Abstract
A 55-year-old woman with no significant medical history or symptoms was incidentally diagnosed with a mediastinal tumor during a routine health checkup. The intraoperative findings of robot-assisted thoracoscopic surgery led to the diagnosis of extralobar pulmonary sequestration (EPS), with multiple vessels connecting to the pulmonary artery and superior pulmonary vein. EPS, an extremely rare condition, is typically supplied with blood from the aorta. Whereas it is uncommon for blood to be supplied from the pulmonary artery and to drain into the pulmonary vein in EPS, it is safely excised through robot-assisted thoracoscopic surgery.
Extralobar pulmonary sequestration (EPS) is a rare subset that composes approximately 10% to 20% of pulmonary sequestrations.1,2 Whereas it is typically identified in infancy, instances of diagnosis in adulthood are documented. EPS often receives blood supply from the aorta.3 In this case, our initial surgical plan involved robot-assisted thoracoscopic surgery (RATS) based on a preoperative diagnosis suggesting a mediastinal tumor. However, intraoperatively, we encountered a unique case of EPS situated between the left hilum and the aortic arch that was characterized by its vascular supply from the pulmonary artery (PA) and drainage into the pulmonary vein (PV).
A 55-year-old woman with an unremarkable medical history was referred to our hospital after a chest computed tomography (CT) scan performed during a routine health check revealed the presence of a mediastinal tumor. Subsequent contrast-enhanced CT scans of the chest delineated a tumor measuring 47 × 19 × 46 mm, spanning from the left anterior mediastinum to the middle mediastinum. The tumor exhibited a lobulated configuration with smooth margins, presenting as a uniformly thick-walled cystic structure devoid of calcification or fat, with an enhancing component evident on imaging (Figure 1). Positron emission tomography/CT findings indicated no significant standardized uptake value within the tumor. Blood tests, including carcinoembryonic antigen, cytokeratin fragments, anti–acetylcholine receptor antibodies, β-human chorionic gonadotropin, and α-fetoprotein, yielded results with values within normal ranges. A provisional diagnosis of a mediastinal tumor (potentially a cystic thymoma or mucosa-associated lymphoid tissue lymphoma) was established, prompting the planning of surgical resection by RATS.
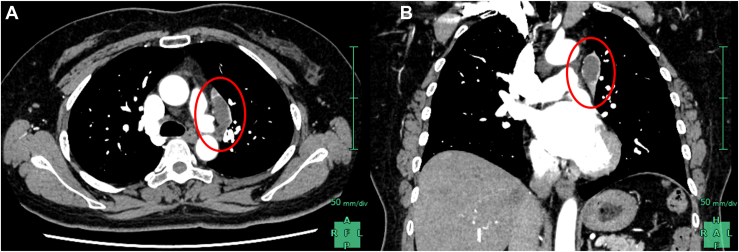
Figure 1.
Contrast-enhanced computed tomography images of a tumor with cysts inside and enhanced margins (circle) extending from the anterior mediastinum to the middle mediastinum. (A) Horizontal section. (B) Coronal section.
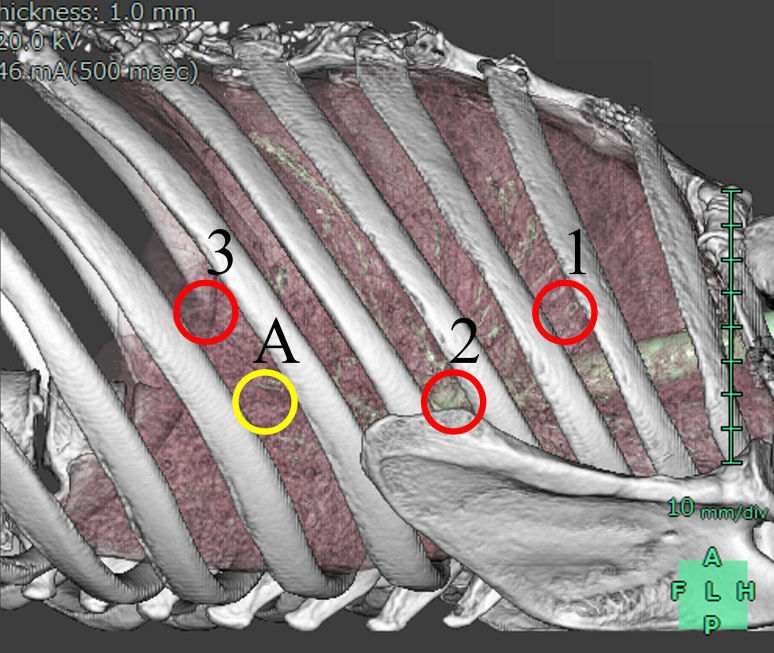
This procedure was performed with the patient in the supine position. Three robotic ports (8 mm) and an additional assist port were introduced (Supplemental Figure). Carbon dioxide insufflation was initiated at 8 cm H2O. The shadow initially presumed to be a tumor preoperatively was situated between the aortic arch and the hilum, more dorsal than the phrenic nerve. Intraoperative diagnosis was most likely to be EPS. The pleurae were divided, and the 2 vessels communicating with the PA and the vessel communicating with the PV were identified. Thereafter, each of them was individually stapled with an Endo GIA (Medtronic). Notably, the cyst revealed by imaging was identified as an ectopic bronchus, discontinuous with the normal tracheobronchial tree (Figure 2). The lung parenchyma was stapled off at the border with the left upper lobe. The excised sequestrated lung’s cystic cavity contained highly viscous white-transparent fluid. The duration of surgery was 187 minutes, with a console time of 152 minutes and a blood loss of 1 mL. The drain was removed on postoperative day 2, and the patient was discharged without complications on postoperative day 5.
