Abstract
There are several options for intrathoracic esophagogastric anastomosis during Ivor Lewis esophagectomy. These include end-to-end stapled anastomosis, handsewn anastomosis, and stapled anastomosis. We present the case of an 84-year-old man with benign esophageal stricture who underwent robot-assisted laparoscopic and thoracoscopic Ivor Lewis esophagectomy with a total portal robotic linear stapled anastomosis that allowed intrathoracic esophagogastric anastomosis creation entirely using the robotic platform. This technique alleviates the need for a skilled bedside assistant and further demonstrates the convenience, maneuverability, and dexterity of the robotic platform.
First described in 1946, Ivor Lewis esophagectomy originally involved a 2-stage procedure wherein the stomach would first be mobilized through a laparotomy followed 10 to 15 days later with an open right thoracotomy, esophageal resection, and intrathoracic esophagogastric anastomosis.1 Laparoscopy and video-assisted thoracoscopy subsequently decreased perioperative morbidity. At our institution, we have adopted a robotic platform (Intuitive Surgical Inc) that offers greater maneuverability and dexterity compared with traditional laparoscopy or thoracoscopy. In this report, we detail the total portal robotic linear stapled anastomosis technique for intrathoracic anastomosis that improves the efficiency and convenience of robot-assisted Ivor Lewis esophagectomy.
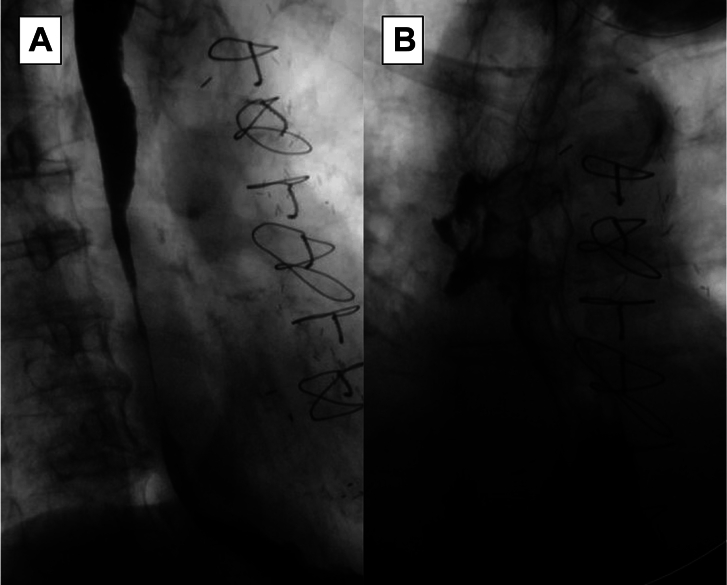
We present the case of an 84-year-old man with a past medical history of coronary artery disease, chronic kidney disease, type 2 diabetes mellitus, and known hiatal hernia. His surgical history was significant for 4-vessel coronary artery bypass graft. He reported a 6-month history of progressively worsening dysphagia and 20-pound weight loss. His gastroenterologist identified a 4-cm-long esophageal stricture 30 cm from the incisors and performed dilations of the stricture up to 8 mm. Biopsy specimens taken during a previous esophagogastroduodenoscopy demonstrated a benign stricture. Esophagography demonstrated severe stenosis at the site of the stricture (Figure 1A). The stricture was refractory to endoscopic dilation, and he was scheduled for robot-assisted Ivor Lewis esophagectomy. He underwent jejunostomy tube placement for preoperative nutritional optimization.
Figure 1.
Barium esophagography. (A) Preoperative esophagogram demonstrates severe stenosis of the midesophagus consistent with esophageal stricture. (B) Postoperative esophagogram demonstrates patent anastomosis without extravasation of contrast material.
