Abstract
ACT in Daily Life (ACT-DL) is a blended-care Ecological Momentary Intervention that extends ACT into the daily life of individuals, improving psychotic distress, negative symptoms, and global functioning. However, it remains unclear whether ACT-DL works equally for everyone. We investigated whether moderators (i.e., sociodemographic information, personality, and trauma history) determine clinical outcomes in individuals with early psychosis receiving ACT-DL. Seventy-one participants from the INTERACT trial, using ACT-DL, were analyzed. Outcomes included psychotic distress, negative symptoms, global functioning, and psychological flexibility. Using multivariate-multilevel models, we evaluated the effects of sociodemographics, personality, and childhood trauma across baseline, post-intervention, and six- and 12-month follow-ups. Sociodemographic characteristics and personality predicted clinical outcomes. Higher education demonstrated more substantial improvement in global functioning at 6- (B = 7.43, p = 0.04) and 12-FU (B = 10.74, p = 0.002) compared to lower education. Higher extraversion showed less improvement in negative symptoms at 12-FU (B = 1.24, p = 0.01) and more improvement in global functioning at post-intervention (B = 0.39, p = 0.046) and 6-FU (B = 1.40, p = 0.02) compared to lower extraversion. Higher negative affectivity showed more improvement in negative symptoms at 12-FU (B = −1.59, p = 0.001) and higher psychological flexibility at 12-FU (B = 8.38, p = 0.001) compared to lower negative affectivity. Our findings suggest that while ACT-DL improves clinical outcomes in individuals with early psychosis, the improvement rate is dissimilar for individuals and predictable by baseline characteristics. If replicated, these findings enable precision medicine approaches in allocating ACT-DL for early psychosis.
Subject terms: Neuroscience, Psychology, Schizophrenia
Introduction
Psychosis exists on a continuum [1, 2], ranging from subclinical psychotic experiences in the Ultra-High-Risk stage (UHR) and First Episode Psychosis (FEP) to fully developed psychotic disorders like schizophrenia [3, 4]. This continuum includes individuals who may not meet the criteria for a clinical diagnosis of psychosis but who experience psychotic-like symptoms, distress, and impairment. Psychological interventions for early-stage psychosis are available and have shown promising results in reducing symptoms and distress, improving functionality, and preventing or delaying the onset of a full-blown psychotic disorder [5, 6]. Blended-care interventions combining digital tools with traditional face-to-face therapy have proven effective in various mental disorders [7–9]. However, it remains unclear what factors predict individual responses to blended-care interventions for early psychosis. This lack of knowledge limits the ability to personalize interventions and create appropriate clinical guidelines about what works for whom [6].
One promising example of a blended-care intervention for early psychosis is the Ecological Momentary Intervention (EMI) named “Acceptance and Commitment in Daily Life” (ACT-DL). ACT-DL combines face-to-face Acceptance and Commitment Therapy (ACT) with a smartphone application (app) that assesses momentary psychological states and provides users with ACT exercises and metaphors in their daily lives outside of the therapy room [10]. The efficacy of ACT-DL as an EMI was evaluated in a Randomized Controlled Trial (RCT) called INTERACT [11]. In the INTERACT trial, the ACT-DL intervention demonstrated improved psychotic distress compared to baseline, although no significant difference was found compared to treatment as usual (TAU). However, ACT-DL generally showed small to moderate effects in improving negative symptoms and global functioning compared to TAU [12]. While specific individuals improved, others may not have benefitted as much or may have potentially deteriorated. Moderator analysis is one way to explore individual differences in treatment response. Variables of interest are sociodemographic information, personality traits, and childhood trauma, which are rooted in their established relevance to psychological therapy outcomes and engagement, particularly within early psychosis populations.
Age, sex, and education level have been consistently highlighted in the literature as variables that shape not only the perception of psychological interventions, including EMI’s, but also the actual engagement with such treatments [13–15]. For instance, young individuals’ generally positive attitudes towards mobile health applications suggest a receptivity that might enhance intervention efficacy compared to older individuals [13, 15, 16]. Differences in sex might similarly affect ACT-DL’s efficacy as women are more likely to engage with apps designed to improve health, whereas young men tend to lose interest more quickly. Conversely, lower education levels have been linked to reduced engagement and poorer outcomes [14, 17, 18]. Thus, age, sex and education level might explain potential barriers that blended-care interventions must overcome to be universally effective. Second, personality traits have been studied in relation to first-episode psychosis (FEP) and offer a window into understanding individual psychological predispositions affecting psychotherapy outcomes [19–24]. Individuals with FEP reported lower levels of extraversion and higher levels of negative affectivity — defined as the inclination towards sociability and positivity, and frequent and intense experiences of negative emotions and interpersonal manifestations respectively— compared to healthy controls [25, 26]. These personality dimensions potentially affect ACT-DL’s efficacy as high-trait negative affectivity and low-trait extraversion are both associated with higher symptom severity at baseline, lower treatment adherence, and less therapeutic improvements [19]. Lastly, the inclusion of childhood trauma as a predictor is necessary because early adverse experiences can fundamentally alter the course and prognosis of FEP [27], with substantial evidence indicating that trauma history adversely affects treatment response [28, 29]. However, research specifically assessing the effects of sociodemographics, personality, and childhood trauma in the context of EMI’s (ACT-DL) is scarce, warranting additional investigation.
To better understand who might benefit most from ACT-DL, the current study aims to explore whether inter-individual factors moderate the effects of ACT-DL on psychotic distress, negative symptoms, global functioning, and psychological flexibility over time. We will investigate the following confirmatory hypotheses: (1) individuals with a lower education level will show less improvement in negative symptoms, psychotic distress, global functioning, and psychological flexibility than individuals with higher education levels over time; (2) individuals who score higher on negative affectivity or lower on extraversion will show less improvement over time in negative symptoms, psychotic distress, global functioning and psychological flexibility than individuals who score lower on negative affectivity or higher on extraversion; and (3) individuals with higher levels of childhood trauma will show less improvement over time in negative symptoms, psychotic distress, global functioning and psychological flexibility than individuals with lower levels of childhood trauma. Additionally, we will perform an exploratory analysis to investigate whether age and sex moderate the effect of ACT-DL on psychotic distress, negative symptoms, global functioning, and psychological flexibility over time. Findings will provide clinical guidance for whom ACT-DL might be an appropriate blended-care intervention. All statistical analyses were a-priori specified in a post-registered analysis plan (https://osf.io/xr9as/?view_only=a1ec33c65c824ca899aef08ffaec2bc6), which is a registration after data is collected but before data has been accessed and analyzed.
Methods
Participants
This study conducts secondary analyses of the INTERACT dataset (Reininghaus et al. [11]). The INTERACT dataset contains one hundred and forty-eight participants (78 UHR and 70 FEP) recruited from secondary mental health services in five regions in the Netherlands and Belgium. For inclusion, individuals needed to be between 15 and 65 years old, fluent in Dutch, and needed to provide written informed consent to be included. If UHR, participants could not use antipsychotic medication for psychotic symptoms before the study; if FEP, participants needed to have had one psychotic episode within the last three years. Exclusion criteria included a primary diagnosis of alcohol/substance abuse or dependence and severe endocrine, cardiovascular, or brain disease. The current study only included individuals randomized to the ACT-DL condition (n = 71). Refer to the protocol paper for more information on the sample and methods used in INTERACT [11].
