Abstract
Aims
To determine the contribution that variation in the unregulated drug market has on the risk of heroin overdose across individuals with different levels of personal overdose risk.
Design
A retrospective cohort study of heroin injecting episodes and overdose cases were examined over a 12‐month period between 30 June 2022 and 30 June 2023.
Setting
The Medically Supervised Injecting Room in Melbourne, Australia.
Cases
1474 witnessed heroin overdose cases were examined amongst a cohort of 337 individuals who were predominantly male (n = 276, 81.7%) with a median age of 43.5 years (interquartile range 37.25–49.00 years, range 20–75 years).
Measurements
The daily overdose rate was used to differentiate High and Low daily overdose risk categories. The number of overdose events that an individual experienced during the study period was used to differentiate people into Standard, Moderate and High personal overdose risk categories. Each overdose case was differentiated by the personal overdose risk of the individual who experienced the overdose, as well as the overdose risk of the day that overdose occurred. A stratified overdose risk profile was then derived across the nine different daily overdose risk and personal overdose risk categories.
Findings
The rate of overdose approximately doubled on High overdose risk days compared with Standard overdose risk days, increasing by a factor of 2.11, 2.41 and 2.03 times for individuals in the Standard, Moderate and High personal overdose risk groups. Conversely, the rate of overdose was also substantially reduced on Low overdose risk days to a factor of 0.17, 0.28 and 0.20, respectively.
Conclusion
Among heroin users in Melbourne, Australia, there is an approximately 10‐times difference in the risk of overdose on some days compared with others, which appears to be attributable to the effects of the unregulated drug market and not the effects of variation in personal overdose risk of individuals.
Keywords: drug checking, heroin overdose, overdose risk, public health, supervised injecting facilities, unregulated drug market
Adverse outcomes associated with opioids are a major public health issue with more than 100 000 people dying globally each year from opioid overdose [1, 2]. The adulteration or substitution of heroin with either fentanyl or novel synthetic opioids is a particular concern because of the increased risk of overdose‐related adverse outcomes [3, 4, 5]. Variability in the composition and strength of illicit opioids obtained from the unregulated drug market may exceed the anticipated dose, and therefore, the opioid tolerance of an individual, which may result in an overdose [6, 7]. Certainly, it has been long believed by people who use heroin on a regular basis that this variability from the unregulated drug market is a direct contributor to the risk of experiencing an overdose [8]. Our understating of this, however, remains unclear because of the interindividual variability in overdose risk between people who use drugs. There are well‐established intra‐individual or ‘personal’ risk factors that increase the risk of an individual to experience an overdose. These include people with a history of non‐fatal overdose, change in opioid tolerance (including recent prison release or periods of abstinence) and the concomitant use of benzodiazepines, alcohol and other opioid analgesic drugs [9, 10, 11, 12, 13]. An unresolved question remains about whether illicit opioids obtained from the unregulated drug market substantially contribute to overdose cases, or whether it is these known personal risk factors for an individual that play the most substantive role as has been previously suggested [14, 15].
Part of the reason for the gap in understanding the potential impact of the unregulated drug market on overdose cases relates to the use of fatal overdose cases to study these effects. Any heroin overdose can result in an adverse or fatal outcome because of the effects of opioid induced ventilatory impairment, including an inability to correct airway occlusion caused by positional asphyxia even at lower levels of opioid toxicity [16]. The use of fatal outcome data provides high‐quality information about overdose risks and contributors, but only represents a small proportion of overdose cases, including ~3% to 6% of heroin overdose cases in Australia [17, 18]. This is also compounded by the fact that in many jurisdictions the direct testing of illicit drug samples using analytical techniques to determine the strength and composition of samples before administration is not permitted. Therefore, demonstrating a direct correlation between variations in an illicit drug sample with an overdose event at an individual level is typically not possible. The aim of this study was to determine the contribution that variation in the unregulated drug market has on the risk of heroin overdose across individuals with different levels of personal overdose risk.
