Abstract
Torsion of extralobar pulmonary sequestration is a rare congenital anomalous condition that can manifest with various symptoms, including abdominal pain. However, a masslike lesion in the mediastinum can be easily overlooked when the clinician focuses only on abdominal pain. By using magnetic resonance imaging, a few features specific to the torsion of extralobar pulmonary sequestration can be identified, and that information will be helpful.
Torsion of extralobar pulmonary sequestration (ELS) is a rare condition that can manifest with various symptoms, including acute chest or abdominal pain, shortness of breath, or hemoptysis. In pulmonary sequestration, a nonfunctioning mass of lung tissue lacks normal communication with the tracheobronchial tree and always receives its arterial blood supply from the systemic circulation. Pulmonary sequestrations are divided into ELS and intralobar sequestration according to the relationship of the aberrant segmental lung tissue with the pleura. Symptomatic ELS caused by pedicle torsion is extremely rare, and early recognition is difficult, especially when a patient presents to the hospital with abdominal pain. Pleural effusion or a masslike lesion in the mediastinum is often seen in imaging tests. However, this finding can be easily overlooked when medical staff focuses only on “abdominal pain.” Magnetic resonance imaging (MRI) is a helpful tool for differential diagnosis in that situation. We describe a case of recurrent abdominal pain and fever caused by torsion of ELS in a 12-year-old girl.
A 12-year-old healthy girl visited our emergency department (Chungnam National University Hospital, Daejeon, Republic of Korea) with a 2-day history of fever and abdominal pain on the right side. She had visited the local emergency department 2 days earlier for acute abdominal pain with mild fever, but symptoms were relieved after intravenous fluid treatment. On the night of discharge, she felt abdominal pain and fever again, and she visited our emergency department. Abdominal roentgenograms taken at a local hospital showed a high-density mass in the right thoracic cavity with a small amount of pleural effusion, which was not noticed initially (Figure 1). There were no remarkable findings in the physical examination and medical history. Laboratory test results showed slight elevations in the white blood cell count (12,300/μL), of which the neutrophils accounted for 77.64%. The C-reactive protein level was 4.98 mg/dL, and other values were within normal ranges. A computed tomographic scan of the chest and abdomen revealed a well-defined, subtly enhancing mass with soft tissue density (4.6 cm × 1.3 cm × 4.6 cm) in the right posterior paravertebral area with a small amount of pleural effusion (Figure 2A). A suspected feeding artery arising from the aorta was identified.
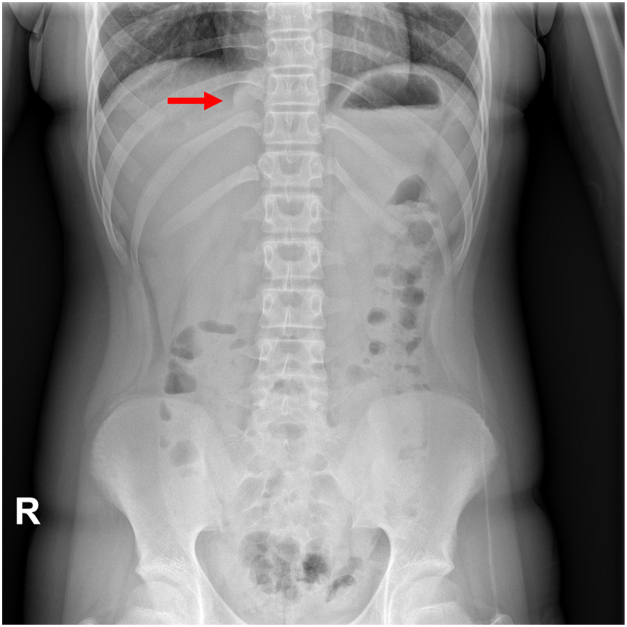
Figure 1.
Initial abdominal roentgenogram. A high-attenuated, dense, masslike lesion (arrow) was found on the right mediastinal area. (R, right.)
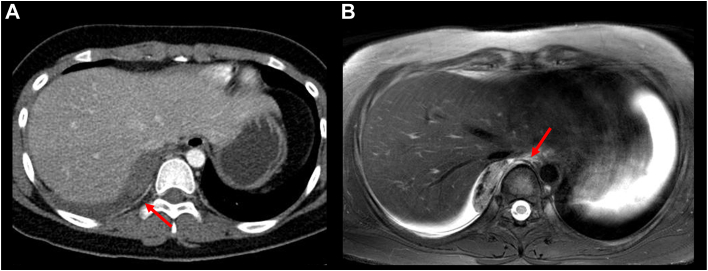
Figure 2.
(A) Axial image of chest computed tomography. There are small amounts of pleural effusion in the right pleural cavity. A nonenhanced soft tissue mass with a suspected feeding artery (arrow) was seen. The mass was not clearly distinguishable from pleural effusion. (B) T2-weighted image of chest magnetic resonance imaging. A well-marginated, oval, heterogeneous mass with a small amount of pleural effusion was seen. The feeding artery from the descending aorta was also found (arrow).
To differentiate between pulmonary sequestration with combined torsion and a posterior mediastinal mass, such as a neurogenic tumor, MRI of the chest was performed. The imaging revealed a well-marginated, oval, heterogeneously enhancing mass in the right posterior mediastinum. In T2-weighted axial images, the mass contained dark signal intensity without enhancement, a finding suggestive of old internal hemorrhage and infarction (Figure 2B).