Procedures
Participants were recruited from secondary mental health services in five regions in the Netherlands and Belgium: (1) Amsterdam, (2) The Hague, (3) Maastricht/Eindhoven, (4) Vlaams-Brabant/Antwerpen and (5) Oost- & West-Vlaanderen. Participants were provided with initial information about the study by their treating clinician. The study team contacted individuals interested in participating, provided a complete explanation, and asked them to sign the informed consent form. When participants signed informed consent, the researcher conducted a full eligibility assessment. Eligible participants were randomly assigned in a 1:1 ratio to either the experimental condition (ACT-DL + TAU) or the control condition (TAU). Post-intervention and follow-up assessments were carried out by trained researchers who were blind to the participants’ assigned condition. Assessments were conducted at baseline, after the 8-week intervention period, and after six-month and 12-month follow-ups. The study received ethical approval from the MERC at Maastricht University Medical Centre (MUMC), the Netherlands (reference: NL46439.068.13) and the University Clinic Leuven, Belgium (reference: B322201629214).
Intervention
The ACT-DL intervention [10, 30] consisted of eight weekly manualized ACT-sessions administered face-to-face by a trained clinician and an EMI in the form of an app. EMIs are interventions that are provided in the context of daily life [31]. ACT uses cognitive and behavioral techniques to improve psychological flexibility (i.e., adapting cognitive strategies to changing environmental conditions), decrease stress, and improve quality of life [32]. The first session involved general psychoeducation; the following six sessions focused on ACT skills, including acceptance, cognitive defusion, self-as-context, contact with the present moment, values, and committed action [32–34]. The final session was a summary of all the previous components. The EMI app prompted participants daily at eight semi-random moments for three days after each face-to-face session, starting from the second session onwards. Participants answered a brief questionnaire about their current mood, psychotic experiences, and activities, followed by an exercise or metaphor related to the ACT component covered in the previous session. Participants could also start ACT exercises from the app at any time on command. After the intervention period, access to the app was discontinued [11].
Measures
Moderators
Demographic variables included sex (male or female), age in years, and education level. Education level was defined as the highest educational degree achieved and was divided into six categories: ‘elementary school,’ ‘secondary school – general education,’ ‘secondary school – technical education,’ ‘secondary school – vocational education,’ ‘Bachelor,’ and ‘Master.’ We redefined education level into two categories: ‘lower education,’ including elementary and all secondary school degrees, and ‘higher education,’ including Bachelor’s and Master’s degrees.
The personality traits extraversion and negative affectivity were assessed with The Eysenck Personality Questionnaire-Revised Short Form (EPQR-SF) [35, 36], a self-report questionnaire consisting of 48 items with a binary (YES or NO) answer option. Extraversion and negative affectivity were assessed using the 12 items of the corresponding subscales, with higher scores reflecting higher trait levels. The internal consistency of the extraversion and neuroticism subscales have been assessed in a reliability generalization study and were found to be very good to excellent, with (α = 0.82) and (α = 0.83), respectively [37]. In our sample, internal consistency was excellent for extraversion (α = 0.85) and neuroticism (α = 0.84).
Childhood trauma was measured using the Childhood Trauma Questionnaire Short Form (CTQ-SF) [38]. The CTQ-SF is a widely used 28-item self-report measure designed to assess the frequency and severity of childhood abuse and neglect, including emotional, physical, and sexual abuse and emotional and physical neglect. Items are rated on a 5-point Likert scale reflecting the frequency of the traumatic experience. Given that the different forms of trauma often occur together and strict separation of individual effects of a specific type is difficult [39–41], we computed a CTQ total score from the sum of all subscale scores (range: 25 to 125). We ran descriptive analyses using the describe function to visually check the variability of childhood trauma responses. Data were positively skewed, indicating that more individuals had lower trauma scores than individuals with high trauma. We used the categories’ no-low trauma’ (CTQ ≤ 51), ‘moderate trauma’ (51 < CTQ ≤ 68), and ‘severe trauma’ (CTQ > 68) based on cut-off scores of the individual trauma type subscales [38]. The internal consistency in our sample was excellent (α = 0.90).
Clinical outcomes
Psychotic distress was measured using the Comprehensive Assessment of At-Risk Mental States (CAARMS) positive symptom subscales [42]. This semi-structured interview assesses the intensity, frequency, and emotional distress of various positive symptoms to determine if an individual meets the criteria for UHR or FEP. The CAARMS has good psychometric properties and is widely adopted as a high-quality tool for assessing changes in psychotic distress in early psychosis [43, 44]. A psychotic distress total score was calculated by summing scores from the four CAARMS positive symptom scales (unusual thought disorder, non-bizarre ideas, perceptual abnormalities, and speech disorder), each ranging from 0 to 100, with 0 meaning ‘not distressed at all’ and 100 meaning ‘extremely distressed.’ Missing distress scores were excluded from the calculation as they indicate a lack of distress for that symptom.
Negative symptoms were assessed with the Brief Negative Symptom Scale (BNSS) [45]. The BNSS captures the five negative symptoms reached by the NIMH consensus [46] (Avolition, Blunted affect, Anhedonia, Alogia, and Asociality) and measures an individual’s ability to experience normal distress (Distress subscale). These six subscales have 13 items each, rated using a 7-point Likert Scale ranging from 0 ‘No impairment’ to 6: ‘Severe deficit’. A total score was calculated by summing the subscale scores (range from 0 to 78), with higher scores indicating more severe negative symptoms. The BNSS has good convergent and discriminant validity, is sensitive to change, and has good internal consistency [47]. The within-person (ω = 0.90) and between-person (ω = 0.93) consistency was excellent in our sample.
Global functioning was assessed using the single-item Social and Occupational Functioning Assessment Scale (SOFAS) [48]. The SOFAS focuses exclusively on the individual’s social and occupational functioning level and is not directly influenced by the overall severity of the individual’s psychological symptoms. The SOFAS is rated on one continuous scale ranging from 1 ‘Severe malfunctioning in a wide range of activities’ to 100 ‘Superior functioning in a wide range of activities’.
Clinical process outcome
Psychological flexibility was measured using the Flexibiliteits Index Test (FIT-60), a reliable and validated self-report instrument sensitive to change [49, 50]. The FIT-60 comprises six subscales: ‘Acceptance,’ ‘Defusion,’ ‘Self as context,’ ‘Attention for here and now,’ ‘Values’, and ‘Commitment.’ Each subscale consists of 10 items scored on a 7-point Likert scale ranging from 0 ‘Strongly disagree’ to 6 ‘Strongly agree’. A total score was calculated by summing the scores from the different skills, with higher scores meaning more psychological flexibility. Within-person and between-person consistency in our sample was excellent (ω = 0.92 and ω = 0.97, respectively).
Data analysis
All statistical analyses were performed in R (version 4.2.2) and specified in the post-registered analysis plan (https://osf.io/dx2rp), which is a registration after data is collected but before data has been accessed and analyzed.
Analyses were conducted in R (version 4.2.2) according to intention to treat principles [12]. Given the hierarchical structure of the data, multilevel modeling was used to examine the effects of inter-individual factors on clinical outcomes over time. Multivariate multilevel models were estimated for the clinical outcomes (psychotic distress, negative symptoms, and global functioning), and univariate multilevel models were estimated for the clinical process outcome (psychological flexibility). Scores at post-intervention, six-month, and 12-month follow-up were the dependent variables. Separate models were estimated for each moderator (age, sex, education, negative affectivity, extraversion, childhood trauma), resulting in six multivariate and six univariate models. Time was added as a categorical moderator in each model with 0 = baseline, 1 = post-intervention, 2 = 6-month follow-up, and 3 = twelve-month follow-up. Age and sex were added as covariates in the models assessing the moderating effects of education level, personality traits, and childhood trauma. In other words, independent variables included moderator values, time, baseline scores (grand-mean centered), and the baseline score × moderator value × time interaction. Continuous moderators (age, extraversion, negative affectivity) were grand-mean centered to reduce multicollinearity and facilitate intercept interpretation. Categorial moderators were coded as follows: sex (0=male, 1=female), education level (0=lower education, 1=higher education), and childhood trauma (0=no-low trauma, 1=mild trauma, 2=high trauma). Models allowed for random intercepts and random slopes per timepoint. All models were estimated with the nmle package [51] using restricted maximum likelihood (REML) estimations. REML estimations allow for the use of all available data under the assumption that data are missing at random and that all variables associated with the missing values are included in the model. As established in the primary RCT analyses [12], there was no association between baseline variables and missingness of psychotic distress.