METHODS
The dataset comprised of non‐fatal overdose cases from the Medically Supervised Injecting Room (MSIR) at North Richmond Community Health in Melbourne, Australia. A retrospective cohort of supervised heroin injecting episodes and overdose cases were examined over a 12‐month period between 30 June 2022 and 30 June 2023. Only witnessed overdose cases associated with a supervised injecting visit that occurred on‐site at the MSIR were included in this study. Heroin overdose cases were diagnosed on the basis of clinical findings and where the individual also stated that they were injecting heroin. Clinical interventions were provided in an escalating manner to provide basic supportive care, including airway management and ventilatory support, as well naloxone administration where clinically indicated as described previously [16]. Briefly, a heroin overdose diagnosis was determined where an individual presented in an altered conscious state with respiratory depression and was unable to maintain oxygen saturation (SpO2) of greater than 93% on room air despite encouragement to breathe in the context of heroin use reported by the individual and witnessed to be self‐administered at the MSIR.
Setting
The MSIR is the only supervised injecting facility or overdose prevention centre in the state of Victoria, and together with the Medically Supervised Injecting Centre in Sydney, the only two services in Australia. The MSIR is an anonymous harm reduction service that provides a supervised setting for people who inject drugs, with a range of health and social support services available onsite. The MSIR is located in close proximity to a well‐established heroin street‐based drug market. People who access the service tend to be more socially vulnerable, have been involved in high‐risk injecting behaviours, have been recently released from prison and are more likely to have had a recent overdose compared to other people who inject drugs across Melbourne [19]. To be eligible to access the MSIR, individuals must be at least 18 years of age, not pregnant, have no bail or parole conditions that prohibit attendance at the MSIR, and have a history of injecting drug use. Pregnancy, serious intoxication and/or severe mental or physical ill health on presentation preclude access to the service. On arrival, clients are required to disclose the pre‐obtained drugs they intend to inject and their substance use history for the preceding 24 hours. After accessing the service, clients prepare and self‐administer their pre‐obtained drugs while being regularly monitored by staff. Staff also provide individualised harm reduction advice and complete a thorough clinical assessment if an adverse clinical event occurs. Any medical issues, including overdose, are assessed and managed by clinical staff onsite.
Differentiating personal overdose risk for individuals
Some people are at greater risk of experiencing an overdose than others. To ensure that variation in the daily overdose rate was not simply associated with the confounding effect of people at higher risk of experiencing an overdose injecting on a particular day, the number of overdose events experienced by an individual over the study period was used to stratify them into three different personal overdose risk categories. We stratified personal overdose risk into ‘standard’ (≤1 overdose), ‘moderate’ (2–7 overdoses) and ‘high’ (≥8 overdoses) risk categories as summarised in Table 1. These criteria were adapted from previous work, which demonstrated an approximately two‐fold and five‐fold increased risk for individuals to experience a fatal overdose in the moderate and high personal overdose risk categories compared to the standard personal overdose risk, respectively [20].
TABLE 2.
Daily overdose risk classification.
| Category | Daily heroin overdose rate |
|---|---|
| Low overdose risk day | ≤0.061% |
| Standard overdose risk day | 0.062%–2.95% |
| High overdose risk day | ≥2.96% |
Differentiating high and low overdose risk days
Quantitative analysis of the individual heroin samples using analytical techniques to determine the strength and composition before administration (i.e. drug checking) is not currently permitted in this jurisdiction. Assessing the direct effect of variation of individual samples on overdose risk was, therefore, not possible as part of this study. Instead, high and low overdose risk days were determined using the daily heroin overdose rate at the MSIR over the 12‐month study period. The distribution of the daily heroin overdose rate (number of heroin injecting episodes to heroin overdose cases) is shown in Figure 1.
FIGURE 1.
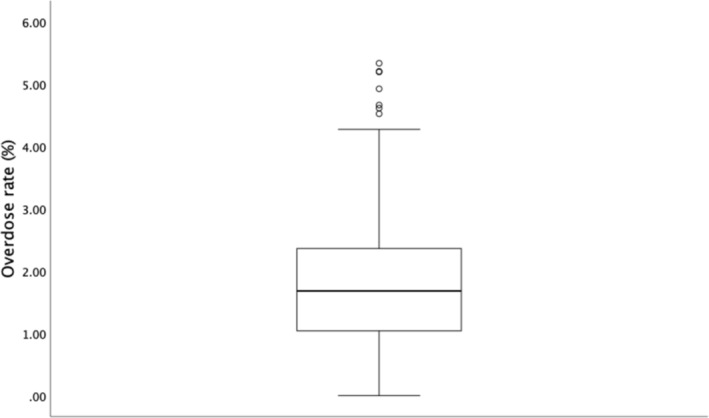
The daily heroin overdose rate over the 12‐month study period.