Two-port video-assisted thoracoscopic surgery was performed. A dark brown ovoid mass (4.2 cm × 3.6 cm × 1.5 cm) adherent to the aortic wall and a small amount of hemorrhagic pleural effusion were found (Figure 3A). The pedicle that connected the mass to the mediastinum was short and twisted multiple times, and it contained feeding vessels (Figure 3B). The mass was clipped and then resected at the pedicle. Pathologic examination revealed nonneoplastic lung parenchyma with diffuse congestion. Clinically, it was ELS with infarction caused by torsion. The patient recovered uneventfully and was discharged on the second day after surgery. No complication or recurrence was observed on the chest and abdominal roentgenograms during a 2-year follow-up period.
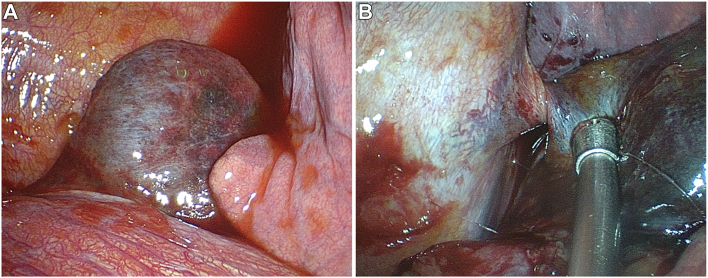
Figure 3.
Intraoperative findings. (A) A congested hemorrhagic mass was seen at the posterior mediastinal space without connection to the pulmonary system. Small amounts of hemorrhagic pleural effusion were found. (B) The pedicle, which contains feeding vessels originating from the descending thoracic aorta, was twisted multiple times.
Comment
Pulmonary sequestration is rare but is the second most common congenital lung anomaly.1 Pulmonary sequestration is divided into intralobar and extralobar subtypes. The intralobar type, which accounts for approximately 75% of pulmonary sequestration, is located within a normal lobe and lacks its own visceral pleura. ELSs account for 25% of pulmonary sequestrations and are located outside the normal lung. ELSs have their own visceral pleura, are usually asymptomatic, and are found prenatally or incidentally. Torsion and infarction of ELS are extremely rare.
ELS has a 3:1 to 4:1 male predominance in most of the reported prenatal series, with 65% of cases occurring on the left side between the left lower lobe and the diaphragm.1 The patient in this case was female, and ELS was found on the right side.
Because the initial symptoms in children mainly consist of abdominal pain, the diagnosis is either missed or delayed.2 The symptoms of ELS with torsion depend on the location of the lesion and whether the child can express their symptoms clearly. If a young patient presents with sudden abdominal pain, and if computed tomography shows a homogenous, well-defined mass of soft tissue density in the thorax, the clinician should suspect ELS with torsion.
The appearance of a feeding artery and the absence of enhancement in the mass may indicate ELS torsion. MRI is known to be helpful in the differential diagnosis of ELS torsion. In most of the reported cases, infarcted lesions were typically found within pleural effusion secondary to poor lymphatic drainage.1 On MRI, even scant pleural effusion can be depicted on T2-weighted images, thus allowing the clinician to distinguish the lesion from the pleural effusion and surrounding soft tissues.2 By using subtraction images of gradient-echo chemical shift images, intact subpleural fat, which suggests that the lesion is located within the pleural cavity, can be identified.2 To differentiate ELS from mediastinal tumors, it is essential to determine whether the mass is in the extrapulmonary and intrapleural space or not.2,3 This placement can also be confirmed with MRI.
Furthermore, when the signal on the subtraction image is lower than that of the normal lung tissue, the presence of iron or hemorrhage is strongly suggested, indicating that ELS was twisted and infarcted.2 The characteristics of an internal hemorrhagic are also important in differentiating ELS torsion from other solitary masses.2,3 Thus, a few features specific to the torsion of ELS can be identified using several MRI protocols.
Surgical resection is the standard treatment for ELS with torsion. Because minimally invasive surgical approaches are possible and surgical procedures are simple, video-assisted thoracoscopic surgery should be considered when ELS with torsion is suspected.
Declaration of Generative Artificial Intelligence and Artificial Intelligence–assisted Technologies
During the preparation of this work, we used Grammarly to check for grammatical errors. After using this tool, we reviewed and edited the content as needed, and we take full responsibility for the content of the publication.
Acknowledgments
Funding Sources
The authors have no funding sources to disclose.
Disclosures
The authors have no conflicts of interest to disclose.
Patient Consent
Obtained.
References
- 1.Gabelloni M., Faggioni L., Accogli S., Aringhieri G., Neri E. Pulmonary sequestration: what the radiologist should know. Clin Imaging. 2021;73:61–72. doi: 10.1016/j.clinimag.2020.11.040. [DOI] [PubMed] [Google Scholar]
- 2.Yokota R., Sakamoto K., Urakawa H., Takeshita M., Yoshimitsu K. Torsion of right lung sequestration mimicking a posterior mediastinal mass presenting as acute abdomen: usefulness of MR imaging. Radiol Case Rep. 2019;14:551–554. doi: 10.1016/j.radcr.2019.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Choe J., Goo H.W. Extralobar pulmonary sequestration with hemorrhagic infarction in a child: preoperative imaging diagnosis and pathological correlation. Korean J Radiol. 2015;16:662–667. doi: 10.3348/kjr.2015.16.3.662. [DOI] [PMC free article] [PubMed] [Google Scholar]