An omnibus-test of no difference was performed at all three time points (Wald-type test with df = 3 and α = 0.05) to determine whether each moderator had a significant overall effect on clinical outcomes. Time-specific contrasts were considered only if a moderator had a significant overall effect (each tested at α = 0.05). This approach precludes adjusting for multiple testing at the level of time-specific contrasts [12].
Results
Table 1 presents the results of the omnibus-test of no difference (df = 3) for the overall effect of each moderator on the clinical outcomes. Table 2 shows descriptive statistics, adjusted mean differences with 95% confidence intervals, and p-values for moderators at each timepoint (post-intervention, six-month, and 12-month follow-up) compared to baseline. Results are interpreted in terms of an improvement in clinical outcomes.
Table 1.
Moderators at baseline, Omnibus-test results.
| Omnibus-testa | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Moderator | Total (N = 71) | CAARMS | BNSS | SOFAS | Fit-60 | ||||||
| n | % | χ² | p-value | χ² | p-value | χ² | p-value | χ² | p-value | ||
| Sex (Female) | 52 | 59% | 11.52 | 0.009 | 3.56 | 0.313 | 0.97 | 0.808 | 5.83 | 0.120 | |
| Education (Higher education) | 27 | 38% | 4.66 | 0.198 | 2.58 | 0.461 | 10.20 | 0.017 | 1.23 | 0.746 | |
| Mean | SD | Range | |||||||||
| Age Male/Female | 26/25.8 | 6.0 | 16−47 | 1.19 | 0.593 | 0.22 | 0.974 | 0.53 | 0.913 | 7.94 | 0.051 |
| Neg. affectivity Male/Female | 6.5/8.6 | 3.4 | 1−12 | 0.29 | 0.962 | 11.28 | 0.010 | 1.63 | 0.653 | 14.22 | 0.003 |
| Extraversion | 6.3/6 | 3.2 | 1−12 | 0.07 | 0.995 | 15.09 | 0.002 | 10.06 | 0.018 | 7.53 | 0.057 |
| Moderate Childhood trauma | 44/54 | 15.6 | 25−92 | 3.40 | 0.334 | 0.30 | 0.961 | 1.82 | 0.611 | 1.34 | 0.720 |
| High Childhood Trauma | 1.21 | 0.750 | 2.82 | 0.421 | 0.30 | 0.961 | 7.88 | 0.049 | |||
CAARMS Comprehensive Assessment of At Risk Mental State, BNSS Brief Negative Symptom Scale, SOFAS Social and Occupational Functioning Scale, Fit-60 Flexibiliteits index test 60.
aOmnibus-test of no differences at all three timepoints (χ²(df) with 3 degrees of freedom), alpha = 0.05.
Table 2.
Outcomes at baseline, post-intervention, and 6-month and 12-month follow-up.
| Outcome | Adjusted mean differences at follow-up timepoints | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time | mean | SD | na | Education | Sex | |||||||||
| CAARMS | Base | 207.4 | 84.1 | 71 | Value | SE | 95%CI | t-value | p-value | Value | SE | 95%CI | t-value | p-value |
| Post | 134.5 | 93.2 | 44 | 21.65 | 27.51 | −32.27;75.58 | 0.79 | 0.432 | −25.17 | 28.12 | −80.29;29.95 | −0.90 | 0.371 | |
| FU6 | 106.0 | 75.1 | 35 | 17.58 | 25.95 | −33.28;68.44 | 0.68 | 0.498 | 18.37 | 25.82 | −32.24;68.98 | 0.71 | 0.477 | |
| FU12 | 106.4 | 88.9 | 34 | −39.35 | 24.63 | −87.63;8.93 | −1.60 | 0.111 | −61.00 | 23.69 | −107.43;−14.57 | −2.58 | 0.010 | |
| BNSS | Base | 17.2 | 11.9 | 71 | ||||||||||
| Post | 15.8 | 13.6 | 50 | 4.31 | 2.79 | −1.16;9.77 | 1.54 | 0.123 | 5.22 | 3.24 | −1.13;11.57 | 1.61 | 0.108 | |
| FU6 | 11.0 | 9.1 | 41 | 2.97 | 3.24 | −3.39;9.32 | 0.92 | 0.361 | 1.15 | 3.30 | −5.32;7.62 | 0.35 | 0.728 | |
| FU12 | 9.5 | 11.4 | 42 | 0.946 | 3.34 | −5.60;7.48 | 0.28 | 0.783 | 3.73 | 2.94 | −2.03;9.49 | 1.27 | 0.205 | |
| SOFAS | Base | 40.0 | 11.1 | 71 | ||||||||||
| Post | 50.4 | 10.9 | 50 | 6.12 | 3.15 | −0.06;12.29 | 1.94 | 0.053 | −2.55 | 3.78 | −9.96;4.86 | −0.68 | 0.500 | |
| FU6 | 57.7 | 10.5 | 41 | 7.43 | 3.62 | 0.34;14.52 | 2.06 | 0.040 | 0.06 | 3.84 | −7.47;7.59 | 0.02 | 0.988 | |
| FU12 | 57.9 | 12.2 | 41 | 10.74 | 3.45 | 3.98;17.49 | 3.12 | 0.002 | −2.41 | 3.33 | −8.94;4.12 | −0.73 | 0.469 | |
| Fit-60 | Base | 171,1 | 52.7 | 66 | ||||||||||
| Post | 195.0 | 53.9 | 47 | 6.73 | 9.88 | −35.64;5.76 | −1.42 | 0.160 | 6.55 | 10.94 | −14.89;27.99 | 0.60 | 0.550 | |
| FU6 | 189.9 | 58.2 | 35 | 10.25 | 11.81 | −22.67;18.17 | −0.22 | 0.830 | 9.92 | 10.50 | −10.66;30.50 | 0.95 | 0.347 | |
| FU12 | 206.5 | 52.3 | 38 | −6.91 | 14.898 | −20.39;13.13 | −0.42 | 0.672 | 5.32 | 8.87 | −12.07;22.71 | 0.60 | 0.550 | |
| Outcome | Adjusted mean differences at follow-up timepoints | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time | Age | Negative affectivity | Extraversion | |||||||||||||
| CAARMS | Base | Value | SE | 95%CI | t-value | p-value | Value | SE | 95%CI | t-value | p-value | Value | SE | 95%CI | t-value | p-value |
| Post | 2.09 | 2.47 | −2.91;7.09 | 0.85 | 0.397 | 0.01 | 4.08 | −7.90;8.10 | 0.02 | 0.981 | 0.21 | 5.63 | −10.83;11.25 | 0.04 | 0.970 | |