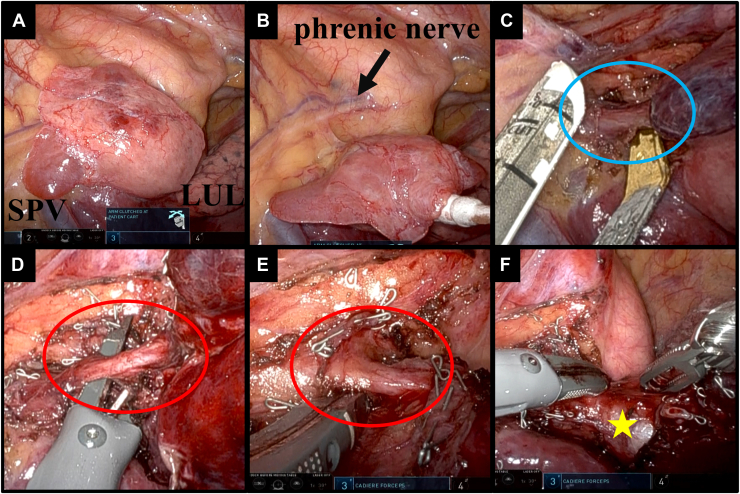
Figure 2.
(A) Intraoperative image of the tumor located dorsal to the phrenic nerve, between the pulmonary hilum and the aorta. (B) Although it is adjacent to the left upper lobe (LUL), it possesses an independent pleura and is considered to be an extralobar pulmonary sequestration. (C) The vessel (circle) communicating with the pulmonary vein was dissected with staples. (D, E) In addition, 2 vessels (circle) communicating with the pulmonary artery were also dissected with staples. (F) The cyst wall (star) consists of tracheal cartilage and does not communicate with the normal bronchus. (SPV, suprapulmonary vein.)
On review of contrast-enhanced CT, 2 vessels flowing into the tumor from a central position more proximal than the left upper lobe’s branching PA and 1 vessel draining into the superior PV were identified. This matched the 3 vessels stapled during surgery. By rendering the tumor invisible on 3-dimensional (3D) CT and displaying the PA and PV, the presence of the 2 vessels connecting to the PA and the vessel connecting to the PV could be confirmed (Figure 3).
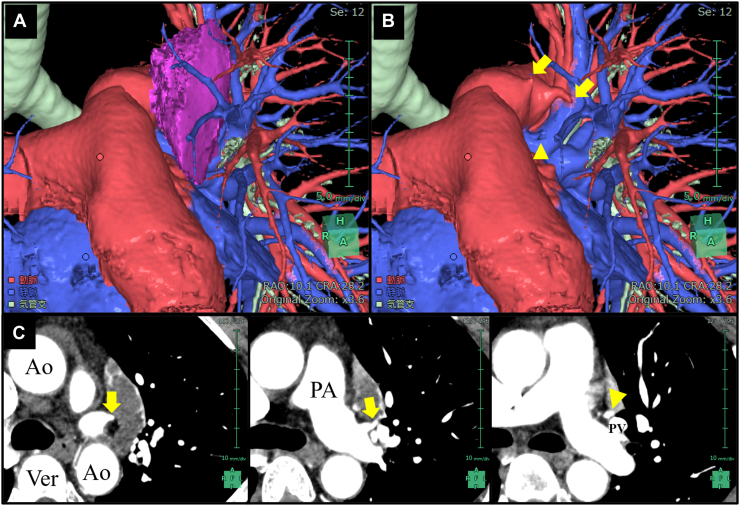
Figure 3.