For this study, days with the lowest rate of heroin overdose were classified as low‐overdose risk days, and included cases where the heroin overdose rate fell below the first one‐eighth or 12.5% of distribution (the lower half of the first quartile). Conversely, days with the highest rate of heroin overdose were classified as high‐overdose risk days, and included cases where the heroin overdose rate was above the top one‐eighth or 12.5% of distribution (the upper half of the fourth quartile). The standard‐overdose risk days were comprised of the remaining 75% of days with a heroin overdose rate that centred around the median. The classifications used for overdose risk days are detailed in Table 2.
TABLE 1.
Personal overdose risk classification for individuals.
| Category | No. of non‐fatal overdose events in 12 months |
|---|---|
| Standard personal overdose risk | ≤1 overdose |
| Moderate personal overdose risk | 2–7 overdoses |
| High personal overdose risk | ≥8 overdoses |
Determining the overdose rate for the different daily overdose risk categories, and the different personal overdose risk categories
For each day across the 12‐month study period, all overdose cases were categorised based on both the overdose risk for the individual who experienced the overdose (standard, moderate and high personal overdose risk categories) and also the rate of overdoses that occurred on that day (low, standard and high daily overdose risk categories). A daily overdose rate was then determined for each of the low, standard and high daily overdose risk categories based on aggregate data across the 12‐month study period. Within each of these daily overdose risk categories the rate of overdose for individuals with standard, moderate and high personal overdose risk was then separated to determine the daily overdose risk across each of these categories for comparison.
Statistical analysis and pre‐registration of the research question
The primary research question and analysis plan were not pre‐registered on a publicly available platform, and therefore, the results of this study should be considered exploratory. Descriptive statistics were used to describe the number and classification of overdose cases, demographic details of individuals who experienced an overdose and variation in drug market overdose risk days. Medians and interquartile range (IQR) presented as upper and lower quartiles were used for comparison because of non‐normally distributed data. Descriptive statistics and analysis were conducted using SPSS for Mac version 28 with graphs produced using both SPSS and Microsoft Excel.
Ethics
This study was approved by the Monash University Human Research Ethics Committee (MUHREC 29519).
RESULTS
Over the 12‐month study period there were a total of 81 911 supervised heroin injecting episodes at the MSIR and a total of 1474 heroin overdose cases. The overdose cases occurred among a cohort of 337 individuals who were predominantly male (n = 276, 81.7%) with a median age of 43.5 years (IQR = 37.25–49.00 years, range = 20–75 years). For all of the overdose cases managed during the study period there were no fatal outcomes for any of the individuals. The majority of cases (98.6%, n = 1453) were managed to clinical resolution on‐site at the MSIR, with 21 complicated heroin overdose cases transported to hospital for a higher level of clinical care.
Of the 1474 heroin overdose cases, approximately two‐thirds of cases (62.5%, n = 921) involved heroin use alone, and approximately one‐third of cases (37.5%, n = 553) involved the concomitant use of heroin with other drugs. The vast majority of overdose cases that involved multiple drug use were related to the concomitant use of heroin and diphenhydramine (97%, n = 537). There were also a further 13 cases that involved heroin co‐administered with either methamphetamine or cocaine, two cases that involved combined heroin and benzodiazepine administration, as well as one case that involved concomitant intravenous administration of both heroin and methadone.
The personal overdose risk for individuals
There were 337 individuals that experienced an overdose in the study period. Almost half (45%, n = 151) experienced a single overdose event, where the remainder (55%, n = 186) experienced two or more overdose events as demonstrated in Figure 2. Across the personal overdose risk spectrum, the number of people in each category decreased from 45% (n = 151) in the standard personal overdose risk category, 42% (n = 143) in the moderate personal overdose risk category, and 13% (n = 43) in the high personal overdose risk category. At the top end of the spectrum, there were six individuals that experienced greater than 40 overdoses, including one person that experienced 94 separate overdose events in the 12‐month study period. The median number of overdose events experienced by individuals during the study period was 2 (IQR = 1–4 events, range = 1–94).