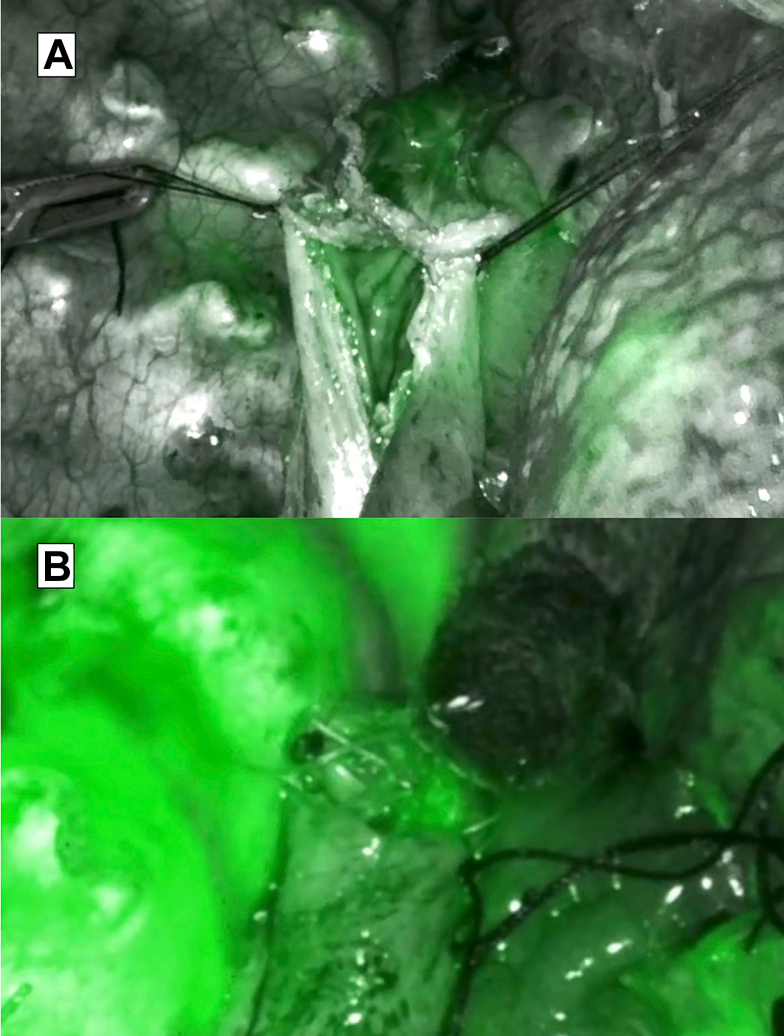
The steps of the operation as well as port placement are highlighted in the Video. The abdominal portion of the case began with dissection of the diaphragmatic hiatus. An omental patch was mobilized from the greater omentum to later reinforce the esophagogastric anastomosis. Care was taken to preserve the omental branch of the left gastroepiploic artery to supply the omental patch and the right gastroepiploic artery to supply the gastric tube. A Penrose drain was passed around the esophagus to aid with retraction. The left gastric artery was ligated and the robotic stapler was used to create a 3-cm gastric tube beginning at the incisura angularis, working toward the fundus of the stomach. Indocyanine green and Firefly fluorescence imaging (Intuitive Surgical Inc) were used to assess perfusion of the gastric conduit. The abdominal component of the operation concluded with Botox injection (100 units) in the pylorus for improved gastric emptying.
The patient was repositioned in the left lateral decubitus position for the thoracic portion of the case. The right lung was retracted medially, and the pleura was dissected from the distal esophagus to the level of the azygos vein, which was divided with the white load robotic stapler. With use of the Penrose drain for retraction, the esophagus was dissected circumferentially with a vessel sealer beginning from the hiatus and continuing proximally until the esophagus proximal to the stricture was mobilized. This was confirmed with intraoperative esophagogastroduodenoscopy. The esophagus was divided with the robotic blue load stapler. The remainder of the proximal stomach, gastric conduit, and omental patch were brought into the chest. Indocyanine green was used to identify the most proximal well-perfused portion of the gastric tube. This was divided with the robotic stapler. The resection of the distal esophagus and remnant stomach was now complete.
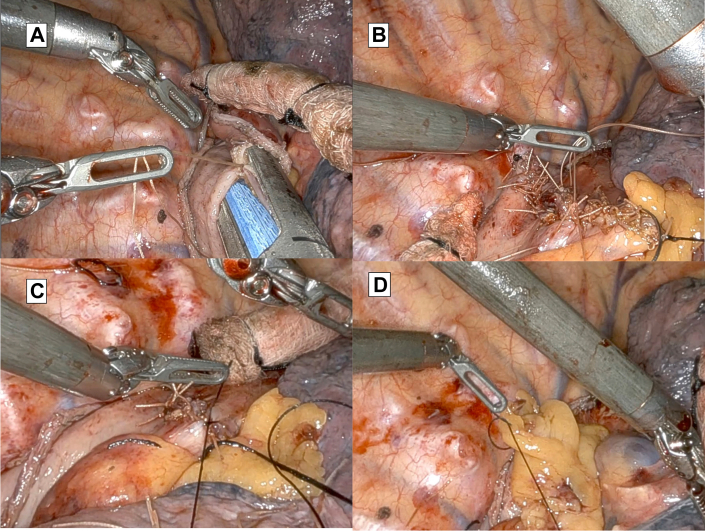
A 3-0 absorbable stitch brought together the esophagus and gastric tube and reduced tension on the anastomosis. Bipolar forceps were used to create a gastrotomy on the greater curvature of the stomach and an esophagotomy in the middle of the esophageal staple line. A common channel was created between the esophagus and gastric tube using a robotic blue load stapler (Figure 2A). Indocyanine green demonstrated adequate perfusion of the stapled anastomosis (Figure 3A). The esophageal staple line was removed and sent for pathologic examination. The common channel was closed with full-thickness simple interrupted, 3-0 absorbable sutures (Figure 2B). Indocyanine green demonstrated adequate perfusion of the anastomosis (Figure 3B). The suture line was imbricated with partial-thickness 3-0 silk sutures in a Lembert fashion (Figure 2C). Finally, the omental patch was secured over the closure with simple interrupted 3-0 silk sutures (Figure 2D). The specimen was removed before the conclusion of the case by enlarging the 12-mm port site. A 28F chest tube and nasogastric tube were placed before the conclusion of the case. Postoperatively, the patient did well. On postoperative day 1, the chest tube was placed to water seal, and trickle feeds were started through the jejunostomy tube and progressively advanced. The chest tube was removed on postoperative day 6, and he was discharged home on postoperative day 7 on jejunostomy tube feeding. Esophagography at postoperative week 2 demonstrated no leak or residual stenosis (Figure 1B). Final pathologic examination finding was benign esophageal mucosa with ulcer and granulation tissue. About 3 months after operation, stricture developed at the anastomosis that was successfully treated with serial endoscopic dilation.