(A) The vessels communicating with the tumor could not be identified on 3-dimensional computed tomography. (B) However, by hiding the tumor (purple mass), 2 vessels communicating with the pulmonary artery (PA, arrows) and 1 vessel communicating with the pulmonary vein (PV, arrowhead) were visualized. (C) These findings can also be confirmed on contrast-enhanced computed tomography. (Ao, aorta; Ver, Vertebra.)
Pathologic examination confirmed the cyst’s composition. It consisted of bronchial structures with cartilage and a bronchial lining, enveloped by lung tissue exhibiting mucin and hemorrhage, which is consistent with EPS.
Comment
We diagnosed mediastinal tumor initially; however, during surgery, we identified EPS. A review of contrast-enhanced CT and 3D CT postoperatively revealed that the PA and PV were contiguous with EPS. EPS would be the primary differential diagnosis if these vessels had been identified before surgery. 3D CT allows easy understanding of structures and is highly valuable for surgical simulation.4 However, it is crucial to know its limitations, especially on visualizing small vessels near tumors.
EPS tends to occur in the left thoracic cavity; its occurrence in the anterior or middle mediastinum is a rarity, although we have previously encountered cases of mediastinal EPS.5 In this case, the EPS was located between the aortic arch and the pulmonary hilum. However, it was compressed by the surrounding lung tissue, and preoperative imaging suggested that most of the sequestrated lung was situated to the left of the anterior mediastinum, leading to an initial diagnosis of a mediastinal tumor.
In recent reports, EPS excision is often performed through video-assisted thoracoscopic surgery, and in cases with associated anomalies, open surgery may also be employed.6 This is an extremely rare report of EPS excision through RATS in which the PA and PV were the inflow and outflow vessels, respectively. The 2 inflow vessels branching from the PA just after the pericardial reflection were observed. In the event of damage to these vessels, achieving hemostasis might be challenging, which underscores the necessity of precise and safe dissection. In the standard procedure for pulmonary lobe resection, the patient is placed in a lateral position. Therefore, if a preoperative diagnosis of EPS has been established, the surgery would have been conducted with the patient in a lateral position. However, in this case, the surgical procedure was conducted with the patient in a supine position because of the initial diagnosis of an anterior mediastinal tumor. Consequently, the upper left lobe was retracted dorsally, providing an excellent field of view. In addition, RATS, which enables precise and intricate maneuvers, proved to be instrumental in the safe dissection of the atypical structure connected to the EPS.
In conclusion, we initially suspected a mediastinal tumor preoperatively but diagnosed it as an EPS during surgery, subsequently excising it by RATS. Despite the presence of abnormal vessels draining into the PA and PV, we performed a safe and effective resection through RATS.
Acknowledgments
The Supplemental Figure can be viewed in the online version of this article [https://doi.org/10.1016/j.atssr.2024.01.009] on http://www.annalsthoracicsurgery.org.
Funding Sources
The authors have no funding sources to disclose.
Disclosures
The authors have no conflicts of interest to disclose.
Patient Consent
Obtained.
Supplementary Data
Supplemental Figure.
References
- 1.Liu X., Wu R., Zhu S., Gu L., Tang Z. Imaging and pathological characteristics, treatment, and prognosis of pulmonary sequestration—a retrospective study of 13 cases. Clin Respir J. 2023;17:865–873. doi: 10.1111/crj.13672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wei Y., Li F. Pulmonary sequestration: a retrospective analysis of 2625 cases in China. Eur J Cardiothorac Surg. 2011;40:e39–e42. doi: 10.1016/j.ejcts.2011.01.080. [DOI] [PubMed] [Google Scholar]
- 3.Abbey P., Das C.J., Pangtey G.S., Seith A., Dutta R., Kumar A. Imaging in bronchopulmonary sequestration. J Med Imaging Radiat Oncol. 2009;53:22–31. doi: 10.1111/j.1754-9485.2009.02033.x. [DOI] [PubMed] [Google Scholar]
- 4.Chen-Yoshikawa T.F., Fukui T., Nakamura S., et al. Current trends in thoracic surgery. Nagoya J Med Sci. 2020;82:161–174. doi: 10.18999/nagjms.82.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fukui T., Hakiri S., Yokoi K. Extralobar pulmonary sequestration in the middle mediastinum. Gen Thorac Cardiovasc Surg. 2017;65:481–483. doi: 10.1007/s11748-016-0735-z. [DOI] [PubMed] [Google Scholar]
- 6.Shadmehr M.B., Jamaati H.R., Saidi B., Tehrai M., Arab M. Extralobar sequestration in anterior mediastinum with pericardial agenesis. Ann Thorac Surg. 2009;88:291–293. doi: 10.1016/j.athoracsur.2008.12.037. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.