| FU6 | −0.41 | 2.56 | −5.41;4.59 | −0.16 | 0.872 | −0.63 | 4.18 | −8.82;7.56 | −0.15 | 0.888 | 7.29 | 5.65 | −3.78;18.36 | 1.29 | 0.198 | |
| FU12 | −2.19 | 2.63 | −7.19;2.81 | −0.83 | 0.406 | 1.99 | 4.07 | −5.99;9.97 | 0.49 | 0.632 | 0.64 | 5.91 | −10.94;12.22 | 0.11 | 0.913 | |
| BNSS | Base | |||||||||||||||
| Post | −0.10 | 0,29 | −0.67;0.47 | −0.33 | 0.742 | −0.56 | 0.43 | −1.40;0.28 | −1.29 | 0.197 | 0.79 | 0.45 | −0.10;1.68 | 1.74 | 0.080 | |
| FU6 | 0.03 | 0,31 | −0.58;0.64 | 0.10 | 0.922 | −0.79 | 0.50 | −1.77;0.19 | −1.58 | 0.114 | 0.15 | 0.52 | −0.88;1.17 | 0.28 | 0.779 | |
| FU12 | −0.06 | 0.26 | −0.57;0.45 | −0.21 | 0.831 | −1.59 | 0.49 | −2.51;−0.61 | −3.28 | 0.001 | 1.24 | 0.48 | 0.29;2.19 | 2.57 | 0.011 | |
| SOFAS | Base | |||||||||||||||
| Post | −0.24 | 0.33 | −0.89;0.41 | −0.72 | 0.473 | −0.48 | 0.59 | −1.64;0.68 | −0.82 | 0.421 | 0.39 | 0.53 | −0.64;1.43 | 0.75 | 0.046 | |
| FU6 | −0.16 | 0.36 | −0.87;0.55 | −0.44 | 0.658 | 0.25 | 0.61 | −0.95;1.45 | 0.406 | 0.698 | 1.40 | 0.59 | 0.26;2.54 | 2.38 | 0.018 | |
| FU12 | −0.15 | 0.29 | −0.72;0.42 | −0.54 | 0.593 | −0.24 | 0.50 | −0.51;1.45 | −0.49 | 0.632 | −0.05 | 0.61 | −1.24;1.14 | −0.08 | 0.934 | |
| Fit-60 | Base | |||||||||||||||
| Post | 0.39 | 0.95 | −1.47;2.25 | 0.41 | 0.683 | 2.98 | 1.59 | −0.14;6.10 | 1.87 | 0.064 | −3.95 | 2.16 | −8.18;0.28 | −1.83 | 0.070 | |
| FU6 | 0.01 | 0.92 | −1.79;1.81 | 0.02 | 0.988 | 2.43 | 1.84 | −1.15;6.02 | 1.32 | 0.189 | −2.67 | 2.22 | −7.02;1.68 | −1.20 | 0.232 | |
| FU12 | 0.23 | 0.75 | −1.24;1.70 | 0.31 | 0.760 | 8.38 | 2.34 | 3.79;12.97 | 3.58 | 0.001 | 3.21 | 1.73 | −0.18;6.60 | −1.85 | 0.067 | |
| Outcome | Adjusted mean differences at follow-up timepoints | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Time | Mild trauma | High trauma | |||||||||
| CAARMS | Base | Value | SE | 95%CI | t-value | p-value | Value | SE | 95%CI | t-value | p-value |
| Post | −18.87 | 28.01 | −73.77;36.03 | −0.67 | 0.501 | 59.14 | 45.04 | −29.14;147.42 | −1.31 | 0.190 | |
| FU6 | 9.80 | 27.37 | −43.85;63.45 | 0.36 | 0.720 | −17.67 | 47.25 | −110.28;74.94 | −0.37 | 0.709 | |
| FU12 | −54.93 | 28.93 | −111.63;1.77 | −1.90 | 0.058 | −25.26 | 41.25 | −106.11;55.59 | −0.61 | 0.541 | |
| BNSS | Base | ||||||||||
| Post | 4.07 | 3.48 | −2.75;10.89 | 1.17 | 0.243 | 3.32 | 5.16 | −6.52;13.16 | 0.64 | 0.521 | |
| FU6 | 0.85 | 3.51 | −6.03;7.73 | 0.24 | 0.809 | −5.59 | 5.23 | −15.43;4.25 | −1.07 | 0.286 | |
| FU12 | −1.15 | 3.27 | −7.56;5.26 | −0.35 | 0.726 | 1.48 | 4.66 | −8.36;11.32 | 0.32 | 0.751 | |
| SOFAS | Base | ||||||||||
| Post | 6.73 | 4.14 | −1.27;14.73 | 1.62 | 0.105 | 4.86 | 6.06 | −6.72;16.44 | 0.80 | 0.423 | |
| FU6 | 4.49 | 4.25 | −3.51;12.49 | 1.06 | 0.291 | 3.05 | 6.22 | −8.53;14.63 | 0.49 | 0.624 | |
| FU12 | 3.81 | 3.84 | −4.19;11.81 | 0.99 | 0.321 | 4.04 | 5.44 | −6.62;14.70 | 0.74 | 0.459 | |
| Fit-60 | Base | ||||||||||
| Post | −0.56 | 11.73 | _23.47;22.35 | −0.05 | 0.962 | −22.94 | 17.17 | −56.59;10.71 | −1.34 | 0.184 | |
| FU6 | 1.25 | 11.65 | −21.66;24.16 | 0.11 | 0.915 | −20.82 | 16.58 | −53.32;11.68 | −1.26 | 0.212 | |
| FU12 | −3.13 | 9.53 | −21.81;15.55 | −0.33 | 0.743 | −8.09 | 13.90 | −35.33;19.15 | −0.58 | 0.562 | |
Adjusted mean differences are based on a complete-case ITT analysis of significant moderators from the omnibus-test.
CAARMS Comprehensive Assessment of At Risk Mental State, BNSS Brief Negative Symptom Scale, SOFAS Social and Occupational Functioning Scale, Fit-60 Flexibiliteits index test 60, SD Standard deviation, CI Confidence Interval, SE Standard error.
aNumber of observations differ from the maximum when participants did not complete the measure.
Sociodemographics
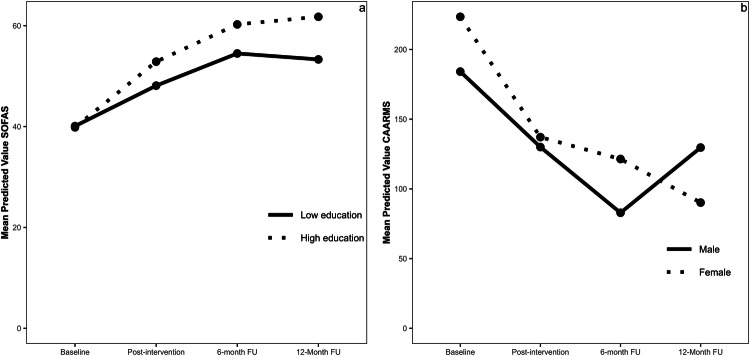
The omnibus-tests investigating the effects of education level were significant for global functioning (χ² = 10.16, p = 0.017) but not the other clinical outcomes (χ²s ≤ 4.66, ps ≥ 0.198). Follow-up contrasts showed significantly greater improvement in global functioning at six-month follow-up (B = 7.43, SE = 3.62, p = 0.040) and 12-month follow-up (B = 10.74, SE = 3.45, p = .002) for individuals with high education compared to individuals with low education (Fig. 1a). There was a similar pattern at post-intervention, although the difference did not reach statistical significance (B = 6.12, SE = 3.15, p = 0.053).
Fig. 1. The effects of education level on Global Functioning (SOFAS), and of Sex on Psychotic Distress (CAARMS).
a The effects of Education on Global Functioning (SOFAS), b The effects of Sex on Psychotic Distress (CAARMS).