Figure 2.
Image of total robotic anastomosis. (A) A common enterotomy between the proximal esophagus and the gastric tube is created using the robotic blue load stapler. (B) The enterotomy is closed with full-thickness, 3-0 absorbable suture in a simple interrupted fashion. (C) Suture line is imbricated with 3-0 silk suture. (D) Omental patch is secured with 3-0 silk suture.
Figure 3.
Indocyanine green angiography. (A) After the stapled anastomosis is made, indocyanine green angiography shows well-perfused mucosa of the esophagus and the gastric conduit. (B) After the closure of the enterotomy, indocyanine green angiography shows a well-perfused suture line.
Comment
Robot-assisted Ivor Lewis esophagectomy demonstrates several advantages compared with other esophagectomy approaches. Compared with traditional thoracoscopic or laparoscopic esophageal dissection, the robotic platform allows greater maneuverability due to the wristed nature of the instruments. Indocyanine green capability is standard on the robotic platform, which allows intraoperative assessment of tissue perfusion, whereas the gross appearance of the tissue may be more transient. In a meta-analysis by Mederos and coworkers2 comparing robot-assisted esophagectomy vs open or video-assisted esophagectomy, robot-assisted esophagectomy demonstrated decreased blood loss and pulmonary and overall complications. Intrathoracic anastomosis was also shown to have lower rate of anastomotic leak and severe complications compared with cervical anastomosis in a randomized clinical trial by van Workum and colleagues.3
Various options exist for intrathoracic esophagogastric anastomosis during Ivor Lewis esophagectomy. In a randomized controlled trial comparing combined stapled/handsewn, totally handsewn, and circular end-to-end stapled anastomoses, Wang and coworkers4 demonstrated that the combined stapled/handsewn technique was associated with a significantly lower incidence of anastomotic stricture. The total portal linearly robotic stapled anastomosis with handsewn closure described here allows the robotic platform to be used to its full extent without the surgeon having to return to the bedside until the conclusion of the operation. This technique also avoids a large thoracotomy, reducing postoperative pain and the risk of significant respiratory complications. Further investigation is needed to quantify the potential benefit of the total portal linearly stapled anastomosis.
The Video can be viewed in the online version of this article [https://doi.org/10.1016/j.atssr.2022.12.006] on http://www.annalsthoracicsurgery.org.
Acknowledgments
Funding Sources
The authors have no funding sources to disclose.
Disclosures
Min P. Kim reports a relationship with Intuitive Surgical Inc that includes: consulting or advisory and speaking and lecture fees. Min P. Kim reports a relationship with Olympus Corporation of the Americas that includes: consulting or advisory and speaking and lecture fees. Min P. Kim reports a relationship with Medtronic Inc that includes: consulting or advisory and speaking and lecture fees. Min P. Kim reports a relationship with AstraZeneca Pharmaceuticals LP that includes: consulting or advisory. Edward Y. Chan reports a relationship with Intuitive Surgical Inc that includes: consulting or advisory and speaking and lecture fees. Edward Y. Chan reports a relationship with Olympus Corporation of the Americas that includes: consulting or advisory and speaking and lecture fees.
Patient Consent
Obtained.
Footnotes
Accepted for presentation at the Video Session of the Sixty-ninth Annual Meeting of the Southern Thoracic Surgical Association, Fort Lauderdale, FL, Nov 9-12, 2022 [canceled].
Supplementary Data
References
- 1.Reed C.E. Technique of open Ivor Lewis esophagectomy. Oper Tech Thorac Cardiovasc Surg. 2009;14:160–175. [Google Scholar]
- 2.Mederos M.A., de Virgilio M.J., Shenoy R., et al. Comparison of clinical outcomes of robot-assisted, video-assisted, and open esophagectomy for esophageal cancer: a systematic review and meta-analysis. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.29228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Workum F., Verstegen M.H., Klarenbeek B.R., et al. Intrathoracic vs cervical anastomosis after totally or hybrid minimally invasive esophagectomy for esophageal cancer: a randomized clinical trial. JAMA Surg. 2021;156:601–610. doi: 10.1001/jamasurg.2021.1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang W.P., Gao Q., Wang K.N., et al. A prospective randomized controlled trial of semi-mechanical versus hand-sewn or circular stapled esophagogastrostomy for prevention of anastomotic stricture. World J Surg. 2013;37:1043–1050. doi: 10.1007/s00268-013-1932-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.