derivation and validation in 3 independent Worldwide cohorts: Algorithm Development and Validation Study. J. Med. Internet Res.26, e55913. 10.2196/55913 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choi, Y. et al. Acute and post-acute respiratory complications of SARS-CoV-2 infection: Population-based cohort study in South Korea and Japan. Nat. Commun.15, 4499. 10.1038/s41467-024-48825-w (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Freudenberg, N., Goldrick-Rab, S., Poppendieck, J. & College students the new face of food insecurity in the United States. Am. J. Public. Health109, 1652–1658. 10.2105/ajph.2019.305332 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Oh, J. et al. National and regional trends in the prevalence of type 2 diabetes and associated risk factors among Korean adults, 2009–2021. Sci. Rep.13, 16727. 10.1038/s41598-023-43353-x (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data are available upon request. Study protocol and statistical code: Available from DKY (yonkkang@gmail.com). Dataset: Available from the Korea Disease Control and Prevention Agency through a data use agreement. Data from the Korea Youth Risk Behavior Web-based Survey can be accessed via the following link: https://www.kdca.go.kr/yhs/.