For exploratory analyses, only the omnibus-test investigating the effects of sex on psychotic distress was significant (χ² = 11.52, p = 0.009). Follow-up contrasts showed significantly greater improvement for females compared to males in psychotic distress at 12-month follow-up (B = −61.00, SE = 23.69, p = 0.010) (Fig. 1b). There were no significant differences at any other time point.
Personality traits
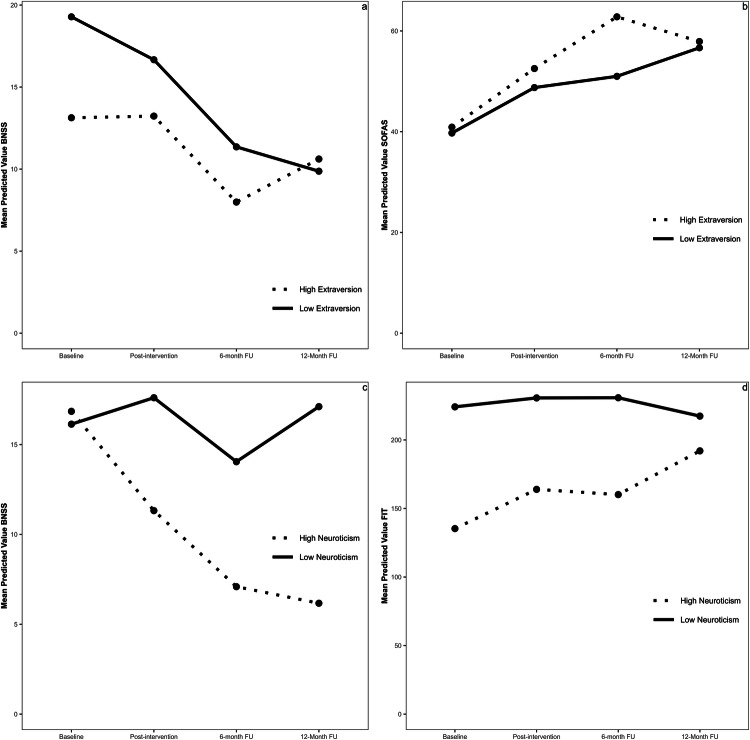
The omnibus-tests investigating the effects of extraversion were significant for negative symptoms (χ² = 15.09, p = 0.002) and global functioning (χ² = 10.06, p = 0.018) but not the other clinical outcomes (χ²s ≤ 7.53, ps ≥ 0.057). For negative symptoms, follow-up contrasts did not show a significant difference at post-intervention (B = 0.79, SE = 0.45, p = 0.080) and six-month follow-up (B = 0.15, SE = 0.52, p = 0.799), but people with lower compared to higher trait extraversion showed a greater improvement at 12-month follow-up (B = 1.24, SE = 0.48, p = 0.011) (Fig. 2a). For global functioning, there was a significantly greater improvement for people with higher compared to lower trait extraversion at post-intervention (B = 0.39, SE = 0.53, p = 0.046) and six-month follow-up (B = 1.40, SE = 0.59, p = 0.018), but this was not retained at the follow-up assessments (p = 0.933) (Fig. 2b).
Fig. 2. The effects of personality traits (extraversion and negative affectivity) on Negative Symptoms (BNSS), Global Functioning (SOFAS), and Psychological Flexibility (FIT).
a The effects of Extraversion on Negative Symptoms (BNSS), b The effects of Extraversion on Global Functioning (SOFAS). c The effects of Negative affectivity on Negative symptoms (BNSS), d The effects of Negative affectivity on Psychological Flexibility (FIT). For the purpose of these plots we redefined the continuous variables Extraversion and Negative Affectivity as binary groups. The 25% lowest scores of Extraversion and Negative Affectivity were defined as the Low-groups, and the 25% highest scores of Extraversion and Negative Affectivity were defined as the High-groups.
The omnibus-tests investigating the effects of negative affectivity were significant for negative symptoms (χ² = 11,28, p = 0.010) and psychological flexibility (χ² = 14.22, p = 0.003). Follow-up contrasts showed significantly greater improvement in negative symptoms (B = −1.59, SE = 0.49, p = 0.001) and psychological flexibility (B = 8.38, SE = 2.43, p = 0.001) at 12-month follow-up for people with higher compared to lower trait negative affectivity (Fig. 2c, d). There were no significant differences at any other time point.
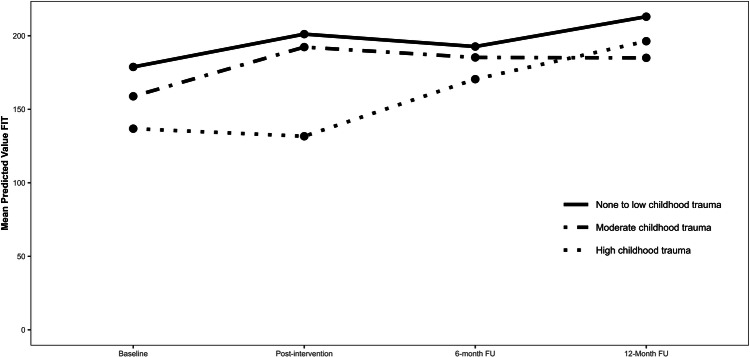
Childhood trauma
The omnibus-tests investigating the effects of childhood trauma were significant only for individuals with high childhood trauma compared to none-to-low childhood trauma on psychological flexibility (χ² = 7.88, p = 0.049). However, follow-up contrasts did not show significant differences at any time point (ps ≥ 0.184) (Fig. 3).
Fig. 3.
The effects of Childhood Trauma on Psychological Flexibility (FIT).
Discussion
The present study examined if inter-individual factors moderated treatment responses in individuals experiencing early-stage psychosis who utilized the blended-care intervention ACT-DL [10]. We found that none of the moderators we examined negatively affected the effect of ACT-DL on clinical outcomes, meaning that ACT-DL may be an appropriate intervention for a wide range of individuals with early psychosis. While ACT-DL was generally effective, some moderators significantly influenced the improvement rate, with the most reliable effects for education and personality traits. Importantly, most of the significant effects were observed at the 6 and 12-month follow-ups, raising the possibility that our results may reflect differences in retention rates rather than immediate treatment responses.
For demographics, individuals with a higher educational background consistently showed more significant improvement in global functioning than those with a lower educational background over time. This result partially confirms our hypothesis that individuals with higher education would benefit more from ACT-DL, and converges with prior research on the effects of education on clinical outcomes in early psychosis [52, 53]. It is possible that the retained benefits in global functioning over time can be explained by other unobserved variables related to education level [54]. For example, socioeconomic status, better cognitive functioning, and baseline symptom severity might have influenced completion of between-session homework activities or ability to implement learned skills during moments of need. Recognizing the importance of equitable health outcomes, we see a need for future research exploring adaptations that could enhance the intervention’s efficacy for those with lower educational backgrounds. Identifying traits of lower-educated individuals who benefit from the intervention could inform these adaptations, aiming for inclusivity and optimal health outcomes for all participants. Moreover, recent qualitative findings of a pilot study testing an EMA tool by de Thurah et al. [55, 56] shows that additional therapist support and help in interpreting the EMA data is key to maximizing the benefits of EMA (and EMI’s). Furthermore, focusing on clear and concise instructions and metaphors might increase usability of the app overall. Our exploratory analyses showed that being female was associated with a significant decrease in psychotic distress at 12month FU. However, given that sex did not significantly affect any other outcome, we should conclude that ACT-DL generally works equally well for males and females. Lastly, age did not significantly affect improvement rates.