FIGURE 2.

The number of overdose events experienced by individuals over the 12‐month study period.
Heroin injecting episodes, overdose cases and the daily heroin overdose rate
Over the study period there was a binomial distribution of supervised injecting episodes at the MSIR, with a greater number of visits during weekdays compared to weekends that also corresponded with differences in operating hours. For weekdays there was a median of 241 heroin injecting episodes each day (IQR = 224–258, range = 80–319 injecting episodes) and for weekends there was a median of 181 heroin injecting episodes each day (IQR = 170.75–198, range = 138–238 injecting episodes). The number of heroin overdoses each day ranged from 0 overdose cases to 14 overdose cases in a single day. The median daily heroin overdose rate was 1.67% (IQR = 1.04%–2.36%) across the study period, with a daily overdose rate that ranged between 0% and 5.33% as illustrated in Figure 1.
The high and low risk overdose days
The low overdose risk days were comprised of days with the lowest heroin overdose rate over the study period, and represented the bottom one‐eighth of the distribution (12.5%, n = 45) with a daily overdose rate between 0% to 0.061%. The high overdose risk days were comprised of days with the highest heroin overdose rate over the study period, and represented the top one‐eigth of the distribution (12.5%, n = 45) with a daily overdose rate between 2.96% to 5.33%. The standard overdose risk days comprised of the remaining middle distributed days (75%, n = 275) with a daily overdose rate between 0.062% and 5.33%.
The risk of overdose on different days separated by both the daily overdose risk classification and personal overdose risk
Overdose cases that occurred on high, standard and low overdose risk days were then differentiated by the personal overdose risk of individuals that experienced the overdose (Table 3). A daily overdose rate was derived based on the number of days within each daily overdose risk category to compare the overdose risk across each of the nine different category combinations. The risk of overdose approximately doubled on high overdose risk days compared to standard overdose risk days for individuals across each of the personal overdose risk categories. More specifically, the overdose rate increased by a factor of 2.11, 2.41 and 2.03 for individuals in the standard, moderate and high personal overdose risk groups, respectively. Conversely, low overdose risk days were associated with a substantial reduction in the risk of overdose compared to standard overdose risk days across each of the personal overdose risk categories. On low overdose risk days, the overdose rate was reduced to a factor of 0.17, 0.28 and 0.20 compared to standard overdose risk days for individuals in the standard, moderate and high personal overdose risk groups, respectively.
TABLE 3.
Cross‐tabulation table of overdose cases on different overdose risk days differentiated by the personal overdose risk classification of the individuals.
| Category | Personal overdose risk | Total | |||
|---|---|---|---|---|---|
| Standard | Moderate | High | Overdose cases (n) | Category days (n) | |
| Daily overdose risk | |||||
| Low | 3 | 14 | 20 | 37 | 45 days |
| Standard | 110 | 332 | 620 | 1062 | 275 days |
| High | 38 | 131 | 206 | 375 | 45 days |
| Total (n) | 151 | 477 | 846 | 1474 | 365 days |
Overall, there was a substantial difference in overdose risk across different days irrespective of the personal overdose risk, including an approximate 10‐times greater risk of overdose on high overdose risk days compared to low overdose risk days. This was seen consistently across the different personal overdose risk groups on these days, with the risk of overdose changing by a factor of 12.67, 9.36 and 10.30 for individuals in the standard, moderate and high personal overdose risk groups, respectively. The different daily overdose risk for individuals in the three different personal overdose risk categories across the different drug market overdose risk conditions are shown in Figure 3.
FIGURE 3.

The overdose rate for people with standard, moderate, and high personal overdose risk across the different daily overdose risk conditions.