For personality traits, our results revealed that both extraversion and negative affectivity impacted responses to ACT-DL, albeit not always in keeping with our hypotheses. Consistent with our expectations, individuals with higher trait extraversion initially experienced a more rapid enhancement in their global functioning. However, at 12-month follow-up, higher and lower trait extraversion individuals converged to similar levels of global functioning. Contrary to our expectations, we found that individuals with lower trait extraversion and higher trait negative affectivity significantly improved negative symptoms and psychological flexibility. The pattern of results showed a steady decline in negative symptoms for individuals with low trait extraversion and high trait negative affectivity over time, alongside a steady increase in psychological flexibility, whereas the comparison groups exhibited stable symptom levels from baseline to 12-month follow-up. These effects could be explained by the possibility that individuals with lower extraversion or higher negative affectivity begin treatment with more severe symptoms and lower psychological skills, allowing them more room for growth. Prior research supports this idea, linking lower extraversion to decreased social skills and higher negative affectivity to more severe negative symptoms [19, 57]. A potential regression to the mean due to a broader margin for improvement could offer one explanation for these observations.
Additionally, it is worth considering that individuals with high trait negative affectivity, defined as frequent and intense experiences of negative emotions and interpersonal manifestations, might experience greater benefits from ACT-DL. This is because ACT emphasizes accepting negative emotions and enhancing values-based behaviors, directly addressing these vulnerabilities [58]. Importantly, we found evidence that childhood trauma did not have any moderating effects on clinical outcomes, proving ACT-DL to be a safe and effective treatment for individuals with a history of childhood trauma.
Our study opens multiple avenues for future research. Given that only 59% of our participants completed the full intervention [12], methods to boost therapy engagement are pivotal to maximizing clinical outcomes. One possible solution is to provide personalized feedback on an individual’s ecological-momentary-assessment data (EMA) in an interactive way. For example, embedding an overview page within the app that provides weekly statistics on the user’s EMA data and ACT-exercises might increase engagement with the intervention. Prior research supports this idea and found that personalized feedback is a strong motivator for using EMA tools and enhances uptake and adherence without altering the intervention’s core principles [59–61].
Additionally, integrating the self-monitoring data in individuals regular treatment, in preparation or during individual treatment sessions, might allow participants to gain more insight into their mental health, and how it relates to their daily lives [62, 63]. Another solution is to enhance ACT-DL’s efficacy at the individual level. Bacon et al. (2014) conducted qualitative research in which participants identified the distinct benefits of various ACT components. Mindfulness and Defusion, Acceptance, and Values were linked to stress reduction, providing life direction and meaning, and mitigating distress from unwanted private events, respectively. These findings suggest that different ACT components uniquely impact distinct facets of an individual’s mental health. Future research should explore whether specific ACT-DL components distinctly influence particular symptoms or psychological processes. Such understanding would allow therapists to tailor the ACT-DL intervention to the individual’s unique problem areas (e.g., psychotic distress).
Limitations and future research
While our study provides valuable insights into the effects of moderators on treatment outcomes, several limitations warrant consideration. First, this study aimed to determine if specific moderators affected treatment outcomes in individuals who received ACT-DL. To maintain sufficient power for our confirmatory hypotheses, we narrowed our analysis exclusively to the ACT-DL group, refraining from comparisons with a control group. While we acknowledge the potential limitation of not having a control group, it is imperative to interpret our findings within the context of the primary outcome paper (Myin-Germeys et al. [12]), which found greater improvement in global functioning in negative symptoms for ACT-DL compared to TAU. These findings suggest that the observed effects may not solely be attributed to natural symptom dynamics or general response to interventions. However, future controlled studies conducted on larger samples are essential to validate our findings. Second, our sample comprised both FEP and UHR participants. While both categories signify early psychosis and are temporally and phenomenologically continuous, they represent different illness stages. Given that individuals with FEP had symptoms that reached the criteria for formal diagnosis and UHR did not, it is possible that both groups responded differently to ACT-DL. However, subgroup analysis in the primary study revealed no discernible differences between the UHR and FEP groups, and due to the study’s randomization [11, 12], these and other potential confounding variables were evenly distributed across conditions. Another potential cofounding variable might be the kind of treatment individuals received after the intervention was completed. For example, FEP individuals may have been prescribed antipsychotics throughout the trial. While this was also true for the control condition, and even though significant differences in treatment outcomes were observed between the ACT-DL and control groups [12], it remains unknown whether the longer-term effects identified in this study can be attributed exclusively to the ACT-DL intervention. In conclusion, this study highlights the importance of inter-individual factors as moderators of ACT-DL on clinical outcomes. Responses to ACT-DL were generally promising.
These limitations notwithstanding, this study highlights the importance of inter-individual factors as moderators of ACT-DL on clinical outcomes. We found evidence that education level, negative affectivity, and extraversion predicted improvement rates of ACT-DL in individuals with early psychosis. Future research should replicate these findings in more extensive and diverse samples and explore strategies to enhance the effectiveness of ACT-DL for a broader range of individuals.
Author contributions
RAB is the primary author of this manuscript and developed the research questions, methodology and analysis plan. JRB and GK supervised and reviewed the writing of this manuscript, of which a final review was done by IMG. GL was consulted in the development of the analysis plan, and helped out with the R-coding of the analysis and data-cleaning. RvW, EvA, FS, LdH, MM, MvdG,TvA, TV and UR were part of the INTERACT trial, and provided feedback in the last feedback round before finalizing and submitting the manuscript.
Funding
RB is funded by the European Union’s Horizon 2020 Research and Innovation Program under grant agreement 945263 (IMMERSE). This work was further supported by an ERC Consolidator Grant (ERC-2012-StG, project 309767-INTERACT) and FWO Odysseus Grant (No. G0F8416N) awarded to IMG as well as a NWO VENI Grant (No. 451-13-022) and DFG Heisenberg professorship (No. 389624707) awarded to UR. JRB was supported by a Marie Skłodowska-Curie fellowship (101063326). GK is supported by the Research Foundation Flanders (12ZZM21N/1204924 N). TV was supported by a Postdoctoral Fellowship grant from Research Foundation Flanders (FWO 1243620 N).
Data availability
Deidentified data are available upon request through a data access system, Data Curation for Open Science (DROPS), administered via REDCap at the Center for Contextual Psychiatry, KU Leuven. Interested researchers can submit an abstract, which is subject to review by the research team to ensure there is no overlap with existing projects. Following abstract approval, a variable access request is submitted, and researchers are required to preregister their analysis plan. A dataset containing only variables required for the proposed analysis is then released to the researchers by a data manager, along with a time- and date-stamped receipt of data access.
Competing interests
The authors declare no competing interests.
Ethical standards
The study received ethical approval from the MERC at Maastricht University Medical Centre (MUMC), the Netherlands (reference: NL46439.068.13) and the University Clinic Leuven, Belgium (reference: B322201629214). Written consent was obtained from each participant prior to assessment and randomization, as detailed in the study protocol (version 12, 18 May 2018). The trial was prospectively registered in the Netherlands Trial Register (NTR4252). All methods were performed in accordance with the relevant guidelines and regulations.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.DeRosse P, Karlsgodt KH. Examining the psychosis continuum. Curr Behav Neurosci Rep. 2015;2:80–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: Evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39:179–95. [DOI] [PubMed] [Google Scholar]
- 3.Yung AR, McGorry PD. The prodromal phase of first-episode psychosis: Past and current conceptualizations. Schizophr Bull. 1996;22:353–70. [DOI] [PubMed] [Google Scholar]
- 4.Fusar-Poli P, Borgwardt S, Bechdolf A, Addington J, Riecher-Rössler A, Schultze-Lutter F, et al. The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiatry. 2013;70:107–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Correll CU, Galling B, Pawar A, Krivko A, Bonetto C, Ruggeri M, et al. Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, meta-analysis, and meta-regression. JAMA Psychiatry. 2018;75:555–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mei C, van der Gaag M, Nelson B, Smit F, Pan Yuen H, Berger M, et al. Preventive interventions for individuals at ultra high risk for psychosis: an updated and extended meta-analysis. Clin Psychol Rev. 2021;86:102005. [DOI] [PubMed] [Google Scholar]
- 7.Pauley D, Cuijpers P, Papola D, Miguel C, Karyotaki E. Two decades of digital interventions for anxiety disorders: a systematic review and meta-analysis of treatment effectiveness. Psychol Med. 2023;53:567–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eilert N, Wogan R, Leen A, Richards D. Internet-delivered interventions for depression and anxiety symptoms in children and young people: systematic review and meta-analysis. JMIR Pediatr Parent. 2022;5:e33551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Witt K, Spittal MJ, Pirkis J, Hetrick S, Currier D, Robinson J, et al. Effectiveness of online and mobile telephone applications (‘apps’) for the self-management of suicidal ideation and self-harm: a systematic review and meta-analysis. BMC Psychiatry. 2017;17:297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vaessen T, Steinhart H, Batink T, Klippel A, Van Nierop M, Reininghaus U, et al. ACT in daily life in early psychosis: an ecological momentary intervention approach. Psychosis. 2019;11:93–104. [Google Scholar]
- 11.Reininghaus U, Klippel A, Steinhart H, Vaessen T, Van Nierop M, Viechtbauer W, et al. Efficacy of Acceptance and Commitment Therapy in Daily Life (ACT-DL) in early psychosis: study protocol for a multi-centre randomized controlled trial. Trials. 2019;20:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Myin-Germeys I, van Aubel E, Vaessen T, Steinhart H, Klippel A, Lafit G, et al. Efficacy of acceptance and commitment therapy in daily life in early psychosis: results from the multi-center INTERACT randomized controlled trial. Psychother Psychosom. 2022;91:411–23. 10.1159/000522274. [DOI] [PubMed] [Google Scholar]
- 13.Zapata BC, Fernández-Alemán JL, Idri A, Toval A. Empirical studies on usability of mHealth apps: a systematic literature review. J Med Syst. 2015;39:1–19. [DOI] [PubMed] [Google Scholar]
- 14.Karyotaki E, Kleiboer A, Smit F, Turner DT, Pastor AM, Andersson G, et al. Predictors of treatment dropout in self-guided web-based interventions for depression: an ‘individual patient data’meta-analysis. Psychol Med. 2015;45:2717–26. [DOI] [PubMed] [Google Scholar]
- 15.Antezana G, Venning A, Smith D, Bidargaddi N. Do young men and women differ in well-being apps usage? Findings from a randomised trial. Health Inform J. 2022;28:1–14. [DOI] [PubMed] [Google Scholar]
- 16.Valentine L, McEnery C, Bell I, O’Sullivan S, Pryor I, Gleeson J, et al. Blended digital and face-to-face care for first-episode psychosis treatment in young people: qualitative study. JMIR Ment Health. 2020;7:e18990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fernandez E, Salem D, Swift JK, Ramtahal N. Meta-analysis of dropout from cognitive behavioral therapy: magnitude, timing, and moderators. J Consulting Clin Psychol. 2015;83:1108–22. [DOI] [PubMed] [Google Scholar]
- 18.Bol N, Helberger N, Weert JCM. Differences in mobile health app use: A source of new digital inequalities? Inf Soc. 2018;34:183–93. [Google Scholar]
- 19.Bucher MA, Suzuki T, Samuel DB. A meta-analytic review of personality traits and their associations with mental health treatment outcomes. Clin Psychol Rev. 2019;70:51–63. [DOI] [PubMed] [Google Scholar]
- 20.Kruisdijk, F, Hopman-Rock, M, Beekman, ATF, Hendriksen, IJM. Personality traits as predictors of exercise treatment adherence in major depressive disorder: lessons from a randomised clinical trial. Int J Psychiatry Clin Pract. 2020;24:380-86. 10.1080/13651501.2020.1787452. [DOI] [PubMed]
- 21.Nguyen PLL, Kim HL, Romain AMN, Tabani S, Chaplin WF. Personality change and personality as predictor of change in psychotherapy: a longitudinal study in a community mental health clinic. J Res Personal. 2020;87:103980. [Google Scholar]
- 22.Thalmayer AG. Personality and mental health treatment: Traits as predictors of presentation, usage, and outcome. Psychol Assess. 2018;30:967–77. [DOI] [PubMed] [Google Scholar]
- 23.Scholte-Stalenhoef AN, Pijnenborg GHM, Hasson-Ohayon I, Boyette L-L. Personality traits in psychotic illness and their clinical correlates: A systematic review. Schizophr Res. 2023;252:348–406. [DOI] [PubMed] [Google Scholar]
- 24.Boyette LL, Korver-Nieberg N, Verweij K, Meijer C, Dingemans P, Cahn W, et al. Associations between the Five-Factor Model personality traits and psychotic experiences in patients with psychotic disorders, their siblings and controls. Psychiatry Res. 2013;210:491–7. [DOI] [PubMed] [Google Scholar]
- 25.Bagby RM, Bindseil KD, Schuller DR, Rector NA, Young LT, Cooke RG, et al. Relationship between the five-factor model of personality and unipolar, bipolar and schizophrenic patients. Psychiatry Res. 1997;70:83–94. [DOI] [PubMed] [Google Scholar]
- 26.Beauchamp MC, Lecomte T, Lecomte C, Leclerc C, Corbière M. Personality traits in early psychosis: relationship with symptom and coping treatment outcomes. Early Interven Psychiatry. 2011;5:33–40. [DOI] [PubMed] [Google Scholar]
- 27.Vila-Badia R, Butjosa A, Del Cacho N, Serra-Arumí C, Esteban-Sanjusto M, Ochoa S, et al. Types, prevalence and gender differences of childhood trauma in first-episode psychosis. What is the evidence that childhood trauma is related to symptoms and functional outcomes in first episode psychosis? A systematic review. Schizophr Res. 2021;228:159–79. [DOI] [PubMed] [Google Scholar]
- 28.Ajnakina O, Trotta A, Di Forti M, Stilo SA, Kolliakou A, Gardner-Sood P, et al. Different types of childhood adversity and 5-year outcomes in a longitudinal cohort of first-episode psychosis patients. Psychiatry Res. 2018;269:199–206. [DOI] [PubMed] [Google Scholar]
- 29.Thomas S, Höfler M, Schäfer I, Trautmann S. Childhood maltreatment and treatment outcome in psychotic disorders: a systematic review and meta-analysis. Acta Psychiatr Scandinavica. 2019;140:295–312. [DOI] [PubMed] [Google Scholar]
- 30.Batink T, Bakker J, Vaessen T, Kasanova Z, Collip D, van Os J, et al. Acceptance and commitment therapy in daily life training: a feasibility study of an mhealth intervention. JMIR Mhealth Uhealth. 2016;4:e103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Myin-Germeys I, Klippel A, Steinhart H, Reininghaus U. Ecological momentary interventions in psychiatry. Curr Opin Psychiatry. 2016;29:258–63. [DOI] [PubMed] [Google Scholar]
- 32.Hayes, SC. Acceptance and commitment therapy and the new behaviour therapies. Mindfulness Accept. Expanding the Cognitive-behavioral Tradition. 1–29 (2004).
- 33.Hayes SC, Strosahl KD, Wilson KG. (2011) Acceptance and commitment therapy: The process and practice of mindful change. Guilford press. ISBN 9781609189648.