DISCUSSION
Understanding the contributors to opioid overdose is extremely important in order to reduce adverse outcomes, including for people who use heroin who are at an estimated six‐times greater risk of premature death than the general age‐matched population [9, 21, 22]. In our study, we demonstrated that there were days when overdose events occurred more frequently than normal (high overdose risk days), and also days when overdose events occurred less frequently than normal (low overdose risk days) that importantly was not associated with differences in the personal risk of overdose of individuals. By examining the overall difference in overdose risk while accounting for the confounding effect of individuals who are at greater risk of experiencing an overdose than others, we were able to demonstrate substantial variation in overdose risk on different days that is reasonably attributable to variation in the unregulated heroin drug market. Significantly, in our study, we demonstrated that there is an approximate 10‐times greater risk of overdose on some days compared to other days. This risk applies equally to people who very rarely experience an overdose, as well as to individuals who are at high‐risk of experiencing an overdose.
The findings of our study are consistent with quantitative analysis of street‐level heroin obtained from this region where clinically significant variation in the strength or effective dose of heroin was observed [6]. The identification of both low and high‐risk overdose days compared to what might be expected by an individual highlight seemingly perfect conditions for overdoses to occur because of the unpredictability of the strength of the heroin obtained from the unregulated illicit drug market. These fluctuations highlight the difficulty that individuals who inject heroin have maintaining equipotent opioid dosing from the unregulated drug market, and where variation from one day to the next may easily result in an individual exceeding their opioid tolerance with no change in their pattern of use or other personal risk factors.
An important public health implication from this study is that both personal overdose risk as well as overdose risk from the unregulated drug market must be considered when designing initiatives to reduce overdose cases and subsequent overdose‐related adverse outcomes. It is for this reason that recent public health interventions including illicit drug checking services and ‘safe supply’ alternatives for illicit opioids may substantially contribute to reducing overdose‐related adverse outcomes [23, 24].
Our study showed that individuals in the high personal overdose risk category had a higher baseline level of risk and were more likely to experience an overdose under any daily overdose risk conditions. The risk of overdose for these individuals on a high overdose risk day was particularly concerning. This finding is consistent with the previous work that these personal overdose criteria were adapted from, whereindividuals had been demonstrated to be five‐times more likely to experience a fatal overdose compared to individuals in the standard personal overdose risk category [20]. These personal overdose risk criteria may be an effective way of identifying individuals at high overdose risk in the general population of people who inject heroin, and may be suitable for providing targeted public health interventions in a similar way that other tailored overdose prevention programs for high‐risk populations such as recent prison release have been established [12, 13, 25].
Limitations
There are several limitations of this study. First, personal overdose risk was differentiated using the number of non‐fatal overdose events alone because these criteria are not subjective, and have been shown to be independently associated with an increased risk for individuals to experience a fatal overdose. There are, however, other contributing factors that can increase the risk of an overdose for an individual, including variation in opioid tolerance, a change in underlying health and the concomitant use of other drugs. Second, the number of non‐fatal overdose events used to differentiate individuals into the different personal overdose risk categories were also adapted from previous work, however, that previous work involved a shorter time‐period rather than the 12‐month time period in the current study. It is, therefore, possible that the personal overdose risk classification of some individuals may have been higher in our study compared to the study that these criteria were adapted from because of the time difference in our study where additional overdoses may have occurred.
A third limitation was the inability to analyse the strength and composition of heroin in any of the individual overdose cases and to directly determine the impact of variation in the heroin administered as to whether an overdose occurred or not at an individual level. Inferential statistical analysis of this individual‐level data would enable a more detailed and sensitive analysis of the impact of the unregulated drug market on overdose cases. In our study, we used population‐level data and were able to demonstrate an overall effect of variation in overdose risk that is reasonably attributable to the unregulated drug market that occurs across all levels of personal overdose risk for individuals. Further work in this area to refine other objective personal overdose risk criteria that could be used and to analytically test heroin or other illicit opioids before administration to determine overdose risk at an individual level is required.
CONCLUSION
We demonstrated that over a 12‐month period there were high overdose risk days when overdose events occurred more frequently than normal and also low overdose risk days when overdose events occurred less frequently than normal. This variation in risk was not associated with differences in the personal risk of overdose of individuals, but rather these changes in overdose risk were reasonably attributable to variation in the unregulated drug market. Importantly, this variation in overdose risk associated with the unregulated drug market can be substantial. In fact, we demonstrated that there is a 10‐times greater risk of overdose on some days compared to other days, and that this risk applies equally to people who very rarely experience an overdose as well as to individuals who are at high‐risk of experiencing an overdose. The findings of this study have important public health implications and demonstrate that interventions that identify and address the variability of the illicit drug market are required to effectively reduce overdose‐related morbidity and mortality.