- 34.Shawyer F, Shawyer F, Farhall J, Thomas N, Hayes SC, Gallop R, et al. Acceptance and commitment therapy for psychosis: Randomised controlled trial. Br J Psychiatry. 2017;210:140–8. [DOI] [PubMed] [Google Scholar]
- 35.Eysenck SBG, Eysenck HJ, Barrett P. A revised version of the psychoticism scale. Personal Individ Differ. 1985;6:21–9. [Google Scholar]
- 36.Maragakis, A (2020). Eysenck Personality Questionnaire‐Revised. The wiley encyclopedia of personality and individual differences: Measurement and assessment, 283-6.
- 37.Caruso JC, Witkiewitz K, Belcourt-Dittloff A, Gottlieb JD. Reliability of scores from the Eysenck personality questionnaire: a reliability generalization study. Educ Psychol Meas. 2001;61:675–89. [Google Scholar]
- 38.Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abus Negl. 2003;27:169–90. [DOI] [PubMed] [Google Scholar]
- 39.Kuzminskaite E, Vinkers CH, Milaneschi Y, Giltay EJ, Penninx BWJH. Childhood trauma and its impact on depressive and anxiety symptomatology in adulthood: a 6-year longitudinal study. J Affect Disord. 2022;312:322–30. [DOI] [PubMed] [Google Scholar]
- 40.Devi F, Shahwan S, Teh WL, Sambasivam R, Zhang YJ, Lau YW, et al. The prevalence of childhood trauma in psychiatric outpatients. Ann Gen Psychiatry. 2019;18:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Longden E, Sampson M, Read J. Childhood adversity and psychosis: generalised or specific effects? Epidemiol Psychiatr Sci. 2016;25:349–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yung AR, Yung AR, Pan Yuen H, Mcgorry PD, Phillips LJ, Kelly D, et al. Mapping the onset of psychosis: the comprehensive assessment of at-risk mental states. Aust NZ J Psychiatry. 2005;39:964–71. [DOI] [PubMed] [Google Scholar]
- 43.Kline E, Schiffman J. Psychosis risk screening: a systematic review. Schizophr Res. 2014;158:11–18. [DOI] [PubMed] [Google Scholar]
- 44.Oliver D, Kotlicka-Antczak M, Minichino A, Spada G, McGuire P, Fusar-Poli P. Meta-analytical prognostic accuracy of the Comprehensive Assessment of at Risk Mental States (CAARMS): the need for refined prediction. Eur Psychiatry. 2018;49:62–8. [DOI] [PubMed] [Google Scholar]
- 45.Kirkpatrick B, Strauss GP, Nguyen L, Fischer BA, Daniel DG, Cienfuegos A, et al. The brief negative symptom scale: psychometric properties. Schizophr Bull. 2011;37:300–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kirkpatrick B, Fenton WS, Carpenter WT, Marder SR. The NIMH-MATRICS consensus statement on negative symptoms. Schizophr Bull. 2006;32:214–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tatsumi K, Kirkpatrick B, Strauss GP, Opler M. The brief negative symptom scale in translation: a review of psychometric properties and beyond. Eur Neuropsychopharmacol. 2020;33:36–44. [DOI] [PubMed] [Google Scholar]
- 48.Goldman HH, Skodol AE, Lave TR. Revising axis V for DSM-IV: a review of measures of social functioning. Am J Psychiatry. 1992;149:1148–56. [DOI] [PubMed] [Google Scholar]
- 49.Batink T, Jansen G, de Mey H. De Flexibiliteits Index Test (FIT-60): Een beknopte beschrijving. GZ - Psychol. 2012;4:18–21. [Google Scholar]
- 50.Batink T, Delespaul P. Meten van psychologische flexibiliteit: De Flexibiliteits Index Test (FIT-60) [Measuring psychological flexibility: The Flexibility Index Test (FIT-60)]. Gedragstherapie. 2015;48:310–332. [Google Scholar]
- 51.Pinheiro J, Bates D, R Core Team (2024). nlme: Linear and Nonlinear Mixed Effects Models. R package version 3.1-166, https://CRAN.R-project.org/package=nlme.
- 52.Swift JK, Greenberg RP. A treatment by disorder meta-analysis of dropout from psychotherapy. J Psychother Integr. 2014;24:193–207. [Google Scholar]
- 53.Ayesa-Arriola R, Miguel-Corredera M, de la Foz VOG, Neergaard KD, Correa-Ghisays P, Setién-Suero E, et al. Education and long-term outcomes in first episode psychosis: 10-year follow-up study of the PAFIP cohort. Psychol Med. 2023;53:66–77. [DOI] [PubMed] [Google Scholar]
- 54.Myin-Germeys, I, Van Aubel, E, Vaessen, T, Steinhart, H, Klippel, A, Lafit, G, et al. Acceptance and Commitment Therapy in Daily Life (ACT-DL) in early psychosis: findings on treatment adherence and acceptability from the multi-center INTERACT randomized controlled trial. Psychother Psychosomatics. (2021) 10.1159/000522274. [DOI] [PubMed]
- 55.Norrgren LJ. The highly educated live longer: the role of time preference, cognitive ability, and educational plans. Health Econ. 2023;32:1767–84. [DOI] [PubMed] [Google Scholar]
- 56.de Thurah L, Kiekens G, Weermeijer JDM, Uyttebroek L, Wampers M. Bonnier R, & Myin-Germeys I. (2024, April 6). Understanding appropriation of digital self-monitoring tools in mental health care – an implementation pilot. 10.31219/osf.io/fm8kt [Preprint].
- 57.Sarubin N, Wolf M, Giegling I, Hilbert S, Naumann F, Gutt D, et al. Neuroticism and extraversion as mediators between positive/negative life events and resilience. Personal Individ Differences. 2015;82:193–8. [Google Scholar]
- 58.Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behav Res Ther. 2006;44:1–25. [DOI] [PubMed] [Google Scholar]
- 59.de Thurah L, Kiekens G, Sips R, Teixeira A, Kasanova Z, Myin-Germeys I. Using experience sampling methods to support clinical management of psychosis: the perspective of people with lived experience. Psychiatry Res. 2023;324:115207. [DOI] [PubMed] [Google Scholar]
- 60.Piot M, Mestdagh M, Riese H, Weermeijer J, Brouwer JM, Kuppens P, et al. Practitioner and researcher perspectives on the utility of ecological momentary assessment in mental health care: A survey study. Internet Interven. 2022;30:100575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Weermeijer J, Kiekens G, Wampers M, Kuppens P, Myin-Germeys I. Practitioner perspectives on the use of the experience sampling software in counseling and clinical psychology. Behav Inform Technol. 2023;0:1–11. [Google Scholar]
- 62.Folkersma W, Veerman V, Ornée DA, Oldehinkel AJ, Alma MA, Bastiaansen JA. Patients’ experience of an ecological momentary intervention involving self-monitoring and personalized feedback for depression. Internet Interven. 2021;26:100436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bell IH, Rossell SL, Farhall J, Hayward M, Lim MH, Fielding-Smith SF, et al. Pilot randomised controlled trial of a brief coping-focused intervention for hearing voices blended with smartphone-based ecological momentary assessment and intervention (SAVVy): Feasibility, acceptability and preliminary clinical outcomes. Schizophr Res. 2020;216:479–87. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Deidentified data are available upon request through a data access system, Data Curation for Open Science (DROPS), administered via REDCap at the Center for Contextual Psychiatry, KU Leuven. Interested researchers can submit an abstract, which is subject to review by the research team to ensure there is no overlap with existing projects. Following abstract approval, a variable access request is submitted, and researchers are required to preregister their analysis plan. A dataset containing only variables required for the proposed analysis is then released to the researchers by a data manager, along with a time- and date-stamped receipt of data access.