AUTHOR CONTRIBUTIONS
All authors contributed to the preparation of the manuscript and have approved the final manuscript.
DECLARATION OF INTERESTS
None.
ACKNOWLEDGEMENTS
We acknowledge the clients and staff of the Medically Supervised Injecting Room at North Richmond Community Health.
Stam NC, Furler J, Hiley S, Schumann JL. Differences in heroin overdose risk associated with the unregulated drug market: Insights from a supervised injecting facility in Melbourne, Australia. Addiction. 2025;120(2):285–292. 10.1111/add.16706
Funding information This research did not receive any specific grant or funding from agencies in the public, commercial, or not‐for‐profit sectors.
DATA AVAILABILITY STATEMENT
Data available on request from the authors.
REFERENCES
- 1. Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths ‐ United States, 2013‐2019. MMWR Morb Mortal Wkly Rep. 2021;70(6):202–207. 10.15585/mmwr.mm7006a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. UNODC . World drug report 2023 United Nations publication; Sales No. E.23.XI.7. [Google Scholar]
- 3. Frank RG, Pollack HA. Addressing the fentanyl threat to public health. N Engl J Med. 2017;376(7):605–607. 10.1056/NEJMp1615145 [DOI] [PubMed] [Google Scholar]
- 4. Rodda LN, Pilgrim JL, Di Rago M, Crump K, Gerostamoulos D, Drummer OH. A cluster of fentanyl‐laced heroin deaths in 2015 in Melbourne. Australia J Anal Toxicol. 2017;41(4):318–324. 10.1093/jat/bkx013 [DOI] [PubMed] [Google Scholar]
- 5. D'Orazio J, Nelson L, Perrone J, Wightman R, Haroz R. Xylazine adulteration of the heroin‐fentanyl drug supply: a narrative review. Ann Intern Med. 2023;176(10):1370–1376. 10.7326/M23-2001 [DOI] [PubMed] [Google Scholar]
- 6. Stam NC, Gerostamoulos D, Gerstner‐Stevens J, Scott N, Smith K, Drummer OH, et al. Determining the effective dose of street‐level heroin: a new way to consider fluctuations in heroin purity, mass and potential contribution to overdose. Forensic Sci Int. 2018;290:219–226. 10.1016/j.forsciint.2018.07.009 [DOI] [PubMed] [Google Scholar]
- 7. Larnder A, Saatchi A, Borden SA, Moa B, Gill CG, Wallace B, et al. Variability in the unregulated opioid market in the context of extreme rates of overdose. Drug Alcohol Depend. 2022;235:109427. 10.1016/j.drugalcdep.2022.109427 [DOI] [PubMed] [Google Scholar]
- 8. Darke S, Ross J, Hall W. Overdose among heroin users in Sydney, Australia: I. Prevalence and correlates of non‐fatal overdose. Addiction. 1996;91(3):405–411. [PubMed] [Google Scholar]
- 9. Darke S, Mills KL, Ross J, Teesson M. Rates and correlates of mortality amongst heroin users: findings from the Australian treatment outcome study (ATOS), 2001‐2009. Drug Alcohol Depend. 2011;115(3):190–195. 10.1016/j.drugalcdep.2010.10.021 [DOI] [PubMed] [Google Scholar]
- 10. Rintoul AC, Dobbin MD, Nielsen S, Degenhardt L, Drummer OH. Recent increase in detection of alprazolam in Victorian heroin‐related deaths. Med J Aust. 2013;198(4):206–209. 10.5694/mja12.10986 [DOI] [PubMed] [Google Scholar]
- 11. Stoove MA, Dietze PM, Jolley D. Overdose deaths following previous non‐fatal heroin overdose: record linkage of ambulance attendance and death registry data. Drug Alcohol Rev. 2009;28(4):347–352. 10.1111/j.1465-3362.2009.00057.x [DOI] [PubMed] [Google Scholar]
- 12. Binswanger IA, Blatchford PJ, Mueller SR, Stern MF. Mortality after prison release: opioid overdose and other causes of death, risk factors, and time trends from 1999 to 2009. Ann Intern Med. 2013;159(9):592–600. 10.7326/0003-4819-159-9-201311050-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bukten A, Stavseth MR, Skurtveit S, Tverdal A, Strang J, Clausen T. High risk of overdose death following release from prison: variations in mortality during a 15‐year observation period. Addiction. 2017;112(8):1432–1439. 10.1111/add.13803 [DOI] [PubMed] [Google Scholar]
- 14. Darke S, Farrell M. Would legalizing illicit opioids reduce overdose fatalities? Implications Nat Exp Addiction. 2014;109(8):1237–1242. 10.1111/add.12456 [DOI] [PubMed] [Google Scholar]
- 15. Darke S. Heroin overdose. Addiction. 2016;111(11):2060–2063. 10.1111/add.13516 [DOI] [PubMed] [Google Scholar]
- 16. Stam NC, Cogger S, Schumann JL, Weeks A, Roxburgh A, Dietze PM, et al. The onset and severity of acute opioid toxicity in heroin overdose cases: a retrospective cohort study at a supervised injecting facility in Melbourne, Australia. Clin Toxicol (Phila). 2022;60(11):1227–1234. 10.1080/15563650.2022.2126371 [DOI] [PubMed] [Google Scholar]
- 17. Darke S, Mattick RP, Degenhardt L. The ratio of non‐fatal to fatal heroin overdose. Addiction. 2003;98(8):1169–1171. 10.1046/j.1360-0443.2003.00474.x [DOI] [PubMed] [Google Scholar]
- 18. Stam NC, Pilgrim JL, Drummer OH, Smith K, Gerostamoulos D. Catch and release: evaluating the safety of non‐fatal heroin overdose management in the out‐of‐hospital environment. Clin Toxicol (Phila). 2018;56(11):1135–1142. 10.1080/15563650.2018.1478093 [DOI] [PubMed] [Google Scholar]
- 19. Van Den Boom W, Del Mar Quiroga M, Fetene DM, Agius PA, Higgs PG, Maher L, et al. The Melbourne safe injecting room attracted people Most in need of its service. Am J Prev Med. 2021;61(2):217–224. 10.1016/j.amepre.2021.02.018 [DOI] [PubMed] [Google Scholar]
- 20. Caudarella A, Dong H, Milloy MJ, Kerr T, Wood E, Hayashi K. Non‐fatal overdose as a risk factor for subsequent fatal overdose among people who inject drugs. Drug Alcohol Depend. 2016;162:51–55. 10.1016/j.drugalcdep.2016.02.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gossop M, Stewart D, Treacy S, Marsden J. A prospective study of mortality among drug misusers during a 4‐year period after seeking treatment. Addiction. 2002;97(1):39–47. 10.1046/j.1360-0443.2002.00079.x [DOI] [PubMed] [Google Scholar]
- 22. Degenhardt L, Bucello C, Mathers B, Briegleb C, Ali H, Hickman M, et al. Mortality among regular or dependent users of heroin and other opioids: a systematic review and meta‐analysis of cohort studies. Addiction. 2011;106(1):32–51. 10.1111/j.1360-0443.2010.03140.x [DOI] [PubMed] [Google Scholar]
- 23. McNeil R, Fleming T, Mayer S, Barker A, Mansoor M, Betsos A, et al. Implementation of safe supply alternatives during intersecting COVID‐19 and overdose health emergencies in British Columbia, Canada, 2021. Am J Public Health. 2022;112(S2):S151–S158. 10.2105/AJPH.2021.306692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kennedy MC, Scheim A, Rachlis B, Mitra S, Bardwell G, Rourke S, et al. Willingness to use drug checking within future supervised injection services among people who inject drugs in a mid‐sized Canadian city. Drug Alcohol Depend. 2018;185:248–252. 10.1016/j.drugalcdep.2017.12.026 [DOI] [PubMed] [Google Scholar]
- 25. Parmar MK, Strang J, Choo L, Meade AM, Bird SM. Randomized controlled pilot trial of naloxone‐on‐release to prevent post‐prison opioid overdose deaths. Addiction. 2017;112(3):502–515. 10.1111/add.13668 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request from the authors.


